Abstract
The management of type 2 diabetes (T2D) involves decreasing plasma glucose levels and reducing cardiovascular and microvascular complications. Diabetic kidney disease (DKD), defined as presence of albuminuria, impaired glomerular filtration, or both, is an insidious microvascular complication of diabetes that generates a substantial personal and clinical burden. The progressive reduction in renal function and increased albuminuria results in an increase of cardiovascular events. Thus, patients with DKD require exhaustive control of the associated cardiovascular risk factors. People with diabetes and renal impairment have fewer options of antidiabetic drugs because of contraindications, adverse effects, or altered pharmacokinetics. Sodium–glucose cotransporter type 2 inhibitors (SGLT2i) reduce blood glucose concentrations by blocking the uptake of sodium and glucose in the proximal tubule and promoting glycosuria, and these agents now have an important role in the management of T2D. The results of several cardiovascular outcomes trials suggested that SGLT2i are associated with improvements in renal endpoints in addition to their reduction in cardiovascular events and mortality, which represents a major advance in the care of this population. The dedicated kidney outcomes trials have confirmed the renoprotective action of SGLT2i across different glomerular filtration and albuminuria values, even in patients with non-diabetic chronic kidney disease. Notably, this improvement in kidney function may indirectly benefit cardiac function through multifaceted interorgan cross talk, which can break the cardiorenal vicious circle linked to T2D. In this article, we briefly review the different mechanisms of action that may explain the renal beneficial effects of SGLT2i and disclose the results of the key renal outcome trials and the subsequent update of related clinical guidelines.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The management of type 2 diabetes (T2D) involves decreasing plasma glucose levels and reducing macrovascular and microvascular complications, including chronic kidney disease (CKD). |
Sodium–glucose cotransporter type 2 inhibitors (SGLT2i) lower blood glucose concentrations by blocking the uptake of sodium and glucose in the renal proximal tubule and promoting glycosuria. |
In addition to the metabolic and cardiovascular benefits, SGLT2i have also demonstrated renoprotective effects across different glomerular filtration and albuminuria values in patients with and without T2D. |
SGLT2i are changing the clinical management of T2D owing to their renal and cardiovascular protection. This can benefit patients with early stages of disease and also those with established cardiovascular and/or renal disease, and even patients without diabetes. |
Introduction
The kidneys are involved in regulating glucose homeostasis, and glucose reabsorption through sodium–glucose cotransporters located in the proximal tubules is one of their tasks [1]. The management of type 2 diabetes (T2D) involves decreasing plasma glucose levels and reducing macrovascular and microvascular complications, including chronic kidney disease (CKD). There have been limited treatment options beyond glycemic control and antihypertensive agents to slow kidney disease progression in these patients. In fact, since the development of renin–angiotensin–aldosterone system (RAAS) inhibitors, such as angiotensin-converting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), almost 20 years ago, no new treatments have become available. Moreover, people with diabetes and CKD may have fewer options of antidiabetic drugs because of contraindications, adverse effects, or altered pharmacokinetics.
Sodium–glucose cotransporter type 2 inhibitors (SGLT2i) are the newest drug class for the management of hyperglycemia in T2D, as they lower blood glucose concentrations by blocking the uptake of sodium and glucose in the proximal tubule and promote glycosuria [2]. In patients with impaired kidney function, the filtered glucose load is reduced and their effectiveness may be blunted [3]. Thus, these agents were initially approved for use as glucose-lowering drugs for people with T2D and (nearly) preserved kidney function. However, the results of several cardiovascular outcomes trials (CVOTs) suggested that SGLT2i are associated with improvements in renal endpoints apart from their reduction in cardiovascular events and mortality [4,5,6], which represents a major advance in the care of this population. On the basis of the findings of CVOTs, dedicated kidney outcomes trials (such as DAPA-CKD and CREDENCE) have been conducted, confirming the renoprotective benefit of SGLT2i across different glomerular filtration and albuminuria values [7, 8]. Herein, we briefly review the different mechanisms of action that may explain the renal beneficial effects of SGLT2i and disclose the results of the key renal outcome trials and the subsequent update of related clinical guidelines. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
CKD and T2D: Dance Partners in CV Disease
The burden of diabetes and hypertension, both considered as leading drivers of CKD, has increased significantly over recent decades. Diabetic kidney disease (DKD), defined as presence of albuminuria, impaired glomerular filtration, or both, is an insidious microvascular complication of diabetes that develops in approximately 40% of patients with T2D and accounts for more than 50% of new patients beginning renal replacement therapy [9, 10]. Apart from genetic susceptibility, the pathogenic mechanisms that contribute to DKD involve metabolic, hemodynamic, profibrotic, and inflammatory factors, which ultimately lead to the development of end-stage kidney disease (ESKD) [11]. As per chronic hyperglycemia, a classic study that followed patients with T2D during 11 years demonstrated a strong association between glycemic control and the incidence of CKD, regardless previous traditional risk factors for CKD and even in the absence of albuminuria and retinopathy [12]. Together with hypertension and hyperglycemia, other risk factors for DKD are older age, early-onset diabetes, and the presence of albuminuria [13, 14] and diabetic retinopathy [15].
Patients with DKD may initially exhibit glomerular hyperfiltration, a process that leads to a progressive reduction in estimated glomerular filtration rate (eGFR) and increased albuminuria, which results in an increase of cardiovascular events [16]. Despite optimal preventive and treatment strategies, classically based on lifestyle modification, reduction of blood glucose levels, lipid levels, and blood pressure and the use of RAAS inhibitors, patients with T2D remain at high risk of developing/worsening renal and cardiovascular complications [17,18,19]. According to the Global Burden of Disease Study 2017, almost 7% of the total cardiovascular disease burden can be attributed to impaired kidney function [20]. Indeed, patients with DKD seem to concentrate most of the excess of all-cause and cardiovascular mortality risk among patients with T2D, with a sixfold higher risk for mortality associated with albuminuria and 15-fold higher risk with the combination of albuminuria and decreased GFR [21]. Micro- and macroalbuminuria are associated with higher risks of incident ischemic stroke, myocardial infarction, and all-cause mortality in patients with T2D without previous cardiovascular disease [22], whereas reduction of albuminuria (owing to better blood pressure or glycemic control) is associated with significantly less all-cause mortality [23]. All this evidence indicates that patients with DKD require exhaustive control of the associated cardiovascular risk factors and that albuminuria may be considered as a relevant target for therapy.
Mechanisms of SGLT2i Effects on Renal Condition
The characteristic ischemic nephropathy associated with T2D is initially provoked by chronic hyperglycemia. This stimulates SGLT2 expression and activity leading to an increase in proximal tubular glucose and sodium reabsorption and reduced sodium uptake at the juxtaglomerular macula densa, blunting the tubuloglomerular feedback (TGF), and dysregulating vasoactive substances. All these processes enhance preglomerular dilatation, postglomerular constriction, intraglomerular capillary pressure, and finally lead to hyperfiltration [24]. SGLT2i can correct TGF/intraglomerular hemodynamics by preventing sodium reabsorption, which partially explains the renoprotective effect of these agents. Enhanced natriuresis and osmotic diuresis contribute to decrease systolic and diastolic blood pressure by an average of 5 and 2 mmHg, respectively [25], and provoke contraction in plasma volume, reduced sympathetic tone and arterial stiffness, thus improving cardiac perfusion [26, 27]. Moreover, the lower glomerular hyperfiltration translates into the reduction of albuminuria, contributing to minimize the progression of kidney disease [28, 29].
Apart from the activation of the TGF, other mechanisms for the beneficial effects of SGLT2i on kidney function have been proposed (Table 1): induction of ketone body production and an elevation in hematocrit concentration, which can contribute to the beneficial effect of these agents on cardiovascular outcomes [30]; lowering of serum uric acid concentrations by inducing renal uric acid excretion [31]; reduction of inflammatory and fibrotic mediators induced by hyperglycemia in proximal tubular cells [32, 33]; stimulation of autophagy, which is essential for homeostasis of podocytes, tubular cells, mesangial and glomerular endothelial cells [34]; and amelioration of renal hypoxia by decreasing renal oxygen demand and increasing oxygen supply [35]. Several clinical trials are ongoing to further explore the impact and mechanism of action of SGLT2i on renoprotection (Table 2), and eventually will be able to identify the subgroups of patients most likely to benefit from them, even among individuals with CKD but without diabetes.
Benefits of SGLT2i on Renal Function Beyond Their Glycemic Control
The Canagliflozin and Renal Events in Diabetes with Established Nephropathy Clinical Evaluation (CREDENCE) was the first dedicated renal outcomes trial that assessed a primary cardiorenal composite endpoint in people with impaired kidney function [7]. The study population differed from previous CVOTs, as the enrolment was restricted to participants with T2D and CKD with macroalbuminuria (baseline eGFR 30 to < 90 mL/min/1.73 m2; urine albumin-to-creatinine ratio [UACR] 300 to < 5000 mg/g) that were receiving an ACE inhibitor or ARB. A total of 4401 patients were randomized, of whom 2202 received a daily dose of 100 mg of canagliflozin and 2199 received a placebo. After a mean follow-up of 2.62 years, the primary outcome (composite of ESKD, defined as the need of dialysis, kidney transplantation, or a sustained eGFR below 15 mL/min/1.73 m2, doubling of serum creatinine, or renal or cardiovascular death) was 30% lower in the canagliflozin group than in the placebo group, with event rates of 43.2 and 61.2 per 1000 patient-years, respectively [7]. Consistent effects were observed for each of the components of the primary composite endpoint, and for the secondary renal, cardiovascular, and mortality endpoints (Table 3). A subgroup analysis showed that canagliflozin reduced the risk of advancing renal disease to kidney failure in subjects with eGFR above and below 30 mL/min/1.73 m2, without differences in the rates of renal adverse events [36], supporting the use and continuation of SGLT2i until initiation of dialysis or kidney transplantation.
In the CVOT evaluating dapagliflozin (DECLARE-TIMI 58), approximately 13.1% of the participants had CKD (defined as eGFR < 60 mL/min/1.73 m2, UACR > 300 mg/g, or both) at baseline [6]. In the whole patient sample, dapagliflozin treatment was associated with a significantly lower risk (− 47%) of the renal composite of decline in eGFR of ≥ 40% to less than 60 mL/min/1.73 m2, ESKD or renal death, compared with placebo [28]. To further confirm this benefit, the Dapagliflozin and Prevention of Adverse outcomes in CKD (DAPA-CKD) trial investigated the safety and renal outcomes of dapagliflozin in patients with CKD, the majority of them (97%) already receiving RAAS blockers as background renoprotective therapy. Unlike CREDENCE, the DAPA-CKD trial also included people without T2D, to explore whether the benefits of SGLT2i may extend to patients with non-DKD [8]. A total of 4304 patients with CKD were enrolled, 2906 (68%) of them with T2D. Dapagliflozin demonstrated a clear reduction (− 39% lower risk) in primary composite outcome events (sustained decline in the eGFR of ≥ 50%, ESKD, or death from renal or cardiovascular causes), regardless of the presence of diabetes. Additionally, dapagliflozin reduced all three secondary endpoints compared with placebo: decline in eGFR of ≥ 50%, ESKD, or death from renal causes (− 44%), hospitalization for heart failure or cardiovascular death (− 29%), and all-cause mortality (− 31%) (Table 3). There were no significant differences in the primary endpoint between patients with diabetes and without [37], indicating that the renal benefit associated with dapagliflozin is at least similar in patients with non-DKD, such as chronic glomerulonephritides, ischemic or hypertensive CKD, or CKD of other or unknown cause. The baseline glycemic status (normoglycemic, prediabetes, or T2D) of DAPA-CKD trial participants did not modify the effect of dapagliflozin on the primary composite endpoint [38], and recent sub-analyses have shown that dapagliflozin significantly reduced albuminuria [39], slowed long-term eGFR decline [40], and reduced the risk of abrupt declines in kidney function [41]. In addition to this, and in a similar fashion to DAPA-HF, dapagliflozin treatment in DAPA-CKD led to a numerical reduction in the cases of new T2D onset, which reaches statistical significance when pooled with DAPA-HF data (33% relative risk reduction) [42].
The ongoing EMPA-KIDNEY trial of empagliflozin in patients with CKD has a similar design to DAPA-CKD and will further evaluate renal outcomes and CV mortality with SGLT2i in patients with and without T2D (NCT03594110).
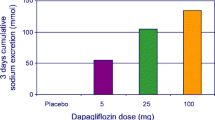
Regarding other renal outcomes trials with dapagliflozin, the DELIGHT study recruited patients with T2D and impaired renal function (UACR ≥ 30 mg/g and eGFR 25–75 mL/min/1.73 m2) to assess the albuminuria-lowering effect of dapagliflozin with and without the dipeptidyl peptidase 4 inhibitor saxagliptin. At week 24, patients treated with dapagliflozin showed a decrease in UACR (− 21%), which was even deeper for the combination of dapagliflozin and saxagliptin (− 38.0%), compared with placebo [43].
Sotagliflozin is a dual SGLT2i that also blocks SGLT1, expressed on small intestine, heart, and brain, apart from the renal proximal tubule [44]. The Sotagliflozin on Cardiovascular and Renal Events in Patients with Type 2 Diabetes and Moderate Renal Impairment Who Are at Cardiovascular Risk (SCORED) trial included patients with T2D and CKD (eGFR 25–60 mL/min/1.73 m2), with or without albuminuria, that were followed for a median of 16 months. Sotagliflozin reduced (− 26%) the composite outcome of cardiovascular death, hospitalization for heart failure, and urgent heart failure, whereas the renal composite outcome was not different in the group treated with sotagliflozin versus placebo [45] (Table 3). However, the trial was prematurely interrupted because of loss of funding, and it was not adequately powered for detecting changes in secondary outcomes, precluding any conclusion regarding a possible renal benefit from the study.
Several meta-analyses have concluded that SGLT2i reduce the risk of renal-related outcomes in patients with T2D, irrespective of the presence or absence of previous renal disease, with a reduction ranging from − 39% to − 33% [46,47,48,49], and one of them calculated the pooled number needed to treat (NNT) to be 20 [49]. Moreover, SGLT2i significantly reduce the annual decline in eGFR slope versus placebo, achieving a mean treatment difference of 1.35 mL/min/1.73 m2/year [50]. “Real world” data from large databases are consistent with the results observed in the clinical trials, demonstrating an important reduction (− 51%) in the composite renal outcome of substantial loss of eGFR and ESKD with SGLT2i [51].
Current Recommendations for Treatment of Renal Complications with SGLT2i
Owing to the robust renoprotective effects demonstrated by SGLT2i in the DAPA-CKD trial, in addition to the previous results of CVOTs, dapagliflozin is the first SGLT2i approved by the European Medicines Agency (EMA) for the treatment of CKD regardless of diabetes status (https://www.ema.europa.eu/en/medicines/human/EPAR/forxiga). This news has also led to a modification of Forxiga SmPC, allowing the therapy to be started in patients with eGFR above 25 mL/min/1.73 m2 for all the approved indications (T2D, heart failure, and CKD). The US prescribing information for canagliflozin, although not in Europe, included a new indication to reduce the risk of ESKD and worsening of kidney function, cardiovascular death, and hospitalization for heart failure in patients with T2D and CKD, allowing the initiation in people with eGFR of ≥ 30 mL/min/1.73 m2 and continuation of treatment in those who reach eGFR < 30 mL/min/1.73 m2 and albuminuria > 300 mg/day until initiation of dialysis or kidney transplantation (https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/204042s036lbl.pdf). These changes have broadened the patients eligible for SGLT2i treatment to ameliorate the progression of CKD.
Additionally, the most relevant professional societies have updated their guidelines and recommendations regarding the use of these agents in people with CKD (Fig. 1). The American Diabetes Association (ADA) guidelines state: “For patients with type 2 diabetes and diabetic kidney disease, use of a SGLT2i in patients with an eGFR ≥ 25 mL/min/1.73 m2 and urinary albumin ≥ 300 mg/g creatinine is recommended to reduce kidney disease progression and cardiovascular events.” The ADA further recommends additional use of SGLT2i in these patients for cardiovascular risk reduction when eGFR and UACR are ≥ 25 mL/min/1.73 m2 or ≥ 300 mg/g, respectively [52].
Pharmacological recommendations to reduce kidney and cardiovascular risks in patients with CKD and T2D. ACEi angiotensin-converting enzyme inhibitor, ADA American Diabetes Association, ARB angiotensin receptor blocker, CV cardiovascular, EASD European Association for the Study of Diabetes, eGFR estimated glomerular filtration rate, ESC European Society of Cardiology, GLP-1 RA glucagon-like peptide 1 receptors agonist, KDIGO Kidney Disease: Improving Global Outcomes, UACR urine albumin-to-creatinine ratio
The European Society of Cardiology, in collaboration with the European Association for the Study of Diabetes, have updated their guidelines to recommend SGLT2i as first-line therapy for the prevention and management of CKD (eGFR 30 to < 90 mL/min/1.73 m2) in patients with T2D and albuminuric kidney disease [53]. The Kidney Disease: Improving Global Outcomes (KDIGO) guidelines recommend the use of metformin in combination with SGLT2i (with GFR ≥ 30 mL/min/1.73 m2) as first-line antihyperglycemic therapy for patients with T2D and CKD. In patients on treatment that have a drop in GFR below 30 mL/min/1.73 m2, the SGLT2i can be continued until initiation of kidney replacement therapy [54]. Finally, a Scientific Statement from the American Heart Association advocated the use of SGLT2i in patients with earlier stages of CKD and postponement of glucagon-like peptide 1 receptors agonists (GLP-1 RAs) in more advanced CKD because there is more experience with these agents in patients with severe CKD [55].
Changing Paradigm: The Cardiorenal and Metabolic Continuum
As stated above, SGLT2i are changing the clinical management of T2D thanks to the evidence supporting their renal and cardiovascular protection, which share common risk factors and pathogenic mechanisms [56]. These agents have demonstrated benefits in different clinical scenarios: patients with T2D with and without established cardiovascular disease [6], patients with T2D with CKD [57], patients with CKD with and without T2D [8], patients with heart failure with and without T2D [58], etc. Indeed, the populations included in the trials of dapagliflozin cover a wide range of diabetic patient profiles, going from those in the earlier stages of the cardiorenal continuum (DECLARE-TIMI 58) to those at more advanced stages (DAPA-CKD and DAPA-HF). Thus, the benefits of SGLT2i are present from the beginning and extend to the advancing disease (Fig. 2).

Adapted from Fontes-Carvalho et al. [56]
Across the cardiorenal continuum and its SGLT2 inhibitors clinical trials
In general, all these trials showed a significant reduction in heart failure hospitalization and a reduction in the composite renal outcome. SGLT2i induce significant natriuresis, enhanced by the combination with loop diuretics, which results in an improvement in blood volume. The diuretic effect facilitates a better management of volume status in patients with heart failure and may contribute to the long-term decrease of heart failure events reported with these agents [59]. Moreover, an improved kidney function itself may indirectly benefit cardiac function through multifaceted interorgan cross talk, breaking the cardiorenal vicious circle [56]. Some authors have defined the cardiorenal disease in patients with T2D as the development of heart failure and CKD, and suggested a novel outcome, major adverse renal and cardiac events (MARCE), to be evaluated in future clinical trials [60, 61].
Patients with T2D suffer multiple comorbid conditions and usually receive several treatments such as antihypertensive agents, diuretics, insulin, or other glucose-lowering medications. The number of therapy choices to be combined is higher early in the course of diabetes, before the development of serious comorbidities, including renal function impairment. Although the glucose-lowering effect of these drugs decreases as glomerular filtration worsens, SGLT2i can be prescribed for patients with renal impairment for organ protection. Moreover, the likelihood of response to treatment is greater with shorter T2D duration [62].
Conclusions
The dedicated kidney outcomes trials of SGLT2i (such as DAPA-CKD and CREDECE) have confirmed the renoprotective benefit of these drugs across different glomerular filtration rates and albuminuria values. SGLT2i can correct TGF/intraglomerular hemodynamics by preventing sodium reabsorption, whereas other mechanisms such as ketone body production, lowering of serum uric acid concentrations, and increasing oxygen supply can contribute to their beneficial effects on cardiovascular outcomes. Accordingly, the most relevant professional societies have updated their guidelines and recommendations regarding the use of these agents in people with CKD. Diabetes is normally addressed by multiple specialists including endocrinologists, cardiologists, and nephrologists, as well as primary care providers. The multidisciplinary team should select the therapeutic strategy on the basis of the target organ of protection and patients’ comorbidities and profile, going beyond glycemic control and ensuring that patients are able to benefit from the metabolic, cardiovascular, and kidney protection associated with SGLT2i.
References
Vallon V, Platt KA, Cunard R, et al. SGLT2 mediates glucose reabsorption in the early proximal tubule. J Am Soc Nephrol. 2011;22:104–12.
Kramer CK, Zinman B. Sodium–glucose cotransporter-2 (SGLT-2) inhibitors and the treatment of type 2 diabetes. Annu Rev Med. 2019;70:323–34.
van Baar MJB, van Ruiten CC, Muskiet MHA, van Bloemendaal L, IJzerman RG, van Raalte DH. SGLT2 inhibitors in combination therapy: from mechanisms to clinical considerations in type 2 diabetes management. Diabetes Care. 2018;41:1543–56.
Zinman B, Wanner C, Lachin JM, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Neal B, Perkovic V, Mahaffey KW, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–57.
Wiviott SD, Raz I, Bonaca MP, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380:347–57.
Perkovic V, Jardine MJ, Neal B, et al. Canagliflozin and renal outcomes in type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–306.
Heerspink HJL, Stefánsson BV, Correa-Rotter R, et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–46.
Xie Y, Bowe B, Mokdad AH, et al. Analysis of the global burden of disease study highlights the global, regional, and national trends of chronic kidney disease epidemiology from 1990 to 2016. Kidney Int. 2018;94:567–81.
Saran R, Robinson B, Abbott KC, et al. Annual data report: epidemiology of kidney disease in the United States. Am J Kidney Dis. 2019;2020:A6-7.
Alicic RZ, Rooney MT, Tuttle KR. Diabetic kidney disease: challenges, progress, and possibilities. Clin J Am Soc Nephrol. 2017;12:2032–45.
Bash LD, Selvin E, Steffes M, Coresh J, Astor BC. Poor glycemic control in diabetes and the risk of incident chronic kidney disease even in the absence of albuminuria and retinopathy: Atherosclerosis Risk in Communities (ARIC) Study. Arch Intern Med. 2008;168:2440–7.
Buyadaa O, Salim A, Morton JI, Magliano DJ, Shaw JE. Rate of decline in kidney function and known age-of-onset or duration of type 2 diabetes. Sci Rep. 2021;11:14705.
Zoppini G, Targher G, Chonchol M, et al. Predictors of estimated GFR decline in patients with type 2 diabetes and preserved kidney function. Clin J Am Soc Nephrol. 2012;7:401–8.
Pearce I, Simó R, Lövestam-Adrian M, Wong DT, Evans M. Association between diabetic eye disease and other complications of diabetes: implications for care. A systematic review. Diabetes Obes Metab. 2019;21:467–78.
Gansevoort RT, Correa-Rotter R, Hemmelgarn BR, et al. Chronic kidney disease and cardiovascular risk: epidemiology, mechanisms, and prevention. Lancet. 2013;382:339–52.
Ting R-D, Keech AC, Drury PL, et al. Benefits and safety of long-term fenofibrate therapy in people with type 2 diabetes and renal impairment: the FIELD Study. Diabetes Care. 2012;35:218–25.
Li Q, Wen F, Wang Y, et al. Diabetic kidney disease benefits from intensive low-protein diet: updated systematic review and meta-analysis. Diabetes Ther. 2021;12:21–36.
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO. Clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2020;2020:S1–115.
GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2020;395:709–33.
Afkarian M, Sachs MC, Kestenbaum B, et al. Kidney disease and increased mortality risk in type 2 diabetes. J Am Soc Nephrol. 2013;24:302–8.
Fangel MV, Nielsen PB, Kristensen JK, et al. Albuminuria and risk of cardiovascular events and mortality in a general population of patients with type 2 diabetes without cardiovascular disease: a Danish cohort study. Am J Med. 2020;133:e269–79.
Anyanwagu U, Donnelly R, Idris I. Albuminuria regression and all-cause mortality among insulin-treated patients with type 2 diabetes: analysis of a large UK primary care cohort. Am J Nephrol. 2019;49:146–55.
De Pascalis A, Cianciolo G, Capelli I, Brunori G, La Manna G. SGLT2 inhibitors, sodium and off-target effects: an overview. J Nephrol. 2021;34:673–80.
Baker WL, Buckley LF, Kelly MS, et al. Effects of sodium–glucose cotransporter 2 inhibitors on 24-hour ambulatory blood pressure: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6(5):e005686.
Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61:2108–17.
Heerspink HJL, Kosiborod M, Inzucchi SE, Cherney DZI. Renoprotective effects of sodium–glucose cotransporter-2 inhibitors. Kidney Int. 2018;94:26–39.
Mosenzon O, Wiviott SD, Cahn A, et al. Effects of dapagliflozin on development and progression of kidney disease in patients with type 2 diabetes: an analysis from the DECLARE-TIMI 58 randomised trial. Lancet Diabetes Endocrinol. 2019;7:606–17.
Mosenzon O, Wiviott SD, Heerspink HJL, et al. The effect of dapagliflozin on albuminuria in DECLARE-TIMI 58. Diabetes Care. 2021;44:1805–15.
Ferrannini E, Mark M, Mayoux E. CV protection in the EMPA-REG OUTCOME trial: a “thrifty substrate” hypothesis. Diabetes Care. 2016;39:1108–14.
Zhao Y, Xu L, Tian D, et al. Effects of sodium–glucose co-transporter 2 (SGLT2) inhibitors on serum uric acid level: a meta-analysis of randomized controlled trials. Diabetes Obes Metab. 2018;20:458–62.
Heerspink HJL, Perco P, Mulder S, et al. Canagliflozin reduces inflammation and fibrosis biomarkers: a potential mechanism of action for beneficial effects of SGLT2 inhibitors in diabetic kidney disease. Diabetologia. 2019;62:1154–66.
Pirklbauer M, Sallaberger S, Staudinger P, et al. Empagliflozin inhibits IL-1β-mediated inflammatory response in human proximal tubular cells. Int J Mol Sci. 2021;22(10):5089.
Xu J, Kitada M, Ogura Y, Liu H, Koya D. Dapagliflozin restores impaired autophagy and suppresses inflammation in high glucose-treated HK-2 cells. Cells. 2021;10(6):1457.
Hesp AC, Schaub JA, Prasad PV, et al. The role of renal hypoxia in the pathogenesis of diabetic kidney disease: a promising target for newer renoprotective agents including SGLT2 inhibitors? Kidney Int. 2020;98:579–89.
Bakris G, Oshima M, Mahaffey KW, et al. Effects of canagliflozin in patients with baseline eGFR <30 ml/min per 1.73 m(2): subgroup analysis of the randomized CREDENCE trial. Clin J Am Soc Nephrol. 2020;15:1705–14.
Wheeler DC, Stefánsson BV, Jongs N, et al. Effects of dapagliflozin on major adverse kidney and cardiovascular events in patients with diabetic and non-diabetic chronic kidney disease: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9:22–31.
Persson F, Rossing P, Vart P, et al. Efficacy and safety of dapagliflozin by baseline glycemic status: a prespecified analysis from the DAPA-CKD trial. Diabetes Care. 2021;44:1894–7.
Jongs N, Greene T, Chertow GM, et al. Effect of dapagliflozin on urinary albumin excretion in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9:755–66.
Heerspink HL, Jongs N, Chertow GM, et al. Effect of dapagliflozin on the rate of decline in kidney function in patients with chronic kidney disease with and without type 2 diabetes: a prespecified analysis from the DAPA-CKD trial. Lancet Diabetes Endocrinol. 2021;9:743–54.
Heerspink HJL, Cherney D, Postmus D, et al. A pre-specified analysis of the dapagliflozin and prevention of adverse outcomes in chronic kidney disease (DAPA-CKD) randomized controlled trial on the incidence of abrupt declines in kidney function. Kidney Int. 2022;101:174–84.
Rossing P, Inzucchi SE, Vart P, et al. Dapagliflozin and new-onset type 2 diabetes in patients with chronic kidney disease or heart failure: pooled analysis of the DAPA-CKD and DAPA-HF trials. Lancet Diabetes Endocrinol. 2022;10:24–34.
Pollock C, Stefánsson B, Reyner D, et al. Albuminuria-lowering effect of dapagliflozin alone and in combination with saxagliptin and effect of dapagliflozin and saxagliptin on glycaemic control in patients with type 2 diabetes and chronic kidney disease (DELIGHT): a randomised, double-blind, plac. Lancet Diabetes Endocrinol. 2019;7:429–41.
Sands AT, Zambrowicz BP, Rosenstock J, et al. Sotagliflozin, a dual SGLT1 and SGLT2 inhibitor, as adjunct therapy to insulin in type 1 diabetes. Diabetes Care. 2015;38:1181–8.
Bhatt DL, Szarek M, Pitt B, et al. Sotagliflozin in patients with diabetes and chronic kidney disease. N Engl J Med. 2021;384:129–39.
Neuen BL, Young T, Heerspink HJL, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2019;7:845–54.
McGuire DK, Shih WJ, Cosentino F, et al. Association of SGLT2 inhibitors with cardiovascular and kidney outcomes in patients with type 2 diabetes: a meta-analysis. JAMA Cardiol. 2021;6:148–58.
Qiu M, Ding L, Zhou H. Effects of SGLT2 inhibitors on cardiovascular and renal outcomes in type 2 diabetes: a meta-analysis with trial sequential analysis. Medicine. 2021;100: e25121.
Martínez-Vizcaíno V, Díez-Fernández A, Álvarez-Bueno C, Martínez-Alfonso J, Cavero-Redondo I. Safety and efficacy of SGLT2 inhibitors: a multiple-treatment meta-analysis of clinical decision indicators. J Clin Med. 2021;10(12):2713.
Toyama T, Neuen BL, Jun M, et al. Effect of SGLT2 inhibitors on cardiovascular, renal and safety outcomes in patients with type 2 diabetes mellitus and chronic kidney disease: A systematic review and meta-analysis. Diabetes Obes Metab. 2019;21:1237–50.
Heerspink HJL, Karasik A, Thuresson M, et al. Kidney outcomes associated with use of SGLT2 inhibitors in real-world clinical practice (CVD-REAL 3): a multinational observational cohort study. Lancet Diabetes Endocrinol. 2020;8:27–35.
American Diabetes Association Professional Practice Committee. 11. Chronic kidney disease and risk management: standards of medical care in diabetes—2022. Diabetes Care. 2022;45:S175–84.
Cosentino F, Grant PJ, Aboyans V, et al. 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J Engl. 2020;41:255–323.
de Boer IH, Caramori ML, Chan JCN, et al. Executive summary of the 2020 KDIGO Diabetes Management in CKD Guideline: evidence-based advances in monitoring and treatment. Kidney Int. 2020:98:839–48.
Rangaswami J, Bhalla V, de Boer IH, et al. Cardiorenal protection with the newer antidiabetic agents in patients with diabetes and chronic kidney disease: a scientific statement from the American Heart Association. Circulation. 2020;142:e265–86.
Fontes-Carvalho R, Santos-Ferreira D, Raz I, Marx N, Ruschitzka F, Cosentino F. Protective effects of SGLT-2 inhibitors across the cardiorenal continuum: two faces of the same coin. Eur J Prev Cardiol. 2021; zwab034. https://doi.org/10.1093/eurjpc/zwab034
Perkovic V, de Zeeuw D, Mahaffey KW, et al. Canagliflozin and renal outcomes in type 2 diabetes: results from the CANVAS Program randomised clinical trials. Lancet Diabetes Endocrinol. 2018;6:691–704.
McMurray JJV, Solomon SD, Inzucchi SE, et al. Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med. 2019;381:1995–2008.
Vaduganathan M, Claggett BL, Jhund PS, et al. Estimating lifetime benefits of comprehensive disease-modifying pharmacological therapies in patients with heart failure with reduced ejection fraction: a comparative analysis of three randomised controlled trials. Lancet. 2020;396:121–8.
Birkeland KI, Bodegard J, Eriksson JW, et al. Heart failure and chronic kidney disease manifestation and mortality risk associations in type 2 diabetes: a large multinational cohort study. Diabetes Obes Metab. 2020;22:1607–18.
Ronco C, Ronco F, McCullough PA. A call to action to develop integrated curricula in cardiorenal medicine. Blood Purif. 2017;44:251–9.
Han E, Kim A, Lee SJ, et al. Characteristics of dapagliflozin responders: a longitudinal, prospective, nationwide dapagliflozin surveillance study in Korea. Diabetes Ther. 2018;9:1689–701.
Acknowledgements
Funding
AstraZeneca funded the writing assistance provided by Springer Healthcare Ibérica SL and the journal’s Rapid Service Fee. This supplement has been sponsored by AstraZeneca.
Editorial Assistance
Editorial assistance in the preparation of this article was provided by Anabel Herrero, PhD, on behalf Springer Healthcare Iberica and was funded by AstraZeneca.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
All authors equally participated in the development of the manuscript, had full editorial control, reviewed and edited various drafts, and provided their final approval of all content and submission for publication.
Disclosures
Olga González-Albarrán has no conflict of interest in close relationship with this paper. Cristóbal Morales has participated in clinical trials for Novo Nordisk, Sanofi, AstraZeneca, Pfizer, Lilly, Merck, Lexicon, FPS, Hanmi, Janssen, Boehringer, Takeda, Roche, and Theracos; has been advisory board member for Novo Nordisk, Lilly, MSD, Boehringer, AstraZeneca, Sanofi and Abbott; and has been speaker for Sanofi, Novo Nordisk, AstraZeneca, Roche, Lilly, Boehringher, MSD, Ferrer, Janssen, and Abbot. Manuel Pérez-Maraver has no conflict of interest regarding this study. José Juan Aparicio-Sánchez is an employee of the Medical Affairs Department of AstraZeneca Farmacéutica Spain. Rafael Simó has no conflict of interest in close relationship with this paper.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Open Access
This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/
Author information
Authors and Affiliations
Corresponding author
Additional information
All authors have equally participated in the development of the manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
González-Albarrán, O., Morales, C., Pérez-Maraver, M. et al. Review of SGLT2i for the Treatment of Renal Complications: Experience in Patients with and Without T2D. Diabetes Ther 13 (Suppl 1), 35–49 (2022). https://doi.org/10.1007/s13300-022-01276-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01276-2