Abstract
Introduction
Frail older people with diabetes often present with or develop walking impairments, in part due to lower-limb sensory-motor neuropathy. Several studies suggest a possible improvement of balance control using somatosensory stimulation. We undertook a novel randomized control trial, the aim of which was to observe whether use of this device for 1 month improves walking speed as measured in the 10-m fast walking speed test standardized to body size at month 1 (M1) (FWS). Secondary outcomes were the differences between intervention (VS) and control (C) in the 10-m normal walking speed test, step length, short physical performance battery, timed up and go test, and posturographic measures.
Methods
Subjects were aged ≥ 70 years and had had type 2 diabetes for at least 2 years. The intervention (VS) at home consisted of 22-min daily vibrating sequences with noise intensity set at 90% of the tactile threshold for each foot. The same device was used in group C but noise was set to 0. Compliance was retrieved from the device.
Results
Among 56 subjects, 27 were in the VS group and 29 in the C group; 35 subjects were frail, 15 were prefrail ,and 6 were non-frail. Bilateral neuropathy was present in 17 subjects. More than half of sessions were done in 36 subjects with no discernible difference according to intervention. At M1 there were no discernible differences in FWS between the groups [VS: 0.96 (0.53) cm s−1 cm−1, C: 0.94 (0.47) cm s−1 cm−1]. There were also no discernible differences in other outcomes, irrespective of the presence of bilateral neuropathy.
Conclusion
In a cohort of frail, prefrail, or non-frail older subjects with diabetes, a 1-month intervention using a vibrating insole device did not alter measures of walking speed and related measures. Larger studies with longer term and different stimulation protocols are required to test this hypothesis more fully.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Improvement of gait may be obtained in older people with diabetes with vibrating insole use; however, the effects have to be tested in a blind randomized control trial (RCT) |
A 1-month intervention using a vibrating insole device did not alter measures of walking speed and related measures |
Different stimulation protocols and combination with other interventions are required to test this hypothesis more fully |
Introduction
Diabetes is a disabling disease due to specific complications and associated disorders such as obesity, arthritis, depression, and social factors [1]. Older people with diabetes experience weakness and have a greater rate of strength decline than older people without diabetes [2, 3]. Specifically, the loss of somatosensory information from the feet’s cutaneous mechanoreceptors in older and/or diabetic patients leads to postural instability [4,5,6,7,8] and increased risk of falling and dependency. It has been suggested that a somatosensory stimulation may improve balance control in these patients [8, 9].
Priplata et al. [9] demonstrated that the application of noise to the soles of feet resulted in a decrease in all of the sway variables in elderly participants, especially in the medio-lateral axis, which is in accordance with the hip strategy, including a loading-unloading behaviour, usually observed in older people. Reduced sway area was also demonstrated with stochastic vibrations in subjects with diabetic neuropathy or post-stroke hemiparesis [8] and in those with exercise-induced fatigue [10]. These findings are potentially important, insofar as impaired sensations lead not only to serious secondary medical complications, but also to disability in performing everyday tasks or walking safely and efficiently and to functional dependency. Sub-sensory threshold noise was able to reduce center of pressure (COP) area in healthy people with diminished sensory ability after ice treatment [11]. In older people with diabetes, the application of sub-sensory threshold noise via vibrating insoles (SENSOLE, part I) led to improvement in posturographic measures and in gait performances (SPPB, short physical performance battery [12] and TUG, timed up and go test [13]) [14, 15]. No adverse event was reported. However, all these studies addressed only the short-time effect of the intervention; measures were performed during or immediately after the vibration session.
SENSOLE part II aims to investigate the effects of an innovative HEXABIO R&D insole device, applied each day at home for 1 month, on gait and posture of older diabetic patients through everyday balance and quality of daily living. The main objective of the study is thus to assess the potential changes in walking speed (maximal speed condition) among participants in the intervention and control arms, as measured in the 10-m fast walking speed test at month 1.
Methods
Participants
Patients with diabetes were recruited during a 2-year period in the University Hospital Centre of Bordeaux. They were eligible if aged ≥ 70 years with a diagnosis of T2D for at least 2 years. Exclusion criteria included basic daily living Barthel index < 60/100 [16], inability to carry out the SPPB test, MMS (Mini-Mental State GRECO) [17] < 20/30 (or < 18/30 with a caregiver to use the vibrating platform), ulcerations and/or infections on the plantar surface of the feet, pacemaker equipment, and participation in another trial. They were recruited during the inclusion period of the MID-Frail study [18] and were asked to participate if they were unwilling to participate in the MID-frail study or were not eligible for it. SENSOLE II study is a substudy of the European project MID-Frail European project (NCT01654341).
Study Design
SENSOLE, part II, is a randomized controlled trial. The study was approved by the Comité de Protection des Personnes (CPP) “SUD-Ouest et Outre Mer III”. After obtaining written informed consent from the participant and having properly checked all eligibility criteria, the participants were individually randomised to receive the intervention (intervention group, IG, platform with vibrations) or not (control group, CG, platform without vibration). The size of the two arms was balanced with a 1:1 ratio. The randomisation was stratified according to the participant’s age (≤ 80 years, > 80 years) and the walking speed (maximal speed condition) on the 10-m walking test normalised according to height (1.19 and 1.11 cm s−1 cm−1 or lower versus over for men and women, respectively) [19]. The full protocol is available as a supplementary file.
Four visits were planned. M0 included baseline characteristic assessment, vibration perception threshold, and distribution of individual vibrating sole platforms, either active or placebo, and instructions for use. The M0.5 visit was done 15 days afterwards to record the outcomes and the compliance and to update the vibrating perception threshold. The intervention terminated after 1 month corresponding to the M1 visit during which compliance and safety data were recorded and outcomes were assessed. Six months after the start of the study (M6) safety data and outcomes were once more recorded. Randomization groups were blind for the assessors.
Intervention
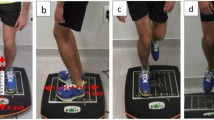
Experimental insoles (16 mm thick) were specially designed by Hexabio R&D Department (French patent nos. FR 11 03355 [2011] and FR 16 01587 [2016]) and were previously fully described [14]. The six vibrating motors are settled in each insole under both anterior and posterior parts of the plantar foot surface, i.e. near the first and fifth metatarsophalangeal joints, and under the heel. The innovative HEXABIO R&D insole concept relies on a membrane that enables propagation of the vibration on the whole insole (see details under European patent no. EP 17817867 [2017]). The input for the three vibrating motors in a single insole is identical. The random noise signal bandwidth varies up to 200 Hz. Each insole provides a vibration, whose strength is set independently with a programme for each foot.
During M0 visit in both groups, the perception thresholds for the noise signal for each foot were determined independently and according to the patient's perceived vibration. The amplitude of the noise frequency was gradually incremented every 10 s from level 1 (0 Hz) to level 25 (200 Hz), with a step of 8 Hz. The patient was instructed to inform the investigator as soon as the vibration was perceptible. This procedure is repeated at M0.5 and M1 visits.
Subjects for both groups are provided a vibrating insole platform for 1 month. The subjects randomized to the control group had a non-vibrating insole platform, i.e. the six vibrators were not present but all the following equipment was kept identical: electronic card, battery, membrane of the soles, remote control, indicator lights, software of functioning and recording of the sequences of use. They were not aware of the group to which they were assigned. The intervention at home consisted of a daily 22-min vibrating sequence in sitting position with noise intensity set at 90% of the vibration threshold for each foot. In control group noise was set at 0. Subjects did not receive specific instructions about exercising or physiotherapy.
Baseline Assessment
Barthel index described the dependence for basic daily living activities with scores ranging from 0 to 100, 100 corresponding to full independence [16]. A history of falls during the last 6 months was searched. BMI (body mass index, kg/m2) was determined. The presence of pressure neuropathy was tested with a 10-g Semmes-Weinstein monofilament and vibration perception with a 128-Hz tuning fork. Lack of perception defined respectively pressure and vibratory neuropathy. At each foot the vibration perception threshold to therapeutic insoles was also considered, with a 0–200-Hz range of vibration delivery. We define “bilateral neuropathy” as lack of protective sensation (pressure perception) in both feet.
Frailty status (frail, prefrail, robust) was determined according to Fried criteria [20]. Gait and posture assessment completes the baseline measures (see outcomes).
Outcomes
The main outcome of this study was the 10-m walking time at fast speed in seconds (s). The 10-m walking test requires the participant to walk 10 m (32.8 ft) without physical assistance. Assistive devices can be used but should be kept consistent and documented from test to test. Each patient was asked to walk at different speeds: comfortable speed (normal speed) and maximal speed (fast speed).
The time taken to complete the intermediate 6 m (19.7 ft) was measured—this allowed for acceleration and deceleration. Three trials per speed condition were done and the average time from the three trials calculated. Accordingly fast speed and normal speed were calculated and expressed in cm s−1 cm − 1 body height. We also assessed physical performance with SPPB and TUG. SPPB is composed of three parts: balance, 4-m walking, and chair rise tests; each maximal subscore is 4. Overall the maximal SPPB score is 12; lower scores indicate lower performances [12]. Length of step was calculated from the SPPB 4-m test. The TUG test measured the time in seconds taken to stand up from a chair, walk 3 m, and walk back to sit in the chair. Fall occurrence is recorded at each visit.
Posturographic data were acquired using a double force platform (Feetest 6, Techno Concept, Mane, France). The acquisition was performed and the global centre of pressure (CoP)-related parameters computed by using Posturewin3 software (Techno Concept, Mane, France). The calibration of both force plates was checked before the beginning of the study. Anterio-posterior and medio-lateral displacements were reported in mm, CoP sway area in mm2, CoP velocity in mm s−1, and CoP variance in mm.
Compliance and Safety
The numbers of vibration sessions actually performed with verum or placebo insoles are retrieved from the platforms at M0.5 and M1 visits; good compliance is defined as ≥ 22 sessions during the intervention month. Adverse events were recorded at each visit. The study was approved by the Comité de Protection des Personnes (CPP) “SUD-Ouest et Outre Mer III”. All participants have given written informed consent; authors were required to include a statement of ethics. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Analyses
Summary statistics of patient baseline characteristics and descriptive tables of the subsequent outcome data were produced. Variables with normal distribution were shown with mean and standard deviation (SD); ordinal variables and those with non-normal distribution were presented with median and interquartile range (IQR).
Assuming a SD of fast 10-m test walking speed of 0.3 [21] and assuming a recruitment of 60 patients and a subsequent 20% attrition, we were able to detect an effect size of 0.51 with 80% power. This translates to a difference of 0.15 m s−1.
Comparisons of 10-m fast walking speed between control and intervention arms were made using analysis of covariance (ANCOVA), controlling for baseline measurements of outcome variables, balancing variables as well as other important covariates (e.g. age and gender). The primary comparison was between baseline and 1 month. In this single-centre study a fixed approach was undertaken. No sensibility analyses were planned and analyses include complete cases. Results were summarised using point estimates, 95% confidence intervals, and p values. The analysis was further adjusted for the presence or absence of bilateral neuropathy. The other outcomes were analysed using appropriated models, ANCOVA for variables with normal distribution, and logistic regression for ordinal variables and non-normally distributed variables. General linear models for repeated measures adjusted for gender, age, and baseline performance were planned for comparisons of gait and posture changes between the two groups during the 6-month follow-up. Adverse events with potential accountability to the intervention were described. SPSS v20 was used to store the data and to produce descriptive tables.
Results
Subjects
Sixty-six subjects were screened among patients attending the diabetes clinic or the geriatric centre or living in one nursing home. The SENSOLE 2 informed consent was signed by 65 subjects. Sixty-three subjects were assessed and 60 were randomised. Two others were excluded because of low Barthel index or low MMS and one death occurred after the signature and before randomization. The CONSORT flow diagram is presented in Fig. 1.
Seven of them were living in a nursing home (3 in intervention group and 4 in placebo group) and six were included during their stay in rehabilitation centre (3 in each group). Thirty-five were frail, 15 prefrail, and 6 were robust (Table 1). Bilateral neuropathy was present in 17 patients and the vibration perception threshold was at the maximum level for both feet in 14 subjects from the intervention group and in 12 subjects from the control group (Fig. 2).
After 1-month intervention the fast speed 10-m walking time was similar in both groups [ANCOVA estimate 1.38 (95% CI − 0.71 to 3.79), p = 0.174, Table 2, Fig. 2]. Adjustment for the diagnosis of bilateral neuropathy did not change the result [1.34 (95% CI − 0.93 to 3.61)]. The effects of intervention on other gait and posture outcomes were neutral (Table 2). As there was no observable effect on outcomes after 1 month, the effects at 6 months were not analysed.
Compliance with the intervention was good with 34/14 who performed > 22 vibration sessions during the 1-month intervention with no observed difference between the two groups (supplementary Table 1). During the 6-month follow-up one person in the control group died (supplementary Table 2). None of the participants was newly admitted to a nursing home. Hospitalisation occurred in three subjects, one in the 1st month in intervention group and one in each group during the remaining follow-up. Falls occurred during the follow-up with no difference in rate between the two groups. No adverse events were attributed to the intervention.
Discussion
In this double-blind RCT on the effects of repeated plantar vibrations on gait and related parameters in older subjects with diabetes, no beneficial effects were observed following a 1-month phase of intervention. With the same device we have previously shown an improvement in the first half hour following a vibration session compared with the performance before vibrations.
The vibrations programme (duration and frequency) was established a priori based on this short-term effect and on a pragmatic basis: feasibility and acceptability.
Vibration sequence programme was established on a pragmatic basis (what is possible). An open RCT with a frequency and duration of vibrating sessions close to the present study did not demonstrate a difference between the intervention and control groups based on the chair rise test [22]. In our study, we only included subjects with diabetes. The gait impairment observed with diabetes is multifactorial [1]. Plantar vibrations are not expected to correct sarcopenia for instance. Acting on only one of the causes of gait disorders is likely to be ineffective. Other programmes should be assessed, possibly combined with balance rehabilitation during the period of efficacy of the device.
Most of the participants had impaired vibration sensibility. The vibration perception threshold was not measurable in about half of them because it was above the higher vibration noise of the device (200 Hz). However, we did not see an effect of an impaired plantar sensibility on outcomes.
The main study limitation is the choice of a pragmatic programme. Second, several subjects were lost to follow-up, particularly at the 6-month visit. The heterogeneity of the health status of the study population may have limited the power of the study to detect an effect. The very high rate of impaired vibration sensibility also makes the interpretation of the results difficult. However, the strengths are important: this is a double-blind study owing to the placebo platforms; the groups are well balanced for most of the characteristics and measures; a large proportion of frail or prefrail patients was included; the acceptability of the intervention was reflected by the overall good compliance.
Conclusion
In frail, prefrail, or non-frail older subjects with diabetes, changes in measures of walking speed and related assessments were not observed with this vibrating insole 1-month intervention. Further studies must explore other stimulation programmes, possibly combined with physiotherapy sessions addressing the other components of gait.
References
Bourdel-Marchasson I, Helmer C, Fagot-Campagna A, Dehail P, Joseph PA. Disability and quality of life in elderly people with diabetes. Diabetes Metab. 2007;33(Suppl 1):S66-74.
Park SW, Goodpaster BH, Strotmeyer ES, et al. Decreased muscle strength and quality in older adults with type 2 diabetes: the health, aging, and body composition study. Diabetes. 2006;55(6):1813–8.
Rantanen T, Masaki K, Foley D, Izmirlian G, White L, Guralnik JM. Grip strength changes over 27 year in Japanese-American men. J Appl Physiol. 1998;85:2047–53.
Dickstein R, Shupert CL, Horak FB. Fingertip touch improves postural stability in patients with peripheral neuropathy. Gait Posture. 2001;14(3):238–47.
Hijmans JM, Geertzen JH, Zijlstra W, Hof AL, Postema K. Effects of vibrating insoles on standing balance in diabetic neuropathy. J Rehabilit Res Dev. 2008;45(9):1441–9.
Horak FB, Dickstein R, Peterka RJ. Diabetic neuropathy and surface sway-referencing disrupt somatosensory information for postural stability in stance. Somatosens Mot Res. 2002;19(4):316–26.
Liu W, Lipsitz LA, Montero-Odasso M, Bean J, Kerrigan DC, Collins JJ. Noise-enhanced vibrotactile sensitivity in older adults, patients with stroke, and patients with diabetic neuropathy. Arch Phys Med Rehabil. 2002;83(2):171–6.
Priplata AA, Patritti BL, Niemi JB, et al. Noise-enhanced balance control in patients with diabetes and patients with stroke. Ann Neurol. 2006;59(1):4–12.
Priplata AA, Niemi JB, Harry JD, Lipsitz LA, Collins JJ. Vibrating insoles and balance control in elderly people. Lancet. 2003;362(9390):1123–4.
Moon J, Pathak P, Kim S, et al. Shoes with active insoles mitigate declines in balance after fatigue. Sci Rep. 2020;10(1):1951.
Chen WM, Li JW, Geng X, Wang C, Chen L, Ma X. The potential influence of stochastic resonance vibrations on neuromuscular strategies and center of pressure sway during single-leg stance. Clin Biomech (Bristol, Avon). 2020;77:105069.
Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49(2):M85-94.
Podsiadlo D, Richardson S. The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8.
Regueme SC, Cowtan C, Sedgelmaci MY, et al. A Therapeutic insole device for postural stability in older people with type 2 diabetes. A feasibility study (SENSOLE Part I). Front Med. 2019;6:127.
Aboutorabi A, Arazpour M, Bahramizadeh M, Farahmand F, Fadayevatan R. Effect of vibration on postural control and gait of elderly subjects: a systematic review. Aging Clin Exp Res. 2018;30(7):713–26.
Mahoney FI, Barthel DW. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–5.
Derouesne C, Poitreneau J, Hugonot L, Kalafat M, Dubois B, Laurent B. Mini-Mental State Examination:a useful method for the evaluation of the cognitive status of patients by the clinician. Consensual French version. Presse Med. 1999;28(21):1141–8.
Rodríguez-Mañas L, Bayer AJ, Kelly M, et al. An evaluation of the effectiveness of a multi-modal intervention in frail and pre-frail older people with type 2 diabetes–the MID-Frail study: study protocol for a randomised controlled trial. Trials. 2014;15:34.
Bohannon RW. Comfortable and maximum walking speed of adults aged 20–79 years: reference values and determinants. Age Ageing. 1997;26(1):15–9.
Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56(3):M146–56.
Dechamps A, Diolez P, Thiaudière E, et al. Effects of exercise programs to prevent decline in health-related quality of life in highly deconditioned institutionalized elderly persons: a randomized controlled trial. Arch Intern Med. 2010;170(2):162–9.
Rogan S, Hilfiker R, Schmid S, Radlinger L. Stochastic resonance whole-body vibration training for chair rising performance on untrained elderly: a pilot study. Arch Gerontol Geriatr. 2012;55(2):468–73.
Acknowledgements
Funding
Sponsorship was received for this study from EU 7th Framework Programme (contract no. 278803). CHU of Bordeaux paid the journal’s Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Isabelle Bourdel-Marchasson, Sophie Regueme, and Joël Poustis were responsible for the conceptualization of the study. Isabelle Bourdel-Marchasson, Sophie Regueme, Mark Kelson, and Alan Sinclair were responsible for the methodology of the study. Formal analysis and investigation were conducted by Isabelle Bourdel-Marchasson, Sophie Regueme, Olga Laosa, and Mark Kelson. The original draft preparation was conducted by Isabelle Bourdel-Marchasson, Joël Poustis, and Pierre Barralon. Isabelle Bourdel-Marchasson, Sophie Regueme, Mark Kelson, Leocadio Rodriguez-Manas, and Alan Sinclair were responsible for reviewing and editing the publication. Isabelle Bourdel-Marchasson, Leocadio Rodriguez-Manas, and Alan Sinclair were responsible for acquiring funding. Alan Sinclair supervised the study. All authors read and approved the final manuscript.
Disclosures
Isabelle Bourdel-Marchasson, Sophie Regueme, Olga Laosa, Joël Poustis, Leocadio Rodriguez-Manas, and Alan Sinclair have received research grants from the EU 7th Framework Programme. Joël Poustis is the owner of the vibrating insoles device patents. Pierre Barralon has nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Comité de Protection des Personnes (CPP) “SUD-Ouest et Outre Mer III”. All participants have given written informed consent. The study was performed in accordance with the Helsinki Declaration of 1964 and its later amendments.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available because of the French regulation rules for personal electronic data (CNIL).
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bourdel-Marchasson, I., Regueme, S.C., Kelson, M. et al. A Therapeutic Vibrating Insole Device for Postural Instability in Older People with Type 2 Diabetes: A Randomized Control Study. Diabetes Ther 13, 995–1006 (2022). https://doi.org/10.1007/s13300-022-01246-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01246-8