Abstract
Introduction
Long-term effectiveness and durability of glucose-lowering medications are important considerations in managing type 2 diabetes (T2D). This study aimed to compare durability of treatment efficacy of once-weekly (OW) semaglutide for T2D with that of the dipeptidyl peptidase 4 inhibitor (DPP–4i) class.
Methods
This observational cohort study used 2017–2022 data from the Optum® Clinformatics® Data Mart to compare long-term clinical outcomes associated with semaglutide or DPP–4i in US adults with T2D. The primary outcomes were HbA1c at 2-year follow-up, change in HbA1c from baseline, and the odds of achieving HbA1c targets. BMI at 2-year follow-up, change in BMI from baseline, odds of reducing BMI category, and the need for treatment augmentation were exploratory outcomes. Bivariate and multivariate analyses were conducted using inverse probability of treatment weighting (IPTW) weighted descriptive statistics.
Results
Weighted HbA1c and BMI cohorts included 865 and 642 semaglutide users and 779 and 537 DPP–4i users, respectively. In the weighted HbA1c cohort, semaglutide and DPP–4i users had an average age of 60 years and similar baseline characteristics including HbA1c level and comorbidity status. Two-year follow-up HbA1c with semaglutide was 0.56% lower than with DPP–4i; reduction in HbA1c from baseline was 0.61% greater. Odds of achieving HbA1c level < 7% were 2.16 times greater after covariate adjustment (all, p < 0.001). Semaglutide was associated with 1.03 kg/m2 greater reduction in BMI and 2.27 times greater odds of reducing BMI category vs DPP–4i (p < 0.001). Semaglutide users were less likely to add new glucose-lowering treatment (hazard ratio [HR] 0.57; p < 0.001) or initiate insulin (HR 0.49; p < 0.001) vs DPP–4i users.
Conclusion
Compared with DPP–4i, semaglutide was associated with lower follow-up HbA1c and BMI, greater reduction in HbA1c and BMI from baseline, and reduced likelihood of requiring treatment augmentation or insulin initiation to manage T2D in US adults, suggesting better durability of semaglutide vs DPP–4i.
Infographic

Plain language summary
Type 2 diabetes (T2D) is a progressive disease. Over time, many patients with T2D will need multiple drugs to manage their disease. Long-term efficacy is important for achieving treatment goals, such as blood sugar control and weight loss. The amount of time that different types of diabetes drugs remain effective varies. This study used real-world data to compare two distinct types of diabetes drugs, semaglutide and dipeptidyl peptidase 4 inhibitors (DPP–4is). We looked at how blood sugar control and body weight changed with each drug after 2 years of use. We also compared how many patients needed to start using new drugs to meet their treatment goals and the odds that a patient would need to start using new drugs. Semaglutide was better than DPP–4i in reducing both blood sugar levels and body weight. Patients had over two times the odds of meeting target blood sugar levels with semaglutide. Fewer patients needed to start using new drugs with semaglutide, and patients were 43% less likely to start using new drugs to lower blood sugar than patients taking DPP–4is.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Treatment failure and subsequent therapeutic intensification is common with T2D; therefore, a better understanding of long-term treatment efficacy and durability of glucose-lowering treatments is needed. |
This observational cohort study used administrative claims data to compare reductions in HbA1c and BMI as well as treatment augmentation in US adults with T2D persistent with either once-weekly semaglutide for T2D or DPP–4i for at least 2 years. |
What was learned from the study? |
After 2 years of use, the reductions in HbA1c level and BMI, as well as greater odds of achieving glycemic targets and BMI category reduction, remain in semaglutide users when compared with DPP–4i users. |
The risk of treatment augmentation, including insulin initiation, was significantly lower with long-term persistent use of semaglutide than DPP–4i. |
Overall, these findings suggest better treatment durability of semaglutide vs DPP–4i. |
Digital Features
This article is published with digital features, including an infographic, to facilitate understanding of the article. To view digital features for this article, go to https://doi.org/10.6084/m9.figshare.24476476.
Introduction
Type 2 diabetes (T2D) is a highly prevalent disease globally [1, 2]. Pharmacotherapy, in addition to proper diet and exercise, is the cornerstone of T2D treatment [3]. Noninsulin glucose-lowering agents currently used to treat T2D in the USA include biguanides, sulfonylureas, thiazolidinediones, α-glucosidase inhibitors, meglitinides, dipeptidyl peptidase 4 inhibitors (DPP–4is), sodium-glucose cotransporter 2 (SGLT2) inhibitors, glucagon-like peptide 1 receptor agonists (GLP-1 RAs), GLP-1/glucose-dependent insulinotropic polypeptide (GIP) dual agonists, bile acid sequestrants, dopamine-2 agonists, and amylin mimetics [3]. The American Diabetes Association [3] recommends using GLP-1 RA for achievement and maintenance of glycemic and weight management goals in adults with T2D and for comprehensive cardiovascular risk management and cardiorenal risk reduction in high-risk individuals with T2D.
Semaglutide, a new-generation GLP-1 RA, is a GLP-1 analogue with 94% homology to human GLP-1 that selectively binds to and activates the GLP-1 receptor, the target for native GLP-1 [4]. Once-weekly (OW) subcutaneous administration of semaglutide (Ozempic®, Novo Nordisk Inc., Plainsboro, NJ; hereafter, semaglutide) achieved superior reductions in glycated hemoglobin (HbA1c) levels and body weight across key efficacy trials when compared with placebo or active comparators in individuals with T2D [5,6,7,8,9,10,11,12,13].
Durability is the duration of time that a treatment is deemed effective for any reason. Substantial evidence supports the short-term efficacy of glucose-lowering treatments; however, understanding the comparative long-term effectiveness and durability of these treatments is equally important [3, 14, 15]. The Glycemia Reduction Approaches in Type 2 Diabetes: A Comparative Effectiveness (GRADE) study [16] found that GLP-1 RA (i.e., liraglutide) was significantly more effective in achieving and maintaining target levels of HbA1c compared with sulfonylureas (i.e., glimepiride) and DPP–4i (i.e., sitagliptin) after an average follow-up of 5 years among those with T2D who were on metformin. Additionally, our recent findings show that persistent GLP-1 RA users had significantly greater reductions in HbA1c level and higher percentages of achieving HbA1c goals compared with persistent DPP–4i users [15]. Given the results of the GRADE study and our recent findings suggesting that persistence with GLP-1 RA is associated with better glycemic control than DPP–4i, a need exists to understand the comparative durability of the new-generation GLP-1 RA semaglutide and the commonly used glucose-lowering agent class DPP–4i in the real-world setting. This study aimed to compare primary HbA1c outcomes and exploratory outcomes of weight and treatment augmentation in US adults with T2D persistent with either semaglutide or DPP–4i for at least 2 years.
Methods
Study Design
To compare treatment effectiveness and durability of semaglutide and DPP–4i in persistent users, this observational cohort study used deidentified data collected from the Optum® Clinformatics® Data Mart (CDM) between January 1, 2017 and September 30, 2022 (end of study; Supplementary Fig. 1). The index date (day 0) was defined as the new initiation date of the index drug (semaglutide or a DPP–4i). The selection window for initiation of the index drug was from January 1, 2018 to 720 days before the end of the study. The baseline period was defined as 1 year before the index date [days − 360, − 1]. Outcomes were assessed in the 2-year follow-up period from the index date to 719 days after the index date [days 0, 719].
Data Source
The Optum® CDM is a database containing administrative claims data for a large managed care population, including commercial and Medicare Advantage health plan members from geographically diverse regions of the USA. Longitudinal medical and pharmacy claims data in the Optum® CDM are verified, adjudicated, adjusted, and deidentified and include information on patient demographics, inpatient and outpatient medical care, pharmacy dispensing, and outpatient laboratory test results from national laboratory vendors.
Study Population
Individuals aged ≥ 18 years were eligible on the basis of their having a pharmacy claim for an index drug (semaglutide or DPP–4i) during the index date selection window (January 1, 2018 to October 10, 2020) and their having a confirmed T2D diagnosis, defined as ≥ 2 claims for International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) code on distinct days between January 1, 2017 and September 30, 2022, with ≥ 1 record during the baseline period. DPP–4is included in this analysis were sitagliptin, saxagliptin, linagliptin, and alogliptin. Individuals were required to have continuous enrollment for 360 days before index date and 719 days after index date as well as persistent use of index drug for ≥ 720 days, defined as ≤ 90-day gap from the date of first pharmacy claim to exhaustion of days’ supply of the last pharmacy claim. For individuals in the DPP–4i cohort, switching in the same drug class during the follow-up was allowed. Exclusion criteria included diagnosis of type 1 diabetes, pregnancy, use of any GLP-1 RA or DPP–4i during the baseline period, use of ≥ 2 types of products in the index drug class on the index date, initiation of another new glucose-lowering drug class on the index date, bariatric surgery, or use of antiobesity medications during the study period.
As a result of data availability and limited sample size, two cohorts were analyzed in this study: the HbA1c cohort and the BMI cohort. The HbA1c cohort was composed of individuals with HbA1c values available in the dataset at baseline (between 120 and 1 days before the index date) and follow-up (between 540 and 719 days after the index date). The BMI cohort was composed of individuals with BMI values available at baseline (between 180 and 1 days before the index date) and follow-up (between 540 and 719 days after the index date).
Outcome and Covariates Measures
Primary HbA1c outcomes were measured for the HbA1c cohort and included HbA1c level at 2-year follow-up, change in HbA1c level from baseline to follow-up, and proportion of individuals achieving HbA1c levels < 7% and < 8% in the follow-up period. Exploratory treatment augmentation outcomes were also measured for the HbA1c cohort. Time to treatment augmentation was measured as the duration from day 60 to the date of adding a new glucose-lowering drug class that was neither the index drug class nor the treatment used at baseline; ≥ 2 prescription claims for the new glucose-lowering drug starting at least 60 days before the last date of the index drug or the end of study, whichever came first, were required. In the subset of individuals who did not use insulin before day 60, the time to insulin initiation was also explored; ≥ 2 prescription claims for insulin initiated at least 60 days before the last date of the index drug or the end of study, whichever came first, were required.
For the BMI cohort, exploratory BMI outcomes were measured using ICD-10-CM codes and included change in BMI from baseline to follow-up and proportion of individuals with decreasing BMI category from baseline to follow-up. In this study, BMI values were defined as the midpoint of the ICD-10-CM code (e.g., ICD-10-CM code Z68.25 [adult BMI 25.0–25.9 kg/m2] was defined as BMI 25.45 kg/m2 in this study). BMI categories were defined as < 25, 25 to < 30, 30 to < 35, 35 to < 40, and ≥ 40.
Covariates included age, sex, race and ethnicity, geographic region, index year, payer type, insurance plan type, prescriber specialty, Charlson Comorbidity Index (CCI; CDMF version) [17, 18], Diabetes Complication Severity Index (DCSI) [19, 20], common comorbidities (yes/no), common concomitant drug classes (yes/no), diseases/conditions related to weight changes, medications associated with weight gain (yes/no), number of glucose-lowering medications, glucose-lowering drug class at baseline, common procedures (yes/no), number of all-cause hospitalizations (60 days before index date), number of all-cause emergency department visits (60 days before index date), baseline out-of-pocket costs for all prescription drugs, and number of follow-up days amid the COVID-19 pandemic (i.e., follow-up days after March 1, 2020).
Statistical Analyses
Descriptive analyses were conducted in both semaglutide and DPP–4i groups. Counts and frequencies were used for categorical variables; means and SDs, for continuous variables.
To reduce the selection bias and observed confounding between the two groups, inverse probability of treatment weighting (IPTW) [21] was derived by conducting a regularized logistic regression with elastic net penalty on the semaglutide group vs DPP–4i group with the following variables: age, race and ethnicity, index year, payer type, CCI, DCSI, glucose-lowering medications, baseline HbA1c level, baseline BMI and obesity diagnosis, health care utilization at baseline, comorbidities, and other medications at baseline. The targeted average treatment effect estimate was unable to be sufficiently balanced; therefore, the average treatment effect of the treated (ATT) was estimated. For all covariates, descriptive statistics were reported with and without IPTWs. Standardized mean differences (SMDs) were presented, and SMD ≥ 0.1 was considered a meaningful difference. Weighted descriptive statistics, bivariate analyses, and multivariate analyses were conducted. Both bivariate analyses and multivariate analyses used linear and logistic regression models with robust SEs. Bivariate analyses were conducted without adjusting for covariates (reported as unadjusted), while multivariate analyses also controlled covariates that were not balanced between groups (reported as adjusted). For time-to-event outcomes, weighted Kaplan–Meier cumulative incidence function and log-rank test statistic, as well as Cox proportional hazards (PH) regression with robust SEs, were used.
Two subgroup analyses were also explored: those with baseline HbA1c ≥ 7.0% and those whose treatment escalated to 1 mg semaglutide in their last dose before the follow-up HbA1c or BMI measures. Subgroup analyses were not reweighted between the subgroup of semaglutide and DPP–4i users, and only bivariate analyses were conducted in subgroup analyses. A sensitivity analysis of main outcomes using 1:1 ratio propensity score matching (PSM) was also conducted. All analyses were performed using R 4.0.4.
Compliance with Ethics Guidelines
The claims data assessed were in accordance with Health Insurance Portability and Accountability Act. This study was exempt from institutional review board review because this study was not classified as research involving human subjects. Database access and use of the data analyzed in this study were permitted by Optum® Clinformatics®. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for the version to be published.
Results
HbA1c and BMI Cohorts
For the HbA1c cohort, the final sample included 865 semaglutide users (weighted and unweighted) and 4225 DPP–4i users (weighted, n = 779; Supplementary Fig. 2). Before weighting, the DPP–4i group (mean [SD] = 69.14 [10.41] years) was older than the semaglutide group (mean [SD] = 60.36 [10.65] years, Table 1). DPP–4i users had worse health and diabetic status than semaglutide users according to CCI and DCSI scores (CCI mean [DPP–4i vs semaglutide users] = 3.42 vs 2.87; DCSI mean [DPP–4i vs semaglutide users] = 2.24 vs 1.62, Table 1). Semaglutide users had a higher average baseline HbA1c than DPP–4i users (mean [SD] = 8.27% [1.67%] for semaglutide; mean [SD] = 8.09% [1.43%] for DPP–4i). After weighting, baseline characteristics were balanced between the two groups, except for index year, prescriber’s specialty, BMI, and feeding difficulty (Table 1 and Supplementary Table 1). Because of estimates of average treatment effect of the treated, baseline characteristics in the DPP–4i group were closer to those of the semaglutide group after weighting. After weighting, the average age in both groups was approximately 60 years, a slightly higher proportion of the population was male, and more than half were commercial insurance enrollees.
For the BMI cohort, the final sample included 642 semaglutide users (weighted and unweighted) and 2105 DPP–4i users (weighted, n = 537; Supplementary Fig. 2). Before weighting, the differences observed between groups in the BMI cohort were similar to those observed in the HbA1c cohort. After weighting, baseline characteristics for the DPP–4i group were weighted toward those of semaglutide users, and most were balanced between groups. Exceptions are noted in Supplementary Tables 1 and 2.
Primary HbA1c Outcomes
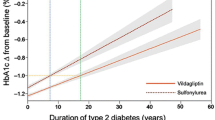
Bivariate and multivariate analyses of HbA1c outcomes showed similar results (Fig. 1 and Table 2). After 2 years of persistent use, semaglutide was associated with 0.58% lower follow-up HbA1c and 0.60% greater reduction in HbA1c from baseline than DPP–4i (0.56% and 0.61%, respectively, after adjusting for unbalanced covariates; all, p < 0.001). In addition, semaglutide users showed more than twice the odds of achieving HbA1c targets vs DPP–4i users (unadjusted odds ratios [OR] = 2.20 and 2.16 for achieving HbA1c < 7.0% and < 8.0%, respectively; adjusted conditional OR = 2.16 and 2.15 for achieving HbA1c < 7.0% and < 8.0%, respectively; all, p < 0.001). Weighted descriptive analyses of HbA1c outcomes are reported in Supplementary Table 3.
Weighted analyses of primary HbA1c outcomes a Weighted descriptive analyses of the change in HbA1c from baseline to 2-year follow-up in the semaglutide and DPP–4i cohorts without covariate adjustment. b Weighted bivariate analyses comparing 2-year follow-up HbA1c in the semaglutide cohort vs DPP–4i cohort without covariate adjustment. c Weighted bivariate analyses comparing the change in HbA1c from baseline to follow-up in the semaglutide cohort vs DPP–4i cohort without covariate adjustment. DPP–4i indicates dipeptidyl peptidase 4 inhibitor; OW, once weekly; T2D, type 2 diabetes
Exploratory BMI Outcomes
After adjustment for unbalanced covariates, semaglutide users were found to have a 0.88 kg/m2 lower average follow-up BMI value (p = 0.012) and 1.03 kg/m2 greater reduction in BMI from baseline (p < 0.001) (Fig. 2 and Table 2). Furthermore, semaglutide users were more likely to change to a lower follow-up BMI category from baseline (unadjusted and adjusted conditional OR = 2.27, all p < 0.001). Weighted descriptive analyses of BMI outcomes are reported in Table 2.
Weighted analyses of exploratory BMI outcomes. a Weighted descriptive analyses of the change in BMI from baseline to 2-year follow-up in the semaglutide and DPP–4i cohorts without covariate adjustment. b Weighted bivariate analyses comparing 2-year follow-up BMI in the semaglutide cohort vs DPP–4i cohort without covariate adjustment. c Weighted bivariate analyses comparing the change in BMI from baseline to follow-up in the semaglutide cohort vs DPP–4i cohort without covariate adjustment. DPP–4i indicates dipeptidyl peptidase 4 inhibitor; OW, once weekly; T2D, type 2 diabetes
Treatment Augmentation
After adjustment, approximately one-third of DPP–4i users added a new glucose-lowering drug class compared with approximately one-fifth of semaglutide users during the 2-year follow-up (31.8% vs 19.3%, respectively; Fig. 3). The cumulative incidence curve and log-rank test confirm a significant difference in the time to addition of a new glucose-lowering drug class between groups (p < 0.001, Fig. 3). Semaglutide users were 43% less likely to add a new glucose-lowering drug class than DPP–4i users as shown in unadjusted and adjusted (conditional) Cox PH regression (HR 0.57, all p < 0.001); logistic regression models showed similar results.
Weighted analyses: addition of glucose-lowering medications. Adjusted and unadjusted rates of addition of new glucose-lowering medications for the semaglutide OW T2D and DPP–4i groups are shown in the left panel. Adjusted conditional and unadjusted HRs and ORs comparing semaglutide OW T2D are shown in the middle panel. Kaplan–Meier curves of time to addition of a new glucose-lowering medication are shown in the right panel. DPP–4i indicates dipeptidyl peptidase 4 inhibitor; HR, hazard ratio; OR, odds ratio; OW, once weekly; PH, proportional hazards; T2D, type 2 diabetes
Among the subset of individuals who did not use insulin at baseline, approximately 2.0% and 4.1% of semaglutide and DPP–4i users, respectively, initiated insulin during follow-up (Fig. 4). All unadjusted and adjusted regression models found that semaglutide users were 51% less likely to initiate insulin vs DPP–4i users (all p < 0.05, Fig. 4). The cumulative incidence curve and log-rank test confirm a significant difference in time to insulin initiation between groups.
Weighted analyses: insulin initiation among US adults with T2D. Adjusted and unadjusted rates of insulin initiation for the semaglutide OW T2D and DPP–4i groups are shown in the left panel. Adjusted conditional and unadjusted HRs and ORs comparing semaglutide OW T2D are shown in the middle panel. Kaplan–Meier curves of time-to-insulin initiation are shown in the right panel. DPP–4i indicates dipeptidyl peptidase 4 inhibitor; HR, hazard ratio; OR, odds ratio; OW, once weekly; PH, proportional hazards; T2D, type 2 diabetes
Subgroup Analyses
For subgroup analyses of those with baseline HbA1c ≥ 7.0% and those who reached semaglutide 1 mg during follow-up, overall results were consistent with those reported for the main analyses; however, no significant differences in insulin initiation were found between the two groups (Supplementary Tables 3 and 4).
Sensitivity Analyses
After PSM, the sample sizes in both groups reduced to 630 (n = 865 in semaglutide vs n = 4225 in DPP–4i before matching). Overall results of PSM were consistent with the main analyses using IPTW with ATT estimation; however, no significant differences were found in insulin initiation (Supplementary Table 5).
Discussion
Among US adults with T2D, semaglutide was associated with sustained glycemic control, BMI reduction, and reduced risks of treatment augmentation, including insulin initiation, after 2 years of persistent use when compared with DPP–4i. This study is among the first to investigate 2-year effects associated with persistence with semaglutide in this population. A broad range of clinically relevant long-term outcomes were assessed against an active comparison group, DPP–4i, in a relatively large sample size, and statistical methods were used to address potential confounding and bias.
After 2 years, semaglutide was associated with significantly larger reductions in both BMI (− 1.00 kg/m2 semaglutide vs DPP–4i) and HbA1c (− 0.60% semaglutide vs DPP–4i) compared with DPP–4i use. Similar reductions in BMI and HbA1c with semaglutide were reported across the SUSTAIN clinical trial program [5,6,7,8,9,10,11,12,13], which compared the efficacy and safety of semaglutide with that of placebo and active comparators over different periods, ranging from 30 to 104 weeks. In the SUSTAIN 2 trial comparing semaglutide vs DPP–4i, reductions in BMI and HbA1c similar to the main and subgroup analyses of the present study were observed with 0.5 mg semaglutide (ETDBMI, − 0.9 kg/m2; ETDHbA1c, − 0.77%); however, greater reductions were observed with 1.0 mg semaglutide (ETDBMI, − 1.58 kg/m2; ETDHbA1c, − 1.06%) [6]. Notably, the main analysis in the present study included 0.25 mg, 0.5 mg, and 1.0 mg doses of semaglutide, and only about 54% of patients had 1.0 mg as the last dose before the follow-up HbA1c measure (approx. 60% in the BMI cohort); subgroup analyses were not reweighted between the groups. A phase 3a trial comparing semaglutide vs DPP–4i in Japan reported a similar reduction in BMI and a greater reduction in HbA1c to the present study (ETDBMI, − 0.84 kg/m2; ETDHbA1c, − 1.13%) [22].
The 2-year HbA1c and BMI outcomes observed in the present study are also congruent with real-world studies on semaglutide conducted globally. Results from the EXPERT study showed significant improvements in HbA1c and body weight among US individuals switching to semaglutide from any other GLP-1 RA; the improvements in HbA1c were sustained from 6 to 12 months [22]. Similarly, HbA1c and body weight were significantly reduced in the observational SURE studies conducted across Europe and Canada; the change in HbA1c ranged from − 1.1% to − 1.5% [23,24,25,26,27,28].
In the present study, 58.5% and 39.5% of individuals met the target HbA1c < 7.0% with semaglutide and DPP–4i, respectively (Supplementary Table 3). These findings support what has been reported for semaglutide in the SURE studies, where a pooled analysis of real-world data from the UK, Canada, Switzerland, and Denmark/Sweden showed 52.6% of individuals achieved HbA1c < 7.0% [29]. Interim results from the ongoing SEPRA pragmatic trial show a comparable proportion of individuals achieving HbA1c < 7.0% at 1 year [30]. The long-term clinical outcomes associated with persistence with semaglutide complement findings from clinical trials and real-world studies, indicating that initial reductions in HbA1c and BMI achieved at 6 months to 1 year are sustained up to 2 years.
Long-term persistent semaglutide users were less likely to require treatment intensification, and fewer users added new glucose-lowering treatments or initiated insulin compared with persistent DPP–4i users. Similarly, fewer users of semaglutide required treatment augmentation vs any other comparator in clinical trials and real-world studies. In the SEPRA pragmatic trial, fewer semaglutide users added a new glucose-lowering treatment at 1 year [30]. At 104 weeks in the SUSTAIN 6 study, fewer individuals added a new glucose-lowering medication or initiated insulin with semaglutide vs placebo [31]. Consistent with the glycemic control achieved and maintained with persistence with semaglutide, these findings emphasize the durability of treatment efficacy of semaglutide.
In the SUSTAIN trials, subgroup analyses based on baseline HbA1c consistently demonstrate that semaglutide is more effective than other comparators [32,33,34]. In the present study, results from the baseline HbA1c ≥ 7.0% and semaglutide 1 mg subgroup analyses were similar to the observations from the larger cohorts; however, subgroup analyses were not weighted or adjusted for covariates. Because the DPP–4i population was weighted toward the semaglutide population, unobserved selection bias may exist in the final sample. In addition, the comparative rates of insulin initiation were not statistically significant. This study may not be sufficiently powered to detect differences in insulin initiation; the rates of insulin initiation observed for both semaglutide and DPP–4i users at the end of the study were markedly lower than what has been reported in the literature [31].
Weight loss with semaglutide has been consistently shown in clinical trials and real-world studies. Although semaglutide was associated with significant reductions in BMI compared with DPP–4i, the present study evaluated BMI outcomes based on estimates derived from ICD-10-CM codes; therefore, comparisons with other studies using absolute weight and BMI measures should be interpreted with caution. Additional analyses are needed to evaluate real-world, long-term weight loss outcomes with semaglutide vs DPP–4i.
Because of the progressive nature of T2D, individuals will often require treatment intensification to achieve and maintain therapeutic goals [3, 35]. The key drivers of improved long-term outcomes are greater reductions in HbA1c and BMI [36]. The consistency in HbA1c reductions at 2 years in the present study and the observations at multiple time points in clinical trials and real-world studies is indicative of sustained glycemic control. The increased odds of achieving glycemic targets and the reduced likelihood of treatment intensification reported here suggest improved durability of semaglutide vs DPP–4i and suggest that long-term persistence with semaglutide may help to alleviate treatment complexity associated with polypharmacy and increased medication load and reduce end-organ complications long-term. In addition, a lesser need for treatment intensification with insulin may translate to a reduced risk of hypoglycemia and weight gain. The improved glycemic control coupled with reduced BMI observed here is perfectly aligned with the current American Diabetes Association standard of care recommendations [3], emphasizing the importance of optimizing the use of semaglutide in clinical practice.
This study has several limitations. First, as a result of the nature of study design, although associations can be directly assessed, causality requires additional assumptions that the study design attempts to address but may not fully meet. Second, some key factors (e.g., granular clinical details) may not be captured or may have missing data in the database, which may result in residual confounding. Additionally, comparing weight loss outcomes of the present study with clinical trials was limited, as absolute weight measures were not available. This study estimated the BMI continuous variable as the midpoint of the value range for the corresponding BMI code; therefore, future studies on weight changes and weight targets are warranted. Third, generalizability of these findings may be limited, as the database includes commercial and Medicare Advantage health plan enrollees. Fourth, some inclusion criteria may cause selection bias; the bias may result in individuals being selected who better manage their health or receive better care owing to the requirement for persistent utilization and collection of both baseline and follow-up HbA1c and BMI data. Fifth, some outcomes/variables may have measurement errors, such as misclassification of billing codes. Sixth, we may not have adequate sample sizes to detect differences between the groups in subgroup and sensitivity analyses especially for insulin initiation, which may warrant future research.
Conclusion
Overall, persistent use of semaglutide was associated with significant improvements in glycemic and weight control that were maintained after 2 years. Compared with DPP–4i users, semaglutide users experienced more substantial reductions in HbA1c and BMI and reduced risks of treatment augmentation after 2 years of persistent use. The real-world evidence presented here complements both randomized clinical trials and real-world studies. These findings may inform routine clinical decision making and encourage adoption and effective management of semaglutide for long-term use to achieve better outcomes in the T2D population.
Data Availability
The data used in this study were provided by Optum, Inc. There are restrictions on the availability of these data, which were used under license for this study and therefore are not publicly available. Requests may be sent to Optum, Inc for more information on data availability and licensing.
References
ElSayed NA, Aleppo G, Aroda VR, et al. 2. Classification and Diagnosis of Diabetes: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S19–40. https://doi.org/10.2337/dc23-S002.
Type 2 diabetes. Centers for Disease Control and Prevention. Updated December 30, 2022. https://www.cdc.gov/diabetes/basics/type2.html. Accessed Aug 4, 2023.
ElSayed NA, Aleppo G, Aroda VR, et al. 9. Pharmacologic Approaches to Glycemic Treatment: Standards of Care in Diabetes-2023. Diabetes Care. 2023;46(Suppl 1):S140–57. https://doi.org/10.2337/dc23-S009.
Ozempic. Prescribing Information. Novo Nordisk Inc.; 2022.
Sorli C, Harashima SI, Tsoukas GM, et al. Efficacy and safety of once-weekly semaglutide monotherapy versus placebo in patients with type 2 diabetes (SUSTAIN 1): a double-blind, randomised, placebo-controlled, parallel-group, multinational, multicentre phase 3a trial. Lancet Diabetes Endocrinol. 2017;5(4):251–60. https://doi.org/10.1016/S2213-8587(17)30013-X.
Ahren B, Masmiquel L, Kumar H, et al. Efficacy and safety of once-weekly semaglutide versus once-daily sitagliptin as an add-on to metformin, thiazolidinediones, or both, in patients with type 2 diabetes (SUSTAIN 2): a 56-week, double-blind, phase 3a, randomised trial. Lancet Diabetes Endocrinol. 2017;5(5):341–54. https://doi.org/10.1016/S2213-8587(17)30092-X.
Ahmann AJ, Capehorn M, Charpentier G, et al. Efficacy and safety of once-weekly semaglutide versus exenatide ER in subjects with type 2 diabetes (SUSTAIN 3): a 56-week, open-label, randomized clinical trial. Diabetes Care. 2018;41(2):258–66. https://doi.org/10.2337/dc17-0417.
Aroda VR, Bain SC, Cariou B, et al. Efficacy and safety of once-weekly semaglutide versus once-daily insulin glargine as add-on to metformin (with or without sulfonylureas) in insulin-naive patients with type 2 diabetes (SUSTAIN 4): a randomised, open-label, parallel-group, multicentre, multinational, phase 3a trial. Lancet Diabetes Endocrinol. 2017;5(5):355–66. https://doi.org/10.1016/S2213-8587(17)30085-2.
Lingvay I, Catarig AM, Frias JP, et al. Efficacy and safety of once-weekly semaglutide versus daily canagliflozin as add-on to metformin in patients with type 2 diabetes (SUSTAIN 8): a double-blind, phase 3b, randomised controlled trial. Lancet Diabetes Endocrinol. 2019;7(11):834–44. https://doi.org/10.1016/S2213-8587(19)30311-0.
Pratley RE, Aroda VR, Lingvay I, et al. Semaglutide versus dulaglutide once weekly in patients with type 2 diabetes (SUSTAIN 7): a randomised, open-label, phase 3b trial. Lancet Diabetes Endocrinol. 2018;6(4):275–86. https://doi.org/10.1016/S2213-8587(18)30024-X.
Rodbard HW, Lingvay I, Reed J, et al. Semaglutide added to basal insulin in type 2 diabetes (SUSTAIN 5): a randomized controlled trial. J Clin Endocrinol Metab. 2018;103(6):2291–301. https://doi.org/10.1210/jc.2018-00070.
Zinman B, Bhosekar V, Busch R, et al. Semaglutide once weekly as add-on to SGLT-2 inhibitor therapy in type 2 diabetes (SUSTAIN 9): a randomised, placebo-controlled trial. Lancet Diabetes Endocrinol. 2019;7(5):356–67. https://doi.org/10.1016/S2213-8587(19)30066-X.
Capehorn MS, Catarig AM, Furberg JK, et al. Efficacy and safety of once-weekly semaglutide 1.0mg vs once-daily liraglutide 1.2mg as add-on to 1–3 oral antidiabetic drugs in subjects with type 2 diabetes (SUSTAIN 10). Diabetes Metab. 2020;46(2):100–9. https://doi.org/10.1016/j.diabet.2019.101117.
Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15(6):e22–33.
Uzoigwe C, Noone J, Liang M, et al. Persistency with GLP-1RA compared with DPP-IVi use on glycemic control and health care costs. JMCP. 2023;29(10-a):S1-S147. Association of Managed Care Professionals 2023 abstract E4.
Grade Study Research Group, Nathan DM, Lachin JM, et al. Glycemia reduction in type 2 diabetes - glycemic outcomes. N Engl J Med. 2022;387(12):1063–1074. https://doi.org/10.1056/NEJMoa2200433.
Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–9. https://doi.org/10.1016/0895-4356(92)90133-8.
Glasheen WP, Cordier T, Gumpina R, Haugh G, Davis J, Renda A. Charlson Comorbidity Index: ICD-9 update and ICD-10 translation. Am Health Drug Benefits. 2019;12(4):188–97.
Glasheen WP, Renda A, Dong Y. Diabetes Complications Severity Index (DCSI)-update and ICD-10 translation. J Diabetes Complications. 2017;31(6):1007–13. https://doi.org/10.1016/j.jdiacomp.2017.02.018.
Young BA, Lin E, Von Korff M, et al. Diabetes complications severity index and risk of mortality, hospitalization, and healthcare utilization. Am J Manag Care. 2008;14(1):15–23.
Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–79. https://doi.org/10.1002/sim.6607.
Lingvay I, Kirk AR, Lophaven S, Wolden ML, Shubrook JH. Outcomes in GLP-1 RA-experienced patients switching to once-weekly semaglutide in a real-world setting: the retrospective, observational expert study. Diabetes Ther. 2021;12:879–96.
Napoli R, Berra C, Catarig AM, et al. Once-weekly semaglutide use in patients with type 2 diabetes: real-world data from the SURE Italy observational study. Diabetes Obes Metab. 2023;25(6):1658–67. https://doi.org/10.1111/dom.15020.
Rudofsky G, Catarig AM, Favre L, et al. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: results from the SURE Switzerland multicentre, prospective, observational study. Diabetes Res Clin Pract. 2021;178:108931. https://doi.org/10.1016/j.diabres.2021.108931.
Yale JF, Catarig AM, Grau K, et al. Use of once-weekly semaglutide in patients with type 2 diabetes in routine clinical practice: results from the SURE Canada multicentre, prospective, observational study. Diabetes Obes Metab. 2021;23(10):2269–78. https://doi.org/10.1111/dom.14468.
Holmes P, Bell HE, Bozkurt K, et al. Real-world use of once-weekly semaglutide in type 2 diabetes: results from the SURE UK multicentre, prospective, observational study. Diabetes Ther. 2021;12(11):2891–2905. https://doi.org/10.1007/s13300-021-01141-8.
Bellido V, Abreu Padin C, Catarig AM, Clark A, Barreto Pittol S, Delgado E. Once-weekly semaglutide use in patients with type 2 diabetes: results from the SURE Spain multicentre, prospective, observational study. J Clin Med. 2022. https://doi.org/10.3390/jcm11174938.
Rajamand Ekberg N, Bodholdt U, Catarig AM, et al. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: results from the SURE Denmark/Sweden multicentre, prospective, observational study. Prim Care Diabetes. 2021;15(5):871–8. https://doi.org/10.1016/j.pcd.2021.06.008.
Yale JF, Bodholdt U, Catarig AM, et al. Real-world use of once-weekly semaglutide in patients with type 2 diabetes: pooled analysis of data from four SURE studies by baseline characteristic subgroups. BMJ Open Diabetes Res Care. 2022. https://doi.org/10.1136/bmjdrc-2021-002619.
Buse JB, Soule BP, Harty BJ, et al. 776-P: Comparative effectiveness of SC semaglutide in adults with T2D in US routine clinical practice—year 1 results of SEPRA, a randomized pragmatic clinical trial. Diabetes. 2023. https://doi.org/10.2337/db23-776-P.
Marso SP, Bain SC, Consoli A, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375(19):1834–44. https://doi.org/10.1056/NEJMoa1607141.
Leiter L, Charpentier G, Chaykin L, et al. Semaglutide reduces body weight across baseline BMI subgroups across SUSTAIN 1–5. Can J Diabetes. 2017;41(5):S6.
Bain S, Araki E, Desouza C, et al. Semaglutide reduces HbA1c across baseline HbA1c subgroups across SUSTAIN 1–5 clinical trials. Diabetes. 2017:66(Suppl 1):A298–A299.
Viljoen A, Bluher M, Chow FC, et al. Semaglutide reduces body weight vs. dulaglutide across baseline BMI subgroups in SUSTAIN 7. Diabetes. 2018;67(Suppl_1):1083-P.
Davies MJ, D'Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;41(12):2669–2701. https://doi.org/10.2337/dci18-0033.
Viljoen A, Hoxer CS, Johansen P, Malkin S, Hunt B, Bain SC. Evaluation of the long-term cost-effectiveness of once-weekly semaglutide versus dulaglutide for treatment of type 2 diabetes mellitus in the UK. Diabetes Obes Metab. 2019;21(3):611–21. https://doi.org/10.1111/dom.13564.
Acknowledgements
Medical Writing/Editorial Assistance
The authors would like to acknowledge Victoria Jeter, PhD, of PRECISIONscientia in Yardley, Pennsylvania for medical writing support, as well as Ryan Ross, MS, of Merative LP in Cambridge, Massachusetts for statistical consulting support, which was funded by Novo Nordisk Inc.
Funding
Funding for this study and the rapid service fee was provided by Novo Nordisk Inc.
Author information
Authors and Affiliations
Contributions
Xi Tan, Yuanjie Liang, Cory Gamble, and Aaron King were involved in the concept and design of the study. Yuanjie Liang performed data analysis. Xi Tan, Yuanjie Liang, Cory Gamble, and Aaron King were involved in data interpretation. Xi Tan, Yuanjie Liang, Cory Gamble, and Aaron King contributed to reviewing, editing, and approving the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Xi Tan, Yuanjie Liang, and Cory Gamble are employees of Novo Nordisk Inc. Aaron King is an employee of Baptist Medical Network MedFirst Primary Care–Quarry, and he serves as the consultant/speaker for Abbott, Astellas, Dexcom, Eli Lilly, Mannkind, and Novo Nordisk Inc.
Ethical Approval
The claims data assessed were in accordance with Health Insurance Portability and Accountability Act. This study was exempt from institutional review board review because this study was not classified as research involving human subjects. Database access and use of the data analyzed in this study were permitted by Optum, Inc. This study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments. All authors meet the International Committee of Medical Journal Editors criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for the version to be published.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Tan, X., Liang, Y., Gamble, C. et al. Durability of Effectiveness Between Users of Once-Weekly Semaglutide and Dipeptidyl Peptidase 4 Inhibitors (DPP–4i) in US Adults with Type 2 Diabetes. Diabetes Ther 15, 427–445 (2024). https://doi.org/10.1007/s13300-023-01509-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01509-y