Abstract
It is a well-evidenced fact that diet significantly impacts type 2 diabetes mellitus (T2DM) prevention and management. However, dietary responses vary among different populations, necessitating personalized recommendations. Substantial evidence supports the role of diet in T2DM remission, particularly low-energy or low-carbohydrate diets that facilitate weight loss, enhance glycemic control, and achieve remission. This review aims to comprehensively analyze and compare personalized nutritional interventions with non-personalized approaches in T2DM remission. We conducted a literature search using the Academy of Nutrition and Dietetics guidelines, focusing on clinical and observational trials published within the past decade. We present the strengths and drawbacks of incorporating personalized nutrition into practice, along with the areas for research in implementing personalized interventions, such as cost-effectiveness and accessibility. The findings reveal consistently higher diabetes remission rates in personalized nutrition studies compared to non-personalized interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Our review is focused on two dietary approaches: personalized nutrition interventions and non-personalized nutritional interventions. These strategies vary globally in the methods used to achieve T2DM remission. |
A global perspective is seen in the diverse dietary therapies for T2DM remission. Articles from Europe, North America, Asia, and Africa collectively emphasize the worldwide relevance of these interventions. |
Personalized interventions show high remission rates, often outperforming non-personalized approaches. They include precision nutrition based on postprandial glucose responses, diabetes subtype-tailored diets, and individualized meal plans. |
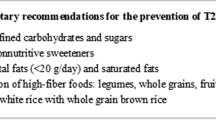
Non-personalized interventions offer general dietary recommendations. These encompass low-carb Mediterranean diets, calorie-restriction diets, and meal replacements. |
Studies demonstrate substantial improvements in HbA1c levels, weight loss, and body fat reduction. Even those not experiencing significant weight loss, see improved HbA1c levels. Personalized dietary interventions based on glycemic responses and diabetes subtypes positively affect body composition and glycemic control. Each approach offers distinct advantages for patients. |
Introduction
Diabetes mellitus (DM), a group of metabolic disorders characterized by elevated blood sugar levels, represents a global health concern. Among its various forms, type 2 diabetes mellitus (T2DM) is the most prevalent, accounting for approximately 90% of cases [1]. T2DM is closely associated with overweight, obesity, and an increased percentage of body fat in the abdominal region [2]. Numerous dietary interventions have been developed to address these issues, and it has become evident that these interventions can also be targeted toward achieving diabetes remission [3].
The concept of “diabetes remission” has evolved since its initial introduction by the American Diabetes Association (ADA) in 2009 [4]. The original definition required normalization of glucose without the use of medications or surgery. In 2021, the ADA refined this concept, using “remission” to describe achieving blood glucose levels below the diagnostic threshold either spontaneously or after medical interventions, including the discontinuation of glucose-lowering drugs. Although the 2021 criteria have become the standard [5], the ADA’s 2009 proposal remains the most commonly used.
Various dietary strategies have been employed to achieve remission, with recent approaches incorporating personalized or precision nutrition. Precision nutrition encompasses multiple synergistic approaches and omics sciences, including dietary habits, health status, food environment, environmental exposures, physical activity, socioeconomic factors, psychosocial characteristics, genomics, microbiomics, and metabolomics [6]. It has the potential to deliver nutrients, foods, or diets to individuals who stand to benefit the most while minimizing potential harm [7].
While there is still no universally accepted definition for personalized nutrition, it can be described as an approach that tailors specific nutritional advice, products, or services based on individual characteristics [8]. Although “personalized nutrition” and “precision nutrition” are sometimes used interchangeably, the latter is more suitable for describing nutritional approaches grounded in biological, environmental, and social factors, which can be applied to individuals or groups with similar characteristics [9].
Studies investigating the variability of individual post-meal responses revealed that differences in microbiota, lifestyle, demographics, and genetic factors collectively contribute to the observed diversity in how individuals’ bodies respond after consuming a meal [10, 11]. While several reviews have examined personalized and precision nutrition in diabetes [12,13,14], none have specifically examined its impact on the remission of T2DM.
The most common non-personalized interventions include Mediterranean dietary patterns, low-carbohydrate diets, very-low-calorie restriction (VLCR) diets, and replacement food diets, or a combination of these. The Mediterranean diet includes a high intake of plant foods, minimally processed and locally grown items, limited consumption of sweets, frequent use of olive oil as the main fat source, moderate dairy and egg intake, low to moderate consumption of fish and poultry, minimal red meat consumption, and moderate wine consumption with meals, setting it apart from other healthy diet patterns [15]. A low-carbohydrate diet is characterized by a reduction in carbohydrate intake to under 130 g per day with different levels of calorie restriction [16]. Low-calorie diets typically offer an energy intake ranging from 800 to 1200 kcal/day, which can be achieved through complete dietary replacement (TDR) or a partial replacement involving traditional foods [17]; this dietary approach includes a diet replacement with low-energy or other diet meal replacement product.
This narrative review includes personalized nutrition and precision nutrition interventions, as well as other non-personalized nutritional therapies such as low-carb diets and meal replacement therapies. It aims to provide a comprehensive overview of these interventions, discussing their proven benefits on diabetes remission and the limitations of each nutritional and lifestyle approach.
Methodology
We conducted a concise review using a systematic search approach to ensure the inclusion of the most relevant studies [18]. Our methodology involved (1) formulating a PICO (Population, Intervention, Comparison, and Outcome) research question; (2) implementing a systematic search process; (3) extracting and synthesizing the data; and (4) analyzing key findings.
Search Process
This study commenced with an exhaustive search of the existing literature aimed at incorporating and interpreting results from diverse study types, populations, and interventions. We searched several electronic databases, including the Virtual Health Library (VHL), Epistemonikos, PUBMED, SciELO, and Google Scholar, from April 1, 2023 to October 30, 2023. The search strings, constructed with Boolean operators, incorporated Medical Subject Heading (MeSH) terms and were based on defined eligibility criteria (see Table 1). These criteria included mentions of T2DM remission, personalized nutrition, diet, physical activity, and exercise in the title, abstract, or full text of the articles. Ethical approval was not required since the study design is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data extraction, Synthesis, and Analysis
Data extraction involved collecting and recording study details (title, author, publication date, study type, follow-up duration), population (subjects, sample size), intervention specifics (diet type, intervention duration, adherence assessment methods), health outcomes (diabetes remission definition), and study limitations.
Each author then conducted two separate rounds of reviews, recording their selection in a shared table. In the first round of review, authors worked independently to choose articles on the basis of their titles, ensuring relevance to the research question and MeSH terms. Subsequently, authors jointly assessed the articles selected for the second review, involving abstract examination and alignment with inclusion and exclusion criteria, determining the articles for inclusion in this review. When discrepancies arose, reviewers discussed their perspectives and sought consensus by jointly reviewing the articles in question to ensure reliability, objectivity, and consistency in our review study selection (Fig. 1).
In the category of personalized nutrition studies, we included those that not only specified their intervention as personalized nutrition but also employed a specific and tailored approach considering different characteristics such as diabetes subtype or with a focus on the postprandial period for glycemic control. Additionally, these studies took into account unique individual characteristics such as age, sex, and goals for metabolic parameters, instead of following a generic plan or a one-size-fits-all approach for all participants.
Results
We initially identified 102 articles, included 29 articles after the initial screening, and assessed a total of 14 for eligibility. After excluding two duplicate studies, we examined a total of 14 articles. A little over half (seven) were conducted in Europe, three each in North America and Asia, and one each in the Middle East and Africa.
We categorized the studies into two main approaches: (1) personalized nutrition interventions and (2) non-personalized nutritional interventions or dietary recommendations and lifestyle changes. Within these studies’ nutritional interventions, three main dietary patterns emerged: the Mediterranean diet, carbohydrate restriction diet, and low- and very-low-calorie diets. Studies employing this type of intervention demonstrated significant potential for weight loss and T2DM remission.
High rates of T2DM remission were observed in personalized dietary interventions. We noted that the methods for customizing the diets varied among the studies. For instance, one study delivered a precision nutrition intervention [19] based on participants’ postprandial glucose responses measured through continuous glucose monitoring (a personalized postprandial-targeting [PPT] diet). Another study personalized the diet on the basis of diabetes subtypes [20], while another developed individual dietary plan including calorie restriction and specific exercise prescriptions intending to achieve a BMI ≤ 25 [21]. Yet another study reported using a personalized dietary intervention, but did not describe how it was personalized nor the participants’ characteristics. The study did, however, describe using a stepwise approach to counseling and providing personalized, individualized, and tailored meal plans [22].
Personalized Nutrition
Personalized nutrition studies achieved high remission rates, sometimes superior to non-personalized intervention studies. For instance, a study by Rein et al. used Zeevi et al.’s machine learning algorithm for predicting postprandial glucose responses (PPGR) in individuals with T2DM [10, 19]. In this study’s crossover design, participants received both algorithm-personalized interventions and a non-personalized Mediterranean diet for 2 weeks. Upon comparison, the personalized diets tailored to glycemic responses outperformed the Mediterranean diet. The average PPGR across all meals was significantly lower during the personalized intervention, ultimately resulting in a remarkable improvement in glycemic control and diabetes remission for over 50% of the participants, even though the personalized diets were high in fat compared to the Mediterranean diet (51% vs. 29% of calories from fat, respectively) [19].
In a study by de Hoogh et al., 75% of the participants in the personalized intervention group experienced remission at 13 weeks, compared to only 22% of their usual care group peers [20]. In this study, seven subtypes of diabetes were identified on the basis of their beta cell function and the presence of hepatic and/or muscle insulin resistance: (1) reduced beta cell function (PB), (2) hepatic insulin resistance (HIR), (3) muscle insulin resistance (MIR), (4) a combination of muscle and liver IR (CIR), (5) PB and HIR, (6) PB and MIR, and (7) PB and CIR [20]. The classification of subgroups was based on clinical and biochemical data, utilizing glucose and insulin responses to the oral glucose test (OGTT) to calculate indices such as disposition index, Matsuda index, hepatic insulin resistance index, and muscle insulin sensitivity index. Subsequently, participants were assigned to seven subtypes according to beta cell function and the presence of hepatic and/or muscular insulin resistance. At the study’s outset, there were no participants with a heathy, MIR, or PB-MIR subtype. A substantial redistribution of participants among subtypes was observed after 13 weeks of intervention.
The HIR and CIR subgroups initially followed a very-low-calorie diet for 1 week, followed by a 12-week low-calorie diet; the PB, PB-HIR, and PB-CIR groups engaged in 13 weeks of low-calorie dieting; and finally, the MIR and PB-MIR groups followed a normal isocaloric diet. In addition to dietary changes, some groups exercised according to Dutch guidelines and under the supervision of a physiotherapist [20]. HIR, PB, and PB-HIR groups were encouraged to do moderate exercise (60 min/day). The CIR and PB-CIR subgroups engaged in physical activity for 1 week followed by 12 weeks of 180 min of strength and endurance training. The MIR and PB-MIR subgroups underwent 13 weeks of strength and endurance training. After the 13-week intervention, all patients returned to standard primary care. Remission was maintained in 29% of the participants in the personalized intervention group after 2 years, although unfortunately there was no control group to compare against.
Weight loss was a significant factor in achieving remission in the de Hoogh et al. study. In the intervention group, patients who achieved remission lost 10.7 kg compared to 4.6 kg in those who did not (p < 0.001). The CIR subgroup experienced a significantly greater weight loss (− 13.1, p < 0.001) compared to the other diabetes subtypes. The PB-HIR subgroup responded best to the personalized intervention in terms of fasting glucose and HbA1c levels, showing a decrease of − 1.1 mmol/L and − 6.2 mmol/mol, respectively, compared to the other groups (p < 0.001) [20]. The most notable trend was observed in the HIR subtype, with 55% of participants transitioning to a heathy subtype after the intervention. Of the participants who ended with a healthy subtype, 36.8% achieved diabetes remission, making it the subgroup with the highest remission rate.
In another study by Roncero-Ramos et al., patients were classified according to their HIR fasting and beta cell functionality, measured as the disposition index (DI) at baseline. Individuals with low HIR fasting or high DI had a higher likelihood of achieving diabetes remission compared to those with high HIR fasting or low DI (HR 1.7 and 2.6, respectively) [23]. This remission was achieved through a personalized dietary intervention without pharmacological treatment and without weight loss.
The combination of low HIR fasting and high DI presented the highest probability of remission (HR 4.6, 95% CI 2.0–10.7). Participants in this study were randomly assigned to receive one of two diets: a Mediterranean diet or a low-fat diet. To further distribute participants, they were divided into eight groups based on sex, age, and history of previous myocardial infarction. These groups were then assigned to different diets using block randomization [23]. In comparison to the high HIR fasting patients (the reference group), the low HIR fasting patients showed a 2.3-fold higher likelihood of achieving T2DM remission. After adjustment for all potential confounding variables, a Cox model demonstrated that low HIR fasting patients had a 1.8-fold higher probability of remission (HR 1.7, 95% CI 1.0–3.0) [23].
Patients with T2DM in the de Hoogh, Rein, and Dave studies observed improvements in HbA1c levels, weight loss, and reductions in body fat [19, 20, 22]. Even those who did not experience weight loss reported healthier HbA1c levels (Roncero-Ramos I) (Ried-Larsen M), resulting in post-intervention remission rates of over 20%. These findings suggest that personalized dietary interventions and food choices based on glycemic responses and diabetes subtypes can positively influence body composition and glycemic control. Consequently, it can be inferred that the effectiveness of such interventions is contingent on reducing body weight and enhancing insulin sensitivity [21, 23].
We only found one study [19] that incorporated the use of omics sciences by integrating participants from a previous study [10]. Precision nutrition, supported by omics sciences, presents significant advantages in diabetes remission. By utilizing genomics, transcriptomics, and metabolomics, it allows for a profound understanding of individual responses to dietary interventions. This enables a more precise customization of nutritional recommendations, taking into account genetic variations, gene expression, and the unique metabolic profiles of each individual. This approach not only enhances the effectiveness of nutritional interventions but is also crucial for improving patient adherence to treatment plans, indicating a promising avenue for future research.
Non-personalized Nutrition
One study (Esposito et al.) tested the potential for a low-carbohydrate Mediterranean diet to prevent the need for drug therapy in people with T2DM [24]. The study found that participants following this diet had a greater likelihood of achieving remission, with a prevalence of 15% within the first year, in contrast to 4% in the low-fat diet group. Another study (Gardner et al.) tested a low-carbohydrate ketogenic diet against the Mediterranean diet and demonstrated improvements in HbA1c levels and blood sugar control among individuals with prediabetes and T2DM [25]. These findings highlight the potential of these dietary strategies in T2DM management [24, 25].
Simplifying carbohydrate reduction in daily life in newly diagnosed and pre-existing T2DM, rather than complex counting, can lead to drug-free T2DM remission. Unwin et al. studied this approach, achieving a 46% remission rate in patients with T2DM within 12 months [26]. They focused on educating patients about the physiological principles of glucose and insulin responses to various foods, emphasizing the importance of starchy carbohydrates, glycemic index (GI), and glycemic load [26].
In a separate study, Durrer et al. explored the role of pharmacists within healthcare teams in facilitating better dietary adherence among patients with T2DM [27]. Their low-carbohydrate energy-restricted diets, led by community pharmacists, significantly improved HbA1c levels, weight, lipid profiles, and blood pressure while reducing the need for glucose-lowering medications. Notably, the low-carbohydrate (< 50 g), energy-restricted diet approach led to a substantial reduction in medication use, with 35.7% of participants discontinuing all glucose-lowering medications at 12 weeks. This suggests that a low-carbohydrate diet can be a practical therapeutic option for patients with prediabetes or newly diagnosed with T2DM who wish to avoid medication [27].
Calorie-restriction-based interventions, including those with meal replacements, offer a non-personalized alternative and have demonstrated the feasibility of achieving diabetes remission, with success rates ranging from 40% to 87% [28]. Most studies in this category involved discontinuing antidiabetic medication at the start of the intervention; instead, they typically implemented an initial phase of calorie restriction, either very-low-calorie (VLCR, < 800 kcal) or low-calorie (LCR, 800–1200 kcal/day), within an intervention period ranging from 9 days to 3 months. This is followed by diet reintroduction and a subsequent follow-up period that includes support for physical activity and behavioral adjustments to maintain adherence [29]. A common outcome observed in all these studies is a significant improvement in weight, accompanied by corresponding changes in BMI.
Two studies highlight the effectiveness of intensive weight management in achieving T2DM remission. In a study conducted by Steven et al., 30 individuals with T2DM received structured weight maintenance support while following a very-low-calorie diet (VLCD) for 8 weeks and then gradually transitioning to an isocaloric diet [28]. Notably, 40% of the participants reached T2DM remission, defined as achieving fasting blood glucose levels below 7 mmol/L after the VLCD [28]. Another study—the DiRECT trial—focused on intensive weight management using a cluster-randomized study design [30]. The intervention included complete diet replacement and structured weight loss support, leading to significant results; 46% of participants in the intervention group achieved remission at 12 months, compared to only 4% of the control group [30].
A study led by Bynoe et al. assessed the feasibility of a short-term, low-calorie diet for individuals with recently diagnosed T2DM in Barbados, involving 25 participants whose hypoglycemic medication was discontinued upon initiating an 8-week liquid diet [31]. Remarkably, 40% of these participants achieved remission from T2DM in response to the dietary intervention, highlighting the potential effectiveness of short-term, low-calorie diets as a strategy to induce T2DM remission in newly diagnosed individuals [31].
The DIADEM-I study, a trial of an intensive lifestyle intervention, addressed weight loss through two phases. In the first phase, known as the “total diet replacement phase,” participants received low-calorie diet meal replacement products to significantly reduce their calorie intake [32]. In the subsequent phase, the “weight-loss maintenance phase”, foods were gradually introduced and physical activity was increased. Diabetes remission was achieved by 61% of the intervention group in comparison to only 12% in the control group [32]. A study by Wei et al.—investigating the effects of a VLCR diet on individuals with T2DM—found similar results [29]. In the study, 39% of participants achieved long-term T2DM remission with a median duration of 7.8 years following the VLCR intervention. These findings highlight the potential of VLCR in the long term in achieving remission [29].
The reduction of HbA1c, a key indicator of glycemic control, was observed in several dietary interventions aimed at managing T2DM. Esposito et al. reported that the low-carbohydrate Mediterranean diet led to a significant decrease in HbA1c (− 0.5% [p < 0.001]) compared to a low-fat diet [24]. Gardner’s study, which compared the low-carbohydrate ketogenic diet (WFKD) and the Mediterranean diet, found both diets resulted in reduced HbA1c levels, with no statistically significant difference between them (WFKD, − 9%, Med-Plus, − 7%). However, the WFKD showed a more substantial decrease in triglycerides and a rise in LDL cholesterol concentrations compared to the low-carb Mediterranean diet [25].
Unwin et al. reinforced the potential of a lower carbohydrate diet, finding significant weight loss in 94% of patients with T2DM and a remarkable drop in HbA1c levels (from a median of 66 to 48 mmol/mol [p < 0.001]) [26]. In the same vein, Durrer et al. reported that 17% of a low-carbohydrate energy-restricted group achieved an HbA1c of < 6.5%, reducing the need for glucose-lowering medications through complete discontinuation of medications [27].
The VLCD intervention by Steven et al. showed substantial improvements in fasting blood glucose levels (− 2.2 mmol/L at 8 weeks and − 1.7 mmol/L at 8 months), insulin sensitivity, and hepatic and pancreatic fat content. This intervention underscores the durable effects of a VLCD in managing T2DM [28]. Bynoe et al. reported a significant reduction of 2.2 mmol/L in fasting plasma glucose levels after an 8-week low-calorie liquid diet, with levels remaining 1.7 mmol/L lower after 8 months [31]. Collectively, these findings emphasize the potential of various dietary approaches to effectively reduce HbA1c levels and improve glycemic control in individuals with T2DM, with each approach offering unique advantages for patients.
In the DiRECT trial, nearly a quarter of the intervention group (24%) successfully achieved substantial weight loss of 15 kg or more. These findings illustrate the feasibility of primary-care-driven T2DM remission and highlight the improvements in participants’ quality of life [30]. Similarly, Bynoe’s study, focusing on a predominantly Black population in Barbados, revealed that participants on a short-term, low-calorie diet achieved significant mean weight loss. Participants lost a mean of 10.1 kg after 8 weeks and maintained the loss at 8.2 kg after 8 months. Notably, over 80% of those who lost more than 10 kg attained fasting plasma glucose levels below 7 mmol/L, underscoring the potential of such interventions for weight loss and diabetes remission. These interventions, of course, face challenges related to cultural food preferences and societal pressures [31]. Participants in the DIADEM-I trial experienced an average weight loss of 12 kg after a low-calorie diet with meal replacement products and intensive lifestyle intervention, while the control group lost only 4 kg [32].
While statistical significance varied across studies, both LCD and VLCD have shown the potential to improve lipid profiles, including elevating HDL levels and reducing non-HDL cholesterol and triglycerides [28, 31, 32]. In Gardner et al.’s study, participants eating a low-carbohydrate ketogenic diet (WFKD) or a modified Mediterranean diet (Med-Plus) exhibited significant reductions in HbA1c levels. Importantly, the WFKD led to a significantly greater reduction in triglycerides compared to the Mediterranean diet (p = 0.02). Additionally, there was a significant increase in LDL cholesterol concentrations in the low-carbohydrate ketogenic diet group compared to a decrease in the Mediterranean diet group (p = 0.01) [25]. These findings underscore the impact of dietary choices on the lipid profiles of individuals with prediabetes and T2DM.
Discussion
This mini-review set out to explore the effect of different diet interventions on T2DM management and whether any of these could effectively achieve ADA-defined diabetes remission [4].
Personalized nutrition has demonstrated superior outcomes compared to the Mediterranean diet, achieving 61% diabetes remission in high-fat personalized diets, even though the Mediterranean diet has better adherence and sustainability. Low-carb restriction and energy-restricted diets effectively manage T2DM, improving lipid profiles, body weight, waist circumference, HbA1c, and blood pressure and reducing medication reliance. While personalized diet studies did not report these results, we believe they are not excluded from these benefits.
As a result of varying reporting methods, weight loss achievements were not able to be compared across studies. However, it was clear that intervention groups consistently achieved more substantial weight loss than the comparison groups. While this may represent a connection between weight loss and T2DM remission, our study does not explore this relationship and thus we do not report on it here. In addition to weight loss, as observed in most of the reviewed studies, which was seen independently of the type of intervention, predictors of response correlating with remission have been identified. One such predictor is the duration of the disease, with early diagnosis of diabetes associated with higher remission chances, as highlighted in various studies [19, 20, 22,23,24, 29, 32]. These studies emphasize that individuals newly diagnosed with diabetes have a better chance of achieving remission, as well as higher fasting glucose levels and acute insulin response in OGTT, which may indicate a better-preserved glucose metabolism at the time of intervention [29].
Interventions for T2DM can vary in duration, with short-term interventions primarily focusing on fast glycemic control, while longer-term interventions focus on improving adherence and achieving remission, with early diagnosis enhancing remission prospects.
Adherence remains a critical and challenging factor in the success of personalized diets, low-carbohydrate diets, and energy-restricted diets for managing and potentially reversing T2DM, especially over the long term. This challenge arises from the complexities of sustaining specific dietary patterns and the technological difficulties involved in evaluating these personalized regimens [33]. These studies underscore the complexity of T2DM and the significance of personalized lifestyle interventions in managing and achieving disease remission.
Each study reports adherence to nutritional intervention differently. Furthermore, the duration of remission may vary, and maintaining it over the long term may necessitate continuous follow-up and individualized care. These findings underscore the effectiveness of a personalized approach that extends beyond weight loss, addressing factors such as glycemic control, physical fitness, and economic aspects in achieving T2DM remission. The research published by de Hoogh et al. revealed a 75% remission rate in the personalized intervention group (personalized by diabetes subtype) at 13 weeks, although it decreased to 28.6% at 104 weeks, emphasizing the challenge of sustaining long-term remission [20]. Patient perception and social networks significantly influence adherence, and strategies such as education, support, motivation, and addressing individual challenges can improve adherence in diabetes management and remission efforts.
The non-personalized interventions were based on general recommendations, such as the studies by Unwin et al. and Durrer et al., which centered on reducing dietary carbohydrates [26, 27]. Their approach led to diabetes remission through improvements in HbA1c values and a reduction in the consumption of hypoglycemic medications. Similarly, low-calorie interventions and meal replacements were found to be effective strategies for achieving diabetes remission in newly diagnosed patients with T2DM, as seen in the study by Wei et al. [29, 32]. However, it is essential to acknowledge some limitations. The observed results were primarily seen in the younger population with recent T2DM diagnoses [29, 32], and not all participants achieved remission, because of the variability in individual responses to these non-personalized interventions. Additionally, long-term adherence remains a subject for further investigation, and it is essential to consider the potential challenges associated with cultural food preferences [31].
Personalized diets offer the advantage of achieving significantly higher remission rates in patients with T2DM. By tailoring dietary guidelines to individuals’ glycemic responses and diabetes subtypes, these interventions demonstrate greater efficacy in blood glucose control and disease remission. Precision medicine can potentially address this enormous problem by accounting for heterogeneity in the etiology, clinical presentation, and pathogenesis of common forms of diabetes and the risks of complications. However, there are challenges associated with personalized diets. Variability in the methods used in studies makes it difficult to compare results and draw general conclusions directly.
Long-term remission sustainability can be an obstacle, as a decrease in remission rates has been observed in some cases after a certain period. Adherence to specific dietary guidelines can be problematic for some patients, and the cost of customizing diets may be a limiting factor for widespread implementation. Furthermore, the lack of adequate control groups in some studies makes it challenging to accurately assess the effectiveness of personalized interventions compared to non-personalized ones.
Limitations
Some limitations of this review were that it was limited to studies in English and Spanish, which may have excluded relevant research in other languages. Expanding our search to additional languages could have provided further insights. It is worth noting that our review exclusively focused on non-pharmacological and non-surgical interventions for managing T2DM. While surgical procedures and medications for weight loss might be important aspects of T2DM remission, our goal was to investigate lifestyle and dietary approaches. However, the included studies had varying follow-ups, limiting conclusions to the medium term. Other limitations included variability in the duration of the interventions across studies, creating difficulty in evaluating and comparing results between studies, as well as variability in the definition of “remission”. This variability can impact the final outcomes for patients who really achieved remission based on the ADA definition in 2021. It also affects the comparability between the studies included in this review.
Perspectives
Together, the findings in this review underline the importance of focusing on individualized approaches and early intervention in diabetes management. It is remarkable how the perception of diabetes, once considered a lifelong condition, has turned towards being potentially curable for some patients. Further research in this area is crucial to gain a comprehensive understanding of the long-term implications of these interventions and their potential to revolutionize T2DM management.
Achieving remission from T2DM is possible for many patients, especially when using personalized and lifestyle-based approaches. This underscores the importance of an early intervention in managing the disease. Both low-calorie and low-carbohydrate diets have demonstrated their effectiveness in promoting weight loss and T2DM remission, although it is important to consider long-term sustainability. Personalized nutrition has proven effective in enhancing blood glucose control by adapting treatments on the basis of individual responses.
These investigations provide valuable insights into T2DM management, emphasizing that achieving disease remission is an attainable goal. Personalized approaches, early intervention, and consideration of physical fitness are key components of disease management, offering the potential to improve patient’s quality of life and healthcare resource efficiency.
Conclusions
The findings presented in this narrative review underscore the impact of dietary choices on the HbA1c% control, weight loss, lipid profiles, and T2DM remission of individuals with prediabetes and T2DM. In conclusion, one needs to look more closely at personalized approaches that consider individual patient characteristics and keep a consistent focus on diet, exercise, and lifestyle factors to better understand the factors influencing long-term remission in T2DM.
Achieving remission in T2DM is a complex process influenced by multiple factors. These include the stage of the disease, the extent of weight loss, the effectiveness of lifestyle changes, and treatment adherence. Therefore, adopting a personalized approach, with ongoing monitoring, is essential for both achieving and maintaining remission. The choice between these dietary strategies should consider individual preferences, tolerances, and metabolic responses, underlining the importance of personalized approaches in T2DM management. Understanding these aspects will help develop more effective and personalized strategies for managing T2DM, ultimately improving the quality of life for individuals living with this condition.
Data Availability
Data supporting this study is available in the supplementary material. No new data was created and no patient-identifiable data was used in the manuscript.
References
Goyal R, Singhal M, Jialal I. Type 2 diabetes. Treasure Island (FL): StatPearls. https://www.ncbi.nlm.nih.gov/books/NBK513253/. Accessed 15 Sep 2023.
Lin CL, Yu NC, Wu HC, et al. Association of body composition with type 2 diabetes: a retrospective chart review study. Int J Environ Res Public Health. 2021;18(9):4421.
Kelly J, Karlsen M, Steinke G. Type 2 diabetes remission and lifestyle medicine: a position statement from the American College of Lifestyle Medicine. Am J Lifestyle Med. 2020;14(4):406.
Buse JB, Caprio S, Cefalu WT, et al. How do we define cure of diabetes? Diabetes Care. 2009;32(11):2133.
Riddle MC, Cefalu WT, Evans PH, et al. Consensus report: definition and interpretation of remission in type 2 diabetes. Diabetes Care. 2021;44(10):2438–44. https://doi.org/10.2337/dci21-0034.
2020–2030 strategic plan for NIH nutrition research. DPCPSI. https://dpcpsi.nih.gov/onr/strategic-plan. Accessed 2 Nov 2023.
Merino J. Precision nutrition in diabetes: when population-based dietary advice gets personal. Diabetologia. 2022;65(11):1839–48. https://doi.org/10.1007/s00125-022-05721-6.
Ordovas JM, Ferguson LR, Tai ES, Mathers JC. Personalised nutrition and health. BMJ. 2018;361. https://www.bmj.com/content/361/bmj.k2173.
Chung WK, Erion K, Florez JC, et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2020;63(9):1671–93. https://doi.org/10.1007/s00125-020-05181-w.
Zeevi D, Korem T, Zmora N, et al. Personalized nutrition by prediction of glycemic responses. Cell. 2015;163(5):1079–94.
Berry SE, Valdes AM, Drew DA, et al. Human postprandial responses to food and potential for precision nutrition. Nat Med. 2020;26(6):964.
Wang DD, Hu FB. Precision nutrition for prevention and management of type 2 diabetes. Lancet Diabetes Endocrinol. 2018;6(5):416–26.
Bashiardes S, Godneva A, Elinav E, Segal E. Towards utilization of the human genome and microbiome for personalized nutrition. Curr Opin Biotechnol. 2018;1(51):57–63.
Chen R, Chen G. Personalized nutrition for people with diabetes and at risk of diabetes has begun. J Future Foods. 2022;2(3):193–202.
Guasch-Ferré M, Willett WC. The Mediterranean diet and health: a comprehensive overview. J Intern Med. 2021;290(3):549–66. https://doi.org/10.1111/joim.13333.
Feinman RD, Pogozelski WK, Astrup A, et al. Dietary carbohydrate restriction as the first approach in diabetes management: critical review and evidence base. Nutrition. 2015;31(1):1–13.
Brown A, Leeds AR. Very low-energy and low-energy formula diets: effects on weight loss, obesity co-morbidities and type 2 diabetes remission—an update on the evidence for their use in clinical practice. Nutr Bull. 2019;44:7–24.
JAND. Guide for authors—Journal of the Academy of Nutrition and Dietetics. https://www.elsevier.com/journals/journal-of-the-academy-of-nutrition-and-dietetics/2212-2672/guide-for-authors. Accessed 15 Sep 2023.
Rein M, Ben-Yacov O, Godneva A, et al. Effects of personalized diets by prediction of glycemic responses on glycemic control and metabolic health in newly diagnosed T2DM: a randomized dietary intervention pilot trial. BMC Med. 2022. https://doi.org/10.1186/s12916-022-02254-y.
de Hoogh IM, Pasman WJ, Boorsma A, van Ommen B, Wopereis S. Effects of a 13-week personalized lifestyle intervention based on the diabetes subtype for people with newly diagnosed type 2 diabetes. Biomedicines. 2022;10(3):643.
Ried-Larsen M, Johansen MY, MacDonald CS, et al. Type 2 diabetes remission 1 year after an intensive lifestyle intervention: a secondary analysis of a randomized clinical trial. Diabetes Obes Metab. 2019;21(10):2257–66.
Dave R, Davis R, Davies JS. The impact of multiple lifestyle interventions on remission of type 2 diabetes mellitus within a clinical setting. Obes Med. 2019;1(13):59–64.
Roncero-Ramos I, Gutierrez-Mariscal FM, Gomez-Delgado F, et al. Beta cell functionality and hepatic insulin resistance are major contributors to type 2 diabetes remission and starting pharmacological therapy: from CORDIOPREV randomized controlled trial. Transl Res. 2021;238:12–24.
Esposito K, Maiorino MI, Petrizzo M, Bellastella G, Giugliano D. The effects of a mediterranean diet on the need for diabetes drugs and remission of newly diagnosed type 2 diabetes: follow-up of a randomized trial. Diabetes Care. 2014;37(7):1824–30. https://doi.org/10.2337/dc13-2899.
Gardner CD, Landry MJ, Perelman D, et al. Effect of a ketogenic diet versus Mediterranean diet on glycated hemoglobin in individuals with prediabetes and type 2 diabetes mellitus: the interventional Keto-Med randomized crossover trial. Am J Clin Nutr. 2022;116(3):640.
Unwin D, Khalid AA, Unwin J, et al. Insights from a general practice service evaluation supporting a lower carbohydrate diet in patients with type 2 diabetes mellitus and prediabetes: a secondary analysis of routine clinic data including HbA1c, weight and prescribing over 6 years. BMJ Nutr Prev Health. 2020;3(2):285.
Durrer C, McKelvey S, Singer J, et al. A randomized controlled trial of pharmacist-led therapeutic carbohydrate and energy restriction in type 2 diabetes. Nat Commun. 2021. https://doi.org/10.1038/s41467-021-25667-4.
Steven S, Hollingsworth KG, Al-Mrabeh A, et al. Very low-calorie diet and 6 months of weight stability in type 2 diabetes: pathophysiological changes in responders and nonresponders. Diabetes Care. 2016;39(5):808–15. https://doi.org/10.2337/dc15-1942.
Wei J, Chen J, Wei X, et al. Long-term remission of type 2 diabetes after very-low-calorie restriction and related predictors. Front Endocrinol (Lausanne). 2022;12(13):968239.
Lean ME, Leslie WS, Barnes AC, et al. Primary care-led weight management for remission of type 2 diabetes (DiRECT): an open-label, cluster-randomised trial. Lancet. 2018;391(10120):541–51.
Bynoe K, Unwin N, Taylor C, et al. Inducing remission of type 2 diabetes in the Caribbean: findings from a mixed methods feasibility study of a low-calorie liquid diet-based intervention in Barbados. Diabet Med. 2020;37(11):1816–24. https://doi.org/10.1111/dme.14096.
Taheri S, Zaghloul H, Chagoury O, et al. Effect of intensive lifestyle intervention on bodyweight and glycaemia in early type 2 diabetes (DIADEM-I): an open-label, parallel-group, randomised controlled trial. Lancet Diabetes Endocrinol. 2020;8(6):477–89.
National Academies of Sciences, Engineering, and Medicine; Health and Medicine Division; Food and Nutrition Board; Food Forum, Callahan AE. Challenges and opportunities for precision and personalized nutrition. Washington (DC): National Academies Press; 2021. https://doi.org/10.17226/26407.
Acknowledgements
We thank for meticulous attention to detail and linguistic expertise provided by Elena Atkinson which significantly improved the clarity and readability of the paper.
Funding
No funding or sponsorship was received for the study or publication of this article.
Author information
Authors and Affiliations
Contributions
Ana T. Arias-Marroquin, Fabiola M. Del Razo-Olvera, Zaira M. Castaneda-Bernal and Daniel B Elias-Lopez contributed significantly to the development and drafting of the manuscript. The selection and revision of articles were conducted by Eustorgio Cruz-Juarez, Maria F. Camacho-Ramirez, Miguel A. Lara-Sanchez, Lucia Chalita-Ramos, and Valeria Rebollar-Fernandez. Carlos A. Aguilar-Salinas reviewed the content, provided valuable intellectual input regarding study ideas and concepts, and granted approval for the manuscript’s submission.
Corresponding author
Ethics declarations
Conflict of Interest
Ana T. Arias-Marroquín, Fabiola M. Del Razo-Olvera, Zaira M. Castañeda-Bernal, Daniel B. Elías-López, Eustorgio Cruz-Juárez, María F. Camacho-Ramírez, Miguel A. Lara-Sánchez, Lucía Chalita-Ramos, and Valeria Rebollar-Fernández declare no conflict of interest. Carlos A. Aguilar-Salinas is an Editorial Board member of Diabetes Therapy. Carlos A. Aguilar-Salinas was not involved in the selection of peer reviewers for the manuscript nor any of the subsequent editorial decisions.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Arias-Marroquín, A.T., Del Razo-Olvera, F.M., Castañeda-Bernal, Z.M. et al. Personalized Versus Non-personalized Nutritional Recommendations/Interventions for Type 2 Diabetes Mellitus Remission: A Narrative Review. Diabetes Ther 15, 749–761 (2024). https://doi.org/10.1007/s13300-024-01545-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-024-01545-2