Abstract
Introduction
Achieving glycemic control can help reduce complications of type 2 diabetes (T2D). This study compared the pharmacy cost per responder and number needed to treat (NNT) of tirzepatide 5 mg, 10 mg, and 15 mg versus semaglutide 1 mg to achieve glycemic, weight loss, and composite treatment endpoints in patients with T2D in the United States.
Methods
The proportions of patients achieving glycemic, weight loss, and composite treatment endpoints were obtained from the phase 3 SURPASS-2 randomized clinical trial which compared tirzepatide 5 mg, 10 mg, and 15 mg to semaglutide 1 mg. Annual pharmacy costs were calculated using 2022 wholesale acquisition costs. Cost per responder and NNT were calculated along with 95% confidence intervals and tests for statistical significance (P ≤ 0.05).
Results
Tirzepatide had a lower cost per responder to achieve glycated hemoglobin A1c (HbA1c) endpoints of ≤ 6.5% (10 mg and 15 mg doses) and < 5.7% (all doses) and weight loss endpoints of ≥ 5% (10 mg and 15 mg doses), ≥ 10% (all doses), and ≥ 15% (all doses). The cost per responder to achieve HbA1c < 7% (all doses of tirzepatide) and ≤ 6.5% (5 mg tirzepatide) were not statistically significantly different between tirzepatide and semaglutide 1 mg. The cost per patient to achieve the composite endpoints (HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 10%/no hypoglycemia) was statistically significantly lower for all doses of tirzepatide than for semaglutide 1 mg. The NNTs for all doses of tirzepatide were statistically significantly lower than that for semaglutide 1 mg to achieve all individual and composite endpoints, with the exception of the 5 mg dose for HbA1c < 7.0% and HbA1c ≤ 6.5%, where tirzepatide had numerically lower NNTs that were not statistically significant.
Conclusion
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist (RA) that may offer the potential to achieve stringent glycemic goals, weight loss targets, and composite treatment goals at a lower cost per responder compared to semaglutide 1 mg among people with T2D.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Many patients with type 2 diabetes (T2D) in the US do not achieve recommended treatment targets. |
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist (RA) indicated as an adjunct to diet and exercise to improve glycemic control in adults with T2D, and has demonstrated superior glycemic efficacy and weight reduction compared with semaglutide 1 mg. |
The objectives of the present study were to compare the cost per responder and number needed to treat (NNT) of tirzepatide and semaglutide 1 mg to achieve glycemic, weight loss, and composite treatment targets in patients with T2D in the United States. |
What was learned from the study? |
Despite a higher annual pharmacy cost, tirzepatide was associated with a lower cost per responder than semaglutide 1 mg for patients with T2D, while offering greater potential to achieve stringent glycemic, weight loss, and composite treatment targets. |
To achieve glycated hemoglobin A1c (HbA1c) endpoints, tirzepatide had a lower cost per responder than semaglutide 1 mg for HbA1c ≤ 6.5% (10 mg and 15 mg) and HbA1c < 5.7% (all doses). The costs per responder to achieve HbA1c < 7.0% (all doses) and HbA1c ≤ 6.5% (5 mg) were not statistically significantly different from the corresponding costs per responder when using semaglutide 1 mg. |
To achieve weight loss endpoints, tirzepatide had a lower cost per responder than semaglutide 1 mg for ≥ 5% weight loss (10 mg and 15 mg), ≥ 10% weight loss (all doses), and ≥ 15% weight loss (all doses). |
All doses of tirzepatide across composite endpoints (HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 10%/no hypoglycemia) had significantly lower costs per responder and NNTs than semaglutide 1 mg, demonstrating that tirzepatide provides better value for achieving lower HbA1c thresholds and weight loss goals without increasing the risk of hypoglycemia. |
Introduction
Diabetes is a complex chronic condition affecting 11.3% of the US population, amounting to 37.3 million people living with diabetes in 2019 [1]. With estimated total combined direct healthcare and lost productivity costs of $327 billion in 2017, diabetes continues to be one of the costliest health conditions in the US [2,3,4]. Type 2 diabetes (T2D) accounts for 90–95% of all diabetes cases [5], and associated microvascular and macrovascular complications have been shown to play an important role in driving long-term costs in patients with T2D [6, 7].
The American Diabetes Association (ADA) clinical practice recommendations identify the achievement of glycemic and weight loss targets as integral to a patient-centered approach to the management of diabetes [8, 9]. Achieving glycemic control (i.e., a glycated hemoglobin A1c (HbA1c) goal of ≤ 6.5 or < 7.0% without significant hypoglycemia for most adults) has been shown to reduce microvascular complications and may reduce long-term cardiovascular disease rates in newly diagnosed patients [8, 10,11,12]. Lower HbA1c values may be beneficial in some patients if achieved safely and without significant hypoglycemia [8, 12]. The benefits of weight loss go beyond glycemic management by improving risk factors for cardiovascular and metabolic disease [9,10,11,12]. Weight loss of 5–10% has been associated with metabolic improvement, while sustained weight loss of ≥ 10–15% may have a disease-modifying effect, leading to improved long-term cardiovascular outcomes and mortality [9,10,11,12].
Treatment of T2D should be tailored to the individual based on comorbidities (e.g., atherosclerotic cardiovascular disease, heart failure, chronic kidney disease) and patient-centered treatment factors [11]. Pharmacologic treatment approaches (i.e., metformin or other agent[s], including combination therapy) should be selected to provide adequate efficacy to achieve and maintain treatment goals. According to the ADA standards of care, weight management is an important part of glucose-lowering management in T2D, and treatment selection should consider weight management goals [11]. Regimens that include agents with high to very high efficacy for glucose lowering and weight loss, such as the glucagon-like peptide 1 receptor agonists (GLP-1 RAs) dulaglutide (high dose) and semaglutide or the glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 RA tirzepatide, typically have a greater likelihood of achieving glycemic and weight management goals [10,11,12].
Tirzepatide is a first-in-class once-weekly GIP/GLP-1 RA that was approved for the treatment of people with T2D in adjunct to diet and exercise, and is currently in phase-3 development for chronic weight management [13, 14]. Tirzepatide has been studied in a wide variety of T2D patient populations in the SURPASS-1 to -5 clinical trial program.
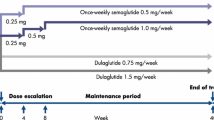
SURPASS-2 was a 40-week phase 3 trial in patients with T2D who were inadequately controlled with metformin, had a HbA1c of 7.0–10.5%, and a body mass index (BMI) of at least 25 kg/m2 that compared one of three once-weekly doses of tirzepatide (5 mg, 10 mg, 15 mg) with once-weekly semaglutide 1 mg [15]. The results of the SURPASS-2 trial showed that at all three doses of tirzepatide were superior to semaglutide 1 mg with respect to mean reduction in HbA1c in patients with T2D who were receiving metformin. Tirzepatide at all three doses was also superior to semaglutide 1 mg with respect to reductions in body weight.
When considering newly available treatment options for patients with T2D, it is important to consider their cost-effectiveness for the management of T2D and relevant outcomes such as glycemic control, effect on weight, and safety (i.e., hypoglycemia risk). Previous studies have assessed the clinical and economic value of the GLP-1 RAs liraglutide [16, 17] and semaglutide [18,19,20], and tirzepatide 10 mg has recently been shown to be cost effective over 1 year compared with semaglutide 1 mg based on a payer willingness-to-pay threshold above $2,247 for a 1% reduction in HbA1c value and $237 for a 1-kg weight loss [21]. However, there has not been any published assessment evaluating the cost of achieving different treatment targets for the management of T2D based on HbA1c and weight with tirzepatide versus relevant GLP-1 RA comparators. The objectives of the present analysis were to evaluate the short-term (1-year) cost-effectiveness of achieving HbA1c, weight loss, and composite treatment outcomes (cost per responder) on tirzepatide 5, 10, and 15 mg versus semaglutide 1 mg and to compare the numbers needed to treat to reach treatment endpoints.
Methods
Clinical Data
Clinical data were obtained from the SURPASS-2 clinical trial [15] and the SURPASS-2 clinical trial post-hoc analysis [22] (See Table S1 in the electronic supplementary material for details). SURPASS-2 was an open-label, 40-week, phase 3 trial (n = 1,879) which randomly assigned patients in a 1:1:1:1 ratio to receive once-weekly subcutaneous injections of either tirzepatide at a dose of 5 mg, 10 mg, or 15 mg or semaglutide at a dose of 1 mg. SURPASS-2 included patients with T2D who were inadequately controlled with metformin, had a HbA1c of 7.0–10.5%, and had a BMI of at least 25 kg/m2. Clinical outcomes included the proportions of patients achieving HbA1c endpoints (< 7.0%, ≤ 6.5%, < 5.7%), weight loss endpoints (≥ 5%, ≥ 10%, ≥ 15%), and composite endpoints (HbA1c < 7.0%, ≤ 6.5%, < 5.7%/weight loss ≥ 10%/no hypoglycemia). HbA1c and weight loss endpoints were prespecified per protocol and based on the treatment-regimen estimand (i.e., treatment effect of tirzepatide or semaglutide, including the effect of any additional antihyperglycemic medication for all patients who underwent randomization, regardless of premature discontinuation of tirzepatide or semaglutide and the use of rescue medication) and the efficacy estimand (i.e., the treatment effect among all patients who underwent randomization had all the patients continued to receive tirzepatide or semaglutide without rescue medication). The composite endpoint of HbA1c ≤ 6.5%/weight loss ≥ 10%/no hypoglycemia was a pre-specified endpoint in the SURPASS-2 trial and was not controlled for the type 1 error rate. The other composite endpoints—HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 5%/no hypoglycemia, HbA1c < 7.0%, or < 5.7%/weight loss ≥ 10%/no hypoglycemia, and HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 15%/no hypoglycemia—were derived from the post-hoc analyses of the SURPASS-2 trial. Hypoglycemia was defined as blood glucose < 54 mg/dL or severe hypoglycemia characterized by an altered mental and/or physical status requiring assistance for treatment of hypoglycemia. All composite endpoints were based on the efficacy estimand.
Cost Data
Pharmacy costs were estimated based on a 28-day supply (4 doses per package) of once-weekly tirzepatide (all doses) [13] and injectable semaglutide 1 mg [23]. Pharmacy package costs were based on wholesale acquisition costs in US dollars ($) from the RED BOOK Online as of October 2022 [24]. Annual pharmacy costs were calculated based on 13.04 (365 days/28 days) packages per year, with per package costs of $974.33 for tirzepatide (all doses) and $892.06 for semaglutide 1 mg and assuming full patient adherence. Any additional use of background therapy was assumed to be identical between the treatments and is therefore not included in the cost estimates. Similarity between the two treatments in the frequency and costs of physician office visits was assumed, so they were not included in the cost estimates. Long-term treatment benefits of macrovascular and microvascular complications are not likely to manifest over the 1-year time horizon, and hence the associated medical costs were not included in the analysis. Given the 1-year time horizon, no discounting was applied.
Short-Term Cost-Effectiveness Analyses
A health economic model was developed in Microsoft Excel (Microsoft, Redmond, WA) to estimate annual pharmacy costs, cost per responder, and number needed to treat (NNT) for tirzepatide (5 mg, 10 mg, 15 mg) and semaglutide 1 mg. Clinical outcomes for HbA1c, weight loss, and composite endpoint thresholds were used to estimate the cost per responder and NNT for treatment with tirzepatide and semaglutide 1 mg. The analysis was conducted from a US healthcare payer perspective over a 1-year time horizon. The model assumed that the levels attained at 52 weeks were the same as the 40-week trial results. This assumption was supported by data from SURPASS-3, where patients were followed for 52 weeks and the HbA1c was visually similar while body weight continued to fall slightly between 40 and 52 weeks [25].
The cost per responder was calculated as the annual pharmacy cost divided by the proportion of patients achieving each endpoint. The NNT was calculated as the reciprocal of the proportion of patients achieving each endpoint (HbA1c, weight loss, or composite) and represents the number of patients that would need to be treated for one patient to achieve each treatment outcome.
A probabilistic sensitivity analysis was conducted in Microsoft Excel with 1,000 trials to estimate 95% confidence intervals. All significance tests were two-sided with an a priori level of significance set at P ≤ 0.05.
Compliance with Ethics Guidelines
This study uses data from a previously conducted clinical trial and published data and does not contain any studies with human participants or animals performed by any of the authors.
Results
Annual Pharmacy Costs
The annual pharmacy cost of once-weekly tirzepatide (5 mg, 10 mg, or 15 mg) was $12,701.09 and $11,628.64 for once-weekly semaglutide (1 mg).
Cost Per Responder
The costs per patient achieving HbA1c endpoints based on the treatment-regimen estimand are shown in Table 1. At the HbA1c < 7.0% threshold, the mean pharmacy cost per responder was numerically higher and not statistically significantly different for all doses of tirzepatide compared with semaglutide 1 mg. Tirzepatide had statistically significantly lower costs per responder to achieve HbA1c ≤ 6.5% (at 10- and 15-mg doses) and HbA1c < 5.7% (at 5-, 10-, and 15-mg doses) than semaglutide 1 mg. The mean costs per patient achieving weight loss endpoints are shown in Table 2. The costs per responder for all tirzepatide doses were statistically significantly lower than those of semaglutide 1 mg across all weight loss thresholds, with the exception of the 5-mg tirzepatide dose at the ≥ 5% weight loss threshold. Cost per responder results for each endpoint based on the efficacy estimand (Table S2 in the electronic supplementary material) were similar to those observed based on the treatment-regimen estimand. The mean cost per responder results for the composite endpoints are shown in Table 3. All doses of tirzepatide across all composite endpoints (HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 10%/no hypoglycemia based on the efficacy estimand) had statistically significantly lower costs per responder than semaglutide 1 mg.
NNT
The number of patients that needed to be treated for one patient to achieve each clinical outcome are shown in Table 4. At the HbA1c < 7.0% and ≤ 6.5% thresholds based on the treatment-regimen estimand, the NNTs for tirzepatide 10 mg and 15 mg were statistically significantly lower than those for semaglutide 1 mg; the NNTs for tirzepatide 5 mg were numerically lower than those of semaglutide 1 mg but the differences were not statistically significant. At the HbA1c < 5.7% threshold, the NNTs for tirzepatide 5 mg, 10 mg, and 15 mg were statistically significantly lower than that for semaglutide 1 mg. The NNTs for all tirzepatide doses were statistically significantly lower than that for semaglutide 1 mg across weight loss thresholds, except for the 5-mg dose at the ≥ 5% weight loss threshold, where there was no statistical difference between treatments. NNT results for each endpoint based on the efficacy estimand (Table S3 in the electronic supplementary material) were similar to those based on the treatment-regimen estimand. All doses of tirzepatide across all composite endpoints (HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 10%/no hypoglycemia based on the efficacy estimand) had a statistically significantly lower NNT than semaglutide 1 mg.
Discussion
The present analysis compared the clinical benefit and economic value of once-weekly tirzepatide (5 mg, 10 mg, and 15 mg) vs once-weekly semaglutide 1 mg among patients with T2D who were inadequately controlled with metformin, had a HbA1c of 7.0–10.5%, and a BMI of at least 25 kg/m2 in terms of achieving glycemic control, weight loss, and composite treatment endpoints using the outcomes data from the pivotal SURPASS-2 clinical trial. The American Association of Clinical Endocrinology, ADA, and European Association for the Study of Diabetes have recognized that achieving HbA1c targets of ≤ 6.5 or < 7.0% (if achieved safely without significant hypoglycemia or other adverse effects) and larger, sustained weight losses (> 10% of baseline weight) can potentially improve long-term outcomes [8,9,10,11,12]; thus, results for composite treatment endpoints with different thresholds for HbA1c reduction and ≥ 10% weight loss with no risk of hypoglycemia provide important insights relevant to the management of diabetes. This analysis showed that despite having a higher annual pharmacy cost, the cost of achieving the triple composite endpoint of HbA1c ≤ 6.5%/≥ 10% weight loss/no hypoglycemia was 26%, 53%, and 60% lower for tirzepatide 5 mg, 10 mg, and 15 mg, respectively, compared with that of semaglutide 1 mg ($53,099). The results also revealed that tirzepatide had a lower cost per responder than semaglutide 1 mg for more stringent treatment goals of HbA1c and weight reduction. At a HbA1c goal of < 7.0%, cost per responder was not statistically different between tirzepatide ($14,734 to $15,489) and semaglutide 1 mg ($14,720). At HbA1c goals of ≤ 6.5% and < 5.7%, cost per responder for tirzepatide ranged from 10% less (10-mg dose at HbA1c ≤ 6.5%) to 55% less (15-mg dose at HbA1c < 5.7%) than for semaglutide 1 mg. For weight loss goals, cost per responder ranged from 23% lower (tirzepatide 10 mg at weight loss ≥ 5%) to 76% lower (tirzepatide 15 mg at weight loss ≥ 15%) than for semaglutide 1 mg.
In this analysis, all tirzepatide doses had numerically lower NNTs to achieve treatment outcomes than semaglutide 1 mg. All doses of tirzepatide across composite endpoints (HbA1c < 7.0%, ≤ 6.5%, or < 5.7%/weight loss ≥ 10%/no hypoglycemia) had a statistically significantly lower NNT than semaglutide 1 mg, demonstrating that tirzepatide provides greater efficacy to achieve lower HbA1c thresholds and weight loss goals without increasing the risk of hypoglycemia.
The differences observed between treatments were more pronounced at more stringent endpoints. At a glycemic goal of HbA1c < 5.7%, the NNTs for tirzepatide 10 mg (2.5) and 15 mg (2.2) were less than half that of semaglutide 1 mg (5.3), meaning that twice as many patients would achieve this endpoint on tirzepatide as on semaglutide 1 mg. The greatest differences between the two agents were observed for the weight loss endpoint of ≥ 15%, where the NNTs for tirzepatide 10 mg (4.2) and 15 mg (2.8) were one-third and one-quarter that of semaglutide 1 mg (12.5), respectively.
This analysis is intended to provide healthcare decision makers with a simple comparison of all doses of tirzepatide and semaglutide 1 mg in terms of achieving different T2D treatment targets and more stringent HbA1c and weight endpoints that may provide additional long-term benefits. The outcomes assessed in this analysis align with current guideline recommendations, recognizing the value of lower glycemic targets and weight loss in a patient-centered approach to T2D management. The findings complement those reported by Zhang and McAdam Marx [21], who concluded that, based on the short-term cost offsets of improved glycemic control and weight loss and the associated downstream benefits, payers may view tirzepatide as a cost-effective treatment in addition to metformin in patients with inadequately controlled T2D who are overweight or obese.
Results of epidemiologic analyses of landmark clinical trials [26, 27] in patients with diabetes suggest that, at a population level, the greatest number of complications will be averted by taking patients from very poor to fair or good glycemic control [26]. The findings indicate that there is no need to deintensify therapy for patients with HbA1c values between 6 and 7% who have a low hypoglycemia risk and long life expectancy. Newer agents such as tirzepatide that have a low incidence of hypoglycemia and positive effects on weight make it possible to maintain glycemic control safely [11, 12, 15] while potentially avoiding microvascular and macrovascular complications and their associated costs in patients with T2D.
The present study analyzed the short-term cost-effectiveness of tirzepatide compared with that of the GLP-1 RA semaglutide 1 mg. One strength of this study is that the clinical data were based on a head-to-head randomized controlled phase 3 trial that compared tirzepatide and semaglutide 1 mg. As this analysis uses a short time horizon of 1 year, only pharmacy costs were included and no assumptions regarding long-term complications or downstream costs were made, thus allowing for a simpler model with greater transparency and replicability. The findings of this short-term analysis can be used to supplement long-term cost-effectiveness studies that estimate total treatment costs and quality-adjusted life years.
Limitations of this analysis include the utilization of a short-term 1-year time horizon. T2D is a chronic condition with patients on long-term treatment. The full clinical impact of T2D, including microvascular and macrovascular events, may require a longer-term horizon. Therefore, this analysis only provides a partial assessment of the value of tirzepatide and should be supplemented with a long-term cost-effectiveness analysis to understand the long-term benefits and costs of treatment. In addition, the analysis only includes patient response and does not include adverse events. However, adverse events with GLP-1 and GIP/GLP-1 RAs primarily involve gastrointestinal upset, which is manageable and time limited in most patients. Costs of managing gastrointestinal events are minimal and may include antiemetics, portion control, or treatment discontinuation. This analysis assumes full patient adherence over the 1-year time horizon; however, real-world patients may not be completely adherent, which could impact both cost and outcomes. Lastly, this analysis utilizes published wholesale acquisition costs that may not be representative of the actual treatment cost to healthcare payers.
Since the publication of the SURPASS-2 study, a semaglutide 2 mg dose has been approved for patients with T2D, but no head-to-head data are currently available to compare semaglutide 2 mg with tirzepatide. Future analyses will be needed to compare the cost-effectiveness of tirzepatide with semaglutide 2 mg.
Conclusion
Tirzepatide, a novel GIP/GLP-1 RA, was associated with a lower cost per responder than semaglutide 1 mg for patients with T2D, while also offering greater potential to achieve stringent glycemic, weight loss, and composite treatment targets. While tirzepatide and semaglutide 1 mg have a similar cost per responder to achieve a HbA1c goal of < 7.0%, tirzepatide provides improved efficacy and better value than semaglutide 1 mg in helping patients achieve lower HbA1c thresholds and weight loss goals without increasing the risk of hypoglycemia. The results of this short-term cost-effectiveness analysis may be helpful to US third-party payers when evaluating new treatment options for patients with T2D who require additional control.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
References
Centers for Disease Control and Prevention. National Diabetes Statistics Report website. https://www.cdc.gov/diabetes/data/statistics-report/index.html. Accessed Oct 5, 2022.
Dieleman JL, Cao J, Chapin A, et al. US health care spending by payer and health condition, 1996–2016. JAMA. 2020;323(9):863–84. https://doi.org/10.1001/jama.2020.0734.
Dieleman JL, Baral R, Birger M, et al. US spending on personal health care and public health, 1996–2013. JAMA. 2016;316(24):2627–46. https://doi.org/10.1001/jama.2016.16885.
American Diabetes Association. Economic costs of diabetes in the U.S. in 2017. Diabetes Care. 2018;41(5):917–28. https://doi.org/10.2337/dci18-0007.
Centers for Disease Control and Prevention. Type 2 diabetes. https://www.cdc.gov/diabetes/basics/type2.html. Accessed Oct 7, 2022.
Visaria J, Iyer NN, Raval AD, et al. Healthcare costs of diabetes and microvascular and macrovascular disease in individuals with incident type 2 diabetes mellitus: a ten-year longitudinal study. Clinicoecon Outcomes Res. 2020;12:423–34. https://doi.org/10.2147/CEOR.S247498.
Wang Y, Zhang P, Shao H, Andes LJ, Imperatore G. Medical costs associated with diabetes complications in Medicare beneficiaries aged 65 years or older with type 2 diabetes. Diabetes Care. 2022;45(11):2570–6. https://doi.org/10.2337/dc21-2151.
ElSayed NA, Aleppo G, Aroda VR, American Diabetes Association, et al. Glycemic targets: standards of care in diabetes-2023. Diabetes Care. 2023;46(Suppl. 1):S97–110. https://doi.org/10.2337/dc23-S006.
ElSayed NA, Aleppo G, Aroda VR, American Diabetes Association, et al. Obesity and weight management for the prevention and treatment of type 2 diabetes: standards of care in diabetes—2023. Diabetes Care. 2023;46(Suppl. 1):S128–39. https://doi.org/10.2337/dc23-S008.
Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753–86. https://doi.org/10.2337/dci22-0034.
ElSayed NA, Aleppo G, Aroda VR, American Diabetes Association, et al. Pharmacologic approaches to glycemic treatment: standards of care in diabetes—2023. Diabetes Care. 2023;46(Suppl. 1):S140–57. https://doi.org/10.2337/dc23-S009.
Blonde L, Umpierrez GE, Reddy SS, et al. American association of clinical endocrinology clinical practice guideline: developing a diabetes mellitus comprehensive care plan-2022 update. Endocr Pract. 2022;28(10):923–1049. https://doi.org/10.1016/j.eprac.2022.08.002. (Published correction appears in Endocr Pract. 2023; 29(1):80–81).
Eli Lilly. Mounjaro (tirzepatide): prescribing information. Indianapolis, IN: Eli Lilly; 2022.
Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med. 2022;387(3):205–16. https://doi.org/10.1056/NEJMoa2206038.
Frías JP, Davies MJ, Rosenstock J, et al. Tirzepatide versus semaglutide once weekly in patients with type 2 diabetes. N Engl J Med. 2021;385(6):503–15. https://doi.org/10.1056/NEJMoa2107519.
Langer J, Hunt B, Valentine WJ. Evaluating the short-term cost-effectiveness of liraglutide versus sitagliptin in patients with type 2 diabetes failing metformin monotherapy in the United States. J Manag Care Pharm. 2013;19(3):237–46. https://doi.org/10.18553/jmcp.2013.19.3.237.
Hunt B, McConnachie CC, Gamble C, Dang-Tan T. Evaluating the short-term cost-effectiveness of liraglutide versus lixisenatide in patients with type 2 diabetes in the United States. J Med Econ. 2017;20(11):1117–20. https://doi.org/10.1080/13696998.2017.1347793.
Wilkinson L, Hunt B, Johansen P, Iyer NN, Dang-Tan T, Pollock RF. Cost of achieving HbA1c treatment targets and weight loss responses with once-weekly semaglutide versus dulaglutide in the United States. Diabetes Ther. 2018;9(3):951–61. https://doi.org/10.1007/s13300-018-0402-8.
Hunt B, Hansen BB, Ericsson Å, et al. Evaluation of the cost per patient achieving treatment targets with oral semaglutide: a short-term cost-effectiveness analysis in the United States. Adv Ther. 2019;36(12):3483–93. https://doi.org/10.1007/s12325-019-01125-y.
Hansen BB, Nuhoho S, Ali SN, et al. Oral semaglutide versus injectable glucagon-like peptide-1 receptor agonists: a cost of control analysis. J Med Econ. 2020;23(6):650–8. https://doi.org/10.1080/13696998.2020.1722678.
Zhang X, McAdam MC. Short-term cost-effectiveness analysis of tirzepatide for the treatment of type 2 diabetes in the United States. J Manag Care Spec Pharm. 2023;29(3):276–84. https://doi.org/10.18553/jmcp.2023.29.3.276.
Lingvay I, Cheng AY, Levine JA, et al. Achievement of glycaemic targets with weight loss and without hypoglycaemia in type 2 diabetes with the once-weekly glucose-dependent insulinotropic polypeptide and glucagon-like peptide-1 receptor agonist tirzepatide: a post hoc analysis of the SURPASS-1 to -5 studies. Diabetes Obes Metab. 2023;25(4):965–74. https://doi.org/10.1111/dom.14943.
Novo Nordisk. Ozempic (semaglutide): prescribing information. Plainsboro, NJ: Novo Nordisk Inc.; 2022.
IBM Micromedex. RED BOOK online. https://www.ibm.com/products/micromedex-red-book. Accessed October 2022.
Ludvik B, Giorgino F, Jódar E, et al. Once-weekly tirzepatide versus once-daily insulin degludec as add-on to metformin with or without SGLT2 inhibitors in patients with type 2 diabetes (SURPASS-3): a randomised, open-label, parallel-group, phase 3 trial. Lancet. 2021;398(10300):583–98. https://doi.org/10.1016/S0140-6736(21)01443-4.
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86. https://doi.org/10.1056/NEJM199309303291401.
Adler AI, Stratton IM, Neil HA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000;321(7258):412–9. https://doi.org/10.1136/bmj.321.7258.412.
Medical Writing and Editorial Assistance
The authors would like to acknowledge Lori Justice, an employee of AmerisourceBergen, for medical writing support, which was funded by Eli Lilly and Company.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Funding
Eli Lilly and Company provided AmerisourceBergen with financial support to conduct the modeling study upon which this manuscript is based. Eli Lilly and Company provided funding for the journal’s Rapid Service Fee.
Author information
Authors and Affiliations
Contributions
All authors were responsible for the conception and design of the study. KBO was responsible for the acquisition and analysis of data. All authors were responsible for data interpretation and contributed substantially to drafting and revising the manuscript. All authors have reviewed and approved the final version of the manuscript for submission to Diabetes Therapy and agree to be accountable for its contents.
Corresponding author
Ethics declarations
Conflict of Interest
Reema Mody and Jennifer Ward are employees and shareholders of Eli Lilly and Company. Kellie Meyer and Ken O’Day are employees of AmerisourceBergen.
Ethical Approval
This study uses published data from a previously conducted clinical trial and does not contain any studies with human participants or animals performed by any of the authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mody, R.R., Meyer, K.L., Ward, J.M. et al. Cost per Patient Achieving Treatment Targets and Number Needed to Treat with Tirzepatide Versus Semaglutide 1 mg in Patients with Type 2 Diabetes in the United States. Diabetes Ther 14, 2045–2055 (2023). https://doi.org/10.1007/s13300-023-01470-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01470-w