Abstract
Introduction
Reducing postprandial (PP) hyperglycemia and PP glucose excursions is important for overall glycemic management. Although most therapeutic lifestyle interventions that reduce caloric intake would affect this, there is no particular nutritional intervention favored.
Methods
We evaluated the effects of a novel natural food adjuvant combining mulberry leaf extract (MLE) with other bioactive ingredients, in people with type 2 diabetes (T2D) originating from Asia, on improving PP glucometabolic response in a randomized controlled exploratory crossover, two-center study (USA, Singapore). A 2-g blend of 250 mg MLE [containing 12.5 mg of 1-deoxynojirimycin (DNJ)], fiber (1.75 g), vitamin D3 (0.75 μg), and chromium (75 μg), compared with a similar blend without the MLE, was sprinkled over a 350-kcal breakfast meal (55.4 g carbs) and PP blood glucose (primary exploratory endpoint), insulin, and incretin hormones (GLP-1, GIP) were evaluated in blood samples over 3 h. Changes in incremental areas under the concentration curve (iAUC) and maximum concentrations (Cmax) were compared.
Results
Thirty individuals (12 women, mean age 59 years, HbA1c 7.1%, BMI 26.5 kg/m2) were enrolled and the MLE-based blend relative to the blend without MLE significantly reduced glucose iAUC at 1 h (− 20%, p < 0.0001), 2 h (− 17%, p = 0.0001), and 3 h (− 15%, p = 0.0032) and Cmax [mean (95% CI) difference − 0.8 (− 1.2, − 0.3) mmol/L, p = 0.0006]. A statistically significant reduction in 1 h insulin iAUC (− 24%, p = 0.0236) was observed, but this reduction was no longer present at either 2 h or 3 h. No difference in GLP-1 was seen, but GIP response (iAUC and Cmax) was less with the MLE-based blend.
Conclusions
The observation of a significant glucose reduction paralleled with a significant lower insulin response supports a reduced gastrointestinal glucose absorption. These results support the use of a 2-g natural blend of MLE, fiber, vitamin D, and chromium in T2D as a convenient dietary adjuvant to improve PP glucometabolic response.
ClinicalTrials.gov identifier NCT04877366.
Plain Language Summary
It is generally accepted that addressing lifestyle factors represents the initial step for treatment of type 2 diabetes. This includes an evaluation of how to optimize physical exercise and diet. However, although most diets that reduce caloric intake would affect sugar levels, there is no particular nutritional intervention favored, and choices depend on factors such as cost, preference, availabilities, and scientific evidence. A multiingredient food adjuvant blend for support of blood sugar levels combined mulberry leaf extract with fiber, vitamin D, and chromium, and was developed with the intended use to be sprinkled on and consumed with a meal. In this study involving 30 people with type 2 diabetes (mean age 59 years, glycated hemoglobin 7.1%, body mass index 26.5 kg/m2) originating from Asia, a 2-g blend of these ingredients was sprinkled over a 350-kcal breakfast meal rich in carbohydrates (55.4 g) and compared to a similar blend without the MLE. Blood sugar spikes following the meal were reduced by 15–20% over an observation period of 3 h. Thus, such a mulberry leaf extract-based blend, which also is a source of fiber, vitamin D, and chromium, may represent a convenient dietary support to improve sugar levels after a meal.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study |
Several nutritional principles can reduce the glycemic impact of dietary carbohydrates, including reducing the rate of gastrointestinal glucose absorption. |
A natural adjuvant that follows this principle is mulberry leaf extract (MLE) that contains iminosugar alkaloids (i.e., analogues of sugars), of which 1-deoxynojirimycin (DNJ) is the most abundant and competitively blocks the active site of polysaccharide-degrading enzymes in the digestive tract, thus reducing the absorption of dietary carbohydrates. |
There are limited studies with this nutraceutical principle in people with T2D. |
We evaluated the postprandial metabolic effects of a natural 2-g powder blend of MLE, fiber, vitamin D3, and chromium, compared with a similar blend without the MLE, sprinkled over a breakfast meal in people with T2D of Asian origin. |
What was learned from this study |
In individuals with T2D, 72% of whom were on metformin, of Asian origin, a natural powder blend of MLE, dietary fiber, vitamin D and chromium significantly reduced the overall glycemic burden and early insulin response when taken with a carbohydrate-rich breakfast, compared to a blend without the MLE. |
The results extend the previous relatively limited knowledge base about effects of MLE in T2D and support its use as a convenient dietary adjuvant to improve PP glucometabolic response. |
Introduction
People with type 2 diabetes (T2D), or with overweight or obesity often, have impaired postprandial (PP) glycemic regulation, ascribed to either insulin resistance, beta-cell dysfunction, or both [1]. Reducing PP hyperglycemia and PP glucose excursions is important for overall glycemic management [2], with implications for symptomatic management and long-term vascular risk [3]. This is particularly important in prediabetes and early stages of T2D, where the relative contribution of PP glucose, as compared with fasting glucose, to HbA1c is more prominent [2]. While there are several pharmaceutical approaches to manage PP glucose, e.g., with fast-acting insulins [4], glinides [5], α-glucosidase inhibitors [6], there are no particular nutritional interventions favored by major scientific societies (e.g., ADA/EASD) [7]; however, most therapeutic lifestyle interventions that reduce caloric intake and attempt to reduce overall carbohydrate intake, in particular, monosaccharides [8], would result in this.
Adults in western countries, such as the USA, obtain approximately half their daily caloric intake from dietary carbohydrates, as illustrated by the Dietary Guidelines for Americans [9]. The latter recommends that carbohydrates should make up between 45% and 65% of the total daily calories in ages 2 years and older [9], whereas in other regions of the world, in particular in Asia, the percentage of carbohydrate intake is higher, which thus poses challenges for glycemic control given some data suggesting that the same food can trigger a slightly higher PP glucose and poorer insulin response than in Caucasians [10]. This is important, as aside from a general reduction in caloric intake, or specific carbohydrate reduction, there are several natural dietary adjuvants that may support reducing the impact of carbohydrates, thus helping improve PP glucose metabolism.
The nutritional principles by which the glycemic impact of dietary carbohydrates can be reduced in general fall into four major categories [10]: (1) by reducing the amount of carbohydrates available for digestion, which usually implies a general reduction in caloric intake, or switching to a low-carbohydrate diet; (2) by reducing the rate of carbohydrate digestion, which could be achieved e.g., by substituting or combining rapidly absorbed carbohydrates with slowly digestible carbohydrates or starch, or other food matrixes that make the carbohydrate less accessible, or by intervening in the gut microbiota (e.g., certain types of dietary fiber [11]); (3) by reducing the rate of glucose absorption, which, e.g., could be accomplished by increasing gut transit time by combining with fiber, or adding natural products that have an inhibitory effect on enzymes involved in carbohydrate cleavage; or (4) increasing the rate of glucose removal from the blood, which could be done by pre-load or with-meal ingestion of products that stimulate the incretin and/or insulin response (e.g., whey proteins [12,13,14]) or improve insulin sensitivity/reduce insulin resistance.
Reducing the rate of glucose absorption is an efficacious principle, and is also the mode of action of a commonly used class of T2D medications, i.e., alpha-glucosidase inhibitors [6]. A natural adjuvant that follows this principle, and that has a long history of use, is mulberry leaf extract (MLE). MLE contains iminosugar alkaloids (i.e., analogues of sugars), of which 1-deoxynojirimycin (DNJ) is the most abundant [15], and predominantly through 1-DNJ, which is structurally similar to glucose (Fig. 1), it competitively blocks the active site of polysaccharide-degrading enzymes in the digestive tract (i.e., α-glucosidases [e.g., sucrase and maltase enzymes]), thus reducing the enzymatic digestion and subsequent absorption of dietary carbohydrates. Of note, other glucose-lowering mechanisms of MLE have been described and linked to the effects of its flavonoid and polyphenolic content (e.g., cholorogenic acid, caffeic acid, coumaric acid, rutin, and quercetin) [16,17,18].
The use of MLE for glucose management has been limited by a lack of a uniform extraction method, rendering the products with a possible unpredictable effect of the MLE. Also, although its principle has been known for centuries in traditional Chinese and Asian medicine [18], its use in the western world has been limited. There have, however, been multiple relatively small studies with MLE in healthy people or people with prediabetes [15, 19,20,21,22,23,24,25,26,27,28], with a few also involving people with T2D [29,30,31,32,33], whose data consistently suggest that there is a moderate effect on PP glucose reduction. Another limitation has been that the MLE has not been extensively studied when taken together with a mixed meal, which would be the typical application of MLE.
We wanted to test the hypothesis that a 2-g blend of MLE, vitamin D, fiber and chromium taken with breakfast could provide clinically meaningful effects on postprandial glucometabolic parameters in individuals with T2D compared to a similar blend without MLE.
Methods
Study Design and Participants
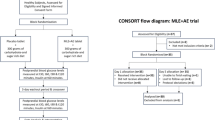
This was a mechanistic, randomized, double-blind, controlled, two-center exploratory crossover study, with a 1-week washout period between interventions, that recruited individuals (men and women age ≥ 18 years) with T2D of Asian origin, who at the time of enrollment were either not taking any medications for glycemic management or were on metformin monotherapy 0.5–3.0 g/day. The study was designed to evaluate the effects of the blend (2 g) containing MLE, compared to a blend without MLE, on PP glucose taken once with a carbohydrate-rich breakfast. We also evaluated the effects on insulin, incretin hormones, inflammation, gastric emptying (GE), and insulin sensitivity (Supplementary Fig. S1). Randomization sequences are depicted in Supplementary Fig. S2. Eligible participants were randomised in a 1:1:1 ratio to receive either sequence ABC, BCA, or CAB on day 1 according to the crossover design randomization schedule developed by SOCAR Research SA. The study protocol was approved by the Institutional Review Board of Orange County Research Center, USA, and Temasek Polytechnic, Glycemic Index Research Unit, Singapore, and the study was carried out in compliance with the Harmonized Tripartite Guideline for Good Clinical Practice from the International Conference on Harmonisation [34] and the Declaration of Helsinki [35]. Signed written informed consent prior to study entry was obtained from all participants.
In addition to a diagnosis of T2D, the other key inclusion criteria were HbA1c 6.5–10.0%; and owing to frequent blood sampling, hematocrit ≥ 34%/40% for women/men, and hemoglobin ≥ 11.0/13.5 g/dL for women/men, respectively. Key exclusion criteria were fasting plasma glucose > 220 mg/dL, estimated glomerular filtration rate (eGFR) < 60 mL/min/1.73 m2, body mass index (BMI) > 35 kg/m2, and ongoing or recent (i.e., < 3 months) treatment with any oral or injectable glucose-lowering medications other than metformin. The full list of in- and exclusion criteria is provided in Supplementary Table S1.
This study included an open-label (OL) exploratory intervention period in which acarbose 100 mg QD was provided as a tablet with the meal and where only glucose and insulin were measured. These results will be reported separately.
Investigational Products
The investigational product was a 2-g blend of MLE in combination with other classical food ingredients that have been reported to modulate glucose. It consisted of 250 mg of MLE, 1.75 g of fiber, 0.75 μg of vitamin D3, and 75 μg of chromium. The blend was tasteless, white in appearance, and was delivered in a stick-pack/sachet to sprinkle on the breakfast meal.
MLE
MLE was supplied as a powder (Reducose®) produced by Phynova (USA), and 250 mg MLE contained 12.5 mg DNJ.
Fiber
The fiber component was provided as resistant maltodextrin (Fibersol®-2, ADM/Matsutani LLC, USA), and an amount of 1.75 g represents approximately 7% of recommended daily value (RDV) in many regions across the globe, where a daily intake for adults of 25–35 g per day is advocated, yet the average intake of dietary fiber by adults worldwide remains low, typically less than 20 g per day. Aside from possible beneficial effects on glucose [11], dietary fiber has also been shown to have several important associations with, e.g., satiety by decreasing hunger, prolonging satiation or increasing satiety signals from the gut [36], metabolic health [37], and mortality [38].
Vitamin D
The vitamin D component of the blend was vitamin D3 (0.75 μg [30 IU]), sourced from DSM (USA). Vitamin D supplementation has been associated with improvements in glycemic control in T2D [39].
Chromium
The chromium blend-component (75 μg chromium picolinate) was sourced from Nutrition 21 (NJ, USA). Several randomized, placebo-controlled clinical trials have demonstrated glucometabolic benefits of various dosages of chromium picolinate taken for periods of 4 weeks to 4 months [40,41,42,43].
Comparator Blend
The comparator blend without MLE consisted of the same ingredients as the blend with MLE, with the exception of the MLE, which was substituted by fiber (250 mg Fibersol®-2) to achieve weight equivalence. The blend was tasteless, off-white in appearance, and was delivered in a stick-pack/sachet with an identical appearance to the blend with the MLE.
Interventions and Meals
To standardize the physiologic conditions ahead of the lunch meal, participants were required to fast overnight (at least 10 h) prior to site arrival in the morning, whereupon blood samples were drawn (t = 0). The intervention was thereafter to be directly sprinkled on top of the breakfast meal and consumed within 15 min. Breakfast was standardized at both sites, and consisted of two slices white bread, two slices of gouda cheese (20 g), and 250 mL apple juice, which contributed in total 350.2 kcal (10.0 g protein, 6.5 g fat, and 55.4 g of carbohydrates). At the start of breakfast, 1 g of acetaminophen (paracetamol), with 150 mL water, was consumed for GE assessment. Exposure to intervention was monitored and captured in the case report form.
All participants, during each period had thereafter frequent blood sampling conducted for glucometabolic, incretin, and inflammation and GE assessment (sampling scheme depicted in Supplementary Fig. S1). All blood samples were taken from subjects by venipuncture or cannulation, and serum and plasma were prepared using standard procedures.
Primary Exploratory Endpoint
The exploratory study hypothesis was that a with-meal blend of MLE combined with other bioactive ingredients, taken with a mixed meal with a relatively high amount of carbohydrates, would lower the PP blood glucose levels compared to the same blend without the MLE, in individuals with T2D. Thus the primary endpoint was to assess the effects on PP glucose over the full observation period, which included assessments at t = 0 (i.e., pre-meal assessment) and thereafter at t = 15, 30, 60, 120, and 180 min (post-meal assessment). Although this was an exploratory study, we defined the 3-h incremental area under the curve (iAUC) as the primary analysis, mainly for sample size estimation. Glucose was analyzed in EDTA-plasma (Cobas c501 System, Roche Diagnostics, Indianapolis, USA).
Other Metabolic Endpoints
Interval blood samples following the same sampling schedule as for glucose, i.e., to 3 h, were also collected for insulin (serum, Immulite 2000 Analyzer, Consolidated Medical Bio-Analysis, Inc., USA), total GLP-1 (EDTA-plasma, MSD, USA), total GIP (EDTA-plasma, Millipore, USA), and interleukin-6 (serum, electrochemiluminescence immunoassay, Labcorp, Burlington, NC, USA).
Effect on Insulin Sensitivity
Whole-body insulin sensitivity was calculated using the Matsuda index (MI), a formula based on insulin and glucose values measured during the test [44], and where higher values indicate more insulin sensitivity. Although the classical approach for calculating the MI is based on an oral glucose tolerance test, it has been demonstrated that a mixed meal can also be applied to derive it [45, 46].
Gastric Emptying (GE) Assessment
Orally administered acetaminophen (N-acetyl-p-aminophenol, paracetamol) is poorly absorbed by the stomach but is rapidly absorbed within the small intestine; thus, GE is the rate-limiting step for the appearance of acetaminophen within blood [47]. Maximum acetaminophen concentrations typically occur approximately 30–60 min post-ingestion; therefore, iAUC, often assessed during the first 60 min, is used as a marker of GE rates, although 2 or 3 h is also frequently reported. Herein we assessed iAUC 0–1 h, 0–2 h, and 0–3 h in interval blood samples [t = 0 (just before start of meal/paracetamol consumption, and post-meal t = 15, 30, 60, 120, and 180 min] following ingestion of 1 g acetaminophen with 150 mL of water. Acetaminophen was analyzed by Sannova Analytical Inc (NJ, USA) using Sciex instruments (liquid chromatographic method, Waltham, MA, USA).
Safety and Adverse Events (AEs)
General safety laboratory tests were performed at the screening visit. Occurrence of AEs was proactively assessed by queries at all visits post screening, and all AEs (spontaneously reported or enquired, as well as those observed) during the course of the study were captured and summarized descriptively.
AEs was coded using Medical Dictionary for Regulatory Activities (MedDRA), Version 23.0.
Statistical Methods and Sample Size Considerations
We defined that the sample size had to be sufficiently large to show a difference of 15% in the incremental area under the curve for iAUC 0–3 h of PP glycemic excursion between the blend with and without MLE. We used a coefficient of variation (CV) approach and on the basis of two previous studies assessing PP glucose trajectories [48, 49] reporting this to be 0.41 and 0.50, we assumed a CV of 0.46. The within-patient correlation observed from a different study was 0.88 (data on file), so we conservatively assumed this would be 0.85. With a repeated measures one-way analysis of variance (ANOVA), 25 completers would then be required to show a statistically significant difference of 15% in iAUC 0–3 h for glucose, at an α-level of 0.05 with a power of 80%.
Patient characteristics were described using mean (standard deviation) for continuous variables and proportions for categorical variables and were reported for the overall population, by study site, and according to initial treatment sequence. eGFR was derived by the Modification of Diet in Renal Disease (MDRD) study equation [50]. The differences in endpoints between the blend with and without MLE were assessed by comparing changes in iAUC between the two interventions over different time periods using ANOVA. The model was adjusted for investigational product, site (i.e., USA or Singapore), and period. P values for the primary, secondary, and additional post hoc exploratory endpoints were not adjusted for multiple comparisons.
All biomarkers were analyzed with an iAUC approach. Relative differences between treatment groups were calculated in percent as estimated treatment difference/estimated mean for placebo × 100%. We also assessed if there were differences in both the time to reach maximum concentration levels of the biomarkers (Tmax) and in the maximum levels of the biomarkers reached (Cmax). Correlations between age, weight, and the MI were analyzed using Pearson’s correlation, and their relation to gender, by a Wilcoxon test. A descriptive analysis by intervention group for glucose iAUC 0–1 h, 0–2 h, and 0–3 h by intervention sequence and period was performed post hoc.
Results
In total 30 individuals (12 women) were enrolled, of whom 29 completed all treatment sequences. One participant withdrew informed consent as outlined in the consort diagram (Supplementary Fig. S2) and exposure to interventions was 100%. Baseline characteristics are provided in Table 1. The mean (SD) age was 58.9 (11.3) years, HbA1c 7.1 (0.8)%/54.0 (8.8) mmol/mol, diabetes duration (7.1 (5.5) years, and eGFR 88.8 (24.8) ml/min/1.73 m2. BMI was 26.5 (4.4) kg/m2, with weight and waist circumference of 73.3 (14.2) kg and 92.9 (11.2) cm, respectively. Twenty-two (73.3%) used concomitant metformin. The baseline characteristics were largely similar between participants from the USA and Singapore with the exception of age and weight; US participants were older and were more overweight. Baseline characteristics were also largely similar regardless of which intervention that was given as the initial sequence (Supplementary Table S2).
Effects on PP Glucose
The with-meal MLE-based blend significantly altered the PP glucose trajectory (Fig. 2, Table 2), and reduced 1 h iAUC by 19.5% [mean (95% CI) ΔiAUC0–60min vs blend without MLE − 0.6 (− 0.8, − 0.3) mmol/L × h, p < 0.0001], 2 h iAUC by 16.6% [ΔiAUC0−120min vs blend without MLE − 1.2 [− 1.8, − 0.6) mmol/L × h, p = 0.0002], and 3 h iAUC by 14.9% [ΔiAUC0−180min vs blend without MLE − 1.4 [− 2.4, − 0.5) mmol/L × h, p = 0.0032]. The magnitude of effect on PP glucose trajectory appeared not to be affected by intervention sequence or period (Supplementary Table S3), suggesting that the washout was complete.
Maximum incremental glucose level (Table 3) was also significantly reduced with the MLE-based blend [mean (95% CI) difference in Cmax vs blend without MLE − 0.8 (− 1.2, − 0.3) mmol/L, p = 0.0006], but not time to reach it (Tmax). The 2-h PP glucose level with the blend with MLE was numerically lower, but not statistically significant [difference vs blend without MLE − 0.4 (− 1.0, 0.1), p = 0.1220]. All analysis were adjusted for product, site, and period.
Effects on PP Insulin
The early (0–60 min) insulin trajectory (Fig. 3, Table 2) was also modulated with the blend with MLE; a reduction of 23.7% in the iAUC was observed [ΔiAUC0−60min vs blend without MLE − 3.4 (− 6.3, − 0.5) μU/mL × h, p = 0.0236], whereas the 2-h and 3-h values were numerically but not significantly reduced. There were no differences in insulin Cmax or Tmax (Table 3).
Effects on Insulin Sensitivity
There were no differential effects of the blend with MLE versus the blend without on the Matsuda index (MI) (Supplementary Table S4).
There was a statistical significant relationship between insulin sensitivity and age with both interventions (blend with MLE ρ = 0.51, p = 0.0053; blend without MLE ρ = 0.57, p = 0.0017) assessed by Spearman’s correlation analysis, and a numerical (but not significant) inverse relationship between insulin sensitivity and body weight (blend with MLE ρ = − 0.32, p = 0.0991; blend without MLE ρ = − 0.26, p = 0.1891). Men tended to be more insulin sensitive, but no statistical differences were observed between sexes (blend with MLE, median (95% CI) MImen 5.62 (3.94, 7.96) vs MIwomen 2.67 (2.02, 10.39); Wilcoxon p = 0.3071; blend without MLE MImen 6.97 (3.48, 14.91) vs MIwomen 2.57 (2.16, 7.20); Wilcoxon p = 0.0608).
Effects on Gut Hormones and IL-6
There were no differential effects of the blend with MLE versus the blend without on the GLP-1 or IL-6 response, neither for overall exposure expressed as iAUC (Table 2) nor Cmax and Tmax (Table 3). The GIP response on the other hand differed and overall there was a reduced GIP response (Table 2) with the blend containing MLE [ΔiAUC0−60min vs blend without MLE − 7.5 (−12.0, −2.9) pmol/L × h, p < 0.0023; ΔiAUC0−120min vs blend without MLE −16.8 (−26.2, −7.4) pmol/L × h; ΔiAUC0−180min vs blend without MLE −24.5 (−37.2, −11.8) pmol/L × h, p = 0.0003]. Also, Cmax was less with the MLE blend [difference in Cmax vs blend without MLE − 13.5 (− 20.9, − 6.0) pmol/L, p = 0.0006], but not Tmax (Table 3).
Effects on GE
No differential effects of the blend with MLE versus the blend without were observed for GE (Tables 2, 3).
Safety and Adverse Events
There were no serious adverse events reported in this study, but one individual experienced fatigue after intake of the blend with MLE that resolved after 4 days.
Discussion
In individuals with T2D of Asian origin, a 2-g natural powder blend of MLE, dietary fiber, vitamin D, and chromium significantly reduced the overall glycemic burden and early insulin response when taken with a carbohydrate-rich breakfast, compared to a blend without the MLE. These results are interesting from several perspectives. Not only do they extend the previous relatively limited knowledge base about MLE effects in T2D [29,30,31,32,33] but they also add to the literature that this principle, with a refined MLE, supports obtaining healthy glucose levels and works even in the context of taking it with a mixed meal, specifically breakfast, which is identified as perhaps the most impactful meal in regulation of diurnal glucose levels in people without [51] or with T2D [52]. These data also confirm that the predominant mode of action of MLE is through reducing the rate of glucose absorption, underscored by reductions in iAUC and Cmax of glucose, and a reduced early insulin response, without notable effects, as also reported by others, on insulin sensitivity [22], GLP-1, or GE.
In this study, we observed a differential effect on GIP where a reduced GIP response was seen with the MLE-based blend, which is at variance with the data observed for the other incretin analyzed in this study, i.e., GLP-1. Aside from potential unknown assay issues, this could be related to the reduced hyperosmolarity of glucose in the duodenum and a reduced glucose load for the nutrient-sensing L cells, related to the inhibition of enzymes involved in carbohydrate cleavage [53, 54], which find support from observations reported by interventions following similar treatment principles specifically for GIP [55, 56]. Another more speculative theory is that the blend with MLE contributes to an acute improvement in “GIP resistance”, a pathophysiologic feature described in T2D of unknown clinical relevance [57].
An interesting concept with this blend, and which represents a study novelty, is that in contrast to many previous studies conducted with MLE, we combined the MLE with three other bioactive ingredients, i.e., vitamin D3, chromium, and dietary fiber, with the rationale that these additional ingredients of the blend would represent a reasonable source of these (micro)nutrients, given that many people across the globe are on the lower side of adequate daily nutrient intake, which is in particular true for people with T2D [58,59,60]. In addition, these ingredients have been implied to offer glycemic benefits [36, 37, 39,40,41,42,43, 61] which may offer additivity with the MLE, although some of the effects of particular blend ingredients for glucose benefits have been debated [62,63,64], in particular low-dose vitamin D3. Thus, this mix can provide added nutritional value to people with T2D, thus supporting long-term adherence, which is also supported by recent guidelines [65] that now advocate a “patient-centered approach,” where, for many people with T2D, nutritional supplements, if supported by evidence, tend to be desired over adding another medication.
Limitations and Strengths
Although combining MLE with other bioactive ingredients is a strength and novelty of this study, the combinatory approach might also be considered a limitation of the current study, as it gives rise to difficulties in comparing the results with studies involving only MLE versus a metabolically inert comparator.
Additional limitations of this study include acute dosing only in relation to a breakfast meal, and we can therefore not extrapolate the results directly to what happens with longer-term use, or to use with multiple meals per day. However, it is conceivable to believe that the glucometabolic effects would be long-lasting, as seen in other longer-term studies using MLE [15, 25,26,27, 32, 33], and also would work when given twice or thrice daily [15, 25,26,27, 32, 33]. A reduction in iAUC of 15–20% we believe is relevant, as illustrated by the effect of the pharmaceutical agent linagliptin, where a lowering of 3-h AUC of 14.7% translated into a 0.22%-point HbA1c reduction after 4 weeks [66]. We also included participants with Asian origin only, which may not be representative of how other populations may respond. However, as there is a large amount of supportive data in other populations [67], in particular in Caucasians [19, 21, 28, 31, 33], we do think that the results are reasonably translatable. Finally, there were some differences in baseline characteristics between the participants from the US and Singapore site, and owing to sample size, some post hoc analyses were not evaluated statistically. The latter could potentially have influenced some results; however, we did adjust for site in our statistical approach, which should take care of this potential confounder.
Conclusions
A 2-g natural powder blend of MLE and dietary fiber, vitamin D, and chromium significantly reduced the overall glycemic burden and early insulin response when taken with a carbohydrate-rich breakfast in T2D, compared to a blend without the MLE, suggesting its use as a convenient dietary adjuvant to improve PP glucometabolic response.
References
Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia. 2003;46(1):3–19.
Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26(3):881–5.
Qiao Q, Tuomilehto J, Borch-Johnsen K. Post-challenge hyperglycaemia is associated with premature death and macrovascular complications. Diabetologia. 2003;46(Suppl 1):M17-21.
Yacoub T. Impact of improving postprandial glycemic control with intensifying insulin therapy in type 2 diabetes. Postgrad Med. 2017;129(8):791–800.
Monnier L, Colette C. Targeting prandial hyperglycemia: how important is it and how best to do this? Curr Diab Rep. 2008;8(5):368–74.
Holman RR, et al. Effects of acarbose on cardiovascular and diabetes outcomes in patients with coronary heart disease and impaired glucose tolerance (ACE): a randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2017;5(11):877–86.
Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia, 2022;65(12):1925–66.
Chang CR, Francois ME, Little JP. Restricting carbohydrates at breakfast is sufficient to reduce 24-hour exposure to postprandial hyperglycemia and improve glycemic variability. Am J Clin Nutr. 2019;109(5):1302–9.
U.S. Department of Health and Human Services and U.S. Department of Agriculture. Dietary Guidelines for Americans, 2020–2025. 2020; 9th. https://www.dietaryguidelines.gov/sites/default/files/2021-03/Dietary_Guidelines_for_Americans-2020-2025.pdf. Accessed Jan 3 2023.
Wee MSM, Henry CJ. Reducing the glycemic impact of carbohydrates on foods and meals: strategies for the food industry and consumers with special focus on Asia. Compr Rev Food Sci Food Saf. 2020;19(2):670–702.
EFSA Panel on Dietetic Products, Nutrition and Allergies (NDA). Scientific Opinion on the substantiation of health claims related to beta-glucans from oats and barley and maintenance of normal blood LDL-cholesterol concentrations (ID 1236, 1299), increase in satiety leading to a reduction in energy intake (ID 851, 852), reduction of post-prandial glycaemic responses (ID 821, 824), and “digestive function” (ID 850) pursuant to Article 13(1) of Regulation (EC) No 1924/2006. EFSA J. 2011;9(6):2207.
Kung B, Anderson GH, Paré S, et al. Effect of milk protein intake and casein-to-whey ratio in breakfast meals on postprandial glucose, satiety ratings, and subsequent meal intake. J Dairy Sci. 2018;101(10):8688–701.
Sartorius T, Weidner A, Dharsono T, Boulier A, Wilhelm M, Schön C. Correction: Sartorius et al. "Postprandial effects of a proprietary milk protein hydrolysate containing bioactive peptides in prediabetic subjects" Nutrients 2019, 11, 1700. Nutrients. 2020;12(5):1266.
Clifton PM, Galbraith C, Coles L. Effect of a low dose whey/guar preload on glycemic control in people with type 2 diabetes–a randomised controlled trial. Nutr J. 2014;13:103.
Kimura T, Nakagawa K, Kubota H, et al. Food-grade mulberry powder enriched with 1-deoxynojirimycin suppresses the elevation of postprandial blood glucose in humans. J Agric Food Chem. 2007;55(14):5869–74.
Varghese SM, Thomas J. Polyphenolic constituents in mulberry leaf extract (M. latifolia L. cv. BC259) and its antidiabetic effect in streptozotocin induced diabetic rats. Pak J Pharm Sci. 2019;32(1):69–74.
Thaipitakwong T, Numhom S, Aramwit P. Mulberry leaves and their potential effects against cardiometabolic risks: a review of chemical compositions, biological properties and clinical efficacy. Pharm Biol. 2018;56(1):109–18.
Amin AR, Kassab RB, Abdel Moneim AE, Amin HK. Comparison among garlic, berberine, resveratrol, Hibiscus sabdariffa, genus Zizyphus, hesperidin, red beetroot, Catha edulis, Portulaca oleracea, and mulberry leaves in the treatment of hypertension and type 2 DM: a comprehensive review. Nat Prod Commun. 2020;15. https://doi.org/10.1177/1934578X20921623.
Lown M, Fuller R, Lightowler H, et al. Mulberry-extract improves glucose tolerance and decreases insulin concentrations in normoglycaemic adults: results of a randomised double-blind placebo-controlled study. PLoS ONE. 2017;12(2):e0172239.
Wang R, Li Y, Mu W, et al. Mulberry leaf extract reduces the glycemic indexes of four common dietary carbohydrates. Medicine (Baltimore). 2018;97(34): e11996.
Józefczuk J, Malikowska K, Glapa A, et al. Mulberry leaf extract decreases digestion and absorption of starch in healthy subjects-a randomized, placebo-controlled, crossover study. Adv Med Sci. 2017;62(2):302–6.
Bumrungpert A, Sukriket P, Lookhanumarnjao S. The effect of mulberry leaf tea on postprandial glycemic control and insulin sensitivity: a randomized, placebo-controlled crossover study. J Pharmacy Nutr Sci. 2016;6:33–37.
Chung HI, Kim J, Kim JY, Kwon O. Acute intake of mulberry leaf aqueous extract affects postprandial glucose response after maltose loading: Randomized double-blind placebo-controlled pilot study. J Funct Foods. 2013;5(3):1502–6.
Mela DJ, Cao XZ, Dobriyal R, et al. The effect of 8 plant extracts and combinations on post-prandial blood glucose and insulin responses in healthy adults: a randomized controlled trial. Nutr Metab (Lond). 2020;17:51.
Kim JY, Ok HM, Kim J, et al. Mulberry leaf extract improves postprandial glucose response in prediabetic subjects: a randomized, double-blind placebo-controlled trial. J Med Food. 2015;18(3):306–13.
Asai A, Nakagawa, K. Higuchi, O, et al. Effect of mulberry leaf extract with enriched 1-deoxynojirimycin content on postprandial glycemic control in subjects with impaired glucose metabolism. J Diabetes Investig. 2011;2(4):318–23.
Thaipitakwong T, Supasyndh, O, Rasmi, Y, Aramwit, P. A randomized controlled study of dose-finding, efficacy, and safety of mulberry leaves on glycemic profiles in obese persons with borderline diabetes. Complement Ther Med. 2020;49:102292.
Gheldof N, Francey, C. Rytz, A, et al. Effect of different nutritional supplements on glucose response of complete meals in two crossover studies. Nutrients. 2022;14(13):2674.
Banu S, Jabir NR, Manjunath NC, et al. Reduction of post-prandial hyperglycemia by mulberry tea in type-2 diabetes patients. Saudi J Biol Sci. 2015;22(1):32–6.
Nakamura S, Hashiguchi M, Yamaguchi Y, Oku T. Hypoglycemic effects of Morus alba leaf extract on postprandial glucose and insulin levels in patients with type 2 diabetes treated with sulfonylurea hypoglycemic agents. J Diabetes Metab. 2011;2:158.
Mudra M, Ercan-Fang N, Zhong L, Furne J, Levitt M. Influence of mulberry leaf extract on the blood glucose and breath hydrogen response to ingestion of 75 g sucrose by type 2 diabetic and control subjects. Diabetes Care. 2007;30(5):1272–4.
Andallu B, Suryakantham V, Lakshmi SB, Reddy GK. Effect of mulberry (Morus indica L.) therapy on plasma and erythrocyte membrane lipids in patients with type 2 diabetes. Clin Chim Acta. 2001;314(1–2):47–53.
Riche DM, Riche KD, East HE, Barrett EK, May WL. Impact of mulberry leaf extract on type 2 diabetes (Mul-DM): a randomized, placebo-controlled pilot study. Complement Ther Med. 2017;32:105–8.
European Agency for the Evaluation of Medicinal Products. Guideline for Good Clinical Practice. Accessed 2021 Sept 21. https://www.ema.europa.eu/en/documents/scientific-guideline/ich-guideline-good-clinical-practice-e6r2-step-5_en.pdf
World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. Adopted by the 18th WMA General Assembly, Helsinki, Finland, June 1964 last amended at the 64th WMA General Assembly, Fortaleza, Brazil, October 2013. Accessed 2021 Sept 22.
Astina J, Sapwarobol S. Resistant maltodextrin and metabolic syndrome: a review. J Am Coll Nutr. 2019;38(4):380–5.
Stachowska E, Portincasa P, Jamioł-Milc D, Maciejewska-Markiewicz D, Skonieczna-Żydecka K. The relationship between prebiotic supplementation and anthropometric and biochemical parameters in patients with NAFLD-a systematic review and meta-analysis of randomized controlled trials. Nutrients. 2020;12(11):3460.
Kim Y, Je Y. Dietary fibre intake and mortality from cardiovascular disease and all cancers: a meta-analysis of prospective cohort studies. Arch Cardiovasc Dis. 2016;109(1):39–54.
Derosa G, D'Angelo A, Martinotti C, et al. Vitamin D3 supplementation improves glycemic control in type 2 diabetic patients: results from an Italian clinical trial. Int J Vitam Nutr Res. 2022;92(2):91–100.
Jovanovic L, Gutierrez M, Peterson CM. Chromium supplementation for women with gestational diabetes mellitus. J Trace Elements Exp Med. 1999;12(2):91–7.
Ghosh D, Bhattacharya B, Mukherjee B, et al. Role of chromium supplementation in Indians with type 2 diabetes mellitus. J Nutr Biochem. 2002;13(11):690–7.
Anderson RA, Cheng N, Bryden NA, et al. Elevated intakes of supplemental chromium improve glucose and insulin variables in individuals with type 2 diabetes. Diabetes. 1997;46(11):1786–91.
Asbaghi O, Fatemeh N, Mahnaz RK, et al. Effects of chromium supplementation on glycemic control in patients with type 2 diabetes: a systematic review and meta-analysis of randomized controlled trials. Pharmacol Res. 2020;161: 105098.
Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999;22(9):1462–70.
Li J, Gower B, McLain A, Yarar-Fisher C. Effects of a low-carbohydrate/high-protein diet on metabolic health in individuals with chronic spinal cord injury: an exploratory analysis of results from a randomized controlled trial. Physiol Rep. 2022;10(22):e15501.
Maki KC, McKenney JM, Farmer MV, Reeves MS, Dicklin MR. Indices of insulin sensitivity and secretion from a standard liquid meal test in subjects with type 2 diabetes, impaired or normal fasting glucose. Nutr J. 2009;8(1):22.
Willems M, Quartero AO, Numans ME. How useful is paracetamol absorption as a marker of gastric emptying? A systematic literature study. Dig Dis Sci. 2001;46(10):2256–62.
Watson LE, Phillips LK, Wu T, et al. Differentiating the effects of whey protein and guar gum preloads on postprandial glycemia in type 2 diabetes. Clin Nutr. 2019;38(6):2827–32.
de Carvalho CM, de Paula TP, Viana LV, Machado VM, de Almeida JC, Azevedo MJ. Plasma glucose and insulin responses after consumption of breakfasts with different sources of soluble fiber in type 2 diabetes patients: a randomized crossover clinical trial. Am J Clin Nutr. 2017;106(5):1238–45.
Levey AS, Coresh J, Greene T, et al. Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med. 2006;145(4):247–54.
Ogata H, Kayaba M, Tanaka Y, et al. Effect of skipping breakfast for 6 days on energy metabolism and diurnal rhythm of blood glucose in young healthy Japanese males. Am J Clin Nutr. 2019;110(1):41–52.
Jakubowicz D, Wainstein J, Ahren B, Landau Z, Bar-Dayan Y, Froy, O. Fasting until noon triggers increased postprandial hyperglycemia and impaired insulin response after lunch and dinner in individuals with type 2 diabetes: a randomized clinical trial. Diabetes Care. 2015;38(10):1820–6.
Thorens B. Glucagon-like peptide-1 and control of insulin secretion. Diabetes Metab. 1995;21(5):311–8.
El K, Gray SM, Capozzi ME, et al. GIP mediates the incretin effect and glucose tolerance by dual actions on on α cells and β cells. Sci Adv. 2021;7(11):eabf1948.
Groop PH, Groop L, Tötterman KJ, Fyhrquist F. Effects of acarbose on the relationship between changes in GIP and insulin responses to meals in normal subjects. Acta Endocrinol (Copenh). 1986;112(3):361–6.
Hücking K, Kostic Z, Pox C, et al. Alpha-glucosidase inhibition (acarbose) fails to enhance secretion of glucagon-like peptide 1 (7–36 amide) and to delay gastric emptying in type 2 diabetic patients. Diabet Med. 2005;22(4):470–6.
Timper K, Grisouard J, Sauter NS, et al. Glucose-dependent insulinotropic polypeptide induces cytokine expression, lipolysis, and insulin resistance in human adipocytes. Am J Physiol Endocrinol Metab. 2013;304(1):E1-13.
Holick MF. The vitamin D deficiency pandemic: approaches for diagnosis, treatment and prevention. Rev Endocr Metab Disord. 2017;18(2):153–65.
Kaur B, Henry J. Micronutrient status in type 2 diabetes: a review. Adv Food Nutr Res. 2014;71:55–100.
Gross LS, Li L, Ford ES, Liu S. Increased consumption of refined carbohydrates and the epidemic of type 2 diabetes in the United States: an ecologic assessment. Am J Clin Nutr. 2004;79(5):774–9.
Chandalia M, Garg A, Lutjohann D, von Bergmann K, Grundy SM, Brinkley LJ. Beneficial effects of high dietary fiber intake in patients with type 2 diabetes mellitus. N Engl J Med. 2000;342(19):1392–8.
Marquina C, Mousa A, Scragg R, de Courten B. Vitamin D and cardiometabolic disorders: a review of current evidence, genetic determinants and pathomechanisms. Obes Rev. 2019;20(2):262–77.
Al Thani M, Sadoun E, Sofroniou A, et al. The effect of vitamin D supplementation on the glycemic control of pre-diabetic Qatari patients in a randomized control trial. BMC Nutr. 2019;5:46.
Lee NA, Reasner CA. Beneficial effect of chromium supplementation on serum triglyceride levels in NIDDM. Diabetes Care. 1994;17(12):1449–52.
ElSayed NA, Aleppo G, Aroda VR, et al. Facilitating positive health behaviors and well-being to improve health outcomes: standards of care in diabetes—2023. Diabetes Care. 2022;46(Suppl_1):S68–S96.
Rauch T, Graefe-Mody U, Deacon CF, et al. Linagliptin increases incretin levels, lowers glucagon, and improves glycemic control in type 2 diabetes mellitus. Diabetes Ther. 2012;3(1):10. https://doi.org/10.1007/s13300-012-0010-y.
Phimarn W, Wichaiyo K, Silpsavikul K, Sungthong B, Saramunee K. A meta-analysis of efficacy of Morus alba Linn. to improve blood glucose and lipid profile. Eur J Nutr. 2017;56(4):1509–21.
Acknowledgements
The authors thank all the study participants and site personnel involved in the study, including Saihah Mohd Salleh, Low Win Nie, and Sharifah Fatanah at Temasek Polytechnic, Singapore. We also acknowledge the early statistical review by Alexander Smith, a former employee of Aimmune, USA and the late statistical review by Zoltan Magos, Aimmune Ltd, UK, the operational work by Bridget Etienne, NHSc and the team at Bionical-EMAS, and the support by Daniela Trevino, NHSc Bridgewater, by Shreeram Sathya, Allan Lim, Elvira Suniega. NHSc Singapore. We also appreciate useful comments from Andrea Hawkinson and David Philippe, NHSc, and the statistical work by Emilie Perrin and Sophie de Brouwer, SOCAR Research SA.
Funding
This study, and the journal’s Rapid Service fee, was funded by Nestlé Health Science (NHSc), Switzerland.
Author Contributions
Study design: OA, MVE and OEJ; Study Methodology: MM, RZ, KB, JN, BNMY, LM, LY, BK, OA, MVE and OEJ; Researched data: KB, JN; Performed statistical analyses: BK; Writing – original draft, OEJ; Writing – review & editing, all authors contributed to the discussion and reviewed/edited the article and approved the final version for submission.
Prior Presentation
A limited portion of this work was presented in abstract form at the American Diabetes Association meeting June 2022, accepted as a late-breaking poster (poster #41-LB).
Disclosures
Maufauzy Mohamed has received consulting fees from NHSc, Roberto Luis Zagury report speaker fees from Abbott, NHSc, Novo Nordisk, AstraZeneca, Merck, Servier, Boehringer Ingelheim, Eli Lilly, and Brace Pharma, Kalpana Bhaskaran has nothing to report, Joel Neutel has received investigator study fees from NHSc, Barakatun Nisak Mohd Yusof has received consulting fees from NHSc, Linda Mooney, Lihe Yeo, Olivier Aprikan, Maximilian von Eynatten and Odd Erik Johansen are employees of NHSc. Bridget Kirwan is an employee of SOCAR Research SA, which recieved funding from NHSc for statistcal work.
Compliance with Ethics Guidelines
The study was conducted in accordance with the Declaration of Helsinki and the study protocol approved by the WCG IRB, USA, with reference number IRB Tracking Number 20213262 and the Temasek Polytechnic Institutional Review Board, Singapore, with reference number IRB201102-Amd1. Signed written informed consent prior to study entry was obtained from all participants.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mohamed, M., Zagury, R.L., Bhaskaran, K. et al. A Randomized, Placebo-Controlled Crossover Study to Evaluate Postprandial Glucometabolic Effects of Mulberry Leaf Extract, Vitamin D, Chromium, and Fiber in People with Type 2 Diabetes. Diabetes Ther 14, 749–766 (2023). https://doi.org/10.1007/s13300-023-01379-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-023-01379-4