Abstract
Introduction
Obesity prevalence has increased in Japan in recent years. Given the strong association of obesity with poor glycemic control, and increased risk of type 2 diabetes (T2D) with central obesity, this study describes the current trends and relationships between glycated hemoglobin (HbA1c), body mass index (BMI), and waist circumference in the Japanese people with T2D.
Methods
This was a retrospective, cross-sectional study of people with T2D who had at least one recorded HbA1c and BMI (or waist circumference) value in the Japan Medical Data Center Claims database. Five annual cohorts of the study population were formed between January 2017 and December 2021. Annual trends of HbA1c across BMI categories (obesity class I [≥ 25 ~ < 30 kg/m2]–IV [≥ 40 kg/m2]) and in people with central obesity (waist circumference: ≥ 85 cm in men; ≥ 90 cm in women) were described by sex and age groups.
Results
Overall, 106,089 people with T2D (HbA1c and BMI data: 106,079; HbA1c and waist circumference data: 105,424) were included, with the majority of people belonging to obesity class I (range: 39.7–40.6%) and obesity class II (range: 16.2–17.7%) categories across all annual cohorts. People in higher BMI categories had higher mean HbA1c, with > 50% of people with T2D in obesity class I–IV (54.8–56.5%) having HbA1c ≥ 7%. Between 2017 and 2021, BMI and waist circumference increased in the age group 18–44 years. More than 50% of people with T2D and central obesity in both sexes and people of age group 18–44 years across obesity class I–IV or with central obesity had HbA1c ≥ 7%.
Conclusion
More than half of the people with T2D belonging to obesity class I–IV or central obesity had poor glycemic control (HbA1c ≥ 7%), especially in the 18–44 age group. This highlights the need for body weight management for better glycemic control in relatively young Japanese people with T2D and obesity.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out the study? |
Obesity prevalence has increased in Japan in recent years. Given the strong association of obesity with poor glycemic control, an increased risk of type 2 diabetes (T2D) with central obesity exists |
Limited data are available describing the trends of glycated hemoglobin (HbA1c) across body mass index (BMI) or waist circumference categories in Japanese people with T2D |
Understanding the trends and relationship among HbA1c, BMI, and waist circumference could help assess future treatment strategies for T2D |
What was learned from the study? |
The results from this Japanese claims-based study indicated that people with T2D in higher BMI categories had higher mean HbA1c |
More than half of the people with T2D in obesity class I–IV and those with central obesity had poor glycemic control (HbA1c ≥ 7%), particularly in the age group 18–44 years |
Body weight management could aid in better glycemic control in people with T2D and obesity, particularly in younger age groups |
Introduction
Prevalence of type 2 diabetes (T2D) has been increasing in Japan from 1990 (6.6%) to 2010 (7.9%) and is estimated to increase to 9.8% by 2030 [1]. In 2014, a retrospective study conducted in 55,452 Japanese working professionals aged 20–69 years reported that the prevalence of T2D was 8.0% in men and 3.3% in women, with approximately 80% of people with T2D having glycated hemoglobin (HbA1c) levels ≥ 6.5% [2].
Obesity is a common comorbidity of T2D, strongly linked to impaired glycemic control, and a known risk factor for cardiovascular disease [3,4,5]. Notably, an analysis of IBM® MarketScan® Explorys® Claims-EMR database in the US from 2012 to 2019 indicated that, with an increase in body mass index (BMI), there was a decrease in the number of people with T2D who achieve glycemic control [6].
Body composition is one of the main determinants for the difference in T2D pathophysiology between Japanese and Caucasians [7]. Interestingly, the definition of obesity categories in Japan is different compared to western countries. The World Health Organization defines BMI 25–30 kg/m2 as overweight, whereas the Japan Society for the Study of Obesity (JASSO) defines this as obesity class I, owing to the differences in body composition [8].
In recent years, there has been an increase in the prevalence of people with obesity in Japan [9]. A 12-year-long study in Japanese people with T2D between 2000 and 2012 reported an increase in prevalence of people in obesity class I (BMI: 25–30 kg/m2) from 27 to 30.9% and in obesity class II–IV (BMI: ≥ 30 kg/m2) from 5.1 to 10% [9]. The study also indicated that the prevalence of overweight and obesity was higher in the younger age groups [9].
In addition to BMI, central obesity is positively associated with T2D in the Japanese population [10] and is reported to increase the risk of T2D by 72% [11]. Waist circumference is a known measuring index of central obesity and an appropriate measure of obesity in the Asian [10, 12] and elderly populations [13]. However, limited data are available that illustrate the trends of HbA1c, BMI, and waist circumference across different age and sex groups in the Japanese population.
The management of obesity is complex. In Japan, elimination diets, improved eating habits, and increased physical activity are used for management of weight [14, 15]. Very few Japanese healthcare providers consider medications and bariatric surgery for the treatment of people with obesity [14]. Therefore, this study primarily focused on exploring the trends of HbA1c, BMI, and waist circumference in Japanese people with T2D, highlighting the importance of glycemic control through weight loss.
Methods
Study Overview
This was a retrospective, cross-sectional study using the data from Japan Medical Data Center (JMDC) claims database, constructed by the JMDC Inc. (Tokyo, Japan), using standardized disease classifications and anonymous record linkage [16]. The JMDC database contains de-identified inpatient, outpatient, dispensing records, medical examination, and ledger information data pooled from different health insurance associations and is therefore commonly used for the estimation of prevalence and incidence rate [17, 18]. The database captured the information of 17 million Japanese people as of December 2023 [16].
As this was a retrospective study conducted to describe the real-world trends of HbA1c and BMI categories by the JASSO guideline in people with T2D in Japan, all the available and eligible people who satisfied the selection criteria were included. This study was conducted in accordance with the Declaration of Helsinki and Good Pharmacoepidemiology Practices. Per the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects [33], ethical review and informed consent were not required, as this was a non-interventional, retrospective study that used anonymized patient data.
Study Design
People with T2D who had at least one recorded value of HbA1c and BMI (or waist circumference) were identified to form five annual cohorts between January 2017 and December 2021 (Fig. 1). Each annual cohort comprised people who were (1) ≥ 18 years of age on the date of annual check-up, (2) had a confirmed diagnosis of T2D (International Classification of Diseases [ICD]-10th revision; ICD-10 code: E11–14) with a prescription for an antihyperglycemic agent (Anatomical Therapeutic Chemical code [ATC] code: A10), and (3) had at least 1 pair of health check-up data which included HbA1c and BMI, or HbA1c and waist circumference values. People were excluded from the annual cohorts if they had a confirmed diagnosis of type 1 diabetes (ICD-10 code: E10), gestational diabetes (ICD-10 code: O24.4–24.9; P70.0), postsurgical hypoinsulinemia (ICD-10 code: E89.1), drug-induced Cushing syndrome (ICD-10 code: E24.2), or cancer (ICD-10 code: C00-D48).
Statistical Analysis
Patient demographics including the age on the date of annual check-up, sex, BMI, waist circumference, HbA1c, fasting blood glucose, comorbidities, and concomitant medications were described for each annual cohort (as defined in Supplementary Table 1).
Trends of HbA1c were categorized based on the American Diabetes Association target of HbA1c < 7% [19], and the trends of BMI were categorized based on the JASSO guideline (Supplementary Table 2) [8]. The proportion of people with central obesity (waist circumference of ≥ 85 cm in men and ≥ 90 cm in women measured at the level of umbilicus) was described based on the Japanese definition of metabolic syndrome [20]. Additionally, the annual distribution of HbA1c across BMI categories and annual distribution of HbA1c with central obesity were described by sex and age groups (18–44, 45–54, 55–64, and ≥ 65 years).
Continuous variables were presented as number, mean (standard deviation), and median (range), whereas categorical variables were presented as frequency and percentage. Analyses were conducted using SAS Software, version 9.4 (SAS Institute Inc., Cary, NC, USA).
Results
Study Cohort Selection
A total of 273,758 people who were ≥ 18 years of age, had a confirmed diagnosis of T2D, and had received a prescription for an antihyperglycemic agent between 2017 and 2021 were selected (Fig. 2). Following exclusion criteria, 106,089 people with T2D with at least one recorded HbA1c and BMI value (or waist circumference) (2017: 37,017; 2018: 41,920; 2019: 51,268; 2020: 60,145; 2021: 72,633) were included (Fig. 2). Of these, 106,079 people with T2D had both HbA1c and BMI data, 105,424 people with T2D had both HbA1c and waist circumference data, and 105,424 people with T2D had both BMI and waist circumference data.
Baseline and Demographic Characteristics
The demographic characteristics were similar across all annual cohorts (mean age range: 53.1–53.6 years; women: 14.2–15.2%) (Table 1). The majority of the people with T2D belonged to the obesity class I (range: 39.7–40.6%), normal weight (range: 34.0–37.2%), or obesity class II (range: 16.2–17.7%) categories (Table 1). Of note, during the study period, while the proportion of people with central obesity increased, the mean BMI of people with T2D did not change (2017: 26.8 kg/m2, 2021: 27.3 kg/m2). Among people with T2D, central obesity was more prevalent in men (range: 72.8–76.7%) than in women (range: 47.4–51.5%) between 2017 and 2021 (Table 1). The proportion of people with T2D with comorbidities (chronic kidney disease, congestive heart failure, and metabolic syndrome), and the prescription of concomitant cardiovascular medications (antihypertensive agent, lipid-lowering drugs) increased from 2017 to 2021 (Table 1).
Annual Trends of HbA1c Across BMI Categories
Overall, in people with higher BMI, mean HbA1c was higher and ranged from 7.1% in the normal weight category to 7.5% in obesity class IV (Fig. 3). The proportion of people with T2D who had poor glycemic control (HbA1c ≥ 7%) increased across obesity class I–IV and ranged from 54.8 to 56.5% (Table 2).
Subgroup Analyses by Sex and Age Groups
Mean HbA1c change was comparable between sexes across the annual cohorts from 2017 to 2021 (Fig. 4a). A larger proportion of men and women had good glycemic control (HbA1c < 7%) compared with poor glycemic control (HbA1c ≥ 7%) in the normal weight category (Table 3). A contrasting trend was observed in men and women belonging to obesity class III–IV with up to 62% of the men and up to 61% of the women having poor glycemic control (HbA1c ≥ 7%) (Table 3).
a Trend of mean HbA1c by sex; b trend of mean BMI by sex; c trend of mean waist circumference by sex. a A total of 106,089 people with T2D had HbA1c data, b a total of 106,079 people with T2D had BMI data, and c a total of 105,424 people with T2D had waist circumference data between 2017 and 2021. BMI, body mass index; HbA1c, glycated hemoglobin; N, total number of people with T2D
Mean HbA1c was comparable across all age groups from 2017 to 2021; however, there was a decrease in mean HbA1c with an increase in age, ranging from 7.0% in ≥ 65 years age group to 7.7% in 18–44 years age group (Fig. 5a). The proportion of people with poor glycemic control was higher in younger (18–44 years) and middle-aged groups (45–55 years and 55–64 years) compared with the older (≥ 65 years) age group, in obesity class I–III categories (Table 4).
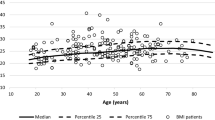
a Trend of mean HbA1c by age group; b trend of mean BMI by age group; c trend of mean waist circumference by age group. a A total of 106,089 people with T2D had HbA1c data, b a total of 106,079 people with T2D had BMI data, and c a total of 105,424 people with T2D had waist circumference data between 2017 and 2021. BMI, body mass index; HbA1c, glycated hemoglobin; N, total number of people with T2D
Mean BMI was comparable in both sexes and consistent from 2017 to 2021 (Fig. 4b). However, a decrease was noted in mean BMI with age, ranging from 24.8 kg/m2 in the ≥ 65 years age group to 29.7 kg/m2 in the 18–44 years age group (Fig. 5b).
Annual Trends of HbA1c by Waist Circumference
There was an increase in mean waist circumference from 2017 to 2021 in both sexes and all age groups. Men had slightly higher mean waist circumference (range: 92.3–93.5 cm) compared with women (range: 89.9–91.2 cm) (Fig. 4c). There was a decrease in mean waist circumference with increase in age (Fig. 5c). Mean waist circumference ranged from 87.1 cm in the ≥ 65 years age group to 97.8 cm in the 18–44 years age group (Fig. 5c). Between 2017 and 2021, mean waist circumference increased with an increase in BMI across obesity class I–IV, with the highest mean waist circumference observed in obesity class IV for both men (range: 127.0–127.7 cm) and women (range: 121.3–122.1 cm) (Fig. 6).
A higher proportion of people with central obesity (men ≥ 85 cm or women ≥ 90 cm) compared to those without central obesity (men < 85 cm or women < 90 cm) had poor glycemic control (Table 5). More than 58% of people in the 18–44 years age group with central obesity had poor glycemic control (Table 5).
Discussion
This retrospective, cross-sectional study in Japanese people with T2D showed that mean HbA1c increased with increase in BMI; more than half of the people with T2D belonging to obesity class I-IV had poor glycemic control. Younger age groups showed higher mean HbA1c, mean BMI, and mean waist circumference than the older age group (≥ 65 years).
Approximately 40% of people with T2D had BMI 25–30 kg/m2 and 25% of people had BMI ≥ 30 kg/m2 in this study. There was an increase in the number of eligible people in annual cohorts from 2017 to 2021, owing to the increase in number of people with T2D who were prescribed an antihyperglycemic agent. The mean BMI of annual cohorts was 27 kg/m2, and there was no change in mean BMI from 2017 to 2021. Our results were consistent with a study National Health Interview Survey demonstrating that the Asian population have lower BMI than their white counterparts, with a larger proportion having BMI 23–27.5 kg/m2 than BMI ≥ 27.5 kg/m2 [21]. However, people in Asia tend to develop diabetes with lower obesity rates [12], which could be attributed to the higher proportion of physiological markers for insulin resistance compared with their white counterparts [22]. Results from a US-based study showed that Asian Americans were 30% more likely to have T2D compared with their white counterparts [21].
A study conducted in Japan between 2009 and 2014 showed that the incidence of overweight (23.0 ≤ BMI < 27.5 kg/m2) and obesity (BMI ≥ 27.5 kg/m2) was approximately double in men (28.3% and 6.7%, respectively) compared with women (14.3% and 3.9%, respectively) [23]. Contrastingly, in our study, mean BMI was comparable between both sexes across all annual cohorts. Although BMI was consistent, waist circumference increased over time in both men and women. These results from our study were in agreement with another study in Japan conducted using annual health check-up data from 2008 to 2017 [24]. The study reported that irrespective of body weight changes, waist circumference increased in men and women over time [24]. Moreover, increase in waist circumference was positively associated with serum triglycerides, low-density lipoprotein cholesterol, and increased mortality risk in the elderly population [13, 24], making waist circumference an important parameter to assess in annual health check-ups.
The results from our study are consistent with the findings from the Japan Diabetes Clinical Data Management Study Group (JDDM), where HbA1c levels had risen in recent years in Japanese people with T2D (from 7.0% in 2016 to 7.1% in 2021) [25]. However, only people in the normal weight category in this study had mean HbA1c of 7.1–7.2% between 2017 and 2021. People with T2D in higher BMI categories had mean HbA1c ranging from 7.3 to 7.5%. The difference in the mean HbA1c could be attributed to the differences in the population demographics between the two databases. Unlike our study, the participating facilities in the JDDM joint study primarily included clinics located across Japan with older patients (mean age 67.7 years) with lower BMI (mean BMI 24.7 kg/m2) [25].
Previous studies have indicated that one in four people with T2D have poor glycemic control with increased BMI [26] and that higher BMI is associated with higher HbA1c and worsened glycemic control [6]. Results from our study conducted on Japanese people with T2D were similar to those obtained from the western population [6], indicating that increased mean HbA1c correlated with increased BMI and waist circumference; people with higher BMI and with central obesity had poor glycemic control. Weight loss has been shown to reduce insulin resistance, consequently improving glycemic control in patients with T2D [5]. Given that reduction in HbA1c is a crucial marker for glycemic control, interventions aiding weight loss could be additional potential therapeutic targets for T2D [5]. Therefore, an understanding of the relationship between HbA1c and BMI could help assess future treatment strategies of T2D while targeting obesity.
The current FDA-approved treatments for people with obesity including lifestyle interventions and pharmacotherapy lead to 3–8.6% weight loss, and invasive procedures such as bariatric surgery reduce 25–30% of body weight within 1–2 years [27, 28], indicating a need for more effective and less invasive treatments targeting obesity in people with T2D. Novel treatments of T2D, such as semaglutide and tirzepatide, have demonstrated body weight reduction of 12.6% and up to 21%, respectively [27, 29]. Hence, T2D treatments demonstrating glycemic control along with weight loss could be promising options. It could be hypothesized that the slight decrease in mean HbA1c in our study population from 2020 to 2021 was due to the introduction of semaglutide in Japan in 2020.
In our study, higher BMI was observed in younger age groups compared with the older age groups, which is consistent with a large-scale study conducted in Japan [9]. Notably, more than 58% of people with central obesity in the 18–44 years age group had poor glycemic control in this study. Higher rates of poor glycemic control and obesity in younger age groups could possibly be due to poor compliance with proper dietary habits and treatment [15]. Furthermore, weight gain in younger age groups increases risk of T2D development [30, 31]. The results suggest that more effective intervention or changes in lifestyle may be necessary for young people in Japan with T2D. Therefore, targeting obesity in people with T2D in younger age groups is necessary.
As the data used for this study were sourced from healthcare insurance associations of company employees and their dependents, data from people aged > 65 years in the JMDC database were limited. Furthermore, the analysis did not examine how several factors such as medication use or insurance affected trends in HbA1c or BMI. Moreover, the trends were examined without adjustment for age and BMI. The relationship between HbA1c and BMI categories (or waist circumference) was described only in people aged 18–75 years. Interestingly, in women at the age of menarche, an inverse relationship exists between BMI and waist circumference (P < 0.001) [32]. As per a multivariate-adjusted model, with each 1-year decrease in age at menarche, BMI and waist circumference increased by 0.25 kg/m2 and 0.6 cm, respectively [32]. Another limitation was that the proportion of women compared with men was smaller (14.6% vs 85.4%). Hence, findings from sex-based subgroup analyses should be interpreted with caution.
Conclusion
Mean HbA1c increased with an increase in BMI in Japanese people with T2D. More than half of the people with T2D belonging to obesity class I–IV or central obesity had poor glycemic control, with the proportions even higher in the 18–44 year age group. An in-depth understanding of the relationship between BMI and central obesity with glycemic control could help to manage T2D better.
Data Availability
The data used for the current study are not publicly available because they were provided by the JMDC to Eli Lilly Japan, and the data license agreement does not permit sharing of datasets with people external to the study team. Interested readers may request the data directly from JMDC (https://www.jmdc.co.jp/en/).
References
Goto A, Noda M, Inoue M, Goto M, Charvat H. Increasing number of people with diabetes in Japan: is this trend real? Intern Med. 2016;55(14):1827–30.
Uehara A, Kurotani K, Kochi T, Kuwahara K, Eguchi M, Imai T, et al. Prevalence of diabetes and pre-diabetes among workers: Japan epidemiology collaboration on occupational health study. Diabetes Res Clin Pract. 2014;106(1):118–27.
Colosia AD, Palencia R, Khan S. Prevalence of hypertension and obesity in patients with type 2 diabetes mellitus in observational studies: a systematic literature review. Diabetes Metab Syndr Obes. 2013;6:327–38.
Lu Y, Hajifathalian K, Ezzati M, Woodward M, Rimm EB, Danaei G. Metabolic mediators of the effects of body-mass index, overweight, and obesity on coronary heart disease and stroke: a pooled analysis of 97 prospective cohorts with 1.8 million participants. Lancet. 2014;383(9921):970–83.
Gummesson A, Nyman E, Knutsson M, Karpefors M. Effect of weight reduction on glycated haemoglobin in weight loss trials in patients with type 2 diabetes. Diabetes Obes Metab. 2017;19(9):1295–305.
Boye KS, Lage MJ, Shinde S, Thieu V, Bae JP. Trends in HbA1c and body mass index among individuals with type 2 diabetes: evidence from a US database 2012–2019. Diabetes Ther. 2021;12(7):2077–87.
Moller JB, Pedersen M, Tanaka H, Ohsugi M, Overgaard RV, Lynge J, et al. Body composition is the main determinant for the difference in type 2 diabetes pathophysiology between Japanese and Caucasians. Diabetes Care. 2014;37(3):796–804.
Kanazawa M, Yoshiike N, Osaka T, Numba Y, Zimmet P, Inoue S. Criteria and classification of obesity in Japan and Asia-Oceania. World Rev Nutr Diet. 2005;94(R):1.
Miyazawa I, Kadota A, Miura K, Okamoto M, Nakamura T, Ikai T, et al. Twelve-year trends of increasing overweight and obesity in patients with diabetes: the Shiga Diabetes Clinical Survey. Endocr J. 2018;65(5):527–36.
Abe M, Fujii H, Funakoshi S, Satoh A, Kawazoe M, Maeda T, et al. Comparison of body mass index and waist circumference in the prediction of diabetes: a retrospective longitudinal study. Diabetes Ther. 2021;12(10):2663–76.
Cao C, Hu H, Zheng X, Zhang X, Wang Y, He Y. Association between central obesity and incident diabetes mellitus among Japanese: a retrospective cohort study using propensity score matching. Sci Rep. 2022;12(1):13445.
Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, et al. Epidemic obesity and type 2 diabetes in Asia. Lancet. 2006;368(9548):1681–8.
de Hollander EL, Bemelmans WJ, Boshuizen HC, Friedrich N, Wallaschofski H, Guallar-Castillón P, et al. The association between waist circumference and risk of mortality considering body mass index in 65- to 74-year-olds: a meta-analysis of 29 cohorts involving more than 58 000 elderly persons. Int J Epidemiol. 2012;41(3):805–17.
Iwabu M, Yamauchi T, Shimomura I, Eguchi K, Ogawa Y. Perceptions, attitudes and barriers to obesity management: Japanese data from the ACTION-IO study. J Diabetes Investig. 2021;12(5):845–58.
Gouda M, Matsukawa M, Iijima H. Associations between eating habits and glycemic control and obesity in Japanese workers with type 2 diabetes mellitus. Diabetes Metab Syndr Obes. 2018;11:647–58.
JMDC. JMDC claims database. 2022. https://www.jmdc.co.jp/en/jmdc-claims-database/. Accessed 14 July 2023.
Takeuchi M, Shinkawa K, Yanagita M, Kawakami K. Prevalence, recognition and management of chronic kidney disease in Japan: population-based estimate using a healthcare database with routine health checkup data. Clin Kidney J. 2021;14(10):2197–202.
Wang D, Ito C, Homma Y, Arimitsu M, Yoshisue H. Prevalence and clinical characteristics of patients with moderate-to-severe asthma in Japan using a JMDC claims database. Int Arch Allergy Immunol. 2023;184(7):698–706.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S66–76.
Matsuzawa Y. Metabolic syndrome–definition and diagnostic criteria in Japan. J Atheroscler Thromb. 2005;12(6):301.
Lee JW, Brancati FL, Yeh HC. Trends in the prevalence of type 2 diabetes in Asians versus whites: results from the United States National Health Interview Survey, 1997–2008. Diabetes Care. 2011;34(2):353–7.
Raji A, Seely EW, Arky RA, Simonson DC. Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab. 2001;86(11):5366–71.
Hasegawa M, Akter S, Hu H, Kashino I, Kuwahara K, Okazaki H, et al. Five-year cumulative incidence of overweight and obesity, and longitudinal change in body mass index in Japanese workers: the Japan epidemiology collaboration on occupational health study. J Occup Health. 2020;62(1): e12095.
Ono H, Akahoshi K, Kai M. Change in waist circumference and lifestyle habit factors as a predictor of metabolic risk among middle-aged and elderly Japanese people: population-based retrospective 10-year follow-up study from 2008 to 2017. Arch Public Health. 2022;80(1).
Japan Diabetes Clinical Data Management (JDDM) Study Group. http://jddm.jp/public-information/index-2021/. Accessed 18 July 2023.
Weng W, Tian Y, Kimball ES, Kong SX, Bouchard J, Hobbs TM, et al. Treatment patterns and clinical characteristics of patients with type 2 diabetes mellitus according to body mass index: findings from an electronic medical records database. BMJ Open Diabetes Res Care. 2017;5(1): e000382.
Jastreboff AM, Aronne LJ, Ahmad NN, Wharton S, Connery L, Alves B, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205–16.
American DA. Obesity management for the treatment of type 2 diabetes: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S89–97.
Zhong P, Zeng H, Huang M, Fu W, Chen Z. Efficacy and safety of once-weekly semaglutide in adults with overweight or obesity: a meta-analysis. Endocrine. 2022;75(3):718–24.
Brancati FL, Wang NY, Mead LA, Liang KY, Klag MJ. Body weight patterns from 20 to 49 years of age and subsequent risk for diabetes mellitus: the Johns Hopkins precursors study. Arch Intern Med. 1999;159(9):957–63.
Resnick HE, Valsania P, Halter JB, Lin X. Relation of weight gain and weight loss on subsequent diabetes risk in overweight adults. J Epidemiol Community Health. 2000;54(8):596–602.
Sumi A, Iwase M, Nakamura U, Fujii H, Ohkuma T, Ide H, et al. Impact of age at menarche on obesity and glycemic control in Japanese patients with type 2 diabetes: Fukuoka Diabetes Registry. J Diabetes Investig. 2018;9(5):1216–23.
Sone S. Ethical guidelines for clinical trials in medical research involving human subjects. Gan To Kagaku Ryoho. 2015;42(8):893–902.
Medical Writing, Editorial, and Other Assistance
Writing and editing assistance for this article was provided by Dr. Shaleen Multani of Eli Lilly Services India Private Limited.
Funding
Funding for this study was provided by Eli Lilly Japan K.K. and Mitsubishi Tanabe Pharma Corporation. The Rapid Service Fee was funded by Eli Lilly Japan K.K.
Author information
Authors and Affiliations
Contributions
Kazuo Hara and Tetsuaki Hirase, helped with interpretation of results, critical revision of the presentation, and final approval. Swathi Pathadka, Zhihong Cai, and Manaka Sato were involved in conception and design of work, interpretation of results, critical revision of the presentation, and final approval. Noriyuki Ishida and Ryo Takemura helped with analysis and interpretation of results, critical revision of the presentation, and final approval.
Corresponding author
Ethics declarations
Conflict of Interest
Kazuo Hara received lecture fees from Eli Lilly Japan K. K., Mitsubishi Tanabe Pharma Corporation, Nippon Boehringer Ingelheim Co. Ltd., AstraZeneca K.K. Ono Pharmaceutical Co. Ltd., Daiichi Sankyo Co. Ltd., Novo Nordisk, and Sumitomo Pharma Co. Ltd. Tetsuaki Hirase, Swathi Pathadka, Zhihong Cai, and Manaka Sato are full-time employees and stakeholders of Eli Lilly Japan. Noriyuki Ishida and Ryo Takemura have nothing to disclose.
Ethical Approval
This study was conducted in accordance with the Declaration of Helsinki and Good Pharmacoepidemiology Practices. Per the Japanese Ethical Guidelines for Medical and Health Research Involving Human Subjects [33], ethical review and informed consent were not required, as this was a non-interventional, retrospective study that used anonymized patient data.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Hara, K., Hirase, T., Pathadka, S. et al. Trends of HbA1c and BMI in People with Type 2 Diabetes: A Japanese Claims-Based Study. Diabetes Ther 15, 801–817 (2024). https://doi.org/10.1007/s13300-024-01543-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-024-01543-4