Abstract
Introduction
In recent years, the role of pharmacists has undergone significant transformation to become more patient-centered and involved in managing chronic diseases. Nonetheless, it remains unclear whether pharmacist involvement in diabetes management is cost-effective. This study aimed to systematically review the cost-effectiveness and reporting quality in comprehensive economic evaluations of pharmacist management compared to standard care in diabetes.
Methods
Eligible studies included cost-effectiveness analyses employing pharmacist professional services as the intervention for diabetes. A literature search was conducted in the bibliographic databases Pubmed, Scopus, China National Knowledge Infrastructure (CNKI), and the International Health Technology Assessment (HTA) database from their inception until July 2023. Two independent reviewers performed title, abstract, full-text screening, and data abstraction and assessed the quality of reporting and methodological approaches using the Consolidated Health Economic Evaluation Reporting Standards (CHEERS 2022) checklists.
Results
Twelve studies were identified with an average research quality score of 19.8, including cost-utility (n = 5) and cost-effectiveness (n = 7) analyses, with only four studies rated as high quality. The efficacy data were derived from randomized controlled trials (n = 7), retrospective studies (n = 2), and published literature sources (n = 2). Half of the included studies were conducted in high-income countries, while the other half was in upper-middle and lower-middle-income countries, respectively. Despite significant variations in the cost of pharmacist intervention, consistent findings demonstrate that pharmacist involvement in diabetes management is more cost-effective or even cost-saving than standard care, primarily attributed to better glycemic control, enhanced patient compliance, and reduced risks of medication-related problems.
Conclusion
This systematic review substantiates that pharmacist involvement in diabetes management is cost-effective compared with standard care. However, the overall quality of reporting needs to be improved, and high-quality evidence is urgently needed to support healthcare decision-making in pharmacy practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Effective and comprehensive management strategies are crucial in reducing complications and healthcare costs related to diabetes. |
Little is currently known about whether the integration of pharmacists into diabetes management can yield more cost-effective results than conventional physician–nurse collaboration. |
What was learned from the study? |
The integration of pharmacists into a diabetes management team can improve cost-effectiveness. |
The overall quality of research warrants improvement, especially in methodology and reporting standards. |
There is an urgent need for high-quality research to provide robust evidence on the cost-effectiveness of pharmacist interventions, facilitating the implementation of charging policies and promoting the expansion of pharmacy practice in diabetes. |
Introduction
Diabetes is characterized by a high prevalence, extended treatment periods, and numerous complications, which impose a substantial economic burden on this patient population. According to the 10th edition of the Diabetes Atlas published by the International Diabetes Federation in 2021 [1], China has become the country with the largest number of patients with diabetes, and effective management of diabetes in primary care has emerged as a formidable challenge. Current evidence suggests that medical management expenditure before the onset of diabetic complications accounted for 8.5% of Chinese national health expenditure [2]. In China, chronic complications affect approximately 73.2% of individuals with diabetes and contribute to over 80% of total medical spending for this population [3].
It is now understood that comprehensive and integrated healthcare is crucial for mitigating diabetes and its complications. Mere diagnosis and treatment are insufficient. Effective diabetes management implementation can lower the risk of complications. Therefore, optimal management patterns of diabetes play an essential role in preventing and treating the disease and its associated complications. Research has demonstrated that implementing diabetes self-management education and support plays a pivotal role in ameliorating the dire situation concerning the prevention and control of its complications [4]. This intervention enhances patient satisfaction and health outcomes and exhibits cost-effectiveness by mitigating emergency department visits, hospitalizations, and readmissions [5, 6].
However, the scarcity of primary care providers and endocrinologists, coupled with the substantial time required for managing complex diabetic complications, makes it challenging to provide comprehensive management, given that providers have little time to devote to every patient. In addition, patients with diabetes may have comorbidities that require special attention, such as mental illness or pregnancy, which further adds to the complexity of the care required. Additional obstacles associated with diabetes control encompass suboptimal medication adherence, intricate treatment regimens, medication side effects, inadequate doctor–patient communication, and patient financial constraints. As integral healthcare team members, pharmacists can leverage their professional expertise and work synergistically with physicians and nurses to actively contribute to the management of patients with diabetes.
The American Diabetes Association’s consensus on self-management education for patients with type 2 diabetes (T2D) highlights the crucial role of pharmacists as integral members of the diabetes care team [4]. Interestingly, in the USA, pharmacists can acquire prescription privileges through collaborative drug therapy management agreements, enabling them to initiate, discontinue, or modify drug treatment plans [7]. Pharmacists can deliver personalized education on medication timing, administration, and adherence while considering the intricacy of medication regimens and the risks associated with polypharmacy and poor adherence in patients with diabetes. Consequently, this leads to improved medication compliance, reduced occurrences of adverse drug reactions, decreased hospital readmission rates, and lowered medical expenses [8]. This approach has emerged as one of the most efficacious tools for controlling pharmaceutical expenditures and enhancing healthcare quality within American insurance systems. Furthermore, a multicenter randomized controlled trial (RCT) research conducted in Asia demonstrated that pharmacist involvement in multidisciplinary collaborative care enhances blood glucose control levels and patient quality of life, alleviates doctors’ workload, and mitigates medical costs [9].
In light of the escalating burden of diabetic complications and limited medical resources, addressing the soaring healthcare costs and alleviating the economic strain on patients has emerged as an urgent issue that necessitates resolution. Consequently, significant emphasis has been placed on whether pharmacist involvement in diabetes management can yield favorable economic outcomes. This systematic review sought to quantitatively assess the quality of economic evaluations and summarize the health benefits, costs, and cost-effectiveness associated with pharmacist participation in diabetes management, providing a reference for payers and policymakers to design reimbursement processes supporting pharmacists for the optimal management of this patient population.
Methods
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [10] and referred to relevant previous studies [11]. The population, intervention, comparator, outcome, and study (PICOS) criteria used to guide the search strategy were as follows:
-
Population: diabetes, including type 1 and 2.
-
Intervention: pharmacists provide professional services, including medication review, education, treatment management, and pharmaceutical care to address drug-related problems in patients, with subsequent interventions based on follow-up outcomes.
-
Comparator: standard care.
-
Outcome: cost, life gain year (LYG), quality-adjusted life year (QALY), incremental cost-effective ratio (ICER), and incremental cost-utility ratio (ICUR).
-
Study design: cost-effectiveness analysis (CEA) and cost-utility analysis (CUA).
Search Strategy and Selection
No protocol was registered for this review. Online databases, including PubMed, Scopus, China National Knowledge Infrastructure (CNKI), International Health Technology Assessment (HTA), and The National Institute for Health and Care Research (NIHR), were searched from inception up to July 2023. Retrieval words were applied with “diabetes”, “pharmaceutical care”, “pharmacist”, “economic evaluation”, “cost-effectiveness”, “cost-utility”, and synonyms for each of these search terms. Detailed electronic search strategies were presented in Supplementary Table S1. Two investigators (JZ, YZ) assessed all articles for inclusion and exclusion criteria (Supplementary Table S2), and disagreements were resolved through discussions with a third investigator (GW).
Data Extraction
Two researchers (JZ, YZ) independently screened the literature and extracted relevant data. The extracted data included the first author, publication year, country, study design, pharmaceutical care type, research perspective, currency, pharmacist’s hourly salary and year, cost, effectiveness, and ICER /IUER, etc. Points of disagreement were resolved by a discussion or consultation with a third researcher (GW). To ensure comparability of costs across studies, pharmaceutical care costs were converted to US dollars for 2023 using the Campbell and Cochrane Economic Methods Group and Education Programme Policy Initiative (CCEMG-EPPI) Center Cost Converter version 1.6 [12]. The results were categorized according to the type of health economic research and presented in tabular form.
Quality Assessment Reporting
The quality of the included studies was assessed by the Consolidated Health Economic Evaluation Reporting Standards (CHEERS 2022) checklist [13]. The assessment involved 28 items grouped into six domains (Title and Abstract, Introduction, Methods, Results, Discussion, and Others). Each item was scored as “Yes” = 1 (fully met), “Partly” = 0.5 (partly met), or “NA” = 0 (not applicable). Total scores for each study were tallied to determine quality strata: high quality for scores > 21, moderate quality for scores ranging from 14 to 21, and poor quality for scores < 14 [14].
Ethical Approval
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Results
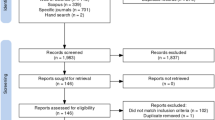
Study Selection
The literature search and screening process is illustrated in Fig. 1. A total of 718 articles were retrieved from the literature, and after removal of duplicate articles (n = 38), 615 were excluded during the title and abstract screening. Following full-text screening, an additional 53 articles were excluded. Ultimately, 12 studies met the inclusion criteria and were included in this systematic review.
Quality of Reporting
Quality assessment of the included studies is shown in Fig. 2. The overall quality of the studies was modest, with a mean quality score of 19.8 (Supplementary Table S3). Most of the studies (7/12, 58.3%) were rated as moderate quality [15,16,17,18,19,20,21], only four studies were ranked as high quality (4/12, 33.3%) [22,23,24,25], and one was poor quality [26].
According to the CHEERS 2022 evaluation standard, the average score for each item was 0.71. Five evaluation items fully satisfied the checklist, including item 3 (Background and objectives), item 6 (Setting and location), item 7 (Comparators), item 9 (Time horizon), item 11 (Selection of outcomes), and item 23 (Summary of main results). However, there were three quality assessment items that no study met: item 19 (Characterizing distributional effects), item 21 (Approach to engagement with patients and others affected by the study), and item 25 (Effect of engagement with patients and others affected by the study).
Characteristics of Included Studies
The characteristics of the included studies are summarized in Table 1.
Study Type
The studies included in the review included CUA and CEA. Five studies (41.7%) conducted CUA with cost and QALYs as the outcome measures [15, 18, 20, 21, 26], while seven studies (7/12, 58.3%) performed CEA [16, 17, 19, 22,23,24,25].
Setting and Location
Five studies were in a primary healthcare setting [17, 18, 20, 22, 24], and two were in a tertiary healthcare [16, 26]. Two studies were performed in the US Veterans Affairs Health System [19, 23], and two were in the community pharmacies [15, 25]. One study did not specify its setting [21].
Six studies were conducted in high-income countries (Australia [15], USA [19, 22, 23], Canada [18], Singapore [20]), three were in upper-middle-income countries (Brazil [17], Malaysia [24], China [26]), and three in lower-middle-income countries (Nigeria [16], Jordan [21], Iran [25]).
Perspective
From the perspective of economic analysis design, the payer perspective was most commonly used (3/12, 25%) [18, 21, 22, 25], and other perspectives included those of the healthcare system (2/12, 16.7%) [15, 17], healthcare providers (2/12, 16.7%) [20, 24], and patients (1/12, 8.3%) [16]. One study used multiple perspectives, including those of the healthcare system, healthcare providers, and payers [23], while two studies did not specify any perspective [19, 26].
Study Design
Seven studies were designed as RCTs, four of which were multicenter [15,16,17,18], and two were single-center [24, 26]. The remaining three were retrospective cohorts [19, 22, 23], and two were based on published literature [21, 25]. Half of the studies (6/12, 50%) used models to simulate long-term outcomes; four were based on Markov models [21, 22, 24, 25], and two on Archimedes models [19, 23].
Sensitivity Analysis
Sensitivity analyses were conducted in all articles except for two [17, 26]. Four of these studies exclusively performed deterministic sensitivity analysis (DSA) [15, 19] or probabilistic sensitivity analysis (PSA) [18, 20], while the remaining six studies employed both DSA and PSA [16, 21,22,23,24,25]. Regarding the DSA variables mentioned above, all studies included the cost of pharmacist intervention. Nevertheless, only three studies performed DSA on indicators of intervention effectiveness [19, 23, 25].
Cost
None of the studies included a social perspective, leading to the exclusion of indirect costs due to productivity loss. Direct medical costs reported mainly comprised pharmaceutical care, healthcare resources, medications, laboratory tests, and diabetic complications.
The cost of pharmaceutical care was considered by most of the included studies (11/12, 91.7%), except for one study [16] (Table 2). Half of these studies were estimated by labor costs, which refers to the remuneration for pharmacists providing pharmaceutical care. Labor costs were calculated by multiplying the pharmacist’s hourly wage by the number of hours. However, there was a significant disparity in hourly wages for pharmacists across countries. Upon converting the reported wages to 2023 US dollars (USD), the hourly wages for pharmacists ranged from 48.9 to 71.5 USD per hour in high-income countries such as Australia, Canada, and the USA [15, 18, 22], while it was only 6.3 USD per hour in upper-middle-income countries like Malaysia [24]. The other two studies from China [26] and the USA [19] did not report specific wages.
Besides, some studies used either the cost of a single visit by a pharmacist or the hourly cost of pharmacist visits as indicators for estimating the cost of pharmacist-led interventions. In Singapore, the cost of the pharmacist-led intervention was 7.5–14.1 USD per visit [20]; in Jordan and the USA, it was 25.2–67.3 USD per hour [21] and 77.7 USD per hour [23], respectively. The Iranian study did not disclose the specific fees charged for pharmacist services [25]. A study from Brazil showed that the average cost per patient for a pharmacist appointment was 3.9 USD (undiscounted) [17].
There were six long-term studies based on model simulations that included complication costs. Of these studies, three considered only coronary heart disease and stroke [21, 22, 24], while the remaining three employed Archimedes modeling to consider common macrovascular and microvascular complications of diabetes [19, 23, 25].
Effectiveness
Hemoglobin A1c (HbA1c) was the commonly used effectiveness measurement to evaluate the cost-effectiveness of pharmacist-led interventions in diabetes (Table 3). Short-term studies (less than 1 year) have shown that the pharmacist-led care group exhibited a significantly greater improvement in HbA1c levels compared to the standard care group (mean difference 0.43%, 95% CI 0.34–0.52) [15]. This intervention not only resulted in a higher proportion of patients achieving HbA1c improvement (HbA1c reduction ≥ 0.1% from baseline) [20] but also achieved higher rates of HbA1c compliance (49.53% vs 72.88%, p < 0.01) [26].
The other two studies utilized LYG and predicted 10-year cardiovascular disease risk [calculated using the United Kingdom Prospective Diabetes Study (UKPDS) Risk Engine] as the measure of long-term effect in the cost-effectiveness analysis, respectively. Pharmacist-led care resulted in a statistically significant reduction in the annual risk of cardiovascular events (mean difference 0.26%, 95% CI 0.08–0.63%) [18] and an increase of 0.29 LYG [21] compared to the standard care group.
The remaining cost-utility analyses employed QALYs as the measure of effectiveness, with two RCTs utilizing the Health Utilities Index (HUI2 and HUI3) [27] and the Malaysian EuroQol-5D-5L questionnaire [28] to access the health-related quality of life. Two cost-utility analyses using Archimedes’ model did not report explicit utility parameters, and the utility values for the other studies were taken from the literature. These studies consistently showed that pharmacist-led care provided a greater average gain in QALYs than standard care.
Cost-Effectiveness Analyses
Despite considerable heterogeneity across cost categories, all included studies consistently concluded that pharmacist-led care was either cost-effective or dominant (both cost-saving and more effective) in certain cases.
Half of the health economic evaluations demonstrated that pharmacist-led care was the dominant strategy, with both cost-saving and effectiveness compared to standard care. Despite an increase in costs associated with pharmacist visits, these expenses were counterbalanced by savings in medication, specialist visits, hospitalization, and diabetic complications, resulting in overall lower total costs than those observed in the standard care control group. The remaining studies indicate that pharmacist care is cost-effective, with reported incremental costs per QALY falling below the national willingness-to-pay threshold.
Discussion
This study aimed to systematically evaluate the cost-effectiveness of pharmacist involvement in diabetes care compared to standard care, which assessed the economic advantages of pharmaceutical care by analyzing the relationship between its inputs and outputs. A total of 12 studies from 10 countries were included in this review. Our results indicated that patients with diabetes receiving care from pharmacists can yield positive economic benefits in both high-income and low- and middle-income countries. Accordingly, pharmacists could play important roles in conserving healthcare resources by significantly improving clinical outcomes and reducing healthcare utilization.
In Chinese primary healthcare institutions, the shortage of medical staff and limited supply of prescription drugs have made the hospital-centered diabetes management model predominant. This differs from high-income countries where community-based management models prevail. While hospital-centered diabetes management ensures comprehensive treatment for patients, it also has significant drawbacks. Physicians in tertiary hospitals are overburdened and may struggle to follow up with patients and achieve management goals, potentially resulting in suboptimal long-term management of diabetes.
Given the increasing demand for medical services and the inequitable allocation of resources within healthcare systems, it is imperative to establish a multidisciplinary model involving pharmacists and medical personnel to manage patients actively. A study on a collaborative management model involving Chinese pharmacists and medical staff demonstrated that patients better received medication guidance provided by pharmacists during medication follow-up [29]. This allows them to leverage their professional strengths and plays a crucial role in standardizing patients’ medication usage while reducing healthcare costs. From the perspective of our included studies, most investigations adopted a payer and medical system standpoint, implying that pharmacists’ provision of pharmaceutical care in healthcare institutions may yield favorable outcomes for controlling medical insurance costs.
Moreover, approximately half of the included studies used a randomized controlled design and applied health economic models to simulate the long-term cost-effectiveness of pharmacist-led care in diabetes. However, there is still considerable scope for enhancing the quality of research in this domain based on the CHEERS scores. Specifically, improvements are warranted in the following areas.
When calculating the cost of pharmaceutical care, most studies typically consider only direct costs and quantify them in terms of pharmacists’ salaries or the corresponding value of pharmaceutical care provided, which may be attributed to the immaturity of fee-for-service systems for pharmaceutical care in certain countries, including China, or challenges associated with data acquisition. Consequently, when conducting cost-effectiveness analysis for pharmacist-led care, most cost measurements were based on the average salary of pharmacists. In addition, all included studies did not consider the costs of preventing adverse drug events. However, studies have shown that pharmacist interventions for medication-related problems in patients with chronic illnesses are cost-effective and generate significant savings, resulting in an annual net benefit of 64,393 USD for healthcare payers [30]. Pharmacist-led care can reduce healthcare expenses by providing rational medication recommendations, discontinuing unnecessary medications, substituting cheaper alternatives, and decreasing the occurrence of adverse drug reactions.
The included studies used Archimedes and Markov models to evaluate the long-term cost-effectiveness of pharmacist-led care in diabetes, respectively. The key distinction between these two models lies in the structure of the Markov model, which comprises discrete health states represented by transition probabilities. Conversely, the Archimedes model has no explicit health states, is continuous in time, has no discrete time steps, and any event can occur at any time [31]. While the Archimedes model offers advantages in capturing the continuous trajectory of diabetes and its complications, it suffers from poor transparency and proprietary restraints that limit its replicability and utilization by other researchers. Complications are important in assessing the long-term benefits of diabetes interventions, but their evaluation is often challenging because of the complexity and interaction of risk factors. In recent years, numerous decision models have been developed and validated for the T2D population, with the Center for Outcomes Research (CORE) model emerging as the predominant choice in this field [32]. It provides a more comprehensive assessment of complications in T2D and includes 17 interdependent sub-models for macrovascular, microvascular, and acute complications of diabetes. Therefore, this well-validated and mature decision model for T2D is recommended to fully evaluate the long-term cost-effectiveness of pharmacist-led care.
Only two studies performed subgroup analyses based on baseline HbA1c levels. Future research is warranted to improve the quality of subgroup analyses and explore the variation in cost and effectiveness of pharmacist interventions according to specific characteristics of patients with diabetes. For instance, assessing differences in cost-effectiveness between patients with type 1 diabetes and those with T2D would enable decision-makers to understand the optimal net benefit of pharmacist involvement in diabetes management and assess the value of their investment.
The limitations and shortcomings of this systematic review should be acknowledged. First, subgroup analyses for specific populations could not be conducted because of limited data availability. Therefore, whether pharmacist-led care could be more cost-effective in patients with multiple comorbidities, co-medications, long course of T2D, and other risk factors cannot be verified. Second, heterogeneity in model assumptions, effectiveness indicator setting, and other study characteristics precluded the possibility of conducting quantitative meta-analyses. Third, these included studies were performed in different countries, each with specific healthcare systems, pricing policies, willingness-to-pay thresholds, and health insurance coverage, which might limit the generalizability of our conclusions.
Conclusion
With the global increase in the incidence of diabetes, healthcare expenditures are on the rise, underscoring the importance of assessing whether including pharmacists in diabetes treatment management can alleviate the strain on limited medical resources and simultaneously improve the quality of healthcare services. For pharmacy professionals, it is imperative to demonstrate the value of their participation in diabetes management to patients and the healthcare system, elucidating their income sources and ensuring the sustainability of their services. For decision-makers, there is a need to consider which professional services pharmacists should be funded in this domain and how limited medical resources can be optimally utilized. Although existing research suggests that pharmacists’ engagement in diabetes management is more cost-effective than standard care, our systematic review reveals a lack of conclusive evidence for informed decision-making, emphasizing the need for improved research quality, especially regarding evaluation methodologies and reporting practices. In future studies, researchers should be encouraged to conduct well-designed cost-effectiveness analyses tailored to local contexts, thereby generating high-quality evidence about the cost and effectiveness of pharmacists’ participation in diabetes management, ultimately achieving optimal health benefits.
Data Availability
This article is based upon previously conducted studies, and all data are publicly available in the referenced publications.
References
Sun H, Saeedi P, Karuranga S, et al. IDF diabetes atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183:109119.
Luo Z, Fabre G, Rodwin VG. Meeting the challenge of diabetes in China. Int J Health Policy Manag. 2020;9:47–52.
He X, Zhang Y, Ruan Z, Li L, Jing Wu. The prevalence and related direct medical costs of chronic complications among patients with type 2 diabetes in China. Chin J Endocrinol Metab. 2019;35:200–5.
Powers MA, Bardsley JK, Cypress M, et al. Diabetes self-management education and support in adults with type 2 diabetes: a consensus report of the American Diabetes Association, the Association of Diabetes Care & Education Specialists, the Academy of Nutrition and Dietetics, the American Academy of Family Physicians, the American Academy of PAs, the American Association of Nurse Practitioners, and the American Pharmacists Association. Diabetes Care. 2020;43:1636–49.
Duncan I, Ahmed T, Li QE, et al. Assessing the value of the diabetes educator. Diabetes Educ. 2011;37:638–57.
Nassar CM, Montero A, Magee MF. Inpatient diabetes education in the real world: an overview of guidelines and delivery models. Curr Diab Rep. 2019;19:103.
Orabone AW, Do V, Cohen E. Pharmacist-managed diabetes programs: improving treatment adherence and patient outcomes. Diabetes Metab Syndrome Obesity. 2022;15:1911–23.
Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;28:421–36.
Siaw MYL, Ko Y, Malone DC, et al. Impact of pharmacist-involved collaborative care on the clinical, humanistic and cost outcomes of high-risk patients with type 2 diabetes (IMPACT): a randomized controlled trial. J Clin Pharm Ther. 2017;42:475–82.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Sanyal C, Husereau D. Systematic review of economic evaluations of services provided by community pharmacists. Appl Health Econ Health Policy. 2020;18:375–92.
Campbell and Cochrane Economics Methods Group (CCEMG), Evidence for Policy and Practice Information and Coordinating Centre (EPPI-Centre). CCEMG - EPPI-Centre Cost Converter v.1.4. http://eppi.ioe.ac.uk/costconversion/default.aspx. Accessed 2 June 2023.
Husereau D, Drummond M, Augustovski F, et al. Consolidated health economic evaluation reporting standards (CHEERS) 2022 explanation and elaboration: a report of the ISPOR CHEERS II good practices task force. Value Health. 2022;25:10–31.
Geng J, Yu H, Mao Y, Zhang P, Chen Y. Cost effectiveness of dipeptidyl peptidase-4 inhibitors for type 2 diabetes. Pharmacoeconomics. 2015;33:581–97.
Taylor SJ, Milanova T, Hourihan F, Krass I, Coleman C, Armour CL. A cost-effectiveness analysis of a community pharmacist-initiated disease state management service for type 2 diabetes mellitus. Int J Pharm Pract. 2005;13:33–40.
Adibe MO, Aguwa CN, Ukwe CV. Cost-utility analysis of pharmaceutical care intervention versus usual care in management of Nigerian patients with type 2 diabetes. Value Health Reg Issues. 2013;2:189–98.
Obreli-Neto PR, Marusic S, Guidoni CM, et al. Economic evaluation of a pharmaceutical care program for elderly diabetic and hypertensive patients in primary health care: a 36-month randomized controlled clinical trial. J Manage Care Spec Pharm. 2015;21:66–75.
Simpson SH, Lier DA, Majumdar SR, et al. Cost-effectiveness analysis of adding pharmacists to primary care teams to reduce cardiovascular risk in patients with type 2 diabetes: Results from a randomized controlled trial. Diabet Med. 2015;32:899–906.
Ourth H, Nelson J, Spoutz P, Morreale AP. Development of a pharmacoeconomic model to demonstrate the effect of clinical pharmacist involvement in diabetes management. J Manage Care Spec Pharm. 2018;24:449–57.
Siaw MYL, Malone DC, Ko Y, Lee JY. Cost-effectiveness of multidisciplinary collaborative care versus usual care in the management of high-risk patients with diabetes in Singapore: short-term results from a randomized controlled trial. J Clin Pharm Ther. 2018;43:775–83.
Mousa R, Hammad E. Cost-effectiveness of pharmacist-led care versus usual care in type 2 diabetic Jordanians: a Markov modeling of cardiovascular diseases prevention. Expert Rev Pharmacoecon Outcomes Res. 2021;21:1069–79.
Yu J, Shah BM, Ip EJ, Chan J. A Markov model of the cost-effectiveness of pharmacist care for diabetes in prevention of cardiovascular diseases: evidence from Kaiser Permanente Northern California. J Manage Care Pharm. 2013;19:102–14.
Hirsch JD, Bounthavong M, Arjmand A, et al. Estimated cost-effectiveness, cost benefit, and risk reduction associated with an endocrinologist-pharmacist diabetes intense medical management “tune-up” clinic. J Manage Care Spec Pharm. 2017;23:318–26.
Rosli MR, Wu DB-C, Neoh CF, Karuppannan M. Economic evaluation of home medication review by community pharmacists (HMR-CP) for patients with type 2 diabetes mellitus (T2DM). J Med Econ. 2021;24:730–40.
Amirsadri M, Torkpour E. Cost-effectiveness and cost-utility analysis of type-2 diabetes screening in pharmacies in Iran. Res Pharm Sci. 2023;18:210–8.
Ji C, Rao H, Li L. Cost-effectiveness analysis of “diabetes comprehensive clinic” with the participation of clinical pharmacists in management of diabetic patients. Chin J Clin Pharm. 2022;31:491–4.
Horsman J, Furlong W, Feeny D, Torrance G. The Health Utilities Index (HUI®): concepts, measurement properties and applications. Health Qual Life Outcomes. 2003;1:1–13.
Shafie AA, Vasan Thakumar A, Lim CJ, Luo N, Rand-Hendriksen K, Md Yusof FA. EQ-5D-5L valuation for the Malaysian population. Pharmacoeconomics. 2019;37:715–25.
Feng Yu, Luo D, He K, Zhongshan Xu. Effects of pharmacists and medical staff co-operation on reduction of re-hospitalization and medical expenses of heart failure of patients. Chin J Cardiovasc Med. 2017;22:206–9.
Al-Qudah RA, Al-Badriyeh D, Al-Ali FM, Altawalbeh SM, Basheti IA. Cost–benefit analysis of clinical pharmacist intervention in preventing adverse drug events in the general chronic diseases outpatients. J Eval Clin Pract. 2020;26:115–24.
Li J, Bao Y, Chen X, Tian L. Decision models in type 2 diabetes mellitus: a systematic review. Acta Diabetol. 2021;58:1451–69.
Palmer AJ, Roze S, Valentine WJ, et al. The CORE diabetes model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(Suppl 1):S5-26.
Funding
This study was supported by the Hangzhou special project for Biomedicine and Health industry Development of Science and Technology [Grant No. 2023WJC061], also funded the Rapid Service fees.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Jiejin Zhu, Ying Zhou and Gang Wang; The first draft of the manuscript was written by Jiejin Zhu and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Corresponding author
Ethics declarations
Conflict of Interest
All authors (Jiejin Zhu, Ying Zhou and Gang Wang) declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Ethical Approval
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Zhu, J., Zhou, Y. & Wang, G. Cost-Effectiveness of Pharmacist Care in Diabetes Management: A Systematic Review. Diabetes Ther 15, 61–76 (2024). https://doi.org/10.1007/s13300-023-01505-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01505-2