Abstract
Nutritional depletion is commonly observed in patients undergoing surgical treatment for a gastrointestinal malignancy. An appropriate nutritional intervention could be associated with improved postoperative outcomes. The study was aimed to determine the effect of a program of gastrointestinal rehabilitation and early postoperative enteral nutrition upon complications and clinical outcomes in patients who experienced gastrointestinal surgery for cancer. This is a prospective study (2013 January–2015 December) of 465 consecutive patients submitted to gastrointestinal surgery for cancer and admitted to an Oncological Intensive Care Unit. The program of gastrointestinal rehabilitation and early postoperative enteral nutrition consisted on: (1) general rules: pain relive, early mobilization, antibiotic prophylaxis, deep vein thrombosis prophylaxis and respiratory physiotherapy; and (2) gastrointestinal rules: gastric protection, control of postoperative nausea and vomiting, early nasogastric tube remove and early enteral nutrition. The most frequent surgical sites were colorectal (44.9%), gynecological with intestinal suturing (15.7%) and esophagus/stomach (11.0%). Emergency surgery was performed in 12.7% of patients. The program of intestinal rehabilitation and early postoperative enteral nutrition reduced major complications (19.2 vs. 10.2%; p = 0.030), respiratory complications (p = 0.040), delirium (p = 0.032), infectious complications (p = 0.047) and gastrointestinal complications (p < 0.001). Intensive care unit mortality (p = 0.018), length of intensive care unit stay (p < 0.001) and length of hospitalization (p < 0.001) were reduced as well. A program of gastrointestinal rehabilitation and early postoperative enteral nutrition is associated with reduced postoperative complications and improved clinical outcomes in patients undergoing gastrointestinal surgery for cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nutritional depletion is commonly observed in patients undergoing surgical treatment for a gastrointestinal malignancy. Studies have indicated a prevalence of 40–80% [1]. A variety of factors are related with perioperative malnutrition, including cancer nature, local effect of tumor, clinical stage of cancer, as well as chemotherapy and radiotherapy. Nausea, vomiting, decreased appetite, early satiety, taste changes, diarrhea, pain, mucositis, physical obstruction of gastrointestinal tract and malabsorption could result in weight loss, which consecutively is a strong prognostic factor of poor outcome in terms of survival and response to treatment [2].
In addition, some patients with gastrointestinal solid tumor develop cancer cachexia, which is a complex syndrome characterized by chronic, progressive and involuntary weight loss, as well as poorly or only partially responsive to standard nutritional support [3]. It is estimated that about 30–50% of all cancer death are related with cancer cachexia [1].
Compared with well-nourished gastrointestinal cancer patients, the risk of postoperative complications is two-fold higher for those with malnutrition [4]. Accordingly, an appropriate nutritional intervention has a positive effect on postoperative outcomes in this subgroup of patients [5].
In the last years, early enteral nutritional is recommended for postoperative gastrointestinal patients because it is associated with enhanced gastrointestinal recovery and lower complication rates [6,7,8]. This study was aimed to determine the effect of a program of gastrointestinal rehabilitation and early postoperative enteral nutrition (IREPEN) on postoperative complications and clinical outcomes in patients underwent gastrointestinal surgery for cancer.
Methods
Design and setting
This was a prospective cohort study (January 2013–December 2015) conducted in the oncological ICU (OICU) of the Institute of Oncology and Radiobiology (IOR). This is a 220-bed, university-affiliated, tertiary care referral center for cancer patients in Havana, Cuba. The OICU is a multidisciplinary medical and surgical unit (with intensivists, anesthesiologists and internists available) with 12 beds, which takes care only of oncologic patients. The current study was conducted in accordance with the Declaration of Helsinki, and it was approved by the Scientific Council and the Ethics Committee for Scientific Research of the IOR. Written informed consent was obtained from all patients.
Participants
A total of 1368 consecutive cancer patients were admitted to the OICU during the study period; of these, 493 underwent gastrointestinal tract surgery (esophagus, stomach, pancreas/liver/biliary tract, small intestine, or colorectal, as well as retroperitoneum, urological or gynecological surgery with intestinal suturing) were included. Patients submitted to palliative surgery and those with incomplete tumor resection were excluded, considering that patients in advanced stages can show basic features that distinguish them from those with cancer in remission (Fig. 1). Thus, their exclusion reduced the risk of selection bias.
Program of gastrointestinal rehabilitation and early postoperative enteral nutrition
The program of gastrointestinal rehabilitation and early postoperative enteral nutrition consisted on:
-
1.
General measures: (a) multimodal analgesia: non-steroidal anti-inflammatory drugs, peridural analgesia and rescue intravenous opioids; (b) early mobilization: outside-bed exercises within first 48 h for non-ventilated patients; (c) antibiotic prophylaxis; (d) deep vein thrombosis prophylaxis; and (e) respiratory physiotherapy.
-
2.
Gastrointestinal measures: (a) gastric protection: anti-H2, proton pump inhibitor or sucralfate; (b) control of postoperative nausea and vomiting (PNV): ondansetron and/or metoclopramide; (c) nasogastric tube remove within first 48 h for non-ventilated patients; and (d) beginning of enteral nutrition within first 48 h. Non-ventilated patients received a similar or better oral feeding (in quality and volume) than those received before surgery at fifth postoperative day. Ventilated patients received the total daily caloric requirements by enteral route at fifth postoperative day. Mixed nutrition was started at seventh postoperative day if these nutritional goals were not achieved.
Data collection and outcomes
The following demographic and clinical data were obtained at OICU admission: age, sex, emergency surgery, American Society of Anesthesiologists Physical Status Score (ASA-PS), location of the surgery, surgical time, Acute Physiology and Chronic Health Evaluation (APACHE) II score, and the need of invasive mechanical ventilation.
Postoperative complications were daily monitored during the patient’s stay in the OICU. Respiratory, neurological, infectious and surgical wound complications were defined according to the Postoperative Morbidity Survey (POMS) [9]. Prolonged postoperative ileus [10] and anastomotic leak [11] were defined as previously described. Major postoperative complication was defined as the need of unplanned reoperation and/or organ failure [12].
The OICU mortality, length of OICU stay, hospital mortality, length of hospital stay, and unplanned OICU readmission were assessed as clinical outcomes.
For those patients who were admitted more than once to the OICU during the same hospitalization, only the first data on OICU admission were analyzed.
Statistical analysis
Categorical variables are showed as count with percentage and numerical variables as mean with standard deviation (SD). Difference between groups was performed using Pearson’s Chi-square test (χ2) or Fisher’s exact test as appropriated for categorical variables; t test was used for numerical variables. The study period was 3 years, from 2013 to 2015. The year 2013 was taken as a reference year for all comparisons.
Statistical test with a two tailed p value ≤ 0.05 was considered as significant. Data were analyzed using IBM® SPSS® Statistics 23.0 (IBM, Chicago, IL, USA).
Results
Characteristics of study population
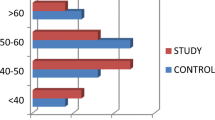
A total of 465 patients were analyzed. The main characteristics of study population are depicted in Table 1. The mean age was 63.7 years (SD 9.7 years). Advanced cancer (stage IIIb–IV) was observed in 106 (22.8%) patients. The most common surgical site was colorectal (44.9%), followed by gynecological with intestinal suturing (15.7%) and esophagus/stomach surgery (11.0%). Emergency surgery was carried out in 12.7% of subjects. The mean APACHE II score was 11.4 points (SD 3.6 points). Thirty-one patients (6.8%) required invasive ventilator support during their stay in ICU.
Application of the program of gastrointestinal rehabilitation and early postoperative enteral nutrition
Along the study period, antibiotic prophylaxis, deep vein thrombosis prophylaxis and gastric protection were implemented in 100, 97.6 and 100% of cases, respectively. Control of PNV (77.6%) and multimodal analgesia (47.3%) were highly implemented as well. However, there were no significant difference among years regarding multimodal analgesia, antibiotic prophylaxis, deep vein thrombosis prophylaxis and gastric protection (Table 2).
Respiratory physiotherapy (2014, p value = 0.011; 2015, p value < 0.001), early mobilization (2014, p value < 0.045; 2015, p value < 0.001), PNV prophylaxis (2015, p value < 0.001), early nasogastric tube remove (2014, p value < 0.001; 2015, p value < 0.001) and early enteral nutrition (2014, p value < 0.001; 2015, p value < 0.001) were significantly improved (Table 2).
Postoperative complications
At least one postoperative complication occurred across 87 participants (18.7%), for a total of 149 complications. Major complications occurred in 52 subjects (11.2%); of these, 36 (69.2%) required unplanned reoperation. Forty-four patients (9.5%) developed gastrointestinal complications. Surgical site infection, respiratory complications and delirium were observed in 8.0, 6.5 and 6.0% of patients, respectively. Total infectious complications accounted for 14.8% of all complications.
Compared with year 2013, a reduction in major complication (2015, p = 0.030), respiratory complications (2015, p value = 0.040), delirium (2015, p value = 0.032), infectious complications (2015, p value = 0.047), total gastrointestinal complications (2014, p value < 0.001; 2015, p value < 0.001) and anastomotic leak (2014, p value = 0.049; 2015, p value = 0.033) was found (Table 3).
Postoperative clinical outcomes
Forty-nine patients (10.5%) died during their stay in OICU because of septic shock (32 patients), acute respiratory failure (11 patients), cardiovascular disorders (3 patients), postoperative stroke (1 patients), drug-induced acute liver failure (1 patient) and hypovolemic shock due to massive intra-abdominal hemorrhage (1 patient). Additionally, other 17 patients died after being readmitted to the OICU (eight patients died from septic shock, five from acute cardiovascular disorders and four from acute respiratory failure), and three patients died in hospital wards after being transferred from OICU (these patients were not readmitted to OICU because the oncologist and the OICU physician were agreed that patients had not a potential chance of recovering from the acute problem). Therefore, the hospital mortality rate was 14.8% (69 patients); of these patients, 39 (56.5%) experienced emergency surgery and 51 (73.9%) had advanced cancer.
Mean length of OICU and hospital stay was 3.1 days (SD 1.0 days) and 8.7 days (SD 2.9 days), respectively. The OICU mortality (2015, p value = 0.018), length of OICU stay (2015, p value < 0.001) and length of hospitalization (2014, p value < 0.001; 2015, p value = 0.004) decreased compared with year 2013 (Table 4).
Discussion
The IREPEN program was developed according to the particular conditions of the OICU, and current therapeutic strategies in postoperative cares. Consequently, our results have a practical implication in the context of modern medicine. A reduction in respiratory complications, delirium, infectious complications, gastrointestinal complications, as well as clinical outcomes was achieved with the IREPEN program application.
The mortality rate was high considering that almost 50% of the series was colorectal surgery. There are four reasons. First, more than 55% of patients experienced emergency surgery, and almost 75% had advanced cancer. Previous studies reported that both emergency surgery and advanced cancer have been associated with increased mortality in patients with intra-abdominal malignancy [13, 14]. Second, high-risk surgeries have been increasing in the past years including esophagectomy, duodeno-pancreatic surgery, liver resection and bile duct surgery, and other intrabdominal surgeries with extensive tissue resection [15]. Third, ASA-PS grade III was found in 36.1% of patients, that is, patients with severe systemic disease at higher risk for postoperative complications [16]. Fourth, mortality rate after abdominal surgery is related with the development of complications. The magnitude of this effect might vary depending on the type of complication. We previously found that respiratory, cardiovascular, gastrointestinal, and renal complications, as well as postoperative infection were associated with higher mortality in cancer patients undergoing abdominal surgery [9].
Postoperative care was not performed according to standardized protocol before 2013. Consequently, several postoperative goals were not achieved such as PNV control, early nasogastric tube remove, early enteral nutrition, respiratory physiotherapy, and early mobilization. On the other hand, during the study period between 2013 and 2015 the IREPEN program was implemented. This fact enhanced the achievement of postoperative goals; and consequently reduced the postoperative complications and improved the clinical outcomes. This is a sort of learning curve of the IREPEN program application, which should be taken into account to be implemented on other scenario.
Other protocols designed to improve outcomes after abdominal surgery, such as the enhanced recovery after surgery (ERAS) program, showed positive results in previous studies. The ERAS program is widely used in many countries around the world, particularly in Europe and United States [17]. The ERAS program has been associated with an accelerated gastrointestinal recovery, lower postoperative complication rates and a reduction in length of hospitalization [18,19,20,21,22].
The IREPEN program was centered in early nasogastric tube remove and early enteral postoperative nutrition. Traditionally, nasogastric tube is placed in the operating room for patients undergoing an abdominal surgery and remains in place several days after operation. However, more than 30 years ago scientific evidence has grown with regard to disadvantages of this strategy because of lack of beneficial effects, insufficient perioperative enteral nutrition and higher postoperative complication rates [7].
Routine postoperative nasogastric tube is associated with patients’ discomfort, anxiety, depression and delirium; increased swallow reflex, which lead to pharyngeal lesions, aerophagia and hydro-electrolytic loss; rhinitis, pharyngitis and sinusitis causing pain, fiver and secondary pneumonia; infective and non-infective pulmonary complications with the need of oxygen and ventilatory support; prolonged postoperative ileus producing discomfort, delayed enteral nutrition and risk of aspiration. On the other hand, beneficial effects of nasogastric tube concerning gastric distension and PNV are limited [23].
In complex gastrointestinal surgeries such as pancreatoduodenectomy, Choi et al. observed no beneficial effects of routine postoperative nasogastric tube on respiratory, gastrointestinal (including anastomotic leak, delayed gastric emptying and postoperative ileus) or surgical wound complications [24]. Fisher et al. found similar results [25]. A meta-analysis conducted by Nelson et al. demonstrated that early nasogastric tube remove in postoperative abdominal patients is associated with enhanced gastrointestinal recovery (p < 0.00001) and reduction in respiratory complication (p = 0.01). In addition, no difference was observed between patients with nasogastric tube and those without nasogastric tube regarding anastomotic leak [26]. Therefore, nasogastric tube in postoperative period of abdominal surgery should be avoided as routine practice because its clinical advantages are minimal and complications could be facilitated.
Early enteral nutrition after surgery, either as standard nutrition or immunonutrition, is associated with lower complication rates and improved clinical outcomes. In patients underwent esophageal surgery for cancer, Wang et al. found that early enteral nutrition reduced infectious complications (p = 0.003), pneumonia (p = 0.008) and total postoperative complications (p = 0.006), as well as the length of hospitalization (p < 0.0001). Thoracic drainage-fluid volume (p = 0.009), time to first defecation (p < 0.0001), changes in serum albumin (p = 0.001) and total proteins concentration (p < 0.0001) were reduced as well [8]. Another recent study and a systematic review confirmed that early enteral nutrition is a safety strategy for these patients [27, 28].
After surgical treatment in patients with gastric cancer, Li et al. found that early enteral nutrition was associated with lesser postoperative fiver (p < 0.05), lower anal exhaust time (78.8 ± 9.3 vs. 85.3 ± 8.4 h; p < 0.05), and shorter length of hospital stay (7.73 ± 2.13 vs. 9.77 ± 1.76 days; p < 0.01) [6]. A beneficial effect on immunological, inflammatory and nutritional status was also observed in this study. At postoperative days 3 and 7, the CD3+, CD4+ and natural killer cell, albumin and prealbumin levels, and CD4+/CD8+ ratio were significantly higher in the early enteral nutrition group than those in the delayed enteral nutrition group (all p < 0.05). CD8+ cell counts were significantly lower in the experimental group than those in the control group (p < 0.05) [6]. Others recent studies also confirmed a better inflammatory, immunological and nutritional pattern with early enteral nutrition in operated patients for a gastric cancer [29, 30].
Early enteral nutrition was also associated with enhanced gastrointestinal recovery, shorter time to gas and stools passage, superior protein synthesis, lower gastrointestinal complication rates and shorter length of hospital stay in operated patients for a colorectal cancer [31, 32]. A recent meta-analysis of 15 randomized controlled trials in 1240 patients undergoing abdominal surgery demonstrated that early enteral nutrition is associated with reduced postoperative complication rates (odds ratio 0.55; 95% confidence interval 0.35–0.87) [33].
Consequently, early enteral nutrition in patients undergoing gastrointestinal surgery for cancer is related with improved nutritional, inflammatory and immunological status; enhanced gastrointestinal function and patients’ comfort; reduced postoperative complication rates and improved clinical outcomes.
Strengths of this study include its prospective nature and the composition of the included patients. Prior studies in this field have limited enrolment to only patients undergoing specific operation such as esophageal, gastric, pancreatoduodenectomy or colorectal surgery. Thus, composition of our studied patients was more representative of current clinical settings. However, it has several shortcomings. First, the study design was not a randomized controlled trial. Second, although the sample size was acceptable for a single center investigation, it could be considered as a limitation. Third, nutritional variables were not directly measured.
Conclusions
A program of gastrointestinal rehabilitation and early postoperative enteral nutrition is associated with reduced medical and surgical complications, and improved postoperative clinical outcomes in patients undergoing gastrointestinal surgery for cancer. This strategy of treatment contributes to progress in improving the quality of care for abdominal cancer patients in the postoperative period. In addition, it could be an alternative to a more complex therapeutic scheme such as the ERAS program. Nevertheless, randomized controlled trials confirming our results are needed.
References
Osland EJ, Memon MA (2010) Early postoperative feeding in resectional gastrointestinal surgical cancer patients. World J Gastrointest Oncol 2:187–191
PDQ Supportive and Palliative Care Editorial Board (2017) Nutrition in cancer care (PDQ): health professional version. PDQ cancer information summaries. Bethesda (MD): National Cancer Institute (US)
Ozorio GA, Barão K, Forones NM (2017) Cachexia stage, patient-generated subjective global assessment, phase angle, and handgrip strength in patients with gastrointestinal cancer. Nutr Cancer 19:1–8
Garth AK, Newsome CM, Simmance N, Crowe TC (2010) Nutritional status, nutrition practices and post-operative complications in patients with gastrointestinal cancer. J Hum Nutr Diet 23:393–401
Wanden-Berghe C, Sanz-Valero J, Arroyo-Sebastián A, Cheikh-Moussa K, Moya-Forcen P (2016) Effects of a nutritional intervention in a fast-track program for a colorectal cancer surgery: systematic review. Nutr Hosp 33:402
Li B, Liu HY, Guo SH, Sun P, Gong FM, Jia BQ (2015) Impact of early postoperative enteral nutrition on clinical outcomes in patients with gastric cancer. Genet Mol Res 14:7136–7141
Abunnaja S, Cuviello A, Sanchez JA (2013) Enteral and parenteral nutrition in the perioperative period: state of the art. Nutrients 5:608–623
Wang G, Chen H, Liu J, Ma Y, Jia H (2015) A comparison of postoperative early enteral nutrition with delayed enteral nutrition in patients with esophageal cancer. Nutrients 7:4308–4317
Martos-Benítez FD, Gutiérrez-Noyola A, Echevarría-Víctores A (2016) Postoperative complications and clinical outcomes among patients undergoing thoracic and gastrointestinal cancer surgery: a prospective cohort study. Rev Bras Ter Intensiva 28:40–48
Gero D, Gié O, Hübner M, Demartines N, Hahnloser D (2017) Postoperative ileus: in search of an international consensus on definition, diagnosis, and treatment. Langenbecks Arch Surg 402:149–158
Chadi SA, Fingerhut A, Berho M, DeMeester SR, Fleshman JW, Hyman NH et al (2016) Emerging trends in the etiology, prevention, and treatment of gastrointestinal anastomotic leakage. J Gastrointest Surg 20:2035–2051
Martos Benítez FD, Guzmán Breff BI, Betancourt Plaza I, González Martínez I (2016) Postoperative complications in thoracic and abdominal surgery: definitions, epidemiology and severity. Rev Cub Cir 55:40–53
Bos MM, de Keizer NF, Meynaar IA, Bakhshi-Raiez F, de Jonge E (2012) Outcomes of cancer patients after unplanned admission to general intensive care units. Acta Oncol 51:897–905
Xia R, Wang D (2016) Intensive care unit prognostic factors in critically ill patients with advanced solid tumors: a 3-year retrospective study. BMC Cancer 16:188
Kristensen SD, Knuuti J, Saraste A, Anker S, Bøtker HE, De Hert S et al (2014) 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management. The Joint Task Force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur J Anaesthesiol 31:517–573
Barnett S, Moonesinghe SR (2011) Clinical risk scores to guide perioperative management. Postgrad Med J 87:535–541
Knott A, Pathak S, McGrath JS, Kennedy R, Horgan A, Mythen M et al (2012) Consensus views on implementation and measurement of enhanced recovery after surgery in England: Delphi study. BMJ Open 2:e001878
Bona S, Molteni M, Rosati R, Elmore U, Bagnoli P, Monzani R et al (2014) Introducing an enhanced recovery after surgery program in colorectal surgery: a single center experience. World J Gastroenterol 20:17578–17587
Greco M, Capretti G, Beretta L, Gemma M, Pecorelli N, Braga M (2014) Enhanced recovery program in colorectal surgery: a meta-analysis of randomized controlled trials. World J Surg 38:1531
Varadhan KK (2010) Enhanced recovery after surgery: the future of improving surgical care. Crit Care Clin 26:527–547
Ni TG, Yang HT, Zhang H, Meng HP, Li B (2015) Enhanced recovery after surgery programs in patients undergoing hepatectomy: a meta-analysis. World J Gastroenterol 21:9209–9216
Małczak P, Pisarska M, Piotr M, Wysocki M, Budzyński A, Pędziwiatr M (2017) Enhanced recovery after bariatric surgery: systematic review and meta-analysis. Obes Surg 27:226–235
Tanguy M, Seguin P, Mallédant Y (2007) Bench-to-bedside review: routine postoperative use of the nasogastric tube—utility or futility? Crit Care 11:201
Choi YY, Kim J, Seo D, Choi D, Kim MJ, Kim JH et al (2011) Is routine nasogastric tube insertion necessary in pancreaticoduodenectomy? J Korean Surg Soc 81:257–262
Fisher WE, Hodges SE, Cruz G, Artinyan A, Silberfein EJ, Ahern CH et al (2011) Routine nasogastric suction may be unnecessary after a pancreatic resection. HPB 13:792–796
Nelson R, Edwards S, Tse B (2007) Prophylactic nasogastric decompression after abdominal surgery. Cochrane Database Syst Rev 3:CD004929
Manba N, Koyama Y, Kosugi S, Ishikawa T, Ichikawa H, Minagawa M et al (2014) Is early enteral nutrition initiated within 24 hours better for the postoperative course in esophageal cancer surgery? J Clin Med Res 6:53–58
Wheble GAC, Benson RA, Khan OA (2012) Is routine postoperative enteral feeding after oesophagectomy worthwhile? Interact Cardiovasc Thorac Surg 15:709–712
Wang F, Hou MX, Wu XL, Bao LD, Dong PD (2015) Impact of enteral nutrition on postoperative immune function and nutritional status. Genet Mol Res 14:6065–6072
Ding D, Feng Y, Song B, Gao S, Zhao J (2015) Effects of preoperative and postoperative enteral nutrition on postoperative nutritional status and immune function of gastric cancer patients. Turk J Gastroenterol 26:181–185
Boelens PG, Heesakkers FF, Luyer MD, van Barneveld KW, de Hingh IH, Nieuwenhuijzen GA et al (2014) Reduction of postoperative ileus by early enteral nutrition in patients undergoing major rectal surgery: prospective, randomized, controlled trial. Ann Surg 259:649–655
Gianotti L, Nespoli L, Torselli L, Panelli M, Nespoli A (2011) Safety, feasibility, and tolerance of early oral feeding after colorectal resection outside an enhanced recovery after surgery (ERAS) program. Int J Colorectal Dis 26:747–753
Osland E, Yunus RM, Khan S, Memon MA (2011) Early versus traditional postoperative feeding in patients undergoing resectional gastrointestinal surgery: a meta-analysis. JPEN 35:473–487
Acknowledgements
The authors would like to thank Lucia Chang-Navarro for his help with the translation into English.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Research involving human participants and/or animals
This article does not involve any studies with animals.
Informed consent
This is a prospective study, and was therefore conducted in accordance with the Declaration of Helsinki. Written informed consent was obtained from all patients.
Rights and permissions
About this article
Cite this article
Martos-Benítez, F.D., Gutiérrez-Noyola, A., Soto-García, A. et al. Program of gastrointestinal rehabilitation and early postoperative enteral nutrition: a prospective study. Updates Surg 70, 105–112 (2018). https://doi.org/10.1007/s13304-018-0514-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-018-0514-8