Abstract
The effectiveness of therapy in patients with diabetes depends on the correct use of the insulin injection technique. However, despite many established recommendations and evidence that an effective insulin injection technique is essential to improve glycaemic control and minimise the risk associated with diabetes, there is still a need to identify impediments to the insulin injection technique among patients and create awareness among patients and healthcare professionals about the importance of the optimisation of insulin injection techniques. This review focuses on the recent advancements in delivery devices, insulin injection technique teaching methods, monitoring, and complication management and highlights regional best practices and recommendations for optimising injection techniques to improve diabetes outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite well-established guidelines being in place and evidence that a proper insulin injection technique is crucial for better glucose control and reducing diabetes risks, there is still a need to recognise barriers to a proper technique among patients and to raise awareness among both patients and healthcare providers about the importance of optimizing insulin injection techniques. |
The use of short and thin needles in insulin injections has been demonstrated to improve the insulin injection technique by decreasing the amount of pain experienced during the injection process, reducing the likelihood of intramuscular injection, and improving the rate and completeness of insulin absorption. |
Re-education and training of patients has been shown to be an effective method to improve the insulin injection technique, resulting in better glycaemic control, increased adherence, a reduced risk of lipohypertrophy, and improved patient outcomes. |
Stakeholders in insulin therapy, including diabetes educators and healthcare providers, play a crucial role in patient education. A physician's goal should be to educate patients with diabetes and their caregivers on the safe handling and use of injectables, proper injection techniques, and cost-effectiveness to ensure they have the necessary knowledge and skills. |
The implementation of comprehensive insulin stewardship programs in healthcare facilities such as hospitals, wards, and intensive care units is crucial in ensuring safe and effective insulin usage by establishing standard procedures and reducing the risk of improper insulin prescription and administration. |
Awareness and the Need to Improve Injection Techniques in Diabetes Management
Diabetes is a major health issue with high prevalence worldwide. Around 537 million adults between the ages of 20 years and 79 years are estimated to have diabetes [1]. Patients with diabetes account for 10.5% of the world's population [1]. Insulin therapy is an important aspect of type 1 and type 2 diabetes management [2]. As insulin injection procedures are operator dependent, a thorough understanding of injection techniques is critical for healthcare professionals (HCPs) and patients to achieve a desirable outcome in patients with diabetes [3].
The use of pen injection devices for daily self-administered insulin injections is well established and commonly used in the treatment of diabetes. Patients consider pen injection devices to be more convenient compared to using a syringe to dispense insulin from a vial [4]. Physicians must be informed that proper injection practice is an aspect of improving glycaemic control in patients. In addition to managing uncontrolled diabetes and its repercussions, nursing staff and physicians also deal with a lack of knowledge and time spent on improving the insulin injection technique [5].
Insulin injection technique recommendations include findings from the Forum For Injection Technique (FITTER) Injection Technique Questionnaire (ITQ), one of the biggest worldwide surveys of its kind [6]. Results from this survey indicated suboptimal knowledge and poor insulin injection skills among patients with diabetes [6]. The lack of knowledge, expertise, and practice associated with insulin administration strategies among patients with diabetes may contribute to erratic insulin absorption and increased therapy costs [6, 7]. This survey served as the basis for numerous recommendations made by various diabetes groups.
Despite many established recommendations and evidence that an effective insulin injection technique is essential to improve glycaemic control and minimise the risk associated with diabetes, there is still a need to identify impediments in the insulin injection technique among patients and create awareness among patients and HCPs about the importance of the optimisation of insulin injection techniques.
This review focuses on the recent advancements in delivery devices, insulin injection technique teaching methods, monitoring, and complication management and highlights regional best practices and recommendations for optimising injection techniques to improve diabetes outcomes. This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Improvement in Delivery Devices and Ancillary Devices
There have been rapid advances in insulin delivery devices in the past decade. The emergence of hybrid closed-loop systems, the incorporation of consumer electronics, and the use of cloud-based data platforms have accelerated diabetes technology advancement, which began with the insulin syringe and evolved to insulin pens, insulin pumps, and sensor-augmented pumps [8].
Vials and Syringes
Insulin was initially delivered using heavy reusable syringes with long, large-bore needles that needed to be disinfected by boiling to enable efficient reuse [8]. In 1924, Becton Dickinson (BD) manufactured the first specialised syringe for insulin injection, which was followed by the launch of the “Novo Syringe” by Novo Nordisk in 1925. The patented innovation of the Luer lock fit for hypodermic needles significantly decreased syringe disengagement during injection, leading to the development of disposable Luer lock syringes [9, 10].
One-millilitre Luer lock syringes with detachable or permanently attached needles were introduced by BD in the 1960s, and were associated with less pain and a reduced risk of needle-related infections [8]. In 2012, a less painful BD Veo insulin syringe with an ultra-fine 6-mm needle was introduced, which presented a lower risk of intramuscular injections and a decreased plunger force to improve the flow of high insulin doses [8]. Even though the demand for the “conventional” syringe technology has decreased in recent times, vials and syringes were the only choices for insulin delivery for more than five decades [8].
Pens and Needles
Insulin pens provide several advantages over conventional vial and syringe injections, including ease of use, particularly for individuals with eyesight or motor dexterity issues, and discretion of use (Table 1) [11,12,13,14]. Attachment of pen needles is required for injecting insulin with pen devices, and this provides a more convenient injection experience [15].
Pen needles have become shorter and thinner over the years [4]. Needles of a smaller bore size and shorter lengths (3.5–4.0 mm) are currently used instead of long, large-bore-sized, reusable needles for insulin injection [8, 16, 17]. The advantages of short, fine-gauge needles over longer needles have been reported in a series of clinical trials, specifically for quality-of-life metrics, such as decreased pain and increased patient preference [17, 18]. In a clinical study on injection experience conducted among patients with type 1 or type 2 diabetes mellitus, pen needles with extra-thin walls were most favoured as they require less time and thumb force to inject and offer higher confidence that a full dosage has been administered compared to traditional pen needles [15].
The safety and efficacy of the 4-mm pen needle have been assessed and proven in several clinical trials in adults and children, as well as in obese and nonobese adults with diabetes [5, 19]. Furthermore, the 4-mm pen needle has been recommended for use in most adult patients of all sizes where the lifting of a skin fold is not required (Fig. 1) [20]. The scientific literature on pen needle length for enhancing insulin delivery from the perspective of the skin thickness and subcutaneous tissue layers has been reviewed and acknowledged by current medical association guidelines, which noted that current evidence supports the effectiveness and acceptability of short needles for subcutaneous tissue insulin [17, 21].
Initially, needle length was determined by local practices or economic considerations, or, at best, based on the patient’s physical assessment [5]. However, studies employing ultrasonography to examine the skin and subcutaneous tissue anatomy have offered accurate data on patients with diabetes, making needle length selection more evidence based [22].
A more recent innovation is the redesign of the needle hub, which is located at the needle shaft (cannula) base and connects the needle to an insulin pen [17]. This redesign was prompted by studies on people and animal models which revealed that the differences in injection depth correlated to the variations in the force applied to the skin during injections [17]. To reduce the effects of varying the injection force, the redesigned hub design distributes insertion forces over a contoured and bigger surface area [17].
The re-engineered hub design of the BD Nano PRO needle was found to precisely accomplish the 4-mm target needle penetration depth with noticeably less variability than commercial posted-hub pen needle devices over the varied range of applied injection forces [23]. The BD Nano PRO needle was rated less painful and more comfortable, associated with better ease of administration, and overall preferred by patients compared to other pen needles of a similar gauge and length [16].
Improvement in Teaching Methods
Despite significant advancements in technology and therapy over the last decade, insulin injection techniques among patients have not improved [24]. Standardised and proper injection techniques should be adhered to, as they have been associated with improved outcomes in patients with diabetes [25, 26]. A proper injection technique is defined as the technique that successfully delivers the drug into the subcutaneous area with minimal pain and no leakage [24, 27]. A good technique includes proper injection site rotation and not injecting into lipohypertrophic areas [18]. However, according to an ITQ survey, nearly 50% of patients have or have had symptoms that suggest lipohypertrophy (LH), and 21% of patients reported repeating a whole day or even a few days of daily injections at the same spot [28]. Furthermore, 26% of respondents reported that they have occasionally injected insulin into lipohypertrophic sites [28].
In response to the lack of proper knowledge and clear recommendations on insulin injection techniques, an international group of 183 nurses, diabetes educators, and HCPs from 54 countries gathered in 2015 to present practical and thorough recommendations for diabetes injections and infusions [21]. Regional, evidence-based recommendations for diabetes injections have been developed in many countries [12, 29].
Individualised injection technique training has been associated with better glycaemic control, increased therapeutic satisfaction, adherence, improved injection techniques, and possibly a lower consumption of insulin [24, 26]. In a study evaluating the effectiveness of the re-education of 87 insulin-treated patients with diabetes on the insulin injection technique, re-education was performed once a month for approximately 4 months. This led to a significant improvement in glycaemic control and a reduction in HbA1c levels (p < 0.01), particularly in those who had poor knowledge of the procedure before re-education [30]. This observation was further supported by a recent survey conducted among 158 patients with type 2 diabetes mellitus, which reported that insulin-treated patients with diabetes require intensive educational refresher courses at 3-month intervals at least. Compared to patients who were left unsupported, patients who received a second follow-up of comprehensive injection-technique-specific education maintained the good results achieved after the initial 6 months of educational intervention [31].
According to the most recent ITQ study, patients who received injection technique guidance from their HCP within the last 6 months were more likely to successfully conduct site rotation [21]. Despite injecting for an average of 9 years, less than 40% of patients surveyed reported receiving injection instructions in the past 6 months, and 10% had never received training on correct injection techniques [21]. Studies have indicated that the use of proper injection techniques by patients, such as the proper rotation of injection sites, using a new needle with each injection, and switching to shorter needles, facilitates good glycaemic control and decreased rates of LH [5, 12, 20, 22, 32]. Liang et al. recently developed a series of training methods that employ simulation tools to provide patients with an opportunity to practise injecting techniques. The use of these simulation tools, coupled with administration videos and manuals (which form the standard procedure used to train patients with diabetes on insulin injection), significantly improved the insulin injection skills of patients and eased patients’ fear of injection [25]. As this educational method is both economical and easily adaptable, it may be utilised outside of hospitals in developing nations to help patients learn more about proper insulin injection techniques.
Figure 2 illustrates an optimal sequence for the insulin injection technique, which can be easily adopted by both patients and HCPs to minimise the associated risks [12].
Optimal injection technique sequence. IM intramuscular. Adapted with permission from [12] (released under Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License (CC BY-NC-SA 4.0))
Improvement in Injection Technique Complication Management
Implementing correct injection techniques and providing structured education on the technique play an important role in decreasing skin complications, including LH, insulin-derived amyloidosis (IDA), local inflammation, bruising, and subsequent hypoglycaemia [31]. LH manifests as an abnormal build-up of fat under the skin surface and is associated with recurrent trauma related to performing frequent or daily insulin injections at the same site [33]. The prevalence of LH has been reported to be 38% in insulin-treated patients according to a recent meta-analysis [34].
Risk factors associated with the development of LH include the reuse of needles, site rotation frequency, duration of insulin treatment, high doses of insulin, glycaemic control issues, and a lack of patient education [24, 33]. Insulin injections into LH lesions can result in an erratic increase in insulin dose and, as a result, the patient may incur greater costs [35]. When insulin analogues were used instead of human insulin, the risk of LH in patients receiving numerous daily insulin injections was lower [36]. LH prevention should be a priority for physicians. Visual and physical examinations are crucial to detect abnormalities at the injection site. Patients should also be educated on how to inspect and recognise LH at injection sites [24].
A complication of insulin treatment that affects the skin is called IDA, a nodular form of the disease [37, 38]. The insulin-derived amyloid fibril protein creates deposits of amyloid at the sites of insulin injection [39]. Despite the lack of actual prevalence data, IDA may be mistaken for LH in insulin-treated patients [38]. As the insulin absorption at the IDA site is remarkably reduced compared to that at the normal site [39], IDA causes poor glycaemic control and increased insulin dose requirements [37, 39]. Additionally, IDA results in hypoglycaemia due to the delivery of an increased dose of insulin into normal sites [39]. Therefore, it is necessary to reduce the dose of insulin when alternating the insulin injection site from the IDA site to the normal site [3, 39]. Recently, cases of IDA without a palpable mass have been reported [40]. In these cases, differentiating between IDA and LH by physical examination is difficult, and imaging studies, such as magnetic resonance imaging (MRI) and ultrasound, are necessary. Long-term, recurrent, same-site insulin injection is regarded as the most significant risk factor for developing IDA [38, 39]. To prevent IDA, it is important to educate patients about proper injection site rotation as well as ways to prevent LH [3].
The patient’s injection site rotation scheme should be reviewed by HCPs at least once annually [12]. An effective and widely used rotation scheme involves dividing the injection site into quadrants for the abdomen or halves for the thighs, buttocks, and arms. The patient should use one quadrant or half per week and then switch to another quadrant or half, either clockwise or anticlockwise, the following week [12]. It is recommended that the new insulin injection site be at least 1–2 cm away from the previous injection site [12].
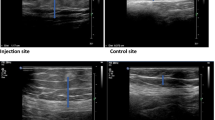
Gentile et al. defined a structured palpation technique that allows HCPs to detect skin LH lesions in insulin-treated patients with diabetes [41]. After undergoing specialised training involving repeated and well-codified palpitation manoeuvres, inexperienced HCPs were able to quickly procure diagnostic accuracy in identifying LH lesions regardless of the site, size, and BMI [41]. However, the palpitation method is not always feasible and is likely insufficient to detect LH, particularly in individuals who need high-dose insulin to manage hyperglycaemia [42]. Superficial subcutaneous ultrasonography would be a suitable method to assess the existence of LH [42].
In a study, Wang et al. reported how the management of LH was affected by ultrasound evaluation and intense injection technique training [43]. The results of the study revealed that a combination of ultrasound examination and intensive injection technique education considerably lowered seven-point glucose control and the occurrence of adverse blood glucose events without increasing the insulin dosage [43]. Ultrasound examination offers higher sensitivity and specificity compared to physical evaluation, particularly in the case of LH lesions without visible or palpable changes [43]. Furthermore, ultrasound examination provides a precise way to measure the subcutaneous fat thickness to select optimal injection sites for patients with diabetes who have concerns related to LH [43].
Improvement in Injection Technique Monitoring
Through connected devices, software, and applications, recent advancements in digital health technologies can address the fundamental challenges associated with blood glucose control in diabetes care [44]. Smart pens have progressed over the last decade from traditional insulin pens in terms of functionality, and they have the potential to facilitate the use of optimal doses of insulin and improve diabetes management by offering automated storing and transmission of insulin dosing data, which can assist physicians in promoting patient-administered self-care [44, 45].
The data recorded and stored by smart pens on the amount and timing of insulin injections allow patients to obtain an accurate overview of their insulin-related data and provide downloadable reports to their HCP [44, 45]. Furthermore, the insulin dosing data from smart pens may be combined with glucose data from continuous glucose monitoring to provide patients with a better understanding of how insulin doses affect glucose levels and thereby allow better dosing decisions [45]. To encourage the usage of smart pens, patients and HCPs must be educated on the benefits of smart pens and provided with recommendations on how to use the technology, evaluate data, and execute suitable treatment strategies [45].
Additionally, the increasing prevalence of insulin regimens, preparations, and delivery methods raises the possibility of injection technique errors. This may jeopardise patient safety and well-being. Self-examination of the insulin injection site (SelfIE) is an important aspect of injection technique monitoring, as it may aid in the early detection of skin complications (such as LH) and unfavourable variability in glucose levels and may help to avoid excessive insulin use [46]. The development of an insulin strategy tailored to each intensive care unit or ward can enhance indoor glycaemic control and lower professional hazards associated with insulin injection. Kalra et al. suggested that the initiation of complete insulin stewardship programmes in hospitals, wards, and intensive care units to address all elements of safe and rational insulin usage. Insulin stewardship programmes will establish standard operating procedures for choosing insulin regimens, preparations, and delivery devices, and will reduce the possibility of inappropriate insulin prescription and administration (Table 2) [47, 48]. Table 3 provides a summary of the key improvements and recommendations for the insulin injection technique discussed here.
Call for Action
Consistent implementation of programmes involving patient education and re-education is needed to resolve issues associated with suboptimal insulin injection techniques. All stakeholders in insulin therapy should be included, particularly diabetes educators and HCPs, as they are at the forefront of patient education [49]. One of the physician’s goals should be to ensure that patients with diabetes and their caregivers have the necessary knowledge and skills for the safe handling and use of injectables and the proper application of injection techniques and are fully informed on the anticipated cost savings. This will ensure that the complete therapeutic potential of insulin therapy can be achieved in patients with diabetes [21, 49, 50]. Figure 3 illustrates the key elements involved in implementing a safe technique for administering insulin injections.
Best Practices
Table 4 highlights regional best practices and suggestions by authors for enhancing injection methods.
Conclusion
An optimal insulin injection technique helps to avoid intradermal or intramuscular injections and ensures efficient insulin delivery to the subcutaneous tissue. Improving the insulin injection technique necessitates the involvement of all key stakeholders in insulin therapy, including diabetes educators and/or nurses, doctors, patients, and manufacturers of needles and devices. However, clear local recommendations for diabetes educators and HCPs are needed so that they may educate patients on how to self-manage their insulin administration. Adherence to recommendations regarding insulin injection techniques may allow patients with diabetes to optimise insulin therapy, experience better outcomes, and incur lower costs.
References
International Diabetes Federation (IDF). IDF diabetes atlas 2021. Brussels: International Diabetes Federation; 2021.
Lepeska M. Insulin users’ perspective profile 2017. Amsterdam: Health Action International; 2017.
Bajwa SS, Bajwa S, Baruah M, Kalra S. An acute need for awareness of insulin injection guidelines in operative and intensive care units. Anesth Essays Res. 2013;7:1. https://doi.org/10.4103/0259-1162.113976.
Gibney MA, Fitz-Patrick D, Klonoff DC, Whooley S, Lu B, Yue W, et al. User experiences with second-generation 32-gauge × 4 mm vs thinner comparator pen needles: prospective randomized trial. Curr Med Res Opin. 2020;36:1591–600. https://doi.org/10.1080/03007995.2020.1803248.
Grassi G, Scuntero P, Trepiccioni R, Marubbi F, Strauss K. Optimizing insulin injection technique and its effect on blood glucose control. J Clin Transl Endocrinol. 2014;1:145–50. https://doi.org/10.1016/j.jcte.2014.07.006.
Frid AH, Hirsch LJ, Menchior AR, Morel DR, Strauss KW. Worldwide injection technique questionnaire study: population parameters and injection practices. Mayo Clin Proc. 2016;91:1212–23. https://doi.org/10.1016/j.mayocp.2016.06.011.
Netere AK, Ashete E, Gebreyohannes EA, Belachew SA. Evaluations of knowledge, skills and practices of insulin storage and injection handling techniques of diabetic patients in Ethiopian primary hospitals. BMC Public Health. 2020;20:1537. https://doi.org/10.1186/s12889-020-09622-4.
Kesavadev J, Saboo B, Krishna MB, Krishnan G. Evolution of insulin delivery devices: from syringes, pens, and pumps to DIY artificial pancreas. Diabetes Ther. 2020;11:1251–69. https://doi.org/10.1007/s13300-020-00831-z.
Dickinson FS. Hypodermic syringe. US Patent US1742497, 1930.
Whitney EH. Disposable Luer lock syringe. US Patent 4220151, 1980.
Masierek M, Nabrdalik K, Janota O, Kwiendacz H, Macherski M, Gumprecht J. The review of insulin pens—past, present, and look to the future. Front Endocrinol. 2022;13:827484. https://doi.org/10.3389/fendo.2022.827484.
Tandon N, Kalra S, Balhara YS, Baruah M, Chadha M, Chandalia H, et al. Forum for injection technique and therapy expert recommendations, India: The Indian recommendations for best practice in insulin injection technique, 2017. Indian J Endocr Metab. 2017;21:600. https://doi.org/10.4103/ijem.IJEM_97_17.
Singh R, Samuel C, Jacob JJ. A comparison of insulin pen devices and disposable plastic syringes—simplicity, safety, convenience and cost differences. Eur Endocrinol. 2018;14:47. https://doi.org/10.17925/EE.2018.14.1.47.
Kesavadev J, Saboo B, Benny N, Basanth A, Krishnan G, Shankar A, et al. One hundred and one years of insulin delivery with transition from syringes to user-friendly technologies. Int J Diabetes Technol 2022;1:25–31.
Aronson R, Gibney MA, Oza K, Bérubé J, Kassler-Taub K, Hirsch L. Insulin pen needles: effects of extra-thin wall needle technology on preference, confidence, and other patient ratings. Clin Ther. 2013;35:923-933.e4. https://doi.org/10.1016/j.clinthera.2013.05.020.
Whooley S, Briskin T, Gibney MA, Blank LR, Berube J, Pflug BK. Evaluating the user performance and experience with a re-engineered 4 mm × 32g pen needle: a randomized trial with similar length/gauge needles. Diabetes Ther. 2019;10:697–712. https://doi.org/10.1007/s13300-019-0585-7.
Heinemann L, Nguyen T, Bailey TS, Hassoun A, Kulzer B, Oliveria T, et al. Needle technology for insulin administration: a century of innovation. J Diabetes Sci Technol. 2021. https://doi.org/10.1177/19322968211059564.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment. Diabetes Care 2021;40:S64–74. https://doi.org/10.2337/dc17-S011.
Hirsch LJ, Gibney MA, Li L, Bérubé J. Glycemic control, reported pain and leakage with a 4 mm × 32 G pen needle in obese and non-obese adults with diabetes: a post hoc analysis. Curr Med Res Opin. 2012;28:1305–11. https://doi.org/10.1185/03007995.2012.709181.
Frid A, Hirsch L, Gaspar R, Hicks D, Kreugel G, Liersch J, et al. New injection recommendations for patients with diabetes. Diabetes Metab. 2010. https://doi.org/10.1016/S1262-3636(10)70002-1.
Frid AH, Kreugel G, Grassi G, Halimi S, Hicks D, Hirsch LJ, et al. New insulin delivery recommendations. Mayo Clin Proc. 2016;91:1231–55. https://doi.org/10.1016/j.mayocp.2016.06.010.
Gibney MA, Arce CH, Byron KJ, Hirsch LJ. Skin and subcutaneous adipose layer thickness in adults with diabetes at sites used for insulin injections: implications for needle length recommendations. Curr Med Res Opin. 2010;26:1519–30. https://doi.org/10.1185/03007995.2010.481203.
Rini C, Roberts BC, Morel D, Klug R, Selvage B, Pettis RJ. Evaluating the impact of human factors and pen needle design on insulin pen injection. J Diabetes Sci Technol. 2019;13:533–45. https://doi.org/10.1177/1932296819836987.
Selvadurai S, Cheah KY, Ching MW, Kamaruddin H, Lee XY, Ngajidin RM, et al. Impact of pharmacist insulin injection re-education on glycemic control among type II diabetic patients in primary health clinics. Saudi Pharm J. 2021;29:670–6. https://doi.org/10.1016/j.jsps.2021.04.028.
Liang K, Xie Q, Nie J, Deng J. Study on the effect of education for insulin injection in diabetic patients with new simulation tools. Medicine. 2021;100: e25424. https://doi.org/10.1097/MD.0000000000025424.
Misnikova IV, Gubkina VA, Lakeeva TS, Dreval AV. A randomized controlled trial to assess the impact of proper insulin injection technique training on glycemic control. Diabetes Ther. 2017;8:1309–18. https://doi.org/10.1007/s13300-017-0315-y.
Pledger J, Hicks D, Kirkland F, Down S. Importance of injection technique in diabetes. Diabetes Prim Care. 2012;14:6.
De Coninck C, Frid A, Gaspar R, Hicks D, Hirsch L, Kreugel G, et al. Results and analysis of the 2008–2009 insulin injection technique questionnaire survey: insulin injection technique survey. J Diabetes. 2010;2:168–79. https://doi.org/10.1111/j.1753-0407.2010.00077.x.
FIT. Forum for Injection Technique. 2022. http://www.fit4diabetes.com/. Accessed 7 June 2022.
Nakatani Y, Matsumura M, Monden T, Aso Y, Nakamoto T. Improvement of glycemic control by re-education in insulin injection technique in patients with diabetes mellitus. Adv Ther. 2013;30:897–906. https://doi.org/10.1007/s12325-013-0066-8.
Gentile S, Guarino G, Della Corte T, Marino G, Satta E, Pasquarella M, et al. The durability of an intensive, structured education-based rehabilitation protocol for best insulin injection practice: the ISTERP-2 study. Diabetes Ther. 2021;12:2557–69. https://doi.org/10.1007/s13300-021-01108-9.
Chen L, Xing Q, Li J, Zhou J, Yuan Y, Wan Y, et al. Injection technique education in patients with diabetes injecting insulin into areas of lipohypertrophy: a randomized controlled trial. Diabetes Ther. 2021;12:813–26. https://doi.org/10.1007/s13300-021-01013-1.
Ucieklak D, Mrozinska S, Wojnarska A, Malecki MT, Klupa T, Matejko B. Insulin-induced lipohypertrophy in patients with type 1 diabetes mellitus treated with an insulin pump. Int J Endocrinol. 2022;2022:1–7. https://doi.org/10.1155/2022/9169296.
Deng N, Zhang X, Zhao F, Wang Y, He H. Prevalence of lipohypertrophy in insulin-treated diabetes patients: a systematic review and meta-analysis. J Diabetes Investig. 2018;9:536–43. https://doi.org/10.1111/jdi.12742.
Gentile S, Strollo F, Guarino G, Brancario C, Corigliano M, Cozzolino G, et al. Why are so huge differences reported in the occurrence rate of skin lipohypertrophy? Does it depend on method defects or on lack of interest? Diabetes Metab Syndr. 2019;13:682–6. https://doi.org/10.1016/j.dsx.2018.11.042.
Barola A, Tiwari P, Bhansali A, Grover S, Dayal D. Insulin-related lipohypertrophy: lipogenic action or tissue trauma? Front Endocrinol. 2018;9:638. https://doi.org/10.3389/fendo.2018.00638.
Nilsson MR. Insulin amyloid at injection sites of patients with diabetes. Amyloid. 2016;23:139–47. https://doi.org/10.1080/13506129.2016.1179183.
Ansari AM, Osmani L, Matsangos AE, Li QK. Current insight in the localized insulin-derived amyloidosis (LIDA): clinico-pathological characteristics and differential diagnosis. Pathol Res Practice. 2017;213:1237–41. https://doi.org/10.1016/j.prp.2017.08.013.
Nagase T, Iwaya K, Iwaki Y, Kotake F, Uchida R, Oh-i T, et al. Insulin-derived amyloidosis and poor glycemic control: a case series. Am J Med. 2014;127:450–4. https://doi.org/10.1016/j.amjmed.2013.10.029.
Nagase T, Iwaya K, Kogure K, Zako T, Misumi Y, Kikuchi M, et al. Insulin-derived amyloidosis without a palpable mass at the insulin injection site: a report of two cases. J Diabetes Investig. 2020;11:1002–5. https://doi.org/10.1111/jdi.13199.
Gentile S, Guarino G, Giancaterini A, Guida P, Strollo F, AMD-OSDI Italian Injection Technique Study Group. A suitable palpation technique allows to identify skin lipohypertrophic lesions in insulin-treated people with diabetes. SpringerPlus. 2016;5:563. https://doi.org/10.1186/s40064-016-1978-y.
Korkmaz FN, Gökçay Canpolat A, Güllü S. Determination of insulin-related lipohypertrophy frequency and risk factors in patients with diabetes. Endocrinol Diabetes Nutr (English Ed). 2022;69:354–61. https://doi.org/10.1016/j.endien.2022.05.006.
Wang W, Tong Y, Chen Y, Tu M, Chen H. Evaluation of ultrasound examination combined with intensive injection technique education on insulin-induced lipohypertrophy (LH) management: a prospective cohort study in China. Int J Diabetes Dev Ctries. 2021;41:669–75. https://doi.org/10.1007/s13410-021-00935-7.
IQVIA. Optimizing insulin use through smart pens: challenges and opportunities in Europe. Durham, NC: IQVIA; 2021.
Sy SL, Munshi MM, Toschi E. Can smart pens help improve diabetes management? J Diabetes Sci Technol. 2020. https://doi.org/10.1177/1932296820965600.
Kalra S, Kumar A, Gupta Y. Prevention of lipohypertrophy. J Pak Med Assoc. 2016;66(7):910–1.
Kalra S, Sahay R, Tiwaskar M. Need for insulin stewardship programmes. J Assoc Physicians India. 2018;66:83–4.
Kalra S, Unnikrishnan AG, Prasanna Kumar KM, Sahay R, Chandalia HB, Saboo B, et al. Addendum 1: forum for injection technique and therapy expert recommendations, India. Diabetes Ther. 2022. https://doi.org/10.1007/s13300-022-01332-x.
Spollett G, Edelman SV, Mehner P, Walter C, Penfornis A. Improvement of insulin injection technique: examination of current issues and recommendations. Diabetes Educ. 2016;42:379–94. https://doi.org/10.1177/0145721716648017.
Strauss K. Best practice diabetes injection technique is key to improved glycaemic variability and avoiding injection site issues. General Med. 2014. https://doi.org/10.4172/2327-5146.1000168.
Kalra S, Mithal A, Sahay R, John M, Unnikrishnan AG, Saboo B, et al. Indian injection technique study: injecting complications, education, and the health care professional. Diabetes Ther. 2017;8:659–72. https://doi.org/10.1007/s13300-017-0244-9.
Kalra S, Mithal A, Sahay R, John M, Unnikrishnan AG, Saboo B, et al. Indian injection technique study: population characteristics and injection practices. Diabetes Ther. 2017;8:637–57. https://doi.org/10.1007/s13300-017-0243-x.
Medical Writing and Editorial Assistance
Excellent medical writing and editorial assistance was provided by Yuvenya Kaeswaren of BioQuest Solutions Pte. Ltd, funded by Becton Dickinson/Embecta (formerly BD Diabetes Care), in accordance with GPP 2022 guidelines (https://www.ismpp.org/gpp-2022).
Funding
The journal’s Rapid Service Fee was funded by Becton Dickinson/Embecta (formerly BD Diabetes Care), in accordance with GPP 2022 guidelines (https://www.ismpp.org/gpp-2022).
Author information
Authors and Affiliations
Contributions
Sanjay Kalra, Faruque Pathan, Ida Ayu Made Kshanti, Nguyen Quang Bay, Terumasa Negase, Teresa OIiveria and Shailendra Bajpai provided critical feedback, contributed to data acquisition and interpretation, and approved the final version for submission.
Corresponding author
Ethics declarations
Conflict of Interest
Sanjay Kalra received speaker fees from Boehringer Ingelheim, Novo Nordisk and Sanofi. Shailendra Bajpai and Teresa Oliveria are employees and stockholders of BD/Embecta (formerly BD Diabetes Care), manufacturer of a range of insulin delivery devices. Faruque Pathan, Ida Ayu Made Kshanti, Nguyen Quang Bay, and Terumasa Nagase have nothing to disclose.
Ethical Approval
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kalra, S., Pathan, F., Kshanti, I.A.M. et al. Optimising Insulin Injection Techniques to Improve Diabetes Outcomes. Diabetes Ther 14, 1785–1799 (2023). https://doi.org/10.1007/s13300-023-01460-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01460-y