Abstract
Introduction
Insulin is the first-line pharmacologic therapy for women with diabetes in pregnancy. However, conducting well-designed randomized clinical trials (RCTs) and achieving recommended glycemic targets remains a challenge for this unique population. This systematic literature review (SLR) aimed to understand the evidence for insulin use in pregnancy and the outcome metrics most often used to characterize its effect on glycemic, maternal and fetal outcomes in gestational diabetes mellitus (GDM) and in pregnant women with diabetes.
Methods
An SLR was conducted using electronic databases in Medline, EMBASE via Ovid platform, evidence-based medicine reviews (2010–2020) and conference proceedings (2018–2019). Studies were included if they assessed the effect of insulin treatment on glycemic, maternal or fetal outcomes in women with diabetes in pregnancy. Studies on any type of diabetes other than gestational or pre-existing diabetes as well as non-human studies were excluded.
Results
In women diagnosed with GDM or pre-existing diabetes, most studies compared treatment of insulin with metformin (n = 35) followed by diet along with lifestyle intervention (n = 24) and glibenclamide (n = 12). Most studies reporting on glycemic outcomes compared insulin with metformin (n = 22) and glibenclamide (n = 4). Fasting blood glucose was the most reported clinical outcome of interest. Among the studies reporting maternal outcomes, method of delivery and delivery complications were most commonly reported. Large for gestational age, stillbirth and perinatal mortality were the most common fetal outcomes reported.
Conclusion
This SLR included a total of 108 clinical trials and observational studies with diverse populations and treatment arms. Outcomes varied across the studies, and a lack of consistent outcome measures to manage diabetes in pregnant women was observed. This elucidates a need for global consensus on study design and standardized clinical, maternal and fetal outcomes metrics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
The prevalence of diabetes during pregnancy has increased in recent years, and many women with this complication require insulin during their pregnancy. Despite this, there remains a paucity of well-designed clinical trials targeting insulin use in this unique population |
This systematic literature review aimed to assess and summarize the current body of evidence for insulin use in pregnant women with gestational or pre-existing diabetes and its effects on clinical, maternal and fetal outcomes |
What was learned from the study? |
This SLR included a total of 108 unique studies, both clinical and observational, and the most commonly reported outcomes were fasting blood glucose, method of delivery and large for gestational age |
Overall, the results of this review revealed that the outcomes evaluated in studies investigating the use of insulin as a treatment option for pregnant women with diabetes varied widely across the included studies, illustrating the need for standardization of study design and outcome metrics |
Introduction
Diabetes is the most prevalent antenatal complication of pregnancy and can be subdivided into two types: pregestational and gestational diabetes mellitus (GDM) [1]. The prevalence of diabetes in pregnancy has been increasing in the USA [2]. About 1–2% of pregnant women have pre-existing diabetes, and approximately 1–14% of all pregnancies are affected by GDM [3, 4]. Women diagnosed with diabetes during pregnancy are at an increased risk to develop other maternal complications such as gestational hypertension, preeclampsia and hypoglycemia, which subsequently can lead to the development of type 2 diabetes (T2D) later in life [3]. They are also at a higher risk to undergo cesarean section or have premature delivery. In addition, diabetes in pregnancy is associated with a risk of developing fetal complications such as macrosomia and neonates with large for gestational age (LGA), small for gestational age, premature birth, neonatal respiratory distress, asphyxia, neonatal hypoglycemia and congenital anomalies [5, 6].
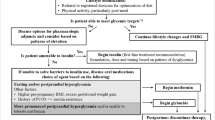
The recommendations from current standard of care of diabetes management in pregnant women are beyond regular blood glucose level monitoring, lifestyle behavioral changes, medical nutrition therapy (MNT), physical exercise and pharmacotherapy (metformin, glyburide or insulin) [7]. Insulin is considered the most efficacious pharmacotherapy for all types of diabetes in pregnancy, including GDM and pregestational diabetes [8]. The 2023 update of the the American Diabetes Association (ADA) guidelines, The American College of Obstetricians and Gynecologists-2018 (ACOG-2018) and International Diabetes Federation (IDF) guidelines recommend use of insulin as a first-line pharmacological therapy for management of pre-existing diabetes and GDM over other oral anti-diabetic agents [9,10,11,12].
Recent advances in insulin therapy are focused on improving the pharmacokinetics and pharmacodynamics of insulin. These goals enable prolonged profile of action, flexible dosing regimen and reduce the risk of hypoglycemia [13]. However, well-powered randomized clinical trials (RCTs) in pregnant women with diabetes are often conducted well after non-pregnant populations, if it is done at all, which leads to delayed implementation of evidence-based practices for insulin use in pregnancy. In addition, designing studies to demonstrate the achievement of stringent glycemic targets as recommended by the guidelines remains challenging for this unique population [14]. A variety of insulins have been commercially available globally, many of which have limited data on their use in pregnancy. Real-world barriers such as access to insulin or newer insulins, access to glucose monitoring and delayed prenatal care can further make adhering to guidelines difficult, if not impossible. Considering the different insulin options available in the global market and understanding the use and effects of types of insulin and/or insulin regimens on glycemic, maternal and fetal outcomes may support clinical practice. This may as well aid in improving study designs for treatment of diabetes in pregnancy. Therefore, to assess and evaluate the current body of evidence including RCTs and real-world observational data, we performed a systematic literature review (SLR) to better understand and summarize the evidence for insulin use in pregnancy to harmonize future study design in this special population.
Methods
Study Design
Search Strategy
A comprehensive search was conducted to identify relevant studies using electronic databases in Medline, EMBASE via Ovid platform and evidence-based medicine reviews from 1 January 2010 to 25 August 2020. In addition, manual (hand) searches were performed for relevant conference abstracts that were published from 2018 to 2019.
Inclusion and Exclusion Criteria
The eligibility for assessing the relevance of each article for data extraction was based on the population, intervention, comparison, outcomes and study design (PICOS) criteria (Supplementary Table 1). Inclusion criteria for the selection of articles consisted of studies that were RCTs, non-RCTs and observational studies (Supplementary Table 1). Studies were included with perinatal women diagnosed with either gestational, pre-existing diabetes (type 1 diabetes [T1D] or type 2 diabetes [T2D]) or mixed population (pregnant women with GDM, T1D or T2D). Specific glycemic (fasting blood glucose [FBG], post prandial glucose [PPG] and time in range), maternal (prevalence of hypoglycemia, cesarean section, preterm labor, hypertension, induced labor and preterm delivery) and fetal (fetal mortality, fetal morbidity and LGA) outcomes were included in this review (Supplementary Table 1). Studies on any type of diabetes other than gestational diabetes or pre-existing T1D or T2D as well as non-human studies were excluded.
Study Selection and Data Extraction
The DistillerSR tool, a cloud-based literature review software, was used to screen, compile and manage all the identified studies. Two independent reviewers screened the identified studies based on their titles and abstracts against the eligibility criteria. Subsequently, full-text articles were retrieved for full-text screening against eligibility criteria. A third, independent reviewer resolved any uncertainties/conflicts between the two reviewers. The reasons for exclusion are reported in the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram (Fig. 1). DistillerSR was used to extract data from the included studies. Details of study characteristics, patient characteristics, interventions and outcomes of interest were extracted in the data extraction form. Studies with multiple publications were identified and linked to the primary study; all relevant data were extracted under the primary study. Identification and screening of the available literature was performed in accordance with PRISMA statement [15], the Centre for Reviews and Dissemination [16] and the Cochrane Collaboration [17].
Quality Assessment
The quality of the included RCTs was assessed using the quality assessment checklist, in accordance with the recommendations by the Centre for Reviews and Dissemination’s Guidance for Undertaking Reviews in Health Care (NICE, 2019) [18]. The quality of observational studies was assessed using the Newcastle-Ottawa Scale, 2019 [19]. Three factors were considered to score the quality of included observational studies: selection, comparability and outcomes assessment.
Ethical Approval
This article is based on previously conducted studies and does not contain any studies with human participants or animals.
Results
Study Selection
A total of 2628 citations were retrieved after initial search through electronic databases and conference proceedings (Fig. 1). After removing duplicates, 2614 articles were assessed for title-abstract screening. Subsequently, 835 articles were assessed for full-text screening. Overall, 724 records were excluded, and 111 publications, representing 108 unique studies were included in the SLR (Fig. 1).
Study and Patient Characteristics
Of the total 108 included studies, 30 were clinical trials, 74 were observational studies, and 1 was a quasi-experimental study. In three studies the study designs were not clear. The RCTs and observational studies included in this review covered perinatal women across different continents, like America, Europe, Asia, Oceania, Africa and/or multinational.
Details on patient characteristics including maternal age, gestational weight, gestational age at diagnosis and treatment initiation and relevant obstetrical history are given in Tables 1 and 2. Study characteristics are summarized in Supplementary Table 2 and 3, and treatment interventions along with types of insulin utilized by the women diagnosed with GDM or pre-existing diabetes are summarized in Supplementary Tables 4 and 5.
Glycemic Outcomes in People with GDM and Pre-existing Diabetes
Of the 108 included studies, 21 clinical trials and 20 observational studies reported the clinical outcomes of interest (FBG, PPG, glycemic range and glycemic variability) in women with GDM (Table 3). Six clinical trials and 12 observational studies reported the clinical outcomes of interest in women with pre-existing diabetes and mixed population (Table 4).
Evidence from Clinical Trials
In women diagnosed with GDM, majority of the trials compared an insulin regimen [basal only, basal/bolus, or bolus only] to metformin (n = 13) (Table 3). In addition, few trials compared insulin to glibenclamide/glyburide (n = 3), (Table 3). The difference in the glycemic outcomes in women treated with insulin versus other therapies varied across the trials and provided very low-quality of evidence for the outcomes. The study design varied widely across the trials.
FBG was the most reported clinical outcome (n = 22). Some RCTs (n = 3) reported a significantly better (p ≤ 0.01) FBG in the metformin-treated group compared to those with insulin [20,21,22]. Two RCTs by Zawiejska et al. and Khan et al. compared glycemic control in women diagnosed with GDM in response to insulin and metformin and reported significantly better FBG in the insulin-treated groups compared to other therapies (p ≤ 0.01) [23, 24]. Arshad et al. compared insulin with diet therapy and exercise and reported a significantly better FBG in the diet-treated group compared to those treated with insulin [25].
In an RCT by Somani et al. with no differences in glycemic outcomes between the metformin and insulin groups at baseline, higher PPG levels were reported in group treated with insulin compared to those treated with metformin (p = 0.005) [26]. In an RCT by Ji et al. with mixed population, a significant improvement in PPG and time in range (TIR) was observed with insulin detemir compared to insulin neutral protamine Hagedorn (NPH) (p < 0.001) [27].
Evidence from Observational Studies
In women with GDM, most observational studies that reported clinical outcomes of interest compared insulin to diet/MNT (n = 6), metformin (n = 5), combination of metformin and/or diet and/or lifestyle interventions (n = 4). Additionally, other studies reported a comparison between different types of insulin (n = 3), insulin versus no insulin (n = 1) and insulin versus glyburide (n = 1) (Table 3). Five studies showed significant improvement in FBG and PPG among those managed with other therapies compared to the insulin-treated group [28,29,30,31,32] (p < 0.05). These observational studies provide an insight into the real-world use of insulin within this specific population, highlighting that potential barriers of insulin use may be limiting its full benefits in optimizing glycemic control.
Maternal Outcomes in People with GDM and Pre-existing Diabetes
Of the 108 included studies, 18 clinical trials and 44 observational studies reported the maternal outcomes of interest (prevalence of hypoglycemia, cesarean section, preterm labor, hypertension, induced labor and preterm delivery) in women with GDM (Table 5). Maternal outcomes in women with diabetes prior to pregnancy and mixed population were reported in 6 trials and 18 observational studies (Table 6).
Evidence from Clinical Trials
Most trials included in this study had small numbers of participants and no prolonged follow-up after the treatment. Some of the included trials had unclear risk of bias due to lack of blinding, unclear methods of randomization and selective reporting of outcomes. The primary outcomes of interest were different across the included studies.
Most included trials reported no difference in the proportion of cesarean sections among women treated with metformin versus insulin [21, 24, 26, 33,34,35,36,37,38,39]. However, two RCTs by Galal et al. and Hassan et al. reported a significantly higher rate (p ≤ 0.05) of cesarean sections in the insulin-treated group [20, 40], while an RCT by Ijas et al. reported a lower rate of cesarean section in the insulin-treated group versus metformin (p = 0.047) [41]. In three RCTs by Khan et al., Mirzamoradi et al. and Huhtala et al., numerically higher rates of preterm delivery, preeclampsia and induced labor were observed in the insulin-treated group relative to comparator group using oral anti-diabetic agents [24, 42, 43]. Other RCTs by Galal et al., Niromanesh et al. and Hassan et al. reported a numerically higher incidence of preterm delivery and induced labor in the group treated with metformin versus insulin [20, 39, 40]. In women with pre-existing diabetes, an open-label, randomized study by Ainuddin et al. reported a significantly high rate of incidence of pregnancy-induced hypertension in the insulin-treated group compared to only metformin group and metformin and insulin-treated group [44], while an RCT by Ji et al. demonstrated a numerically higher incidence of gestational hypertension in the insulin NPH-treated group compared to the insulin detemir-treated-group [27].
Evidence from Observational Studies
Among women diagnosed with GDM, across different interventions, retrospective analyses revealed that cases of cesarean section and preterm delivery were higher in women managed with insulin than in those managed with other interventions such as diet/MNT, metformin and metformin + insulin [28, 32, 45, 46]. Compared with other interventions, insulin did not show a significant difference in the rate of gestational hypertension and induced labor in women treated with insulin and those managed with lifestyle modification [47, 48] or metformin [49, 50]. In the mixed population, a prospective cohort study by Negrato et al. compared insulin glargine with NPH and reported a significantly higher rate of preeclampsia in the NPH-treated group compared to the glargine-treated group (p < 0.0001) in women diagnosed with diabetes prior to pregnancy [51].
Maternal Hypoglycemia in Clinical Trials and Observational Studies
The overall rate of hypoglycemia in women with GDM and a mixed population was significantly higher in the insulin-treated group compared to metformin and metformin with additional insulin therapy [27, 52, 53]. Contrarily, a significantly lower incidence of hypoglycemia was reported with insulin (p < 0.001) compared to glyburide [54, 55].
Fetal Outcomes in Women with GDM and Pre-existing Diabetes or Mixed Population
Of the 108 included studies, 7 RCTs and 24 observational studies reported fetal outcomes of interest in women with GDM, and 2 trials and 14 observational studies reported fetal outcomes of interest in women diagnosed with diabetes prior to pregnancy and a mixed population (Tables 7, 8). Most of the included studies scored low to moderate on the Newcastle-Ottawa Scale and quality assessment checklist; they had limited power, relatively small sample size, long individual study period and a high drop-out rate.
Evidence from Clinical Trials
A number of studies on women with GDM and pre-existing diabetes reported a numerically higher proportion of LGA in women treated with insulin compared to women treated with metformin [34, 36, 41, 56], with a significant difference (p = 0.001) reported by Eid et al. [34]. In an RCT, Hod et al. compared insulin detemir with NPH in pregnant women diagnosed with diabetes and reported a significantly higher rate of LGA in the group treated with insulin NPH compared to the group treated with insulin detemir [57]. Other RCTs by Ainuddin et al. and Mukopadhyay et al. reported a lower proportion of LGA in women treated with basal/bolus insulin compared to metformin + insulin and glibenclamide, respectively [44, 58]. In another RCT, Somani et al. compared stillbirth in women treated with insulin (regular or NPH or both) versus metformin. This trial reported one case of stillbirth in the insulin-treated group compared to no stillbirth in the metformin group (p = 0.32) [26].
Evidence from Observational Studies
In women diagnosed with GDM, three retrospective cohort studies by Koren et al., Castillo et al. and Hedderson et al. compared insulin versus glyburide and reported no substantial differences in the proportion of LGA in between the treatment groups [55, 59, 60]. However, other retrospective analyses by Simeonova-Krstevska et al., Benhalima et al. and Bogdanet et al. reported a significantly higher proportion of LGA in the insulin-treated group compared to diet/MNT and metformin (p < 0.0001–p < 0.05) [28, 32, 46]. In women diagnosed with diabetes prior to pregnancy, one retrospective database review by Neff et al. reported a significantly higher rate of delivery of LGA in mothers treated with CSII-aspart and NPH compared to those treated using MDI-aspart and NPH (p = 0.03) [61]. Most of the studies did not report stillbirth, with only five studies reporting this outcome. Perinatal mortality among women with pre-existing diabetes was reported in retrospective studies by Bartal et al., Abell et al. and Billionnet et al., and no differences across the treatment arms were observed [48, 62, 63]. However, in a prospective cohort study by Negrato et al., a significantly higher rate of perinatal mortality (p = 0.028) in pregnant women diagnosed with diabetes prior to pregnancy was reported among NPH-treated women compared to those treated with glargine [51].
Discussion
We conducted an SLR that assessed the paradigm of reported insulin use in pregnant women with diabetes, as well as the outcomes, including recommended clinical parameters related to glycemic control as part of their treatment goals and maternal and fetal outcomes. The wide variety in outcomes of interest when comparing insulin use with other anti-diabetic agents across the included studies makes it extremely difficult and potentially misleading to summarize findings and make management recommendations, illustrating the need for standardization of study design with consistent glycemic and maternal/fetal efficacy outcomes to evaluate the use of glucose-lowering medications in pregnancy.
Glycemic outcomes of interest were reported in 27 clinical trials and 32 observational studies. Notably, while 1-h and 2-h PPGs are the recommended treatment goals in patients with GDM, many of the studies captured in this review focused on HbA1c as a primary outcome measure. Furthermore, compared to the non-pregnant population, there are very few well-powered RCTs evaluating insulin use in pregnancy. Ji et al. published a well-designed RCT in 2020 showing that in pregnant women diagnosed with diabetes prior to pregnancy, a significant improvement in PPG and TIR was observed among those treated with detemir compared with insulin NPH as basal insulin. Both groups received the short-acting human insulin three times a day before the meals [27]. These results increase the options for women requiring basal insulin therapy for diabetes management in pregnancy [27]. Use of continuous glucose monitoring (CGM) was also observed to be effective in improving glycemic range metrics in women treated with insulin. However, at the time of this SLR there was limited evidence to draw a conclusive statement on the impact of CGM role in improving glycemic outcomes for diabetes in pregnancy. Overall, there was no clear consensus between the study outcomes and use of various intervention types and regimens. The quality of the included studies was assessed, and they were found to be low on evidence with high risk of bias. Therefore, we could not conclude which intervention type or regimen was best for pregnant women with diabetes.
Maternal outcomes such as hypoglycemia, preeclampsia, cesarean delivery, preterm delivery and induced labor were reported in 18 RCTs, which may be due to the difficulty in collecting these outcome measures. They were reported more frequently in studies designed to compare an insulin regimen to another regimen such as in women treated with insulin versus those treated with metformin, diet/MNT and other anti-diabetic agents [20, 28, 32, 40, 45, 46, 64]. Most of the studies included in this review used insulin therapy as the last option of treatment, after the failure of nutritional therapy or in association with other drug interventions such as metformin and/or sulfonylureas. This suggests that these patients could have had more severe insulin resistance and/or deficiency than the other patients, and this would likely confound glycemic, maternal and fetal outcomes. Heterogeneity was observed across maternal outcomes among the studies, including rates of cesarean delivery, gestational age at delivery and induction of labor. The plausible reason for heterogeneity could be due to various ethnic groups, study designs, treatment requirements and selection criteria.
The most common fetal complication reported across the included studies for any type of diabetes during pregnancy was LGA, confirming that these patients were mostly in hyperglycemic state, a common cause of LGA. Other common neonatal outcomes observed, commonly associated with LGA and the mother’s hyperglycemia, included the rate of complications such as preterm birth and neonatal hypoglycemia. Across studies covered in this review, insulin was associated with fewer cases of LGA only compared with glibenclamide, as observed in a study by Mukopadhyay et al. that compared insulin and glibenclamide for treatment of GDM [58]. In accordance with another meta-analysis, women treated with glibenclamide reported the highest incidence of LGA, preeclampsia, neonatal hypoglycemia and preterm birth; metformin (plus insulin when required) had the lowest risk of macrosomia, pregnancy hypertension, LGA, preterm birth and low birth weight [65]. Overall, there was no clear evidence of the risk of delivery of LGA in those born of mothers with diabetes treated with insulin versus other oral anti-diabetic agents. Based on the current results, it is difficult to make a conclusive affirmation of the most effective form of treatment to reduce incidence of neonatal complications in pregnant women with diabetes.
Across the included studies, treatments with metformin and diet/MNT were associated with better clinical, maternal and fetal outcomes than those treated with insulin therapy. However, the studies did not provide enough evidence on whether insulin can help achieve improved outcomes compared with other therapies. Overall, the quality of the evidence of RCTs ranged from low to moderate, whereas for observational studies the quality ranged from low to good. A variety of methods was used to diagnose GDM in the included studies. Furthermore, it is difficult to draw conclusions about the optimal approach to treatment of diabetes in pregnancy because of inconsistencies in the criteria for management of glucose targets, patient adherence to treatment, clinical outcome measures across studies and lack of long-term safety data.
The current SLR included clinical trials and observational studies with diverse populations and treatment arms. Some studies lacked appropriate sample size, and many studies utilized a variety of methods for diagnosis of GDM. Data on pregnant women diagnosed with diabetes prior to pregnancy were very limited. Furthermore, high-quality studies are needed to identify the optimal treatment regimens for women with diabetes in pregnancy who are treated with insulin.
There were clear limitations to the current SLR. With limited evidence and meta-analyses, the included studies did not provide sufficient evidence to identify clear differences between the various insulin types and regimens. Most of the included studies did not adjust for other potential confounding factors such as maternal age, educational status, income, ethnicity and other factors that might influence the results; therefore, findings should be interpreted with caution. This SLR included clinical trials and observational studies with varied populations and treatment arms. For some studies, sample size was small, and many studies did not report statistical tests for significance. In the included studies, there was no consensus on the types of outcome measures reported in pregnant women with diabetes. Most of the studies reported that there was no evidence of clear-cut benefit of one intervention type or regimen over the other. Hence, no firm conclusions or management recommendations could be made about different insulin types and regimens in pregnant women with diabetes. Future trials are required that are multi-centered, randomized, well-powered and of improved methodological quality with standardization of glycemic and maternal/fetal efficacy outcome measures. Furthermore, more research is warranted with larger groups of pregnant women, with transparent reporting of how the trials were conducted, and that reports clinical, maternal and fetal outcomes.
Conclusion
In summary, the findings of this review were comparable to the existing reviews evaluating treatment of diabetes in pregnancy. There is a tremendous paucity of well-designed RCTs and no consensus for the study design and definition of diabetes in pregnancy in the existing literature. We identified a variety of definitions being used that did not always overlap. We observed that the lack of standard diagnosis also results in a diversity of outcomes that are used in clinical practice to evaluate optimal medical management in pregnant women with diabetes. It would be helpful for the practitioners and patient populations if the outcomes were consistently defined and reported globally. According to the ADA Management of Diabetes in Pregnancy guidelines, the standard treatment goals for pregnant women with diabetes are aimed at maintaining target blood glucose levels (fasting glucose 70–95 mg/dl [3.9–5.3 mmol/l], 1-h postprandial glucose 110–140 mg/dl [6.1–7.8 mmol/l] and/or 2-h postprandial glucose 100–120 mg/dl [5.6–6.7 mmol/l]) to prevent maternal and fetal complications, achieved through stringent glucose monitoring and insulin therapy [11]. However, the universal adoption of these recommendations in the real-world is limited, as we identified in the observational studies analyzed, and some misalignment still exists in randomized clinical trials as well. This makes identifying any real-world association of the effectiveness of insulin in maternal and fetal outcomes difficult. With the increased access to CGM, the collection of glycemic values will increase, and more glycemic outcome data will be generated. However, this will require a more standardized approach, especially without a clear consensus on clinically relevant CGM metrics for GDM and T2D.
Conducting well-designed RCTs to evaluate the efficacy of various insulins or insulin regimens in this unique population remains an area that requires specialized attention. There is a need to be better aligned on clinical endpoints to study pregnant populations to delineate what treatment or therapies unequivocally demonstrate improvement in maternal and neonatal outcomes, especially with introduction of innovative insulin formulations and improved technologies that evaluate glucose management.
References
Metzger BE. Proceedings of the fourth international workshop conference on gestational diabetes mellitus. Diabetes Care. 1998;21(2):B1–167.
Hunt KJ, Schuller KL. The increasing prevalence of diabetes in pregnancy. Obstet Gynecol Clin North Am. 2007;34(2):173–99.
CDC. Diabetes During Pregnancy. Centers for Disease Control and Prevention. 2018. https://www.cdc.gov/diabetes/basics/gestational.html#:~:text=Gestational%20diabetes%20is%20a%20type,pregnancy%20and%20a%20healthy%20baby
Association AD. Gestational diabetes mellitus. Diabetes Care. 2004;27(suppl 1):s88–90.
Tyrala EE. The infant of the diabetic mother. Obstet Gynecol Clin. 1996;23(1):221–41.
Pollex E, Moretti ME, Koren G, Feig DS. Safety of insulin glargine use in pregnancy: a systematic review and meta-analysis. Ann Pharmacother. 2011;45(1):9–16.
Serlin DC, Lash RW. Diagnosis and management of gestational diabetes mellitus. (0002-838X (Print)).
Pantea-Stoian A, Stoica RA, Stefan SD. Insulin therapy in gestational diabetes. Gestational diabetes mellitus—an overview with some recent advances. London: IntechOpen; 2019.
Bulletins-Obstetrics C. ACOG practice bulletin no. 190: gestational diabetes mellitus. Obstet Gynecol. 2018;131(2):e49–64.
Cho N, Shaw J, Karuranga S, Huang YD, da Rocha Fernandes J, Ohlrogge A, et al. IDF Diabetes Atlas: global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res Clin Pract. 2018;138:271–81.
ElSayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, et al. 15. Management of diabetes in pregnancy: standards of care in diabetes—2023. Diabetes Care. 2023;46(Supplement_1):S254–66.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183: 109119.
Wilson LM, Castle JR. Recent advances in insulin therapy. Diabetes Technol Ther. 2020;22(12):929–36.
Oude Rengerink K, Logtenberg S, Hooft L, Bossuyt PM, Mol BW. Pregnant womens’ concerns when invited to a randomized trial: a qualitative case control study. BMC Pregnancy Childbirth. 2015;15(1):1–11.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Dissemination C. Systematic reviews: CRD’s guidance for undertaking reviews in healthcare. York: University of York NHS Centre for Reviews & Dissemination; 2009.
Higgins J. Cochrane handbook for systematic reviews of interventions. Version 5.1. 0 [updated March 2011]. The Cochrane Collaboration. http://www.cochrane-handbook.org. 2011.
NICE. Appendix C: methodology checklist: randomised controlled trials. 2019. https://www.nice.org.uk/process/pmg6/resources/the-guidelines-manual-appendices-bi-2549703709/chapter/appendix-c-methodology-checklist-randomised-controlled-trials. Accessed on Sept 2020.
The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. 2019. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed on Sept 2020.
Galal M, El Bassiou WM, Sherif L. Metformin versus insulin in treatment of gestational diabetes mellitus: a randomized controlled trial. Res J Obstet Gynecol. 2019;12(1):23–7.
Wasim T, Shaukat S, Javaid L, Mukhtar S, Amer WJ. Comparison of metformin and insulin for management of gestational diabetes mellitus: a randomized control trial. Pak J Med Sci. 2019;13:823–7.
Ashoush S, El-Said M, Fathi H, Abdelnaby M. Identification of metformin poor responders, requiring supplemental insulin, during randomization of metformin versus insulin for the control of gestational diabetes mellitus. J Obstet Gynaecol Res. 2016;42(6):640–7.
Zawiejska A, Wender-Ozegowska E, Grewling-Szmit K, Brazert M, Brazert. Short-term antidiabetic treatment with insulin or metformin has a similar impact on the components of metabolic syndrome in women with gestational diabetes mellitus requiring antidiabetic agents: Results of a prospective, randomised study. J Physiol Pharmacol. 2016;67(2):227–33.
Khan R, Mukhtar A, Khawar A. Comparison of metformin with insulin in the management of gestational diabetes. Med Forum Mon. 2017;28(11):105–9.
Arshad R, Karim N, Ara HJ. Effects of insulin on placental, fetal and maternal outcomes in gestational diabetes mellitus. Pak J Med Sci. 2014;30(2):240–4.
Subhash Somani P, Kumar Sahana P, Chaudhuri P, Sengupta N. Treatment of gestational diabetes mellitus: insulin or metformin? J Evol Med Dent Sci. 2016;5(63):4423–9.
Ji J, He Z, Yang Z, Mi Y, Guo N, Zhao H, et al. Comparing the efficacy and safety of insulin detemir versus neutral protamine Hagedorn insulin in treatment of diabetes during pregnancy: a randomized, controlled study. BMJ Open Diabetes Res Care. 2020;8(1).
Simeonova-Krstevska S, Bogoev M, Bogoeva K, Zisovska E, Samardziski I, Velkoska-Nakova V, et al. Maternal and neonatal outcomes in pregnant women with gestational diabetes mellitus treated with diet, metformin or insulin. Open Access Maced J Med Sci. 2018;6(5):803–7.
Ozgu-Erdinc AS, Iskender C, Uygur D, Oksuzoglu A, Seckin KD, Yeral MI, et al. One-hour versus two-hour postprandial blood glucose measurement in women with gestational diabetes mellitus: which is more predictive? Endocrine. 2016;52(3):561–70.
Yanagisawa K, Muraoka M, Takagi K, Ichimura Y, Kambara M, Sato A, et al. Assessment of predictors of insulin therapy in patients with gestational diabetes diagnosed according to the IADPSG criteria. Diabetol Int. 2016;7(4):440–6.
Tang L, Xu S, Li P, Li L. Predictors of insulin treatment during pregnancy and abnormal postpartum glucose metabolism in patients with gestational diabetes mellitus. Diabetes Metab Syndr Obes. 2019;12:2655–65.
Benhalima K, Robyns K, Van Crombrugge P, Deprez N, Seynhave B, Devlieger R, et al. Differences in pregnancy outcomes and characteristics between insulin- and diet-treated women with gestational diabetes. BMC Pregnancy Childbirth. 2015;15:271.
Ghomian N, Vahed SHM, Firouz S, Yaghoubi MA, Mohebbi M, Sahebkar A. The efficacy of metformin compared with insulin in regulating blood glucose levels during gestational diabetes mellitus: a randomized clinical trial. J Cell Physiol. 2019;234(4):4695–701.
Eid SR, Moustafa RSI, Salah MM, Hanafy SK, Aly RH, Mostafa WFG, et al. Is metformin a viable alternative to insulin in the treatment of gestational diabetes mellitus (GDM)? Comparison of maternal and neonatal outcomes. Egypt Pediatr Assoc Gazette. 2018;66(1):15–21.
Hamadani A, Zahid S, Butt ZB. Metformin versus insulin treatment in gestational diabetes in pregnancy and their effects on neonatal birthweight. Pak J Med Sci. 2017;11:914–6.
Ainuddin J, Karim N, Hasan AA, Naqvi SA. Metformin versus insulin treatment in gestational diabetes in pregnancy in a developing country: a randomized control trial. Diabetes Res Clin Pract. 2015;107(2):290–9.
Ruholamin S, Eshaghian S, Allame Z. Neonatal outcomes in women with gestational diabetes mellitus treated with metformin in compare with insulin: a randomized clinical trial. J Res Med Sci. 2014;19(10):970.
Tertti K, Ekblad U, Koskinen P, Vahlberg T, Ronnemaa T. Metformin vs. insulin in gestational diabetes. A randomized study characterizing metformin patients needing additional insulin. Diabetes Obes Metab. 2013;15(3):246–51.
Niromanesh S, Alavi A, Sharbaf FR, Amjadi N, Moosavi S, Akbari S. Metformin compared with insulin in the management of gestational diabetes mellitus: a randomized clinical trial. Diabetes Res Clin Pract. 2012;98(3):422–9.
Hassan JA, Karim N, Sheikh Z. Metformin prevents macrosomia and neonatal morbidity in gestational diabetes. J Pak J Med Sci. 2012;28(3):384–9.
Ijas H, Vaarasmaki M, Morin-Papunen L, Keravuo R, Ebeling T, Saarela T, et al. Metformin should be considered in the treatment of gestational diabetes: a prospective randomised study. BJOG. 2011;118(7):880–5.
Mirzamoradi M, Heidar Z, Faalpoor Z, Naeiji Z, Jamali R. Comparison of glyburide and insulin in women with gestational diabetes mellitus and associated perinatal outcome: a randomized clinical trial. Acta Med Iran. 2015;53:97–103.
Huhtala MS, Tertti K, Pellonpera O, Ronnemaa T. Amino acid profile in women with gestational diabetes mellitus treated with metformin or insulin. Diabetes Res Clin Pract. 2018;146:8–17.
Ainuddin JA, Karim N, Zaheer S, Ali SS, Hasan AA. Metformin treatment in type 2 diabetes in pregnancy: an active controlled, parallel-group, randomized, open label study in patients with type 2 diabetes in pregnancy. J Diabetes Res. 2015;2015: 325851.
Varghese R, Thomas B, Hail MA, Rauf A, Sadi MA, Sualiti AA, et al. The prevalence, risk factors, maternal and fetal outcomes in gestational diabetes mellitus. J Int J Drug Dev Res. 2012;4(3):356–68.
Bogdanet D, Egan A, Reddin C, Kirwan B, Carmody L, Dunne F. ATLANTIC DIP: despite insulin therapy in women with IADPSG diagnosed GDM, desired pregnancy outcomes are still not achieved. What are we missing? Diabetes Res Clin Pract. 2018;136:116–23.
Donovan LE, Boyle SL, McNeil DA, Pedersen SD, Dean SR, Wood S, et al. Label of gestational diabetes mellitus affects caesarean section and neonatal intensive care unit admission without conventional indications. Can J Diabetes. 2012;36(2):58–63.
Fishel Bartal M, Ward C, Refuerzo JS, Ashimi SS, Joycelyn CA, Chen HY, et al. Basal insulin analogs versus neutral protamine Hagedorn for type 2 diabetics. Am J Perinatol. 2020;37(1):30–6.
Landi SN, Radke S, Boggess K, Engel SM, Sturmer T, Howe AS, et al. Comparative effectiveness of metformin versus insulin for gestational diabetes in New Zealand. Pharmacoepidemiol Drug Saf. 2019;28(12):1609–19.
Morais Rodrigues I, Figueiredo A, Pereira N, Amaral N, Pratas S, Valadas C, et al. Metformin as a safe option to insulin in gestational diabetes mellitus: a retrospective study. SN Compr Clin Med. 2020;2(3):272–7.
Negrato CA, Rafacho A, Negrato G, Teixeira MF, Araujo CA, Vieira L, et al. Glargine vs. NPH insulin therapy in pregnancies complicated by diabetes: an observational cohort study. Diabetes Res Clin Pract. 2010;89(1):46–51.
Hickman MA, McBride R, Boggess KA, Strauss R. Metformin compared with insulin in the treatment of pregnant women with overt diabetes: a randomized controlled trial. Am J Perinatol. 2013;30(6):483–90.
Garcia-Dominguez M, Herranz L, Hillman N, Martin-Vaquero P, Janez M, Moya-Chimenti E, et al. Use of insulin lispro during pregnancy in women with pregestational diabetes mellitus. Med Clin (Barc). 2011;137(13):581–6.
Senat MV, Affres H, Letourneau A, Coustols-Valat M, Cazaubiel M, Legardeur H, et al. Effect of glyburide vs subcutaneous insulin on perinatal complications among women with gestational diabetes: a randomized clinical trial. JAMA. 2018;319(17):1773–80.
Koren R, Ashwal E, Hod M, Toledano Y. Insulin detemir versus glyburide in women with gestational diabetes mellitus. Gynecol Endocrinol. 2016;32(11):916–9.
Mesdaghinia E, Samimi M, Homaei Z, Saberi F, Moosavi SGA, Yaribakht M. Comparison of newborn outcomes in women with gestational diabetes mellitus treated with metformin or insulin: a randomised blinded trial. Int J Prev Med. 2013;4(3):327.
Hod M, Mathiesen ER, Jovanovic L, McCance DR, Ivanisevic M, Duran-Garcia S, et al. A randomized trial comparing perinatal outcomes using insulin detemir or neutral protamine Hagedorn in type 1 diabetes. J Matern Fetal Neonatal Med. 2014;27(1):7–13.
Mukhopadhyay P, Bag TS, Kyal A, Saha DP, Khalid N. Oral hypoglycemic glibenclamide: can it be a substitute to insulin in the management of gestational diabetes mellitus? A comparative study. J South Asian Fed Obstet Gynaecol. 2012;4(1):28–31.
Camelo Castillo W, Boggess K, Sturmer T, Brookhart MA, Benjamin DK Jr, Jonsson FM. Association of adverse pregnancy outcomes with glyburide vs insulin in women with gestational diabetes. JAMA Pediatr. 2015;169(5):452–8.
Hedderson MM, Xu F, Neugebauer R, Ferrara A. editors. Glyburide versus insulin for the treatment of women with gestational diabetes in Kaiser Permanente Northern California. In: Pharmacoepodemiology and drug safety. Hoboken: Wiley; 2018.
Neff KJ, Forde R, Gavin C, Byrne MM, Firth RG, Daly S, et al. Pre-pregnancy care and pregnancy outcomes in type 1 diabetes mellitus: a comparison of continuous subcutaneous insulin infusion and multiple daily injection therapy. Ir J Med Sci. 2014;183(3):397–403.
Abell SK, Suen M, Pease A, Boyle JA, Soldatos G, Regan J, et al. Pregnancy outcomes and insulin requirements in women with type 1 diabetes treated with continuous subcutaneous insulin infusion and multiple daily injections: cohort study. Diabetes Technol Ther. 2017;19(5):280–7.
Billionnet C, Mitanchez D, Weill A, Nizard J, Alla F, Hartemann A, et al. Gestational diabetes and adverse perinatal outcomes from 716,152 births in France in 2012. Diabetologia. 2017;60(4):636–44.
Koivunen S, Kajantie E, Torkki A, Bloigu A, Gissler M, Pouta A, et al. The changing face of gestational diabetes: the effect of the shift from risk factor-based to comprehensive screening. Eur J Endocrinol. 2015;173(5):623–32.
Liang H-L, Ma S-J, Xiao Y-N, Tan H-Z. Comparative efficacy and safety of oral antidiabetic drugs and insulin in treating gestational diabetes mellitus: an updated PRISMA-compliant network meta-analysis. Medicine. 2017;96(38):e7939.
Das V, Priyanka Y, Smriti A, Anjoo A, Namrata K. Oral/free communication session abstracts. 2018;143(S3):158–542.
Behrashi M, Samimi M, Ghasemi T, Saberi F, Atoof F. Comparison of glibenclamide and insulin on neonatal outcomes in pregnant women with gestational diabetes. Int J Prev Med. 2016;7:88–88.
Spaulonci CP, Bernardes LS, Trindade TC, Zugaib M, Francisco RP. Randomized trial of metformin vs insulin in the management of gestational diabetes. Am J Obstet Gynecol. 2013;209(1):34 (e31–37).
Balaji V, Balaji MS, Alexander C, et al. Premixed insulin aspart 30 (BIAsp 30) versus premixed human insulin 30 (BHI 30) in gestational diabetes mellitus: a randomized open-label controlled study. Gynecol Endocrinol. 2012;28(7):529–32.
Herrera KM, Rosenn BM, Foroutan J, et al. Randomized controlled trial of insulin detemir versus NPH for the treatment of pregnant women with diabetes. Am J Obstet Gynecol. 2015;213(3):426 (e421–427).
Refuerzo JS, Gowen R, Pedroza C, Hutchinson M, Blackwell SC, Ramin S. A pilot randomized, controlled trial of metformin versus insulin in women with type 2 diabetes mellitus during pregnancy. Am J Perinatol. 2015;30(2):163–70.
Han D, Lu B, Pang Z. Efficacy of metformin combined with insulin lispro on gestational diabetes and effects on serum miR-16. Int J Clin Exp Med. 2020;13(3):1728–35.
Krishnakumar S, Govindarajulu Y, Vishwanath U, Nagasubramanian VR, Palani T. Impact of patient education on KAP, medication adherence and therapeutic outcomes of metformin versus insulin therapy in patients with gestational diabetes: a hospital based pilot study in South India. Diabetes Metab Syndr. 2020;14(5):1379–83.
Osuagwu UL, Fuka F, Agho K, Khan A, Simmons D. Adverse maternal outcomes of Fijian women with gestational diabetes mellitus and the associated risk factors. Reprod Sci. 2020;27(11):2029–37.
Zaharieva D, Krishnamurthy B, Teng J, et al. Assessment of glycaemia by fingerstick blood glucose monitoring may underestimate the requirement for insulin to address elevated nocturnal glucose levels in women with GDM. Paper presented at: Diabetes Technology and Therapeutics, 2020.
Cade TJ, Polyakov A, Brennecke SP. Implications of the introduction of new criteria for the diagnosis of gestational diabetes: a health outcome and cost of care analysis. BMJ Open. 2019;9(1): e023293.
Meghelli L, Vambergue A, Drumez E, Deruelle P. Complications of pregnancy in morbidly obese patients: what is the impact of gestational diabetes mellitus? J Gynecol Obstet Hum Reprod. 2020;49(1): 101628.
Munn AJ, Hersh AR, Vinson AR, Brennan TD, Valent AM, Caughey AB. 492: Neonatal outcomes in gestational diabetes managed with insulin vs. glyburide therapy: a cost-effectiveness analysis. Am J Obstet Gynecol. 2019;220(1):S330.
Ng A, Liu A, Nanan R. Association between insulin and post-caesarean resuscitation rates in infants of women with GDM: a retrospective study. J Diabetes. 2019;12(2):151–7.
Christian SJ, Boama V, Satti H, et al. Metformin or insulin: logical treatment in women with gestational diabetes in the Middle East, our experience. BMC Res Notes. 2018;11(1):426.
Leung A, Yu G, Smith L. 993: Adverse pregnancy outcomes with glyburide vs insulin among patients with gestational diabetes established by the International Association of Diabetes and Pregnancy Study Group (IADPSG). Am J Obstet Gynecol. 2018;218(1):S586.
McGrath RT, Glastras SJ, Scott ES, Hocking SL, Fulcher GR. Outcomes for women with gestational diabetes treated with metformin: a retrospective, case–control study. J Clin Med. 2018;7(3):50.
Meregaglia M, Dainelli L, Banks H, Benedetto C, Detzel P, Fattore G. The short-term economic burden of gestational diabetes mellitus in Italy. BMC Pregnancy Childbirth. 2018;18(1):58.
Patanjali CP, Ayyar V, Bantwal G, George B, Perumal N. Maternal and neonatal outcomes in gestational diabetes treated with metformin. Indian J Endocrinol Metab. 2018;22:S44 (ESICON 2018).
Rowan JA, Rush EC, Plank LD, et al. Metformin in gestational diabetes: the offspring follow-up (MiG TOFU): body composition and metabolic outcomes at 7–9 years of age. BMJ Open Diabetes Res Care. 2018;6(1): e000456.
Vanlalhruaii, Dasgupta R, Ramachandran R, et al. How safe is metformin when initiated in early pregnancy? A retrospective 5-year study of pregnant women with gestational diabetes mellitus from India. Diabetes Res Clin Pract. 2018;137:47–55.
Bowker SL, Savu A, Yeung RO, Johnson JA, Ryan EA, Kaul P. Patterns of glucose-lowering therapies and neonatal outcomes in the treatment of gestational diabetes in Canada, 2009–2014. Diabet Med. 2017;34(9):1296–302.
Gibbons A, Flatley C, Kumar S. Cerebroplacental ratio in pregnancies complicated by gestational diabetes mellitus. Ultrasound Obstet Gynecol. 2017;50(2):200–6.
Olmos PR, Borzone GR. Basal-bolus insulin therapy reduces maternal triglycerides in gestational diabetes without modifying cholesteryl ester transfer protein activity. J Obstet Gynaecol Res. 2017;43(9):1397–404.
Xie J, Dai L, Tang X. The comparison of the safety and effectiveness of multiple insulin injections and insulin pump therapy in treating gestational diabetes. Biomed Res. 2017;28(18):7830–3.
Fazel-Sarjoui Z, Namin AK, Kamali M, Namin NK, Tajik A. Complications in neonates of mothers with gestational diabetes mellitus receiving insulin therapy versus dietary regime. Int J Reprod BioMed. 2016;14(4):275.
Ito Y, Shibuya M, Hosokawa S, et al. Indicators of the need for insulin treatment and the effect of treatment for gestational diabetes on pregnancy outcomes in Japan. Endocr J. 2016;63(3):231–7.
Koning SH, Hoogenberg K, Scheuneman KA, et al. Neonatal and obstetric outcomes in diet- and insulin-treated women with gestational diabetes mellitus: a retrospective study. BMC Endocr Disord. 2016;16(1):52.
Saleem N, Godman B, Hussain S. Comparing twice-versus four-times daily insulin in mothers with gestational diabetes in Pakistan and its implications. J Comp Effect Res. 2016;5(5):453–9.
Watanabe M, Katayama A, Kagawa H, Ogawa D, Wada J. Risk factors for the requirement of antenatal insulin treatment in gestational diabetes mellitus. J Diabetes Res. 2016;2016:9648798.
Cosson E, Bihan H, Reach G, Vittaz L, Carbillon L, Valensi P. Psychosocial deprivation in women with gestational diabetes mellitus is associated with poor fetomaternal prognoses: an observational study. BMJ Open. 2015;5(3): e007120.
Inocêncio G, Braga A, Lima T, et al. Which factors influence the type of delivery and cesarean section rate in women with gestational diabetes? J Reprod Med. 2015;60(11–12):529–34.
Kopec JA, Ogonowski J, Rahman MM, Miazgowski T. Patient-reported outcomes in women with gestational diabetes: a longitudinal study. Int J Behav Med. 2015;22(2):206–13.
You JY, Choi SJ, Roh CR, Kim JH, Oh SY. Pregnancy and neonatal outcomes in gestational diabetes treated with regular insulin or fast-acting insulin analogues. Gynecol Obstet Invest. 2016;81(3):232–7.
Deepaklal M, Joseph K, Kurian R, Thakkar NA. Efficacy of insulin lispro in improving glycemic control in gestational diabetes. Indian J Endocrinol Metab. 2014;18(4):491.
Konig AB, Junginger S, Reusch J, Louwen F, Badenhoop K. Gestational diabetes outcome in a single center study: higher BMI in children after six months. Horm Metab Res. 2014;46(11):804–9.
Marques P, Carvalho MR, Pinto L, Guerra S. Metformin safety in the management of gestational diabetes. Endocr Pract. 2014;20(10):1022–31.
Al-Rubeaan KA, Youssef AM, Subhani SN, Ahmad NA, Al-Sharqawi AH, Ibrahim HM. A web-based interactive diabetes registry for health care management and planning in Saudi Arabia. J Med Internet Res. 2013;15(9):e202
Hernandez-Rivas E, Flores-Le Roux JA, Benaiges D, et al. Gestational diabetes in a multiethnic population of Spain: clinical characteristics and perinatal outcomes. Diabetes Res Clin Pract. 2013;100(2):215–21.
Latif L, Hyer S, Shehata H. Metformin effects on treatment satisfaction and quality of life in gestational diabetes. Br J Diabetes Vasc Dis. 2013;13(4):178–82.
Tempe A, Mayanglambam RD. Glyburide as treatment option for gestational diabetes mellitus. J Obstet Gynaecol Res. 2013;39(6):1147–52.
Cheng YW, Chung JH, Block-Kurbisch I, Inturrisi M, Caughey AB. Treatment of gestational diabetes mellitus: glyburide compared to subcutaneous insulin therapy and associated perinatal outcomes. J Matern Fetal Neonatal Med. 2012;25(4):379–84.
Thomas N, Chinta AJ, Sridhar S, Kumar M, Kuruvilla KA, Jana AK. Perinatal outcome of infants born to diabetic mothers in a developing country-comparison of insulin and oral hypoglycemic agents. Indian Pediatr. 2013;50(3):289–93.
Goh JE, Sadler L, Rowan J. Metformin for gestational diabetes in routine clinical practice. Diabet Med. 2011;28(9):1082–7.
Wong VW, Jalaludin B. Gestational diabetes mellitus: who requires insulin therapy? Aust NZ J Obstet Gynaecol. 2011;51(5):432–6.
Flores-Le Roux JA, Chillaron JJ, Goday A, et al. Peripartum metabolic control in gestational diabetes. Am J Obstet Gynecol. 2010;202(6):568 (e561–566).
Demasio KA, Richley M. 434: Neonatal hypoglycemia; does basal insulin choice matter? Am J Obstet Gynecol. 2020;222(1):S285.
Kong L, Nilsson IAK, Gissler M, Lavebratt C. Associations of Maternal Diabetes and Body Mass Index With Offspring Birth Weight and Prematurity. JAMA Pediatr. 2019;173(4):371–78.
Mathiesen E, Alibegovic A, Husemoen L, et al. Risk of major congenital malformations, perinatal or neonatal death with insulin detemir vs other basal insulins in pregnant women with pre-existing diabetes: EVOLVE study. Paper presented at: Diabetologia 2020.
Sperling M, Bentley J, Girsen A, et al. 759: Comparing insulin, metformin, and glyburide in treating diabetes in pregnancy and analyzing obstetric outcomes. Am J Obstet Gynecol. 2020;222(1):S481.
Alexander LD, Tomlinson G, Feig DS. Predictors of large-for-gestational-age birthweight among pregnant women with type 1 and type 2 diabetes: a retrospective cohort study. Can J Diabetes. 2019;43(8):560–6.
Christman L, Piszczek J, Magee M, Ferris L, Duong J, Farley D. Patients with diabetes mellitus managed with insulin detemir: hospital outcomes [18E]. Obstet Gynecol. 2019;133:56S.
Sleeman A, Odom J, Schellinger M. Comparison of hypoglycemia and safety outcomes with long-acting insulins versus insulin NPH in pregestational and gestational diabetes. Ann Pharmacother. 2020;54(7):669–75.
Smrz S, Finneran MM, Landon MB, Gabbe SG. Difference in glycemic profile with the pump vs multiple daily injections in treating type 1 diabetes in pregnancy [32F]. Obstet Gynecol. 2019;133:70S-71S.
Vasquez BA, Sarumi M, Shultz L, Bedell J, Gherman R, Johnson MJ. Glycemic efficacy with U-500 insulin in pregnancy: a retrospective cross-over study [21K]. Obstet Gynecol. 2019;133:123S.
Gupta S, Gupta K, Gathe S, Bamhra P, Gupta S. Insulin therapy in women with pregestational type 2 diabetes and its relevance to maternal and neonatal complications. Int J Diabetes Dev Ctries. 2018;38(1):47–54.
Sunjaya AF, Sunjaya AP. Comparing outcomes of nutrition therapy, insulin and oral anti-diabetics in managing diabetes mellitus in pregnancy: retrospective study and review of current guidelines. Diabetes Metab Syndr. 2019;13(1):104–9.
Stanirowski PJ, Szukiewicz D, Pyzlak M, Abdalla N, Sawicki W, Cendrowski K. Impact of pre-gestational and gestational diabetes mellitus on the expression of glucose transporters GLUT-1, GLUT-4 and GLUT-9 in human term placenta. Endocrine. 2017;55(3):799–808.
Dalfra MG, Soldato A, Moghetti P, et al. Diabetic pregnancy outcomes in mothers treated with basal insulin lispro protamine suspension or NPH insulin: a multicenter retrospective Italian study. J Matern Fetal Neonatal Med. 2016;29(7):1061–5.
Becquet O, El Khabbaz F, Alberti C, et al. Insulin treatment of maternal diabetes mellitus and respiratory outcome in late-preterm and term singletons. BMJ Open. 2015;5(6): e008192.
Colatrella A, Visalli N, Abbruzzese S, Leotta S, Bongiovanni M, Napoli A. Comparison of insulin lispro protamine suspension with NPH insulin in pregnant women with type 2 and gestational diabetes mellitus: maternal and perinatal outcomes. Int J Endocrinol. 2013;2013: 151975.
Fresa R, Visalli N, Di Blasi V, et al. Experiences of continuous subcutaneous insulin infusion in pregnant women with type 1 diabetes during delivery from four Italian centers: a retrospective observational study. Diabetes Technol Ther. 2013;15(4):328–34.
Bruttomesso D, Bonomo M, Costa S, et al. Type 1 diabetes control and pregnancy outcomes in women treated with continuous subcutaneous insulin infusion (CSII) or with insulin glargine and multiple daily injections of rapid-acting insulin analogues (glargine-MDI). Diabetes Metab. 2011;37(5):426–31.
Medical Writing and Editorial Assistance
Medical writing and editorial assistance was provided by Mythili Ananth and Era Seth, employees of Eli Lilly Services India Private Limited.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
This research and the journal’s Rapid Service Fee was funded by Eli Lilly and Company, Indianapolis, IN.
Author information
Authors and Affiliations
Contributions
Beatrice Osumili, Theophilus Lakiang, Carolina Piras De Oliveira, and Kristin Castorino contributed to the conception and design of the study. Beatrice Osumili, Theophilus Lakiang, Carolina Piras De Oliveira, and Kushal Kumar Banerjee were involved in data collection. All authors Goldyn contributed to the interpretation of study results, provided critical revisions, and have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Beatrice Osumili, Kushal Kumar Banerjee, Andrea Goldyn, and Carolina Piras De Oliveira are full-time employees and shareholders of Eli Lilly and Company. Theophilus Lakiang was an employee of Eli Lilly and Company at the time this research was conducted and is currently an employee of GE Healthcare. Kristin Castorino receives research support provided to her institution from Dexcom, Abbott, Medtronic, Novonordisk, Ely Lilly, and Insulet and consulting fees from Dexcom. Theophilus Lakiang: Author affiliation has changed since the time this research was conducted. Assigned affiliation is the institution of employment at the time this research was conducted.
Ethical Approval
This article is based on previously conducted studies and does not contain any studies with human participants or animals.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Castorino, K., Osumili, B., Lakiang, T. et al. Insulin Use During Gestational and Pre-existing Diabetes in Pregnancy: A Systematic Review of Study Design. Diabetes Ther 15, 929–1045 (2024). https://doi.org/10.1007/s13300-024-01541-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-024-01541-6