Abstract
Introduction
In general surgery, it has been shown that poor peri-operative diabetes control, as measured by glycated haemoglobin (HbA1c), is associated with adverse post-operative outcomes. National data for the UK suggest that the post-operative complication rate for cataract surgery is 2.8%. It is unknown whether people with diabetes who undergo cataract surgery are also at increased risk.
Methods
This single-centre retrospective study looked at the association of peri-operative HbA1c and estimated glomerular filtration rate (eGFR) with the risk of post-operative complications in people undergoing phacoemulsification and intraocular lens implantation under local anaesthesia during 2016.
Results
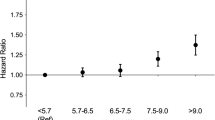
4401 individuals had cataract surgery. Of these, 34.6% (1525) had diabetes. Of those with diabetes, 114 (7.5%) developed a post-operative ophthalmological complication (as defined by the Royal College of Ophthalmologists) necessitating at least one eye clinic appointment. Mean HbA1c did not differ between those who did and those who did not develop complications (52 vs 50 mmol/mol, p = 0.12). After adjustment, HbA1c was not a significant risk (OR 1.00; 95% CI: 0.99–1.05; p = 0.85). However, eGFR had a small but statistically significant effect on outcome (OR 0.99; 95% CI: 0.98–1.00; p = 0.02).
Conclusions
This study has shown that more people who undergo cataract surgery have diabetes than previously reported. Also, people with diabetes are at higher risk of developing complications than previously reported. HbA1c concentration was not a factor in these adverse post-operative outcomes. However, eGFR was a predictor of risk. More focus should be placed on pre-operatively optimising co-morbidities than diabetes control in those undergoing cataract surgery.
Plain Language Summary
People with suboptimally controlled diabetes (as measured by glycated haemoglobin, HbA1c) who have an operation are at increased risk of post-operative complications. However, whether this risk extends to cataract surgery is unknown. Our single-centre study showed that 34.6% of all cataract operations during the calendar year 2016 were performed on someone with diabetes—a number far higher than previously reported. In addition, we looked at the post-operative outcomes of the 1525 people with diabetes who had a cataract operation. We showed that, overall, more people with diabetes had complications than previously reported: 7.5%. However, in the whole cohort, HbA1c did not differ between those who did and those who did not develop complications. The factors that were associated with differences in the risk of developing complications were whether the person was looked after in secondary care for their diabetes and whether they had any kidney disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
People with poorly controlled diabetes (as measured by glycated haemoglobin) who undergo general surgery are at increased risk of post-operative complications, but whether this risk extends to cataract surgery is unknown. |
We conducted a single-centre study that looked at all cataract surgeries done during the calander year 2016 to see whether diabetes was a factor in the development of post-operative complications. |
What was learned from the study? |
Our data show that HbA1c is only a significant risk for developing post-operative complications after cataract surgery in those under secondary-care diabetes follow-up, but also that renal function, as measured by the estimated glomerular filtration rate, has a small but significant effect. |
Furthermore, 34.6% of all people who underwent cataract surgery had diabetes. |
For people undergoing cataract surgery, more focus should be placed on pre-operatively optimising co-morbidities than diabetes control. |
Introduction
Diabetes mellitus remains one of the most prevalent long-term conditions in the world, with 537 million people estimated to have the condition in 2021, which is expected to rise to 783 million by 2045 [1].
While retinopathy remains one of the most feared ophthalmic complications of diabetes, cataracts are possibly of greater concern, as they cause greater morbidity than sight-threatening diabetic retinopathy. In the UK, cataract surgery remains the most frequent surgical procedure, with almost 410,000 cataract operations performed in 2018–2019 alone [2]. Previous work has suggested that approximately 20% of all cataract operations were carried out in people with diabetes [3]. However, these data are over 25 years old and, with the rise in prevalence of diabetes, this number is now likely to be much higher.
It has been known for some time that good long-term glycaemic control, as measured by glycated haemoglobin (HbA1c), in people with diabetes reduces their risk of developing micro- and macrovascular complications [4, 5]. In particular, tight glycaemic control has been shown to reduce the need for ocular surgery in those with type 1 diabetes [6], but not necessarily in those with type 2 diabetes [7]. Furthermore, there are observational data indicating that in many different surgical specialities, poor peri-operative glycaemic control, as measured by glucose or HbA1c, is associated with an increased risk of adverse post-operative outcomes [8,9,10,11,12,13,14,15]. However, there are very few data on ophthalmic surgical outcomes in people with inadequately controlled diabetes [16].
This retrospective study looked at the correlation between peri-operative HbA1c and risk of post-operative complications in over 4000 people undergoing cataract surgery.
Methods
Study Design, Setting and Patients
This study was carried out in a single centre: the Norfolk and Norwich University Hospitals NHS Foundation Trust, Norfolk, UK. This was deemed a service improvement exercise by our audit department, who work with our ethics committee. They felt that ethical approval was not necessary.
Data Collection
Individuals were included in the study if they were listed on the database used to collect surgical procedures, ORSOS® (Per-Se Technologies, Atlanta, USA), and had a phacoemulsification and intraocular lens implant (IOL) procedure under local anaesthesia between 1 January 2016 and 31 December 2016. The dataset included a description of the surgery (“Phacoemulsification lens plus implant of lens”), the date of surgery, laterality, hospital number and date of birth. Individuals were excluded if they had non-ophthalmic surgery or were coded as having any additional procedures in addition to phacoemulsification and intraocular lens implant. Individuals on dialysis were excluded.
The HbA1c and estimated glomerular filtration rate (eGFR) were extracted from our electronic pathology system, ICE® (Sunquest Information Systems, Tucson, USA). Where available, the results obtained closest to the day of surgery were used, within 3 months of the procedure. Individual patient-level data obtained using our in-house patient administration system from the hospital eye clinic were cross-checked with the individuals’ National Health Service numbers. We also determined if their diabetes was under primary or secondary care follow-up.
Study Outcomes
The primary outcome was the development of post-operative complications (as defined in the Royal College of Ophthalmologists Cataract Surgery Guidelines 2010 [17]) that necessitated at least one eye clinic visit. For each person who underwent surgery, all ophthalmology clinic letters since the date of surgery were reviewed in our electronic letter warehouse for any evidence of post-surgical complications affecting the operated eye.
Statistical Analysis
Initial descriptive analyses were undertaken to compare subjects who had complications with subjects who did not have complications post cataract surgery.
A univariate logistic regression was undertaken to determine if there was any significant association between complications and the clinical factors HbA1c and eGFR and being on the secondary-care diabetes register.
Results
4401 individuals met our inclusion and exclusion criteria. Of these, 1525 (34.6%) had diabetes and are the subject of this analysis. An HbA1c value was available for all of them; the values for 958 individuals (62.8%) were from before the surgery while those for the remaining 567 individuals (37.2%) were obtained within 3 months after their operation.
Complications
Of the 1525 subjects included in this analysis, 569 (37.3%) were known to be on the secondary-care diabetes register. Table 1 shows the data for the entire cohort, 114 (7.5%) of whom developed post-op complications. It also shows the differences in HbA1c, eGFR and age between those who did and those who did not develop post-operative complications. The mean HbA1c was slightly higher in the 114 individuals with complications compared to the 1411 people with no complications: 52 mmol/mol (95% CI: 49–55) vs 50 mmol/mol (95% CI: 49–51). Table 2 shows that this was not statistically significant after adjustment (p = 0.85).
Table 1 also shows that in the 94 people for whom data were available, the mean eGFR was slightly lower in those with complications (67.1 mL/min/1.73 m2; 95% CI: 63.0–71.2) compared to the 1303 individuals with no complications (70.8 mL/min/1.73 m2; 95% CI: 69.8–71.8). Table 2 shows that this difference remained statistically significant after adjustment (p = 0.03).
Table 1 also shows that the mean HbA1c for subjects under primary care (n = 956) was much lower than for those who had their diabetes managed in secondary care (n = 569): 45 mmol/mol (95% CI: 44–45) vs 59 mmol/mol (95% CI: 58–61). The mean eGFR for the 906 people under primary care follow-up for their diabetes was higher than the eGFR of the 491 under secondary-care diabetes follow-up: 71.6 mL/min/1.73m2 (95% CI: 70.5–62.8) vs 68.5 mL/min/1.73m2 (95% CI: 66.7–70.4).
Table 2 also shows the unadjusted and adjusted odds ratios of the HbA1c, eGFR and age for those with and without complications as well as for those under secondary-care diabetes follow-up. A slightly higher proportion of those under secondary care had complications: 9.5% (n = 54) compared to 6.3% (n = 60). After adjustment, this was not significant (p = 0.47).
Age also had a very small effect size, with an OR of 0.98 (95% CI: 0.97–1.00, p = 0.05). Being under secondary care follow-up was a confounding factor for eGFR and HbA1c because it was no longer significant (p = 0.41) after adjusting for HbA1c, eGFR and age.
Table 2 also shows that the unadjusted OR for HbA1c was 1.12 (95% CI: 1.11–1.14, p < 0.01) for those on the secondary-care diabetes register, and the unadjusted OR was 0.99 (95% CI: 0.99–0.99, p = 0.01) for eGFR. When adjusting for HbA1c, eGFR, age and complications, the OR remained almost unchanged for HbA1c and eGFR: 1.13 (95% CI, 1.11–1.15, p < 0.01) and 0.99 (95% CI: 0.98–1.00, p = 0.02), respectively.
Discussion
Our single-centre study has shown that in people with diabetes, peri-operative glycaemic control as measured by HbA1c was not associated with the risk of developing post-operative ophthalmic complications (as defined by the Royal College of Anaesthetists—Table 3) [17] after cataract surgery (adjusted OR 1.00; 95% CI: 0.99–1.02; p = 0.85). However, for those under secondary care follow-up for their diabetes, there was an increased risk (adjusted OR 1.55, 95% CI: 1.06–2.27, p = 0.03). For the overall cohort, the eGFR was a stronger predictor of the risk of developing complications than HbA1c (adjusted OR 0.99, 95% CI: 0.98–1.00, p = 0.03). We accept, however, that the small difference in value is likely to be of little clinical significance. We have also shown that a higher than previously reported number of people with diabetes underwent cataract surgery—34.6% of the whole cohort.
Our data are in line with recently published data from a UK Biobank study looking at the relationship between HbA1c and the risk of post-operative complications in all forms of surgery. Those authors showed that, whilst the unadjusted risk of an adverse post-operative event was significant (OR [95% CI] 1.43 [1.02–2.02]; p = 0.04) in individuals who underwent any form of surgery within 1 year of an abnormal HbA1c measurement, the risk of poor pre-operative glycaemic control no longer remained significant after adjustment for hyperglycaemia-related comorbidity (OR [95% CI] 1.37 [0.97–1.93]; p = 0.07) [18].
Diabetes causes macrovascular and microvascular complications, namely myocardial infarction, stroke, and renal, nerve and eye disease. Discussions of eye disease in diabetes most often centre on retinopathy, but cataract formation is a recognised ophthalmic complication of diabetes and a leading cause of blindness worldwide [19]. In people with diabetes, cataracts occur more frequently and at an earlier age than in those without diabetes [20, 21]. Age is the major risk factor for those with type 2 diabetes, whilst the presence of other microvascular diseases is the main risk in those with type 1 diabetes [22]. It is believed that diabetes causes cataract formation by causing thickening of the posterior capsule of the lens. The molecular mechanism is believed to be a combination of the non-enzymatic glycation of lens proteins and the accumulation of sorbitol together with polyol pathway activation leading to oxidative stress and apoptosis of lens epithelium [23]. The cascade is similar to that described as one of the unifying mechanisms for the development of other microvascular complications in diabetes [24].
Cataracts are usually treated surgically, with the preferred method being phacoemulsification, which was first introduced almost 50 years ago but became more widely accepted in the mid-1990s [25, 26]. Phacoemulsification is preferred partly because it has better outcomes for visual acuity and has a lower cost compared to extracapsular cataract extraction [27]. As with all forms of surgery, it has a complication rate.
The most recent audit from the Royal College of Ophthalmologists showed that a complication occurred in 2.8% of all cataract operations carried out in 2018–2019 [2]. These complications included uveitis, keratopathy, worsened visual acuity, retinopathy and maculopathy [28,29,30]. Although the overall outcome of phacoemulsification is excellent, results may differ in people with diabetes [31].
There are data to show that inadequate glycaemic control, measured as high peri-operative glucose [9,10,11,12] or HbA1c [13,14,15], is associated with poor post-operative outcomes. These include increased risk of surgical site infection, the development of acute kidney injury, risk of myocardial infarction, time in the intensive care unit, or death [32]. For cataract surgery, several studies have compared the outcomes with and without diabetes. A review from 1998 showed that people with diabetes had a number of structural and functional corneal abnormalities that significantly increased the risk of post-operative harm [33]. However, there are no data on the outcomes of cataract surgery in people with high pre-operative HbA1c [16]. A small study compared the outcomes of cataract surgery in 56 eyes in people with either type 1 or type 2 diabetes to the outcomes of cataract surgery in 220 eyes of people without diabetes [34]. The glycaemic control of those with diabetes was generally excellent, with a median HbA1c of 44 mmol/mol (6.2%; the threshold HbA1c for diagnosing diabetes is 48 mmol/mol, and below 43 mmol/mol is considered normal). If, as the Royal College of Ophthalmologists report suggested, only 2.8% of people develop complications, this equates to 2 eyes vs 6 eyes in this study, a number that would suggest that the study was significantly underpowered to detect any differences [2]. It is therefore perhaps unsurprising that because of this lack of data, the most recent guideline on eye care for people with diabetes from the International Council of Ophthalmology makes no comment on peri-operative glycaemic control [35].
We found that a far higher proportion of those undergoing cataract surgery had diabetes than was reported over 25 years ago [3]. Those authors quoted a prevalence of approximately 20%, whilst our prevalence was 34.6%. This may reflect the increased prevalence of diabetes in the general population and the ageing population.
We also found that the outcome of cataract surgery is worse for those under secondary care follow-up for their diabetes, with a greater percentage of those people having post-operative complications. This is perhaps unsurprising because the vast majority of diabetes is looked after in primary care, and it is only those who have more difficult-to-control diabetes who would be referred to secondary care for ongoing diabetes management. Despite that, the diabetes control of those with and without complications may be deemed very good: 52 and 50 mmol/mol, respectively. These values are well below the target of 69 mmol/mol set by the UK national guideline for the management of people with diabetes undergoing surgery [36].
Our study has several strengths. We had a large sample size and, because our institution is rather geographically isolated, almost everyone operated on at our hospital is followed up here, and it is their predominant diabetes care provider if they are looked after in secondary care. We also use only one laboratory, meaning that we have access to the biochemical and haematological results for almost everyone.
We acknowledge that there are some limitations to our work. This is a single-centre retrospective cohort study, and as such may not be generalisable. We believe that we have captured everyone who was operated on because we have a specified database that is used for all surgical procedures undertaken at our hospital. We also have a single provider for diabetes-related eye screening across primary and secondary care for the majority of our geographical catchment area. However, there are alternative providers of diabetes eye screening at the peripheral margins of our catchment area. In those regions, cataract operations are carried out at local hospitals, and thus the number of people that travelled to our unit and were thus missed out in our database was likely to have been very small. Furthermore, we do not do ‘community clinics’, and so everyone listed on the diabetes register would be under secondary-care diabetes follow-up. People with long-standing type 2 diabetes, i.e. mainly the elderly population, may have other pre-existing comorbidities that could increase the risk of post-operative complications and are thus cofounding factors that were not adjusted for in our analysis. Furthermore, because cataract surgery is an elective procedure, it may have been that individuals were encouraged to improve their pre-operative glycaemic control in line with national guidance for general surgery [36]. This would have reduced the impact of chronic hyperglycaemia. Because of the retrospective note-based nature of this study, we were also unable to look for other factors that may have further confounded our results, such as smoking, alcohol, body mass index, anaemia, duration of diabetes and blood pressure. Several ophthalmic variables were also not determined because that was not the primary focus of the study. These included pre-operative intraocular pressure, pre-operative spherical equivalent, anterior chamber depth, mean keratometry, intraocular lens power and the presence of previous laser treatment or surgery. Furthermore, because this was a retrospective analysis interrogating clinic letters generated from eye clinic visits to see whether complications were mentioned, we were unable to determine if a complication occurred at the time of surgery or in the post-operative period.
Conclusions
Our study has shown that in people with diabetes, there was no relationship between peri-operative glycaemic control as measured by HbA1c and the risk of developing post-operative complications after cataract surgery. The exception to this was for those under secondary care follow-up for their diabetes, who showed a significantly increased risk. However, for the overall cohort, the eGFR was a stronger predictor of the risk of developing complications than HbA1c. We have also shown that a higher than previously reported number of people underwent catarct surgery—34.6% of the whole cohort.
References
International Diabetes Federation. Diabetes atlas 2021 [article online]. 2021. Available from https://diabetesatlas.org/.
Royal College of Ophthalmologists. National Ophthalmology Audit annual report on cataract surgery, September 2020 [article online]. 2020. Available from https://www.nodaudit.org.uk/u/docs/20/hqsrgmurnv/NOD%20Audit%20Full%20Annual%20Report%202020.pdf
Hamilton AM, Ulbig MW, Polkinghorne P. Management of diabetic retinopathy. London: BMJ Publishing Group; 1996. p. 1–15.
The Diabetes Control and Complications Trial Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
The United Kingdom Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
The DCCT/EDIC Research Group. Intensive diabetes therapy and ocular surgery in type 1 diabetes. N Engl J Med. 2015;372:1722–33.
Azad N, Agrawal L, Bahn G, Emanuele NV, Reaven PD, Hayward R, Reda D. Eye outcomes in Veteran Affairs Diabetes Trial (VADT) after 17 years. Diabetes Care 2021;2021:dc202882. https://doi.org/10.2337/dc20-2882.
Dhatariya K, Levy N. Perioperative diabetes care. Clin Med. 2019;19:437–40.
Khuri SF, Henderson WG, DePalma RG, Mosca C, Healey NA, Kumbhani DJ. Determinants of long-term survival after major surgery and the adverse effect of postoperative complications. Ann Surg. 2005;242:326–41.
Kotagal M, Symons RG, Hirsch IB, Umpierrez GE, Dellinger EP, Farrokhi ET, Flum DR. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2016;261:97–103.
Frisch A, Chandra P, Smiley D, Peng L, Rizzo M, Gatcliffe C, Hudson M, Mendoza J, Johnson R, Lin E, Umpierrez GE. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care. 2010;33:1783–8.
Akirov A, Shochat T, Dotan I, Diker-Cohen T, Gorshtein A, Shimon I. Glycemic variability and mortality in patients hospitalized in general surgery wards. Surgery. 2019;166:184–92.
Yong PH, Weinberg L, Torkamani N, Churilov L, Robbins RJ, Ma R, Bellomo R, Lam QT, Burns JD, Hart GK, Lew JF, Martensson J, Story D, Motley AN, Johnson D, Zajac JD, Ekinci EI. The presence of diabetes and higher HbA1c are independently associated with adverse outcomes after surgery. Diabetes Care. 2018;41:1172–9.
Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R. Preoperative A1C and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care. 2014;37:611–6.
van den Boom W, Schroeder RA, Manning MW, Setji TL, Fiestan GO, Dunson DB. Effect of A1C and glucose on postoperative mortality in noncardiac and cardiac surgeries. Diabetes Care. 2018;41:782–8.
Kumar CM, Seet E, Eke T, Dhatariya K, Joshi GP. Glycaemic control during cataract surgery under loco-regional anaesthesia: a growing problem and we are none the wiser. Br J Anaesth. 2016;117:687–91.
Royal College of Ophthalmologists. Cataract surgery guidelines, September 2010 [article online]. 2010. Available from https://www.rcophth.ac.uk/wp-content/uploads/2014/12/2010-SCI-069-Cataract-Surgery-Guidelines-2010-SEPTEMBER-2010-1.pdf.
Lam S, Kumar B, Loke YK, Orme SE, Dhatariya K. Glycated haemoglobin (HbA1c) and the risk of postoperative complications in people without diabetes: a prospective population-based study in UK Biobank. Anaesthesia 2022. https://doi.org/10.1111/anae.15684.
Leasher JL, Bourne RR, Flaxman SR, Jonas JB, Keeffe J, Naidoo K, Pesudovs K, Price H, White RA, Wong TY, Resnikoff S, Taylor HR. Global estimates on the number of people blind or visually impaired by diabetic retinopathy: a meta-analysis from 1990 to 2010. Diabetes Care. 2016;39:1643–9.
Klein BE, Klein R, Moss SE. Prevalence of cataracts in a population-based study of persons with diabetes mellitus. Ophthalmology. 1985;92:1191–6.
Nielsen NV, Vingding TR. The prevalence of cataract in insulin dependent and non-insulin dependent diabetes mellitus. Acta Ophthalmol. 1984;62:595–602.
Klein BE, Klein R, Moss SE. Incidence of cataract surgery in the Wisconsin Epidemiologic Study of Diabetic Retinopathy. Am J Ophthalmol. 1995;119:295–300.
Javadi M-A, Zarei-Ghanavati S. Cataracts in diabetic patients: a review article. J Ophthalmic Vis Res. 2008;3:52–65.
Brownlee M. Biochemistry and molecular cell biology of diabetic complications. Nature. 2001;414:813–20.
Linebarger EJ, Hardten DR, Shah GK, Lindstrom RL. Phacoemulsification and modern cataract surgery. Surv Ophthalmol. 2019;44:123–47.
Goldstein JL. How a jolt and a bolt in a dentist’s chair revolutionized cataract surgery. Nat Med. 2004;10:1032–3.
de Silva SR, Riaz Y, Evans JR. Comparing two different techniques of removing cataracts: phacoemulsification with posterior chamber intraocular lens versus extracapsular cataract extraction (ECCE) with posterior chamber intraocular lens for age-related cataract (Cochrane Database review) [article online]. 2014. Available from https://www.cochrane.org/CD008812/EYES_comparing-two-different-techniques-of-removing-cataracts.
Sadiq SA, Chatterjee A, Vernon SA. Progression of diabetic retinopathy and rubeotic glaucoma following cataract surgery. Eye. 1995;9:728–32.
Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE. Macular edema. Surv Ophthalmol. 2004;49:470–90.
Sahu PK, Das GK, Agrawal S, Kumar S. Comparative evaluation of corneal endothelium in patients with diabetes undergoing phacoemulsification. Middle East Afr J Ophthalmol. 2017;24:74–80.
Pollreisz A, Schmidt-Erfurth U. Diabetic cataract—pathogenesis, epidemiology and treatment. J Ophthalmol. 2010;2010:608751.
Dhatariya K, Levy N, Kilvert A, Watson B, Cousins D, Flanagan D, Hilton L, Jairam C, Leyden K, Lipp A, Lobo D, Sinclair-Hammersley M, Rayman G, for the Joint British Diabetes Societies for Inpatient Care. NHS diabetes guideline for the perioperative management of the adult patient with diabetes. Diabetic Med 2012;29:420–433.
Sanchez-Thorin JC. The cornea in diabetes mellitus. Int Ophthalmol Clin. 1998;38:19–36.
Danni R, Taipale C, Ilveskoski L, Tuuminen R. Diabetes alone does not impair recovery from uneventful cataract surgery. Am J Ophthalmol. 2019;198:37–44.
Wong TY, Sun J, Kawasaki R, Ruamviboonsuk P, Gupta N, Lansingh VC, Maia M, Mathenge W, Moreker S, Muqit MM, Resnikoff S, Verdaguer J, Zhao P, Ferris F, Aiello LP, Taylor HR. Guidelines on diabetic eye care: The International Council of Ophthalmology recommendations for screening, follow-up, referral, and treatment based on resource settings. Ophthalmology. 2018;125:1608–22.
Royal College of Anaesthetists, Centre for Perioperative Care. Guideline for perioperative care for people with diabetes mellitus undergoing elective and emergency surgery [article online]. 2021. Available from https://cpoc.org.uk/guidelines-resources-guidelines-resources/guideline-diabetes.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
KD had the original idea. ABB collected the data and wrote the first draft of the manuscript. IN did the data analysis. KD wrote the final draft of the manuscript. All of the authors saw and approved the final submitted manuscript.
Disclosures
Ketan Dhatariya has nothing to disclose. Ayda Borjian Boroojeny has nothing to disclose. Ian Nunney has nothing to disclose.
Compliance with Ethics Guidelines
The project was registered with the audit department at our institution who work with the ethics committee. They deemed that ethical approval was not required due to the anonymised, retrospective nature of the data collection.
Data Availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Boroojeny, A.B., Nunney, I. & Dhatariya, K.K. The Association Between Glycaemic Control, Renal Function and Post-operative Ophthalmic Complications in People With Diabetes Undergoing Cataract Surgery—A Single-Centre Retrospective Analysis. Diabetes Ther 13, 723–732 (2022). https://doi.org/10.1007/s13300-022-01241-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01241-z