Abstract
Introduction
Maternal height has been shown to be associated with adverse outcomes in women with gestational diabetes mellitus (GDM). The aim of this study is to evaluate the association between maternal height and adverse outcomes stratified for gestational weight gain (GWG) and pre-pregnancy body mass index (BMI) in women with GDM.
Methods
We conducted a retrospective study that included 2048 women diagnosed with GDM during 24–28 gestational weeks from July 1, 2017, to June 30, 2018, in Zhejiang Province, China. Demographic data, maternal characteristics and pregnancy complications were extracted from medical records. Maternal height was divided into three categories by tertiles. Chi-square was used to evaluate categorical data while one-way ANOVA was utilized to analyze continuous variables. The relationship between maternal height and adverse outcomes was examined using logistic regression.
Results
We found that shorter women had higher rates of low birth weight (LBW) (p = 0.003) and primary cesarean section (primary CS) (p < 0.001) while taller women had higher rates of abnormal neonatal ponderal index (p < 0.001), postpartum hemorrhage (p = 0.044) and macrosomia (p < 0.001). In taller women who had excess GWG, maternal height was positively associated with the risk of macrosomia (aOR 1.97, 95% CI 0.95–4.10). In shorter women who had inadequate GWG, maternal height was significantly associated with LBW (aOR 2.20, 95% CI 1.13–4.29) and primary CS (aOR 2.08, 95% CI 1.38–3.12). Maternal height was a protective factor of postpartum hemorrhage (aOR 0.15, 95% CI 0.03–0.72) in shorter women with excess GWG. In women with normal pre-pregnancy BMI, maternal height was positively associated with LBW (aOR 2.00, 95% CI 1.15–3.49) and primary CS (aOR 1.71, 95% CI 1.28–2.28) in shorter women while it was negatively associated with the risk of abnormal neonatal ponderal index in both shorter and taller women compared to average height women (aOR 0.71, 95% CI 0.55–0.92; aOR 0.66, 95% CI 0.51–0.85).
Conclusion
The association between maternal height and adverse pregnancy outcomes varies with pre-pregnancy BMI and GWG in GDM women. Taking maternal height, pre-pregnancy BMI and GWG into account and using personalized prenatal management may reduce the risk of adverse pregnancy outcomes in GDM.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
It has been reported that maternal height is significantly associated with increased risk of GDM and GDM-related adverse outcomes. We aim to evaluate association between maternal height and adverse outcomes stratified for gestational weight gain (GWG) and pre-pregnancy body mass index (BMI) in women with GDM. |
What was learned from the study? |
The association between maternal height and adverse pregnancy outcomes including low birth weight (LBW), primary CS, macrosomia, abnormal neonatal ponderal index and postpartum hemorrhage varies with prepregnancy BMI and GWG in GDM women. Our results provide evidence for prenatal management in consideration of maternal height by pre-pregnancy BMI and GWG to prevent adverse pregnancy outcomes in GDM women. |
Introduction
Gestational diabetes mellitus (GDM) is glucose intolerance that occurs for the first time during pregnancy [1]. Globally, the prevalence of GDM is rising, and its deleterious consequences, including pregnancy-induced hypertension, macrosomia, preterm birth, and maternal and fetal metabolic disorders, have a serious negative impact on public health [2]. The mode of delivery and adverse pregnancy outcomes have long been related to height, weight, and other anthropometric parameters. Preterm birth, hypertension, fetal growth restriction, and cesarean delivery have all been independently associated with short height [2,3,4].
Height, weight and other anthropometric measurements have long been related to mode of delivery and pregnancy complications. Short stature was found to be an independent risk factor for cesarean delivery, preterm birth, preeclampsia and fetal growth restriction [5,6,7], whereas being taller was found to be a significant risk factor for macrosomia [8,9,10]. Maternal height has been reported to be significantly associated with increased risk of GDM and GDM-related adverse outcomes [4, 8, 9]. These findings suggest that maternal height may play an important role in predicting adverse outcomes in women with GDM.
It is also important to note that gestational weight gain (GWG) and pre-pregnancy BMI have independent effects on pregnancy outcomes in GDM [11]. GWG has been reported to have a significant relationship with large gestational age (LGA) in women with GDM [12]. Moreover, a study showed that shorter women with pre-pregnancy obese body mass index (BMI) had three times higher risk of macrosomia compared to shorter women with normal or overweight pre-pregnancy BMI [13]. Therefore, when determining the effect of maternal height on pregnancy outcomes in women with GDM, it is reasonable to consider pre-pregnancy BMI and GWG.
Given this background, the goal of our study is to evaluate the association between maternal height and adverse outcomes in different pre-pregnancy BMI and GWG groups. Findings from this study may help identify Chinese women with GDM at higher risk of adverse outcomes.
Methods
Study Design and Population
This retrospective study included 2639 women with singleton pregnancy and GDM who were diagnosed using a 75 g oral glucose tolerance test (OGTT) at 24–28 gestational weeks. Women who received prenatal care and gave birth to a livebirth singleton of > 28 gestational weeks at Women’s Hospital, Zhejiang University School of Medicine, from July 1, 2017, to June 30, 2018, in Zhejiang Province, China were included. Relevant information about pregnant women including age, height, weight before pregnancy (within 1 month before pregnancy), weight gain during pregnancy, gravidity, parity, OGTT levels, glycated hemoglobin (HbA1c), mode of delivery, gestational week of delivery, neonatal birth weight, pregnancy complications such as macrosomia, pregnancy-induced hypertension (PIH, including gestational hypertension, preeclampsia, eclampsia) and postpartum hemorrhage was obtained from medical records. Women with previous history of diabetes mellitus, overt diabetes, chronic illnesses (hypertension, diseases of the liver, kidney, heart, lung and other major organs), autoimmune conditions (Sjogren’s syndrome, anticardiolipin syndrome, myasthenia gravis), tumors or autoimmune diseases and women with missing medical records were excluded. A total of 2048 women with GDM were included in this study (Fig. 1). This study was approved by the Human Ethics Committee at Women’s Hospital, School of Medicine, Zhejiang University (IRB-20210269-R), and all participants signed the informed consent form. This study was performed in accordance with the Helsinki Declaration.
Diagnostic Criteria
GDM
According to International Association of Diabetes and Pregnancy Study Group (IADPSG) standards, GDM was identified using a 75 g OGTT with cutoff values of 5.1 mmol/l for fasting plasma glucose (FPG), 10.0 mmol/l for 1 h-postprandial glucose (1 h-PG) and 8.5 mmol/l for 2 h-PG. At 24–28 gestational weeks, OGTT and HbA1c tests were conducted in the morning following an overnight fast of at least 8 h.
Maternal Anthropometry
Maternal weight was measured in kilograms (kg), and maternal height was measured in centimeters (cm). Maternal height and weight were self-reported. Pre-pregnancy BMI was calculated as pre-pregnancy weight in kilograms (kg) divided by the square of height in meters(m). Pre-pregnancy BMI was categorized into underweight (< 18.5 kg/m2), normal weight (18.5–24.9 kg/m2), overweight (25.0–29.9 kg/m2) and obese (≥ 30.0 kg/m2). GWG was the difference between pre-delivery weight and pre-pregnancy weight. According to the standard definition of IOM guidelines in 2009 [14], appropriate GWG was 12.5–18.0 kg for underweight BMI, 11.5–16.0 kg for normal BMI, 7.0–11.5 kg for overweight and 5.0–9.0 kg for obesity, respectively. GWG below the thresholds was defined as inadequate GWG, while exceeding the thresholds was defined as excessive GWG.
Adverse Outcomes
Newborns with gestational age ≥ 28 weeks but < 37 weeks were considered preterm neonates. Newborns with birth weight ≥ 4000 g were defined as having macrosomia while those < 2500 g were defined as having low birth weight (LBW) [15]. LGA was defined as neonate birth weight > 90th percentile based on national population references for age and sex. PIH was diagnosed in women with no previous history of hypertension with systolic blood pressure (SBP) ≥ 140 mmHg and diastolic blood pressure (DBP) ≥ 90 mmHg on two occasions at least 4 h apart after 20 gestational weeks with or without proteinuria [16]. Primary cesarean section (CS) was defined as cesarean section performed on women with no previous history of cesarean delivery. Postpartum hemorrhage was defined as blood loss ≥ 500 ml after vaginal delivery or ≥ 1000 ml after cesarean section [17]. The ponderal index was determined by the ratio of birth weight to birth length (birth weight [kg] /length [m3]), and abnormal neonatal ponderal index was defined as < 10th percentile or > 90th percentile [18].
Statistical Analysis
Maternal and neonatal demographic and clinical features were reported as frequency (%) or mean (SD). Continuous variables were analyzed using one-way ANOVA while categorical variables (maternal age groups, parity, gravidity, pre-pregnancy BMI groups, GWG groups, adverse pregnancy outcomes) were analyzed using chi-square test. Maternal height was divided into three different categories by tertiles: shorter: ≤ 158.0 cm, average: (158.1–162.0 cm) and taller: > 162.0 cm [19]. The relationship between maternal height and adverse outcomes in different pre-pregnancy BMI groups and GWG groups was analyzed using logistic regression. Two-sided p values < 0.05 were considered significant. Statistical analyses were done with SPSS 26.0.
Results
General Characteristics and Incidence of Adverse Outcomes Among Maternal Height Categories
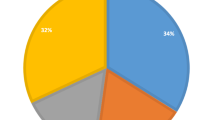
There were differences in GWG (p = 0.006), pre-pregnancy weight (p = 0.001), birthweight (p = 0.001), birth length (p < 0.001) and neonatal ponderal index (p < 0.001) among maternal height categories. We also noted no difference in pre-pregnancy BMI, maternal age, parity, HbA1c, fasting plasma glucose, 1 h-PG or 2 h-PG among maternal height categories. We found differences in the incidence of abnormal neonatal ponderal index, macrosomia, postpartum hemorrhage, primary CS and LBW among height categories. Women with shorter stature had higher rates of LBW (p = 0.003) and primary CS (p < 0.001). Taller women had higher rates of abnormal neonatal ponderal index (p < 0.001), postpartum hemorrhage (p = 0.044) and macrosomia (p < 0.001). The incidence of preterm birth did not significantly differ among maternal height categories (p = 0.136) (Table 1).
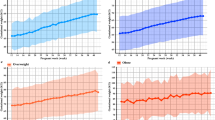
Association Between Maternal Height and Adverse Outcomes Stratified for GWG
Maternal height was positively associated with the risk of macrosomia in taller women who gained excess GWG compared to average height women who gained excess GWG (aOR 1.97, 95% CI 0.95–4.10). Maternal height was negatively associated with postpartum hemorrhage in shorter women who gained excess GWG compared to average height women who had excess GWG (aOR 0.15, 95% CI 0.03–0.72). Maternal height was associated with an increased risk of LBW (aOR 2.20, 95% CI 1.13–4.29) and primary CS (aOR 2.08, 95% CI 1.38–3.12) among shorter women who gained inadequate gestational weight compared to average height women with inadequate GWG. In women who gained adequate GWG, maternal height was negatively associated with the risk of abnormal neonatal ponderal index in both shorter and taller women compared to average height women (aOR 0.68, 95% CI 0.49–0.96; aOR 0.51, 95% CI 0.37–0.71) (Table 2).
Association Between Maternal Height and Adverse Outcomes Stratified for Pre-pregnancy BMI
In women with normal pre-pregnancy BMI, maternal height was positively associated with LBW (aOR 2.00, 95% CI 1.15–3.49) and primary CS (aOR 1.71, 95% CI 1.28–2.28) in shorter women while it was negatively associated with the risk of abnormal neonatal ponderal index in both shorter and taller women compared to average height women (aOR 0.71, 95% CI 0.55–0.92; aOR 0.66, 95% CI 0.51–0.85). However, there was no significant association between maternal height and macrosomia and postpartum hemorrhage when stratified for pre-pregnancy BMI (Table 3).
Discussion
This study found that the association between maternal height and adverse pregnancy outcomes (macrosomia, postpartum hemorrhage, primary CS and LBW) varied in different pre-pregnancy BMI groups and GWG groups. Taller women with excess GWG had a higher risk of macrosomia compared to average height women with excess GWG. Shorter women with inadequate GWG had more than two times the risk of LBW and primary CS compared to women with average height who had inadequate GWG. Excess GWG was a protective factor for postpartum hemorrhage in shorter women. Shorter women with normal pre-pregnancy BMI had an increased risk of low birth weight and primary CS compared to average women with average height. Our findings suggest that maternal height can be used as a reference to identify Chinese women at high risk of adverse outcomes; however, pre-pregnancy BMI and GWG should be considered.
A study showed that pre-pregnancy BMI was independently associated with neonatal birth weight in women with normal glucose tolerance [20]. Higher pre-pregnancy BMI and excess GWG were far more important in macrosomia prediction than other maternal characteristics [21]. However, the rate of women with higher BMI is lower than in western countries [22]. In fact, the prevalence of underweight women is higher in East Asian countries [23,24,25]. Taller height and GDM are two distinct risk factors that could interact to cause macrosomia. According to studies, GDM only had an impact on macrosomia in taller women [8, 9]. Thus, hyperglycemia and excess GWG can be the main contributing factors to macrosomia compared to other factors in Chinese women [22]. Therefore, taller Chinese women with GDM can benefit from strict counseling on appropriate weight gain during pregnancy to decrease the risk of macrosomia.
A study showed that shorter women have a higher risk of LBW [26]. Risk of LBW may decrease with increasing maternal height from < 160.0 cm to 160.0 cm [27]. However, what causes LBW in women of short stature is still unclear. We found that shorter women had a higher incidence of LBW in accordance with previous studies [26, 28]. Inadequate GWG has been reported as a risk factor for LBW, similar to our findings [29]. A study involving Spanish women showed that women who gain inadequate GWG in both the second and third trimesters have increased risk of LBW [30]. On the other hand, a systemic review showed that high GWG was a protective factor against LBW in singleton pregnancy [31]. Malnutrition is known cause of LBW in shorter women; however, for Chinese women, particularly in Zhejiang Province, malnutrition is not the cause of short stature. Contrarily, different studies have shown that the GWG recommendation using IOM guidelines (2009) in Chinese women may not be appropriate; thus, GWG guidelines considering Chinese women's characteristics have been emphasized [32, 33]. Studies have reported that adopting appropriate GWG following Chinese population characteristics may reduce adverse pregnancy outcomes [34, 35]. According to our findings, Chinese women with shorter stature are at increased risk of LBW, particularly those who gain inadequate GWG or with normal pre-pregnancy BMI; clinicians should counsel shorter women on increasing GWG appropriately to decrease the risk of LBW. Nevertheless, further studies are needed to evaluate GWG cutoffs according to Chinese population characteristics.
Additionally, recent studies assessed birth size by birth length, birthweight, head circumference and ponderal index rather than only birthweight, which was associated with adverse preteen cardiometabolic health [36, 37]. Therefore, we further explored the association between maternal height and neonatal ponderal index, which has been researched in few studies. A previous observational cohort study showed that maternal height had no impact on offspring's ponderal index [9]. Another study revealed a significant correlation between infant ponderal index and maternal height for nulliparas but not for the multiparas [38]. We found maternal height was negatively associated with the risk of abnormal neonatal ponderal index in both shorter and taller women with adequate GWG or normal pre-pregnancy BMI, which showed the effect of maternal height on the ponderal index was dependent on GWG and pre-pregnancy BMI. Thus, it is recommended to consider these maternal anthropometric parameters when assessing the birth size. Furthermore, our study lacked offspring’s metabolic indices, and this warrants further study.
According to a research study, increasing maternal height reduces the risk of CS [39]. Also, studies have reported that excess GWG increases risk of delivery by cesarean section [40, 41]. Therefore, it is imperative to counsel shorter women on appropriate GWG during pregnancy. A study showed that overweight and obese pre-pregnancy BMIs were the leading risk factors of primary CS in women of average height, whereas excess GWG was the leading risk factor of primary CS in women of taller stature, similar to our findings [42,43,44]. Another study showed that women with pre-pregnancy BMI > 30 kg/m2 had increased risk of primary CS compared to women with pre-pregnancy BMI < 20 kg/m2 [41]. Excess GWG and obesity increase risk of delivery by cesarean section because of increased abdominal fat, thus hindering abdominal muscle contraction. Strict health education and counseling of women with overweight/obese pre-pregnancy BMI earlier in pregnancy and strict monitoring of GWG might reduce the risk of delivery by CS [45, 46].
Maternal height was previously related to postpartum hemorrhage in singleton pregnancy [47]. In a deep machine learning prediction study model, the relationship between maternal height and postpartum hemorrhage following vaginal delivery was positive [48]. According to one study, the risk of postpartum hemorrhage increased with maternal height (160–170 cm versus 160 cm) [49]. On the other hand, a study showed that shorter stature < 151 cm was significantly associated with risk of postpartum hemorrhage [50]. Another study found that maternal and fetal genes may contribute to postpartum hemorrhage, which may help explain the inconsistency [51]. It is critical to consider the relationship between maternal height and postpartum hemorrhage; however, more extensive studies are required.
To the best of our knowledge, this is the first study to evaluate the relationship between maternal height and adverse outcomes in different pre-pregnancy BMI and GWG groups. Our findings can help clinicians prevent GDM-related adverse outcomes when different maternal heights are considered, as well as pre-pregnancy BMI and GWG.
Limitations of Our Study
Our study had several limitations. First, it is a retrospective study including a small sample from a single health center. Maternal weight and height were self-reported, which might affect the accuracy of the result. Second, data on social demographic characteristics and nutrition status information were not found. Third, the association between maternal height and risk of adverse outcomes was not adjusted for other associated clinical conditions such as cervix incompetence, maternal infections, fetal malpresentation and so on [49]. Thus, further research is needed to evaluate the association between maternal height and adverse outcomes in GDM by BMI and GWG considering relevant clinical conditions.
Conclusion
The relationship between maternal height and adverse pregnancy outcomes varies with pre-pregnancy BMI and GWG in GDM women. Comprehensive counseling and health education considering maternal height and pre-pregnancy BMI and GWG may help prevent adverse outcomes in GDM women.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Classification and Diagnosis of Diabetes. Standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S17-s38.
Lee KW, Ching SM, Ramachandran V, Yee A, Hoo FK, Chia YC, et al. Prevalence and risk factors of gestational diabetes mellitus in Asia: a systematic review and meta-analysis. BMC Pregnancy Childbirth. 2018;18(1):494.
Najafi F, Hasani J, Izadi N, Hashemi-Nazari SS, Namvar Z, Shamsi H, et al. Risk of gestational diabetes mellitus by pre-pregnancy body mass index: a systematic review and meta-analysis. Diabetes Metab Syndr. 2021;15(4): 102181.
Brite J, Shiroma EJ, Bowers K, Yeung E, Laughon SK, Grewal JG, et al. Height and the risk of gestational diabetes: variations by race/ethnicity. Diabetic Med. 2014;31(3):332–40.
Okewole IA, Faiola S, Fakounde A, Yoong W, Phillip H, Amer S. The relationship of ethnicity, maternal height and shoe size, and method of delivery. J Obstet Gynaecol. 2011;31(7):608–11.
Poon LC, Volpe N, Muto B, Syngelaki A, Nicolaides KH. Birthweight with gestation and maternal characteristics in live births and stillbirths. Fetal Diagn Ther. 2012;32(3):156–65.
Dickey RP, Xiong X, Xie Y, Gee RE, Pridjian G. Effect of maternal height and weight on risk for preterm singleton and twin births resulting from IVF in the United States, 2008–2010. Am J Obstet Gynecol. 2013;209(4):349.e1-6.
Chu AHY, Yuan WL, Loy SL, Soh SE, Bernard JY, Tint MT, et al. Maternal height, gestational diabetes mellitus and pregnancy complications. Diabetes Res Clin Pract. 2021;178: 108978.
Masalin S, Laine MK, Kautiainen H, Gissler M, Raina M, Pennanen P, et al. Impact of maternal height and gestational diabetes mellitus on offspring birthweight. Diabetes Res Clin Pract. 2019;148:110–8.
Bao C, Zhou Y, Jiang L, Sun C, Wang F, Xia W, et al. Reasons for the increasing incidence of macrosomia in Harbin, China. BJOG. 2011;118(1):93–8.
Alberico S, Montico M, Barresi V, Monasta L, Businelli C, Soini V, et al. The role of gestational diabetes, pre-pregnancy body mass index and gestational weight gain on the risk of newborn macrosomia: results from a prospective multicentre study. BMC Pregnancy Childbirth. 2014;14:23.
Cosson E, Cussac-Pillegand C, Benbara A, Pharisien I, Nguyen MT, Chiheb S, et al. Pregnancy adverse outcomes related to pregravid body mass index and gestational weight gain, according to the presence or not of gestational diabetes mellitus: a retrospective observational study. Diabetes Metab. 2016;42(1):38–46.
Marshall NE, Biel FM, Boone-Heinonen J, Dukhovny D, Caughey AB, Snowden JM. The association between maternal height, body mass index, and perinatal outcomes. Am J Perinatol. 2019;36(6):632–40.
Institute of M, National Research Council Committee to Reexamine IOMPWG. The National Academies Collection: reports funded by National Institutes of Health. In: Rasmussen KM, Yaktine AL, editors. Weight gain during pregnancy: reexamining the guidelines. Washington: National Academies Press; 2009.
Shen L, Wang J, Duan Y, Yang Z. Prevalence of low birth weight and macrosomia estimates based on heaping adjustment method in China. Sci Rep. 2021;11(1):15016.
Gestational Hypertension and Preeclampsia: ACOG Practice Bulletin, Number 222. Obstetrics and gynecology. 2020;135(6):e237–e60
ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists number 76, October 2006: postpartum hemorrhage. Obstet Gynecol. 2006;108(4):1039–47.
Landmann E, Reiss I, Misselwitz B, Gortner L. Ponderal index for discrimination between symmetric and asymmetric growth restriction: percentiles for neonates from 30 weeks to 43 weeks of gestation. J Matern Fetal Neonatal Med. 2006;19(3):157–60.
Lampl M, Gotsch F, Kusanovic JP, Gomez R, Nien JK, Frongillo EA, et al. Sex differences in fetal growth responses to maternal height and weight. Am J Hum Biol. 2010;22(4):431–43.
Di Cianni G, Miccoli R, Volpe L, Lencioni C, Ghio A, Giovannitti MG, et al. Maternal triglyceride levels and newborn weight in pregnant women with normal glucose tolerance. Diabet Med. 2005;22(1):21–5.
Lewandowska M. The role of maternal weight in the hierarchy of macrosomia predictors; overall effect of analysis of three prediction indicators. Nutrients. 2021;13(3):801.
Li G, Kong L, Li Z, Zhang L, Fan L, Zou L, et al. Prevalence of macrosomia and its risk factors in china: a multicentre survey based on birth data involving 101,723 singleton term infants. Paediatr Perinat Epidemiol. 2014;28(4):345–50.
Jaacks LM, Slining MM, Popkin BMJ. Recent underweight and overweight trends by rural–urban residence among women in low-and middle-income countries. J Nutr. 2015;145(2):352–7.
He Y, Pan A, Yang Y, Wang Y, Xu J, Zhang Y, et al. Prevalence of underweight, overweight, and obesity among reproductive-age women and adolescent girls in rural China. Am J Public Health. 2016;106(12):2103–10.
Inoue S, Naruse H, Yorifuji T, Kato T, Murakoshi T, Doi H, et al. Association between short maternal height and low birth weight: a hospital-based study in Japan. J Korean Med Sci. 2016;31(3):353–9.
Goto E. Dose-response relationships of maternal height and weight with risk of low birthweight neonates: a meta-analysis. Minerva Pediatr. 2023;75(1):110–6.
Han Z, Lutsiv O, Mulla S, McDonald SD. Maternal height and the risk of preterm birth and low birth weight: a systematic review and meta-analyses. J Obstet Gynaecol Can. 2012;34(8):721–46.
Uchinuma H, Tsuchiya K, Sekine T, Horiuchi S, Kushima M, Otawa S, et al. Gestational body weight gain and risk of low birth weight or macrosomia in women of Japan: a nationwide cohort study. Int J Obes. 2021;45(12):2666–74.
Deierlein AL, Messito MJ, Katzow M, Berube LT, Dolin CD, Gross RS. Total and trimester-specific gestational weight gain and infant anthropometric outcomes at birth and 6 months in low-income Hispanic families. Pediatr Obes. 2020;15(3): e12589.
McDonald SD, Han Z, Mulla S, Lutsiv O, Lee T, Beyene J, et al. High gestational weight gain and the risk of preterm birth and low birth weight: a systematic review and meta-analysis. J Obstet Gynaecol Can. 2011;33(12):1223–33.
Huang X, Tan H, Cai M, Shi T, Mi C, Lei J. Gestational weight gain in Chinese women—results from a retrospective cohort in Changsha, China. BMC Pregnancy Childbirth. 2018;18(1):185.
Wang J, Duan YF, Pang XH, Jiang S, Yin SA, Yang ZY, et al. Gestational weight gain and optimal ranges in Chinese mothers giving singleton and full-term births in 2013. Zhonghua Yu Fang Yi Xue Za Zhi [Chin J Prev Med]. 2018;52(1):31–7.
Li C, Liu Y, Zhang W. Joint and independent associations of gestational weight gain and pre-pregnancy body mass index with outcomes of pregnancy in Chinese women: a retrospective cohort study. PLoS ONE. 2015;10(8): e0136850.
Jiang X, Liu M, Song Y, Mao J, Zhou M, Ma Z, et al. The Institute of Medicine recommendation for gestational weight gain is probably not optimal among non-American pregnant women: a retrospective study from China. J Maternal-Fetal Neonatal Med. 2019;32(8):1353–8.
Landsverk E, Westvik-Johari K, Romundstad LB, Opdahl S. Birth size after embryo cryopreservation: larger by all measures? Hum Reprod (Oxf, Engl). 2023;38(7):1379–89.
Wang H, Li W, Yang J, Wang Y, Du H, Han M, et al. Gestational exposure to perfluoroalkyl substances is associated with placental DNA methylation and birth size. Sci Total Environ. 2023;858(Pt 1): 159747.
Callanan S, Killeen SL, Delahunt A, Cooney N, Cushion R, McKenna MJ, et al. The impact of macrosomia on cardiometabolic health in preteens: findings from the ROLO longitudinal birth cohort study. Nutr Metab. 2023;20(1):37.
Rossi E, Szerszen A, Ahn C, Keith LG, Rhea DJ, Blickstein I. The ponderal index in triplets: IV. Relationship with maternal height. J Perinat Med. 2004;32(1):74–7.
Mogren I, Lindqvist M, Petersson K, Nilses C, Small R, Granåsen G, et al. Maternal height and risk of caesarean section in singleton births in Sweden—a population-based study using data from the Swedish Pregnancy Register 2011 to 2016. PLoS ONE. 2018;13(5): e0198124.
Stotland NE, Hopkins LM, Caughey AB. Gestational weight gain, macrosomia, and risk of cesarean birth in nondiabetic nulliparas. Obstet Gynecol. 2004;104(4):671–7.
Zhang CX, Lai JQ, Liu KY, Yang NH, Zeng G, Mao LM, et al. Optimal gestational weight gain in Chinese pregnant women by Chinese-specific BMI categories: a multicentre prospective cohort study. Public Health Nutr. 2021;24(11):3210–20.
Shepard MJ, Saftlas AF, Leo-Summers L, Bracken MB. Maternal anthropometric factors and risk of primary cesarean delivery. Am J Public Health. 1998;88(10):1534–8.
Young TK, Woodmansee B. Factors that are associated with cesarean delivery in a large private practice: the importance of prepregnancy body mass index and weight gain. Am J Obstet Gynecol. 2002;187(2):312–8.
Cnattingius R, Cnattingius S, Notzon FC. Obstacles to reducing cesarean rates in a low-cesarean setting: the effect of maternal age, height, and weight. Obstet Gynecol. 1998;92(4 Pt 1):501–6.
Graham LE, Brunner Huber LR, Thompson ME, Ersek JL. Does amount of weight gain during pregnancy modify the association between obesity and cesarean section delivery? Birth (Berkeley, CA). 2014;41(1):93–9.
Xiong C, Zhou A, Cao Z, Zhang Y, Qiu L, Yao C, et al. Association of pre-pregnancy body mass index, gestational weight gain with cesarean section in term deliveries of China. Sci Rep. 2016;6:37168.
Li S, Gao J, Liu J, Hu J, Chen X, He J, et al. Incidence and risk factors of postpartum hemorrhage in China: a multicenter retrospective study. Front Med. 2021;8: 673500.
Akazawa M, Hashimoto K, Katsuhiko N, Kaname Y. Machine learning approach for the prediction of postpartum hemorrhage in vaginal birth. Sci Rep. 2021;11(1):22620.
Oberg AS, Hernandéz-Diaź S, Frisell T, Greene MF, Almqvist C, Bateman BT. Genetic contribution to postpartum haemorrhage in Swedish population: cohort study of 466,686 births. BMJ (Clin Res Ed). 2014;349: g4984.
Lao TT, Sahota DS, Cheng YK, Law LW, Leung TY. Advanced maternal age and postpartum haemorrhage—risk factor or red herring? J Matern Fetal Neonatal Med. 2014;27(3):243–6.
Derraik JG, Lundgren M, Cutfield WS, Ahlsson F. Maternal height and preterm birth: a study on 192,432 Swedish women. PLoS ONE. 2016;11(4): e0154304.
Acknowledgements
We gratefully thank Women’s Hospital, Zhejiang University School of Medicine, and women who participated in this study.
Funding
This work and its publication, including the journal’s Rapid Service Fee, were funded by the Key R&D Program of Zhejiang Province under Grant 2022C03058, Medical and Health Technology Program of Zhejiang Province under Grant WKJ-ZJ-2324, and 4 + X Clinical Research of Women’s Hospital, School of Medicine, Zhejiang University under Grant ZDFY2022-4XB101.
Author information
Authors and Affiliations
Contributions
Zhaoxia Liang and Danqing Chen contributed to the study conception and design. Mengkai Du and Marie Parfaite Uwimana Muhuza did analysis and drafted the article. All authors contributed to interpretation of the data. Zhaoxia Liang, Danqing Chen, Lixia Zhang, Yibo Tang and Yanmin Chen revised the manuscript for intellectual content. Zhaoxia Liang contributed acquisition of data, analysis and interpretation of data, drafting and revising the manuscript, statistical analysis, and study supervision. All authors have contributed to the proofreading and agreed to the final content of the manuscript for submission. All authors agree to accountability for all aspects of the work.
Corresponding authors
Ethics declarations
Conflict of Interest
Mengkai Du, Marie Parfaite Uwinana Muhuza, Yibo Tang, Yanmin Chen, Danqing Chen, Lixia Zhang and Zhaoxia Liang report no conflict of interest.
Ethical Approval
This study was approved by the Human Ethics Committee at Women’s Hospital, School of Medicine, Zhejiang University (IRB-20210269-R). The methods were performed in accordance with the Helsinki Declaration.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Du, M., Muhuza, M.P.U., Tang, Y. et al. Maternal Height Is an Independent Risk of Adverse Outcomes in Women with Gestational Diabetes Mellitus. Diabetes Ther 15, 461–472 (2024). https://doi.org/10.1007/s13300-023-01512-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01512-3