Abstract
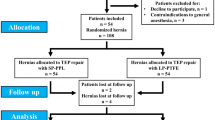
Our study was conducted to compare self-fixing lightweight polyester mesh (group I) to the standard heavy weight polypropylene mesh (group II) using tension-free Lichtenstein hernioplasty as regard to the effect of mesh implantation and perimesh fibrosis on testicular blood flow. 80 patients with uncomplicated inguinal hernia were divided in two groups. Doppler ultrasonography measured testicular volume, testicular artery velocity preoperative and 3rd month post operative. Blood flow in the testicles was represented by resistive index (RI). No case of testicular atrophy occurred in either group, however, in both groups a significant postoperative decrease in testicular volume (p = 0.001 in group I and p < 0.001 in group II) was accompanied by a significant increase in RI as compared to their pre-operative values (p < 0.001 in group I and p = 0.009 in group II). Comparing the two groups, patients in group I showed higher values of decrease in testicular volume accompanied by more increase in RI values postoperatively compared to group II patients, but these values did not reach a significant value (p = 0.107, p = 0.136). There was a significant increase in the number of post-operative varicocele and hydrocele in group I compared to group II. Mesh implantation has an effect on testicular size and blood flow by decreasing the testicular size and increasing the RI. This effect was more obvious in the parietex progrip. Although there is an indirect relation between RI and the sperm count, testicular blood flow alone is not enough to judge fertility.
Similar content being viewed by others
References
Yamaguchi K, Ishikawa T, Nakano Y, Kondo Y, Shiotani M, Fujisawa M (2008) Rapidly progressing, late-onset obstructive azoospermia linked to herniorrhaphy with mesh. Fertil Steril 90(5):e5–e7
Shin D, Lipshultz LI, Goldstein M, Barme GA, Fuchs EF, Nagler HM et al (2005) Herniorrhaphy with polypropylene mesh causing inguinal vasal obstruction: a preventable cause of obstructive azoospermia. Ann Surg 241(4):553–558
Ramadan SU, Gokharman D, Tuncbilek I, Ozer H, Kosar P, Kacar M et al (2009) Does the presence of a mesh have an effect on the testicular blood flow after surgical repair of indirect inguinal hernia? J Clin Ultrasound 37(2):78–81
Klinge U, Klosterhalfen B, Muller M, Schumpelick V (1999) Foreign body reaction to meshes used for the repair of abdominal wall hernias. Eur J Surg 165(7):665–673
Klosterhalfen B, Klinge U, Hermanns B, Schumpelick V (2000) Pathology of traditional surgical nets for hernia repair after long-term implantation in humans. Der Chirurg 71(1):43–51
Tekatli H, Schouten N, van Dalen T, Burgmans I, Smakman N (2012) Mechanism, assessment, and incidence of male infertility after inguinal hernia surgery: a review of the preclinical and clinical literature. Am J Surg 204(4):503–509
Uzzo RG, Lemack GE, Morrissey KP, Goldstein M (1999) The effects of mesh bioprosthesis on the spermatic cord structures: a preliminary report in a canine model. J Urol 161(4):1344–1349
Peiper C, Junge K, Klinge U, Strehlau E, Krones C, Ottinger A et al (2005) The influence of inguinal mesh repair on the spermatic cord: a pilot study in the rabbit. J Invest Surg 18(5):273–278
Ridgway PF, Shah J, Darzi AW (2002) Male genital tract injuries after contemporary inguinal hernia repair. BJU Int 90(3):272–276
Fitzgibbons RJ Jr (2005) Can we be sure polypropylene mesh causes infertility? Ann Surg 241(4):559–561
Hallen M, Sandblom G, Nordin P, Gunnarsson U, Kvist U, Westerdahl J (2011) Male infertility after mesh hernia repair: a prospective study. Surgery 149(2):179–184
Aydede H, Erhan Y, Sakarya A, Kara E, Ilkgul O, Can M (2003) Effect of mesh and its localisation on testicular flow and spermatogenesis in patients with groin hernia. Acta Chir Belg 103(6):607–610
Sucullu I, Filiz AI, Sen B, Ozdemir Y, Yucel E, Sinan H et al (2010) The effects of inguinal hernia repair on testicular function in young adults: a prospective randomized study. Hernia 14(2):165–169
Valenti G, Baldassarre E, Torino G (2006) Vas deferens obstruction due to fibrosis after plug hernioplasty. Am Surg 72(2):137–138
Pinggera GM, Mitterberger M, Bartsch G, Strasser H, Gradl J, Aigner F et al (2008) Assessment of the intratesticular resistive index by colour Doppler ultrasonography measurements as a predictor of spermatogenesis. BJU Int 101(6):722–726
Chastan P (2006) Tension free open inguinal hernia repair using an innovative self gripping semi-resorbable mesh. J Minim Access Surg 2(3):139–143
Chastan P (2009) Tension-free open hernia repair using an innovative self-gripping semi-resorbable mesh. Hernia 13(2):137–142
Mihmanli I, Kantarci F, Kulaksizoglu H, Gurses B, Ogut G, Unluer E et al (2004) Testicular size and vascular resistance before and after hydrocelectomy. AJR Am J Roentgenol 183(5):1379–1385
Celik AS, Memmi N, Celebi F, Guzey D, Celik A, Kaplan R et al (2009) Impact of slit and nonslit mesh technique on testicular perfusion and volume in the early and late postoperative period of the totally extraperitoneal preperitoneal technique in patients with inguinal hernia. Am J Surg 198(2):287–291
Lichtenstein IL, Shulman AG, Amid PK, Montllor MM (1989) The tension-free hernioplasty. Am J Surg 157(2):188–193
Beddy P, Ridgway PF, Geoghegan T, Peirce C, Govender P, Keane FB et al (2006) Inguinal hernia repair protects testicular function: a prospective study of open and laparoscopic herniorraphy. J Am Coll Surg 203(1):17–23
Bendavid R (2004) The unified theory of hernia formation. Hernia 8(3):171–176
Akbulut G, Serteser M, Yucel A, Degirmenci B, Yilmaz S, Polat C et al (2003) Can laparoscopic hernia repair alter function and volume of testis? Randomized clinical trial. Surg Laparosc Endosc Percutan Tech 13(6):377–381
Lima Neto EV, Goldenberg A, Juca MJ (2007) Prospective study on the effects of a polypropylene prosthesis on testicular volume and arterial flow in patients undergoing surgical correction for inguinal hernia. Acta Cir Bras 22(4):266–271
Wantz GE (1993) Testicular atrophy as a risk of inguinal hernioplasty. II Giornale di Chir 14(4–5):205–206
Peeters E, Spiessens C, Oyen R, De Wever L, Vanderschueren D, Penninckx F et al (2010) Laparoscopic inguinal hernia repair in men with lightweight meshes may significantly impair sperm motility: a randomized controlled trial. Ann Surg 252(2):240–246
Zinther NB, Wara P, Friis-Andersen H (2010) Shrinkage of intraperitoneal onlay mesh in sheep: coated polyester mesh versus covered polypropylene mesh. Hernia 14(6):611–615
LeBlanc KA, Booth WV, Whitaker JM, Baker D (1998) In vivo study of meshes implanted over the inguinal ring and external iliac vessels in uncastrated pigs. Surg Endosc 12(3):247–251
Peiper C, Junge K, Klinge U, Strehlau E, Ottinger A, Schumpelick V (2006) Is there a risk of infertility after inguinal mesh repair? Experimental studies in the pig and the rabbit. Hernia 10(1):7–12
Goldenberg A, Paula JF (2005) Effects of the polypropylene mesh implanted through inguinotomy in the spermatic funiculus, epididim and testis of dogs. Acta Cir Bras 20(6):461–467
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Heba El Komy, Ahmed El-Gendi, Wael Abdel-salam, Mohamed Elseidy, Elsaid Elkayal declare that they have no conflict of interest.
Research involving human participants and/or animals
The ethics committee and review board in our institute approved the study and treatment protocol.
Informed consent
Informed consent was obtained from all patients who agreed to participate in the study.
Rights and permissions
About this article
Cite this article
El-Komy, H., El-Gendi, A., Abdel-salam, W. et al. Self-fixing parietex progrip versus the standard sutured prolene mesh in tension-free repair of inguinal hernia: effect on testicular volume and testicular blood flow. Updates Surg 70, 513–520 (2018). https://doi.org/10.1007/s13304-018-0554-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0554-0