Abstract
Objective
Diabetes Self-Management Education and Support (DSMES) is a critical component of diabetes care. This study aims to examine the effect of online-based educational interventions on diabetes management compared to face-to-face interventions.
Methods
A systematic review was conducted by searching three databases for studies in English or Spanish between December 2023 and March 2024. The inclusion criteria were studies that compared face-to-face DSMES with online interventions.
Results
The follow-up duration of the trials ranged from 1 to 12 months. Multidisciplinary teams delivered online DSMES through various means, including Short Message Service (SMS), telephone calls, video calls, websites, and applications. Online DSMES was found to be comparable to face-to-face interventions in terms of glycated hemoglobin (HbA1c) levels in people with type 1 diabetes (T1D). In contrast, online interventions that focus on weight management in people with type 2 diabetes (T2D) have shown a significant reduction in HbA1c compared to face-to-face interventions. Online DSMES was found to be superior in terms of quality of life and cost-effectiveness in both T1D and T2D. None of the analyzed studies explored the differences between individual and group methodologies.
Conclusions
The current evidence indicates that online DSMES services provide at least comparable biomedical benefits to face-to-face interventions, suggesting that online interventions could be incorporated into clinical practice as a complement or reinforcement. However, further research is needed to explore the potential benefits and effectiveness of online group sessions in DSMES.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Diabetes Self-Management Education and Support (DSMES) is essential for integrated care of people with diabetes. It may be delivered face-to-face or online. |
Online education has an advantage over face-to-face interventions because it can be delivered synchronously or asynchronously, with multiple benefits in both scenarios. |
The present systematic review aimed to evaluate the potential of online education to replace face-to-face interventions for individuals with diabetes, taking into account not only biomedical markers such as HbA1c but also psychosocial aspects. |
Online DSMES was found to be comparable to face-to-face interventions in terms HbA1c in people with type 1 diabetes (T1D) but superior in people with type 2 diabetes (T2D). |
Conversely, there was uniformity across both T1D and T2D in the superiority of online DSMES over face-to-face in terms of quality of life and cost-effectiveness. Instead of replacing one approach with another, online interventions could complement our clinical practice. |
Given the current time constraints and difficulties in balancing personal life, work, and health, online DSMES could provide easier access to knowledge for managing their condition on a daily basis, customized to the unique needs of individuals with diabetes. |
Introduction
Diabetes is a chronic disease that affects 537 million adults worldwide, or 1 in 10 people, and it is expected to increase to 643 million by 2030 [1]. This chronic condition requires continuous effort from the individual to manage their treatment and health behaviors in order to achieve an optimal physical and emotional state [2].
Diabetes Self-Management Education and Support (DSMES) is the cornerstone of integrated care for people with diabetes. It aims to provide a person-centered model of care that empowers individuals to make informed decisions, solve problems, set personal goals, and cope with the psychosocial burden of their condition in collaboration with their healthcare team [3, 4]. DSMES facilitates the development of competencies in knowledge, skills, and attitudes [5]. Thus, DSMES has led to a more personalized and comprehensive approach to educating people with diabetes by incorporating behavioral and self-management techniques into structured educational interventions [6]. Several studies have demonstrated the positive impact of DSMES not only on improving biomedical outcomes such as glycated hemoglobin (HbA1c), cardiovascular events, and mortality risk, but also on psychosocial outcomes such as quality of life, disease knowledge and daily management, while reducing healthcare costs [2, 7,8,9,10,11].
DSMES should be provided using technology to make education and training more accessible [2], without requiring a change in treatment type or insulin titration. In particular, online DSMES has an advantage over face-to-face interventions because it can be delivered synchronously (in real time) and asynchronously (delayed), with multiple benefits in both scenarios [12]. Health information technologies have been shown to effectively improve HbA1c levels in people with type 2 diabetes (T2D) compared to face-to-face care, as well as in people with type 1 diabetes (T1D) [12,13,14,15,16,17,18,19,20,21,22]. Although long-term studies assessing the barriers to proper self-care are lacking [23], most of the studies mentioned above compare online interventions with usual care. This indicates that the telematic medium could be a useful complementary tool, and face-to-face and online formats can coexist to optimize assistance. On the other hand, while some pre-2020 studies have evaluated the role of technology in diabetes [13], the COVID-19 pandemic undoubtedly triggered the use of online interventions in clinical practice, being online DSMES the main delivery method during the lockdown period [20]. However, further research is needed to fully understand the experiences and needs of people with diabetes in relation to the process of receiving DSMES. This will help to maximize the benefits of these technologies.
The significant changes in social relationships resulting from the emergence and rapid development of communication technologies, as well as the exponential increase in the use of technology in healthcare, particularly in diabetes, since the COVID-19 pandemic, lead us to question at what point online education could be established. Therefore, the aim of this review was to assess the potential of online education to replace face-to-face interventions.
Methods
Study Inclusion and Exclusion Criteria
Population
This review aimed to identify the outcomes of educational interventions for individuals diagnosed with T1D or T2D. Studies involving individuals with gestational diabetes, pre-diabetes, and interventions for chronic complications (retinopathy, diabetic foot, kidney disease) were excluded.
Intervention
Inclusion criteria included studies that compared outcomes of face-to-face and online DSMES. A DSMES intervention refers to all encounters, engagement, and interactions with the people with diabetes (PWD). A DSMES intervention includes individual and/or group sessions and is initiated with an assessment of the individual’s current concerns, needs, and priorities to create a DSMES plan of care guided by the PWD’s preferred delivery method and timing. The DSMES plan guides the delivery of sessions, utilizing a variety of methods, while supporting and reinforcing positive self-care behaviors [4].
Additionally, studies comparing online educational interventions with standard care were excluded (no structured educational intervention was specified to compare with standard care, which was defined as follow-up clinic visits with undefined educational content).
Outcomes
Studies that were eligible for inclusion examined outcomes related to diabetes management, such as HbA1c levels, knowledge, and quality of life.
Context and Study Design
Studies can be conducted in any context, including clinical and community settings, and in countries of any income level. Excluded from this review were comments, letters to the editor, and systematic reviews. Conference or poster abstracts were excluded due to the limited information provided.
Other Criteria
Only studies in English or Spanish were eligible for inclusion.
Search Strategy
A literature search was conducted using three electronic databases: PubMed, Cochrane, and CINAHL. The search terms used were diabetes mellitus, education, education programs, self-management education, telemedicine, telehealth, telecare, ehealth, online, and Internet based. The detailed search strategy is provided in Table S1 (see Table S1 in the electronic supplementary material for details).
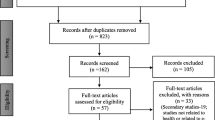
The papers were selected from December 2023 to March 2024 without any restrictions on the date of publication. The articles were manually searched and stored on Mendeley. The systematic review results were presented following the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [24] (see Fig. S1 in the electronic supplementary material for details). No published protocol is available for this systematic review.
Study Selection
One reviewer (NA) completed the search for studies and removed duplicates. The titles and abstracts were then blindly reviewed by two separate reviewers (NA and VP). Any disagreements regarding article relevance were resolved through discussion.
Data Extraction
Data extraction was performed by NA and reviewed by VP. Any disagreements were resolved through discussion. To ensure quality, we deemed it important for the studies to possess some of the characteristics suggested by the standards for identifying best practices in education. The 2022 National Standards include six main points: Standard (1) Support for DSMES Services (institutional support is necessary for the implementation of educational interventions), Standard (2) Population and Service Assessment (interventions should be individualized and tailored to the needs and preferences of people with diabetes), Standard (3) DSMES Team (the organization of educational interventions by a multidisciplinary team is recommended), Standard (4) Delivery and Design of DSMES Services (educational interventions should cover the following topics: ‘pathophysiology, healthy coping, healthy eating, being active, taking medication, monitoring, reducing risk, and problem-solving), Standard (5) Person-Centered DSMES (is a recurring process over the life span for people with diabetes), and Standard (6) Measuring and Demonstrating Outcomes of DSMES Services (continuous evaluation of educational interventions) [4]. Although there are various types of telematics interventions [25], we chose to concentrate on those with an educational focus. This is due to the high heterogeneity of educational interventions and their primary objectives.
Regarding the curriculum for these programs, they should include the following topics in a person-centered manner: healthy coping, healthy eating, being active, taking medication, monitoring, reducing risk, and problem solving [26]. For all these reasons, the extracted data includes the author and year, participants and sampling, compliance with the National Standards, main outcome, endpoint time, and results.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Results
Study Results and Characteristics
A total of 2041 publications were found in the three databases, resulting in 1706 for review after manually removing duplicates. Before screening, 1320 studies were excluded for not being in English or Spanish, being related to prediabetes or preventing diabetes, or treating diseases other than diabetes. A total of 386 records were available for screening, of which 366 were excluded as they did not compare face-to-face interventions with online interventions. We identified 20 publications. Details of all included studies can be found in Table S2 (see Table S2 in the electronic supplementary material for details).
Findings
Type of Diabetes for Intervention
Of the 20 studies selected, half were aimed at people with T2D [27,28,29,30,31,32,33,34,35,36], seven at people with T1D [37,38,39,40,41,42,43] and three at both type of diabetes [44,45,46]. Interventions targeting T2D addressed weight management, diabetes self-management, and diet. Interventions targeting T1D addressed carbohydrate counting, diabetes self-management, caregiver training, and fasting. Interventions targeting both types focused on diabetes self-management.
Main Objectives
Thirteen of the studies considered HbA1c as the primary endpoint [30,31,32,33,34,35,36, 38, 39, 41, 42, 45, 46]. Four studies included other metabolic parameters [29,30,31, 44], such as glucose, lipid profile, weight, and blood pressure. Three studies used validated self-management questionnaires [28, 31, 39]. Two of these studies included quality of life as the primary endpoint [27, 39]. Only one study presented cost as the primary endpoint [43].
Effect on HbA1c
In people with T1D, online interventions were not superior to face-to-face DSMES in terms of HbA1c levels, neither in short-term (3-month) nor long-term follow-up (12-month) [38, 39, 41, 42, 47]. In contrast, long-term online interventions focused on weight management in people with T2D showed a significant reduction in HbA1c [27, 34]. In a 12-month randomized controlled trial including 563 adults with T2D, the use of online tools for weight management was associated with a reduction of 0.32% in HbA1c compared to an increase of 0.16% in HbA1c in the in person-training group [34]. When interventions focused on diabetes self-management, only three studies showed differences in HbA1c between the interventions. An improvement was observed in the online group. These studies targeted adults with both T1D and T2D [29, 32, 44].
Quality of Life
In terms of quality of life, both studies that investigated this outcome found that the group that received the online intervention reported higher levels of perceived quality of life [27, 39]. Ayar et al. found that web-based diabetes education was an effective method for enhancing the quality of life of adolescents with T1D. Similarly, Holland-Carter et al. found that enhanced online weight program for individuals with T2D was superior in improving a range of psychosocial outcomes specific to T2D and obesity.
Cost-Effectiveness
Paxton’s study is the only one that presents results regarding cost. They concluded that online interventions saved both travel time and mileage, despite the time dedicated to training being the same [43]. Online education was associated with significant reductions in time and costs compared to face-to-face education. The time spent on travelling for delivering face-to-face education in a year was 124 h. However, in a year of online education, this time was reduced to 47 h. This resulted in a savings of 10 working days and approximately £1420. Additionally, there was a significant reduction in the number of miles driven, which had a positive impact on both the environment and costs.
Characteristics of Online DSMES Programs
The duration of the studies ranges from a minimum of 1 month to a maximum of 12 months: one study was conducted at 1 month [28], four at 3 months [30, 37, 44, 47], five at 6 months [36, 39, 41, 42, 46], one at 9 months [33], one at 10 months [32], and six at 1 year [27, 29, 31, 34, 35, 38].
Regarding intervention duration, it is often not reported in publications and can be a complex measure depending on the delivery format. Several methods exist for delivering online DSMES, including Short Message Service (SMS), e-mail, phone calls, video calls, websites, and applications. Asynchronous interventions, such as web consultations [29, 36], videos [30], or training messages [34, 38], can be difficult to time accurately. Synchronous interventions can last anywhere from 4 h to 3 weeks, depending on the scheduled training [28, 37, 42, 45, 46].
When 2022 National Standards for DSMES were evaluated, all of the studies meet Standards 1, 2, 5, and 6. However, for Standard 3, eleven studies described intervention by a multidisciplinary team [29, 30, 32, 35, 36, 38, 41, 42, 44, 46, 47]. Regarding Standard 4, which refers to the educational content that DSMES services should include, 12 studies included the required thematic completeness [28, 29, 31,32,33, 36, 38, 39, 43, 44, 46, 47]. None of the analyzed studies explore the differences between individual and group methodologies.
Discussion
While many studies have assessed the effectiveness of online interventions for individuals with diabetes, only a limited number have utilized technology to deliver structured education and included an active comparator. Nevertheless, current evidence indicates that online DSMES is at least as effective as face-to-face approaches in terms of both biomedical and psychosocial outcomes.
This systematic review described the potential of online DSMES for individuals with T1D or T2D, across both adolescents and adult populations. Most of the studies in this field compared online interventions with routine care (follow-up visits without any educational intervention defined) [13,14,15,16,17,18, 20,21,22, 48]. However, conclusions derived from these studies could be more related to DSMES itself than to the specific delivery method. Thus, the present study only selected studies with an active comparator. In contrast to studies without active comparator, online DSMES was not superior to face-to-face intervention in terms of HbA1c in people with diabetes. The effectiveness of online interventions is influenced by the user’s technological literacy and adherence to technology use [49]. The use of online DSMES was found to be most beneficial for patients who used the program more frequently [31, 50]. This relationship has been observed previously with continuous glucose monitoring systems, where a higher percentage of device use was associated with a greater reduction in HbA1c levels [51]. Various technologies can be used for online interventions to overcome digital barriers. These include mobile apps, the web, social media, gamification, and artificial intelligence [17, 23, 52,53,54,55,56]. In our constantly and rapidly changing technological environment, it is crucial to adapt to social changes in order to provide effective interventions.
Interestingly, the better results of online DSMES were observed when the intervention focused on weight management in people with T2D. In fact, these results were consistent with weight loss trials in people with T2D using anti-obesity drugs [34, 57]. Compared with people with T1D, those with T2D were older and less likely to receive diabetes education [58]. It is also important to note that access to both diabetes education and online tools is limited. Although adults over the age of 65 were receptive to using technology for diabetes education [59], Cherrez-Ojeda et al. [60], who studied 248 people with T2D, found that 72.8% did not have Internet access and less than half owned a smartphone. Therefore, it is important to consider users’ access to communication technologies in addition to their preferences. Using an online diabetes community can enhance the knowledge, self-care, and peer support of older adults with diabetes [61].
While the effect on HbA1c was at least equal between both delivery methods, there is a uniformity in the positive role of online DSMES over cost-effectiveness. As demonstrated by the results, Paxton noted a significant reduction in travel time and mileage when conducting education online [43]. Previous studies have shown that using online interventions in DSMES programs is a cost-saving strategy for both the person with T1D and the healthcare provider [62, 63]. Jansà et al. [16] found that online care, compared to routine care, resulted in lower costs for the person with T1D, including less time off work and lower transport costs, as well as for the healthcare provider. Similarly, Biermann et al. concluded that online management is a cost- and time-saving procedure [64].
Group-based online DSMES has only been evaluated to in few studies and in short-term precluding conclusions [65]. However, face-to-face DSMES using group sessions is widely used due to the numerous benefits observed [2, 66,67,68]. People with diabetes benefit from group sessions as they experience increased motivation and engagement in diabetes self-management. Additionally, group sessions have been shown to be cost-effective, enabling healthcare professionals to reach a larger number of people in each time frame [2, 67]. Online peer-to-peer interaction could be beneficial for managing diabetes daily. Internet forums offer a platform to exchange practical tips and insights based on personal experience, which goes beyond the theoretical information provided by healthcare professionals [69]. These forums also promote empowerment by encouraging individuals to take an active role in managing their health and condition [70]. However, it has been suggested by user experience data that providing asynchronous access to explanatory videos could be a beneficial option. This would allow individuals with diabetes to select content based on their knowledge or skill gaps. In general, healthcare professionals should consider exploring Internet forums as a new platform for group based DSMES [71].
It is important to note that the use of online tools requires compliance with the General Data Protection Regulation [72] of the country where the intervention takes place. Therefore, online DSMES programs must comply with regulations to ensure the safe use of user data. Additionally, new roles should be introduced in multidisciplinary care teams for people with diabetes, including those for information and communication technology, data management and legal departments [73]. Their collaboration should aim to reduce the potential risk associated with protecting personal and clinical data [72, 74].
Our study should be interpreted considering both its limitations and strengths. Among its strengths, the present review only selected studies with an active comparator (face-to-face DSMES). Previous systematic reviews included studies with an active control arm and routine care. When comparisons were made using routine care as a control arm, the conclusion of the study reflects more on the intervention itself than the delivery method [13, 14]. Thus, the inclusion criteria of the present study allowed us to address the main question about the superiority of one delivery method over another. Second, the present review evaluated both biomedical and psychosocial aspects of diabetes management, reflecting a comprehensive approach to the disease and its impact on patients’ well-being. However, limitations should also be acknowledged. First, the heterogeneity in the type of educational interventions presents a limitation in drawing conclusions. It is important to note that some of the selected studies focus on a single aspect of diabetes management, rather than the comprehensive approach that includes healthy coping, healthy eating, being active, taking medication, monitoring, reducing risk, and problem-solving, as per the standards of care [26]. Second, only six of the 20 studies included had a duration of 12 months [27, 29, 31, 34, 35, 38]. This duration is relatively short considering the chronic nature of the disease. To maintain diabetes control over time, individuals with diabetes require ongoing self-management support to sustain necessary self-care behaviors [4]. The effectiveness of educational interventions depends on maintaining the motivation of individuals to apply the knowledge and skills acquired in their daily lives. Therefore, it is essential to include the perspectives of individuals with diabetes in educational programs to ensure that they are tailored to their specific needs and preferences. Finally, studies involving individuals with gestational diabetes, pre-diabetes, and interventions for chronic complications were excluded, precluding conclusions in these populations.
Conclusions
Current evidence indicates that online DSMES can provide similar biomedical benefits to face-to-face interventions. Therefore, instead of replacing one approach with another, online interventions could complement our clinical practice. Given the current time constraints and difficulties in balancing personal life, work, and health, online DSMES could facilitate access to knowledge for the daily management of their condition, adapted to the specific needs of people with diabetes.
References
IDF Diabetes Atlas 10th edition [Internet]. www.diabetesatlas.org.
5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2022 45(Supplement_1):S60–82.
Hurley L, O’Donnell M, O’Hara MC, Carey ME, Willaing I, Daly H, et al. Is diabetes self-management education still the Cinderella of diabetes care? Vol 100 patient education and counseling. Elsevier Ireland Ltd; 2017. p. 1957–60.
Davis J, Fischl AH, Beck J, Browning L, Carter A, Condon JE, et al. 2022 national standards for diabetes self-management education and support. Diabetes Care. 2022;45(2):484–94.
Yoldi C. Formación en educación terapéutica en diabetes. Qué tenemos y qué nos falta? Avances en Diabetología. 2011;27(3):100–5.
Chatterjee S, Davies MJ, Heller S, Speight J, Snoek FJ, Khunti K. Diabetes structured self-management education programmes: a narrative review and current innovations. Vol 6 the lancet diabetes and endocrinology. Lancet Publishing Group; 2018. p. 130–42.
Hypoglycemia in the Diabetes Control and Complications Trial. The Diabetes control and complications trial research group. Diabetes. 1997;46(2):271–86.
2. NICE. Type 1 diabetes in adults: diagnosis and management.
Heller S, Lawton J, Amiel S, Cooke D, Mansell P, Brennan A, et al. Improving management of type 1 diabetes in the UK: the Dose Adjustment For Normal Eating (DAFNE) programme as a research test-bed. A mixed-method analysis of the barriers to and facilitators of successful diabetes self-management, a health economic analysis, a cluster randomised controlled trial of different models of delivery of an educational intervention and the potential of insulin pumps and additional educator input to improve outcomes. Prog Grants Appl Res. 2014;2(5):1–188.
Mühlhauser I, Bruckner I, Berger M, Cheţa D, Jörgens V, Ionescu-Tîrgovişte C, et al. Evaluation of an intensified insulin treatment and teaching programme as routine management of type 1 (insulin-dependent) diabetes. Diabetologia. 1987;30(9):681–90.
Reichard P, Nilsson BY, Rosenqvist U. The effect of long-term intensified insulin treatment on the development of microvascular complications of diabetes mellitus. N Engl J Med. 1993;329(5):304–9.
Pereira K, Phillips B, Johnson C, Vorderstrasse A. Internet delivered diabetes self-management education: a review. Diabetes Technol Ther. 2015;17(1):55–63.
Marcolino MS, Maia JX, Alkmim MBM, Boersma E, Ribeiro AL. Telemedicine application in the care of diabetes patients: systematic review and meta-analysis. PLoS ONE. 2013;8(11): e79246.
Eberle C, Stichling S. Telemetric interventions offer new opportunities for managing type 1 diabetes mellitus: systematic meta-review. JMIR Diabetes. 2021;6(1): e20270.
Ballesta S, Chillarón JJ, Inglada Y, Climent E, Llauradó G, Pedro-Botet J, et al. Telehealth model versus in-person standard care for persons with type 1 diabetes treated with multiple daily injections: an open-label randomized controlled trial. Front Endocrinol (Lausanne). 2023;27:14.
Jansà M, Vidal M, Viaplana J, Levy I, Conget I, Gomis R, et al. Telecare in a structured therapeutic education programme addressed to patients with type 1 diabetes and poor metabolic control. Diabetes Res Clin Pract. 2006;74(1):26–32.
Wang X, Shu W, Du J, Du M, Wang P, Xue M, et al. Mobile health in the management of type 1 diabetes: a systematic review and meta-analysis. BMC Endocr Disord. 2019;19(1):21.
Ruiz de Adana MS, Alhambra-Expósito MR, Muñoz-Garach A, Gonzalez-Molero I, Colomo N, Torres-Barea I, et al. Randomized study to evaluate the impact of telemedicine care in patients with type 1 diabetes with multiple doses of insulin and suboptimal HbA1c in Andalusia (Spain): PLATEDIAN study. Diabetes Care. 2020;43(2):337–42.
Hoe CYW, Ahmad B, Watterson J. The use of videos for diabetes patient education: a systematic review. Diabetes Metab Res Rev. 2024;40(2):3722.
Nkhoma DE, Soko CJ, Bowrin P, Manga YB, Greenfield D, Househ M, et al. Digital interventions self-management education for type 1 and 2 diabetes: a systematic review and meta-analysis. Comput Methods Programs Biomed. 2021;210: 106370.
Yoshida Y, Boren SA, Soares J, Popescu M, Nielson SD, Simoes EJ. Effect of health information technologies on glycemic control among patients with type 2 diabetes. Curr Diabetes Rep. 2018;18(12):130.
Lee PA, Greenfield G, Pappas Y. The impact of telehealth remote patient monitoring on glycemic control in type 2 diabetes: a systematic review and meta-analysis of systematic reviews of randomised controlled trials. BMC Health Serv Res. 2018;18(1):495.
Bassi G, Mancinelli E, Dell’Arciprete G, Rizzi S, Gabrielli S, Salcuni S. Efficacy of eHealth interventions for adults with diabetes: a systematic review and meta-analysis. Int J Environ Res Public Health. 2021;18(17):8982.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. Declaración PRISMA 2020: una guía actualizada para la publicación de revisiones sistemáticas. Rev Esp Cardiol. 2021;74(9):790–9.
Faruque LI, Wiebe N, Ehteshami-Afshar A, Liu Y, Dianati-Maleki N, Hemmelgarn BR, et al. Effect of telemedicine on glycated hemoglobin in diabetes: a systematic review and meta-analysis of randomized trials. Can Med Assoc J. 2017;189(9):E341–64.
Kolb L. An effective model of diabetes care and education: the ADCES7 self-care behaviors™. Sci Diabetes Self-Manag Care. 2021;47(1):30–53.
Holland-Carter L, Tuerk PW, Wadden TA, Fujioka KN, Becker LE, Miller-Kovach K, et al. Impact on psychosocial outcomes of a nationally available weight management program tailored for individuals with type 2 diabetes: results of a randomized controlled trial. J Diabetes Complicat. 2017;31(5):891–7.
Ildarabadi EH, Tabei MG, Mosaferi KA. Effects of face-to-face and online training on self-care of middle-aged and elderly people with type 2 diabetes: a comparative study. Open Access Maced J Med Sci. 2019;7(7):1214–9.
Avdal EU, Uran BNÖ, Pamuk G, Yildirim JG, Konakçi G, Ateş M, et al. Investigation of the effect of web-based diabetes education on metabolic parameters in people with type 2 diabetes: a randomized controlled trial. J Infect Public Health. 2020;13(12):1892–8.
Molavynejad S, Miladinia M, Jahangiri M. A randomized trial of comparing video telecare education vs in-person education on dietary regimen compliance in patients with type 2 diabetes mellitus: a support for clinical telehealth providers. BMC Endocr Disord. 2022;22(1):116.
Pacaud D, Kelley H, Downey AM, Chiasson M. Successful delivery of diabetes self-care education and follow-up through eHealth media. Can J Diabetes. 2012;36(5):257–62.
Orsama AL, Lähteenmäki J, Harno K, Kulju M, Wintergerst E, Schachner H, et al. Active assistance technology reduces glycosylated hemoglobin and weight in individuals with type 2 diabetes: results of a theory-based randomized trial. Diabetes Technol Ther. 2013;15(8):662–9.
Greenwood DA, Hankins AI, Parise CA, Spier V, Olveda J, Buss KA. A comparison of in-person, telephone, and secure messaging for type 2 diabetes self-management support. Diabetes Educ. 2014;40(4):516–25.
O’Neil PM, Miller-Kovach K, Tuerk PW, Becker LE, Wadden TA, Fujioka K, et al. Randomized controlled trial of a nationally available weight control program tailored for adults with type 2 diabetes. Obesity. 2016;24(11):2269–77.
Han Y, Ye X, Li X, Yang P, Wu Y, Chen L, et al. Comparison of an online versus conventional multidisciplinary collaborative weight loss programme in type 2 diabetes mellitus: a randomized controlled trial. Int J Nurs Pract. 2023;29(1): 13126.
Mitchell SE, Bragg A, De La Cruz BA, Winter MR, Reichert MJ, Laird LD, et al. Effectiveness of an immersive telemedicine platform for delivering diabetes medical group visits for African American, Black and Hispanic, or Latina women with uncontrolled diabetes: the women in control 2.0 noninferiority randomized clinical trial. J Med Internet Res. 2023;25: e43669.
Pais V, Patel BP, Ghayoori S, Hamilton JK. “Counting carbs to be in charge”: A comparison of an Internet-based education module with in-class education in adolescents with type 1 diabetes. Clin Diabetes. 2021;39(1):80–7.
McGill DE, Laffel LM, Volkening LK, Butler DA, Levy WL, Wasserman RM, et al. Text message intervention for teens with type 1 diabetes preserves HbA1c: results of a randomized controlled trial. Diabetes Technol Ther. 2020;22(5):374–82.
Ayar D, Öztürk C, Grey M. The effect of web-based diabetes education on the metabolic control, self-efficacy and quality of life of adolescents with type 1 diabetes mellitus in Turkey. J Pediatr Res. 2021;8(2):131–8.
Alharthi S, Alrajeh A, Alyusuf E, Alguwaihes AM, Jammah A, Al-Sofiani ME. “Pre-Ramadan” telemedicine: effect on fasting experience and glycemic control during Ramadan in people with type 1 diabetes. Diabetes Metab Syndr. 2022;16(8): 102567.
Rossi MC, Nicolucci A, Lucisano G, Pellegrini F, Di Bartolo P, Miselli V, et al. Impact of the “Diabetes interactive diary” telemedicine system on metabolic control, risk of hypoglycemia, and quality of life: a randomized clinical trial in type 1 diabetes. Diabetes Technol Ther. 2013;15(8):670–9.
Rossi MCE, Nicolucci A, Di Bartolo P, Bruttomesso D, Girelli A, Ampudia FJ, et al. Diabetes interactive diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life. Diabetes Care. 2010;33(1):109–15.
Paxton R (2021) School diabetes education: the benefits of a virtual package during the COVID-19 pandemic. J Diabetes Nurs 25(3):195
Moattari M, Hashemi M, Dabbaghmanesh MH. The impact of electronic education on metabolic control indicators in patients with diabetes who need insulin: a randomised clinical control trial. J Clin Nurs. 2013;22(1–2):32–8.
Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care. 2003;26(4):1002–7.
Kearns JW, Bowerman D, Kemmis K, Izquierdo RE, Wade M, Weinstock RS. Group diabetes education administered through telemedicine: tools used and lessons learned. Telemed e-Health. 2012;18(5):347–53.
Izquierdo V, Pazos-Couselo M, González-Rodríguez M, Rodríguez-González R. Educational programs in type 2 diabetes designed for community-dwelling older adults: a systematic review. Geriatr Nurs (Minneap). 2022;46:157–65.
Gupta U, Gupta Y, Jose D, Mani K, Jyotsna VP, Sharma G, et al. Effectiveness of a video-based lifestyle education program compared to usual care in improving HbA1c and other metabolic parameters in individuals with type 2 diabetes: an open-label parallel arm randomized control trial (RCT). Diabetes Therapy. 2020;11(3):667–79.
Azar M, Gabbay R. Web-based management of diabetes through glucose uploads: has the time come for telemedicine? Diabetes Res Clin Pract. 2009;83(1):9–17.
Turnin MC, Gourdy P, Martini J, Buisson JC, Chauchard MC, Delaunay J, et al. Impact of a remote monitoring programme including lifestyle education software in type 2 diabetes: results of the Educ@dom randomised multicentre study. Diabetes Therapy. 2021;12(7):2059–75.
Lameijer A, Lommerde N, Dunn TC, Fokkert MJ, Edens MA, Kao K, et al. Flash Glucose Monitoring in the Netherlands: increased monitoring frequency is associated with improvement of glycemic parameters. Diabetes Res Clin Pract. 2021;177: 108897.
Petrovski G, Zivkovic M, Stratrova SS. Social media and diabetes: can facebook and skype improve glucose control in patients with type 1 diabetes on pump therapy? One-year experience. Diabetes Care. 2015;38(4):e51–2.
Hosseinzadeh M, Sharifzadeh G, Hosseinzadeh M, Torshizi M. Comparison of the effect of face-to-face and social media-based training on the self-care of women with gestational diabetes mellitus (GDM) in Birjand. Modern Care J. 2022;19(2): 119456.
Brown SJ, Lieberman DA, Gemeny BA, Fan YC, Wilson DM, Pasta DJ. Educational video game for juvenile diabetes: results of a controlled trial. Med Inform. 1997;22(1):77–89.
Li J, Huang J, Zheng L, Li X. Application of artificial intelligence in diabetes education and management: present status and promising prospect. Front Public Health. 2020;29:8.
Hussein SZ, Hong Chuo C, Mohd Said F, Tumingan K, Sahar Shah N, Abu Bakar SH. The best online tools based on media preference reflected by health information received on social media amongst diabetic patients in Hospital Canselor Tuanku Muhriz, Kuala Lumpur Malaysia. Malay J Med Sci. 2021;28(3):118–28.
Hollander P, Gupta AK, Plodkowski R, Greenway F, Bays H, Burns C, et al. Effects of naltrexone sustained-release/bupropion sustained-release combination therapy on body weight and glycemic parameters in overweight and obese patients with type 2 diabetes. Diabetes Care. 2013;36(12):4022–9.
Ali MK, Bullard KM, Saaddine JB, Cowie CC, Imperatore G, Gregg EW. Achievement of goals in US diabetes care, 1999–2010. N Engl J Med. 2013;368(17):1613–24.
Hall J, Skinner F, Tilley P, MacRury S. Service user preferences for diabetes education in remote and rural areas of the Highlands and Islands of Scotland. Rural Remote Health. 2018;18:1–12.
Chérrez-Ojeda I, Vanegas E, Calero E, Plaza K, Cano JA, Calderon JC, et al. What kind of information and communication technologies do patients with type 2 diabetes mellitus prefer? An Ecuadorian cross-sectional study. Int J Telemed Appl. 2018;2018:1–8.
Litchman ML, Rothwell E, Edelman LS. The diabetes online community: older adults supporting self-care through peer health. Patient Educ Couns. 2018;101(3):518–23.
Cunningham SG, Stoddart A, Wild SH, Conway NJ, Gray AM, Wake DJ. Cost-utility of an online education platform and diabetes personal health record: analysis over ten years. J Diabetes Sci Technol. 2023;17(3):715–26.
Mounié M, Costa N, Gourdy P, Latorre C, Schirr-Bonnans S, Lagarrigue JM, et al. Cost-effectiveness evaluation of a remote monitoring programme including lifestyle education software in type 2 diabetes: results of the Educ@dom study. Diabetes Therapy. 2022;13(4):693–708.
Biermann E, Dietrich W, Rihl J, Standl E. Are there time and cost savings by using telemanagement for patients on intensified insulin therapy? Comput Methods Programs Biomed. 2002;69(2):137–46.
Bisno DI, Reid MW, Pyatak EA, Flores Garcia J, Salcedo-Rodriguez E, Torres Sanchez A, et al. Virtual peer groups reduce HbA1c and increase continuous glucose monitor use in adolescents and young adults with type 1 diabetes. Diabetes Technol Ther. 2023;25(9):589–601.
Trento M, Passera P, Borgo E, Tomalino M, Bajardi M, Brescianini A, et al. A 3-year prospective randomized controlled clinical trial of group care in type 1 diabetes. Nutr Metab Cardiovasc Dis. 2005;15(4):293–301.
Housden L, Wong ST, Dawes M. Effectiveness of group medical visits for improving diabetes care: a systematic review and meta-analysis. Can Med Assoc J. 2013;185(13):E635–44.
Franco L, Bozzetto L, De Angelis R, Calabrese I, Cavagnuolo L, Gasparro T, et al. Beneficial effects on body weight of group vs individual care in adults with type 1 diabetes on advanced technologies. Health Sci Rep. 2021;4(4): e385.
Årsand E, Bradway M, Gabarron E. What are diabetes patients versus health care personnel discussing on social media? J Diabetes Sci Technol. 2019;13(2):198–205.
Brady E, Segar J, Sanders C. Accessing support and empowerment online: the experiences of individuals with diabetes. Health Expect. 2017;20(5):1088–95.
https://commission.europa.eu/law/law-topic/data-protection/data-protection-eu_es.
Schultz M. Telehealth and remote patient monitoring innovations in nursing practice: state of the science. OJIN: Online J Issues Nurs. 2023. https://doi.org/10.3912/ojin.vol28no02st01.
Frielitz F, Storm N, Hiort O, Katalinic A, von Sengbusch S. Die Erstellung eines Datenschutzkonzeptes: eine Anleitung für telemedizinische Versorgungsprojekte. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2019;62(4):479–85.
Funding
This research was supported by a grant from Fundació Docència i Recerca Mútua Terrassa, specifically the ‘Beca d’Intensificació FMT per a Infermeria de MT 2022’ (halving working hours for research). No funding or sponsorship was received for the publication of this article.
Author information
Authors and Affiliations
Contributions
Núria Alonso-Carril: conceptualization, methodology, analysis, writing original draft and review; Verónica Perea: methodology, analysis, writing review and editing. Silvia Rodríguez, Carmen Quirós, Belen Berrocal, AJ Amor: writing review and editing; Maria-José Barahona, Davinia Martinez and Carme Ferré: supervision. Each of the named authors reviewed and critically appraised the manuscript during development and approved the final version for publication.
Corresponding author
Ethics declarations
Conflict of Interest
Núria Alonso-Carril, Silvia Rodríguez-Rodríguez, Carmen Quirós, Belén Berrocal, Maria-José Barahona, Davinia Martínez, Carme Ferré and Verónica Perea have nothing to disclose. Antonio J. Amor is an Editorial Board member of Diabetes Therapy. Antonio J. Amor was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Alonso-Carril, N., Rodriguez-Rodríguez, S., Quirós, C. et al. Could Online Education Replace Face-to-Face Education in Diabetes? A Systematic Review. Diabetes Ther 15, 1513–1524 (2024). https://doi.org/10.1007/s13300-024-01595-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-024-01595-6