Abstract
Aims
To investigate the efficacy and safety of fast-acting insulin aspart (faster aspart) compared with insulin aspart (IAsp) in participants with type 2 diabetes (T2D) across different subgroups.
Methods
We report on a post hoc analysis of onset 9, a 16-week trial of participants with T2D randomised to faster aspart (n = 546) or IAsp (n = 545). Participants were grouped by baseline HbA1c (< 7.0%, ≥ 7.0%), meal test bolus insulin dose (≤ 10 units [U], > 10 U to ≤ 20 U, > 20 U), body mass index (< 30 kg/m2, ≥ 30 to < 35 kg/m2, ≥ 35 kg/m2), and age (< 65 years, ≥ 65 years). Outcomes assessed were change from baseline in HbA1c and in 1-h postprandial glucose (PPG) increment, and severe or blood glucose (BG)-confirmed hypoglycaemia.
Results
Faster aspart provided reductions in HbA1c comparable to IAsp across all subgroups, with improved 1-h PPG control compared with IAsp in several subgroups. Faster aspart had comparable or improved rates of severe or BG-confirmed hypoglycaemia versus IAsp, particularly in participants with good glycaemic control (HbA1c < 7.0%), the elderly (≥ 65 years old), and those with insulin resistance (> 20 U meal test bolus insulin dose).
Conclusions
Faster aspart provides effective overall glycaemic control, with improved early PPG control compared with IAsp across a range of patient characteristics.
Clinical Trial Registration
NCT03268005.
Plain Language Summary
Fast-acting insulin aspart (faster aspart) is a type of insulin used at mealtimes to reduce the spike in blood sugar resulting from that meal. Faster aspart works in the body more quickly and more effectively than insulin aspart (IAsp), the previous version of this insulin. The properties of insulins in the body can change according to certain patient characteristics. In this study, the researchers wanted to find out if there were differences between various subgroups of patients in the effectiveness and safety of faster aspart compared with IAsp in the treatment of type 2 diabetes. Data were used from a clinical trial (onset 9), in which 546 patients were treated with faster aspart and 545 were treated with IAsp. Patients were grouped by baseline glycated haemoglobin (HbA1c), meal test actual bolus insulin dose, body mass index, and age. Faster aspart provided reductions in HbA1c comparable to IAsp across all subgroups, with improved glucose control 1 hour after a meal compared with IAsp, in several subgroups. Faster aspart had comparable or improved rates of hypoglycaemia versus IAsp, particularly in participants with good glucose control, the elderly (≥ 65 years old), and those with insulin resistance. In summary, the researchers found that faster aspart provides effective overall glucose control, with improved early mealtime glucose control compared with IAsp across patients with a range of baseline characteristics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Fast-acting insulin aspart (faster aspart) is a modified formulation of insulin aspart (IAsp) with an earlier onset and greater initial exposure and glucose-lowering effect than IAsp in patients with type 2 diabetes (T2D) treated with basal insulins. |
The aim of this study was to investigate the efficacy and safety of faster aspart compared with IAsp in participants with T2D across different subgroups. |
What was learned from the study? |
Faster aspart provides effective overall glycaemic control in T2D. |
Improved early postprandial glucose control with faster aspart versus IAsp. |
These results were observed across a range of baseline characteristics. |
Introduction
Safely reaching glycated haemoglobin (HbA1c) targets can be difficult for individuals with diabetes because of ineffective treatment regimens, complications of treatment such as severe hypoglycaemia, or comorbid diseases [1,2,3]. In recent years, treatment guidelines have focused on patient-centred care and individualised treatments, including consideration of patients’ clinical characteristics and comorbidities [4]. Evidence suggests that these clinical characteristics in heterogeneous populations of adults with type 2 diabetes (T2D) can impact patients’ therapeutic response to treatment [5,6,7]. Such parameters include glycaemic control (measured by HbA1c level), age, duration of disease, and background antidiabetic medication [5,6,7,8].
There are other factors that may influence the choice of diabetes treatment. For example, increased body mass index (BMI) has been associated with poor glycaemic control and insulin resistance; weight loss in individuals with a high BMI can lead to lower insulin requirements [9]. A further consideration is the risk of hypoglycaemia, which is higher in people with poor glycaemic control (HbA1c ≥ 9.0%) or lower HbA1c levels (< 6.0%) [6], and in older people [10].
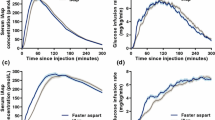
Postprandial glucose (PPG) control is an important aspect to consider when choosing a basal–bolus insulin intensification regimen that controls mealtime blood glucose (BG) excursions, while minimising the risk of severe hypoglycaemia [11,12,13]. Rapid-acting insulin analogues are used to control PPG excursions, and are effective in doing so because their pharmacokinetic/pharmacodynamic profile approximates that of endogenous insulin secretion in response to meals [14]. With basal insulin, the majority of treatment effect on glycaemic control is achieved by 12 weeks after dose optimisation [15, 16]. Clinically, the healthcare practitioner can then optimise the bolus insulin regimen.
Fast-acting insulin aspart (faster aspart) is a modified formulation of insulin aspart (IAsp) containing the excipients niacinamide, which accelerates initial absorption, and l-arginine, which optimises the stability [17]. Faster aspart has been shown to have an earlier onset and greater initial exposure and glucose-lowering effect [18], improved 1-h PPG control, with similar rates of hypoglycaemia compared with IAsp [19]. Faster aspart demonstrated superior 1-h PPG control and a lower rate of treatment-emergent severe or BG-confirmed hypoglycaemia compared with IAsp when used in combination with insulin degludec (degludec) in patients not optimally controlled on a basal–bolus insulin regimen [20].
The pharmacokinetic responses of insulins, including faster aspart, may change according to certain patient characteristics, leading to varied responses to treatment [21, 22]. Therefore, in this post hoc analysis of onset 9 trial data, we aimed to investigate whether there were differences between various subgroups of patients in the efficacy and safety of faster aspart compared with IAsp in the treatment of T2D. The patient populations were analysed according to clinical parameters at baseline including HbA1c level, meal test bolus insulin dose, BMI, and age, which are commonly used to guide treatment decisions in these patients. In this analysis, baseline characteristics (specifically HbA1c and daily basal and bolus insulin dose) were measured following 12 weeks of degludec dose optimisation.
Methods
Participants
Participants were adults aged ≥ 18 years who had been diagnosed with T2D for ≥ 10 years and who were not optimally controlled on a basal–bolus insulin regimen for ≥ 1 year before screening with or without oral antidiabetic drugs. A basal–bolus regimen was defined as basal insulin administered once or twice daily and a bolus insulin analogue taken with meals at least three times daily. Participants were required to have HbA1c 7.0–10.0% at screening and ≤ 9.0% at randomisation.
Key exclusion criteria of the onset 9 trial included treatment with injectable glucagon-like peptide-1 receptor agonists ≤ 90 days before screening, and any anticipated initiation or change in concomitant medications (for > 14 consecutive days) known to affect body weight or glucose metabolism. Full inclusion and exclusion criteria have been published previously [20].
Study Design
This study was a post hoc analysis of onset 9 trial data. The detailed trial design and methods of onset 9 (NCT03268005) have been described previously [20]. Briefly, onset 9 was a multicentre, double-blind, treat-to-target randomised active-controlled parallel-group trial (Fig. 1 in the electronic supplementary material, ESM). Participants were randomised 1:1 to faster aspart or IAsp, both delivered in a basal–bolus regimen in combination with degludec, with or without metformin. The trial consisted of a 12-week run-in period during which the dose of degludec was optimised, followed by a 16-week treatment period (during which participants titrated their bolus insulin using a predefined bolus-dosing algorithm), with two follow-up appointments at 7 and 30 days after end of treatment. Baseline was at treatment randomisation (week 0). A standardised mixed-meal tolerance test (described later in this subsection) was performed at baseline and week 16 to examine the effect of faster aspart and IAsp on PPG. The trial was conducted in accordance with the Declaration of Helsinki (64th amendment) and International Conference on Harmonization of Good Clinical Practice. The protocol of the onset 9 trial and patient consent forms were approved by research ethics boards/institutional review boards for all sites. The committee names and reference numbers of all research ethics boards/institutional review boards are provided in ESM Table 1. Informed consent from all participants was obtained in writing prior to any trial-related activities.
For the current post hoc analyses, participants were grouped according to baseline HbA1c (< 7.0%, ≥ 7.0%), actual bolus insulin dose used during the standardised meal test (≤ 10 units [U], > 10 U to ≤ 20 U, > 20 U), BMI (< 30 kg/m2, ≥ 30 to < 35 kg/m2, ≥ 35 kg/m2), and age (< 65 years, ≥ 65 years). The grouping for HbA1c was based on the general guideline-recommended glycaemic target (< 7.0%) [23]. Meal test actual bolus insulin dose, calculated using the ‘500 rule’, is a measure of bolus insulin required, which reflects body weight and insulin resistance. BMI categories are in line with definitions of obesity [24], and the age cut is based on the American Diabetes Association (ADA) Standards of Medical Care in Diabetes for older adults (i.e. 65 years) [25].
For the meal test, study participants consumed a liquid meal containing 78 g carbohydrate (Ensure, Fortisip or NutriDrink), before which they administered a bolus dose of their pre-trial insulin analogue, which had also been used during the run-in period. This test was conducted at baseline when they had a fasting self-monitored BG of 4.0–8.8 mmol/L (71–160 mg/dL). The bolus dose was calculated by dividing the digestible carbohydrate content of the liquid meal by an insulin to carbohydrate ratio. This ratio was calculated using the ‘500 rule’, whereby 500 was divided by the participant’s total daily dose of both basal and bolus insulin [20, 26]. Blood samples were taken 2 min before the meal, and 30 min and 1, 2, 3, and 4 h after the start time of meal consumption. The meal test was repeated at week 16 with the participant’s randomised trial product using the same bolus dose calculated at the baseline meal test.
The following endpoints were analysed for each subgroup at week 16: change from baseline in HbA1c, change from baseline in 1-h PPG increment (meal test), severe or BG-confirmed hypoglycaemia and daily insulin dose (basal, bolus and total insulin dose) [20]. Change from baseline in HbA1c and change from baseline in 1-h PPG increment (meal test) were efficacy endpoints; severe or BG-confirmed hypoglycaemia was a safety endpoint. Hypoglycaemic episodes were defined as treatment-emergent if the onset of the event occurred up to 7 days after the last day of randomised treatment and excluded the events occurring in the run-in period. Severe hypoglycaemia was defined according to ADA classification as a hypoglycaemic event requiring the assistance of another person to take corrective actions [27]. BG-confirmed hypoglycaemia was defined by a plasma glucose value < 3.1 mmol/L (56 mg/dL).
Statistical Analysis
All statistical analyses were based on the full analysis set and were carried out using SAS v9.4 (TS1M5). Estimated treatment difference (ETD) for the change from baseline in HbA1c at week 16 was analysed using an analysis of covariance (ANCOVA) model following multiple imputation, as described below. The factors and covariates used in the models were the same as those in the primary analysis [20] and other onset clinical trials, apart from the addition of the subgroup and its interaction term, and sex and duration of diabetes were included as factors.
Participants with missing HbA1c data at scheduled visits (weeks 4, 8, 12, and 16) had their HbA1c values imputed using available information from the treatment arm to which the participant had been randomised. In the first step, a Markov chain Monte Carlo method was used to obtain a monotone missing data pattern. This imputation was carried out for each treatment group separately and 100 copies of the data set consisting of all randomised participants were generated. In the second step, for each copy, an analysis of variance model was used with sex, region, duration of diabetes, and metformin use at baseline (yes/no) as factors and baseline HbA1c as covariate; the model was fitted to the change in HbA1c from baseline to week 4 for each treatment group separately. The estimated parameters, and their variances, from these models were used to impute missing values at week 4 for participants in each treatment group, based on sex, region, duration of diabetes, metformin use at baseline (yes/no), and baseline HbA1c. In the third step, for each copy of the data set, missing values at week 8 were imputed in the same way as for week 4, with the same factors, but an additional covariate of change from baseline in HbA1c at week 4. This stepwise procedure was repeated sequentially for week 12 and week 16. For each of the complete data sets, the change from baseline to week 16 was analysed using an analysis of variance model with treatment, region, sex, duration of diabetes, and metformin use at baseline (yes/no) as factors, baseline HbA1c as a covariate, and the interaction between treatment and subgroup. Each imputed data set was analysed separately, and the estimates and standard deviations were combined into one estimate and associated standard deviation using Rubin’s formula [28]. The 95% confidence interval (CI) for the treatment differences was calculated from the combined estimate and standard deviation.
A similar statistical model was used to analyse the ETD for change from baseline to week 16 in PPG increments (meal test), and daily basal and bolus insulin doses. For change from baseline in PPG increments (meal test), participants with missing data had their PPG values at week 16 imputed on the basis of information from the IAsp arm.
The number of treatment-emergent severe or BG-confirmed hypoglycaemic episodes was analysed using a negative binomial regression model. The model included treatment, region, and metformin use at baseline as factors, and the interaction between treatment and subgroup.
For treatment differences in HbA1c and PPG, homogeneity across the subgroups was evaluated by performing an F test (p ≥ 0.05 for homogeneity). Homogeneity of hypoglycaemia treatment ratios across the subgroups was determined using a Wald test (p ≥ 0.05 for homogeneity).
Results
A total of 1091 participants were randomised 1:1 to faster aspart (n = 546) or IAsp (n = 545) during the onset 9 trial. All randomised participants from the trial were included in the current post hoc analysis.
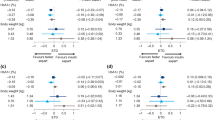
Efficacy and Safety of Faster Aspart Compared with IAsp at Week 16 by Baseline HbA1c
Baseline characteristics were similar between the treatment arms and between the two baseline HbA1c subgroups (ESM Table 2a). Overall reductions from baseline in HbA1c at week 16 were seen for both faster aspart and IAsp (Fig. 1a). The change from baseline in HbA1c was similar between treatments in the baseline HbA1c < 7.0% subgroup (Fig. 1a), while HbA1c was non-significantly lower with faster aspart compared with IAsp in the baseline HbA1c ≥ 7.0% subgroup; ETD − 0.09% (95% CI − 0.18; 0.01) (Fig. 1a). Change from baseline in 1-h PPG increment (meal test) was statistically significantly greater for faster aspart compared with IAsp in both the < 7.0% and ≥ 7.0% baseline HbA1c subgroups; ETD − 0.48 mmol/L (95% CI − 0.87; − 0.09) and − 0.39 mmol/L (95% CI − 0.74; − 0.04), respectively (Fig. 1b).
Analysis by HbA1c: a change from baseline in HbA1c, b change from baseline in 1-h PPG increment, c rates of severe or BG-confirmed hypoglycaemia and estimated treated ratios, at week 16. aChange from baseline in HbA1c was analysed using an analysis of covariance model after multiple imputation assuming treatment according to randomisation. The model included treatment, region, sex, duration of diabetes, and metformin use at baseline (yes/no) as factors, and an interaction between treatment and subgroup, with baseline HbA1c and earlier changes from baseline in HbA1c as covariates. Multiple imputation is used to sequentially impute missing values. An F test is performed to evaluate the homogeneity of the treatment difference across the levels of the subgroup. bObserved data, except for cases where glucose or glucagon is administered. If glucose or glucagon is administered, then the last measurement before rescue intervention is carried forward. Change from baseline in PPG increment (meal test) was analysed using an analysis of variance model after multiple imputation assuming patients on faster aspart switch to insulin aspart. The model included treatment, region, sex, duration of diabetes, and metformin use at baseline (yes/no) as factors, and an interaction between treatment and subgroup, with PPG increments as a covariate. Multiple imputation is used to impute missing values. The conversion factor from PG mmol/L to mg/dL is 18.02. cSevere or BG-confirmed hypoglycaemia was defined according to the American Diabetes Association classification [27] or BG-confirmed by a plasma glucose value < 3.1 mmol/L (56 mg/dL), and episodes were treatment-emergent. The number of hypoglycaemic episodes was analysed using a negative binomial regression model with a log-link function and the logarithm of the time period in which a hypoglycaemic episode is considered treatment-emergent as offset. The model includes treatment, region, sex, duration of diabetes, and metformin use at baseline (yes/no) as factors and the interaction between treatment and subgroup. The p value for homogeneity of treatment differences across levels of the covariate is from a Wald test. BG blood glucose, BMI body mass index, CI confidence interval, ETD estimated treatment difference, ETR estimated treatment ratio, faster aspart fast-acting insulin aspart, HbA1c glycated haemoglobin, IAsp insulin aspart, LS least squares, PPG postprandial glucose, PYE patient-years of exposure
The rate of severe or BG-confirmed hypoglycaemia was statistically significantly lower for faster aspart compared with IAsp in the baseline HbA1c < 7.0% subgroup (estimated treatment ratio [ETR] 0.68 [95% CI 0.52; 0.88]), and was similar between treatments in the baseline HbA1c ≥ 7.0% subgroup (Fig. 1c). In the baseline HbA1c ≥ 7.0% subgroup, of participants treated with IAsp, the basal dose decreased slightly during the trial (ESM Table 3a).
Efficacy and Safety of Faster Aspart Compared with IAsp at Week 16 by Meal Test Bolus Insulin Dose
Baseline characteristics were similar across meal test bolus insulin dose subgroups, except for BMI which increased with greater meal test doses (ESM Table 2b). Change from baseline in HbA1c at week 16 was similar for faster aspart compared with IAsp across meal test bolus insulin subgroups (Fig. 2a). Change from baseline in 1-h PPG increments (meal test) was significantly greater for faster aspart compared with IAsp in the subgroups; > 10 to ≤ 20 U and > 20 U, ETD − 0.39 mmol/L (95% CI − 0.77; − 0.02) and − 0.54 mmol/L (95% CI − 1.07; − 0.01), respectively (Fig. 2b).
Analysis by meal test bolus insulin dose: a change from baseline in HbA1c, b change from baseline in 1-h PPG increment, c rates of severe or BG-confirmed hypoglycaemia and estimated treated ratios, at week 16. For definitions of the superscript letters a–c, see Fig. 1
The rate of severe or BG-confirmed hypoglycaemia was significantly lower in the > 20 U meal test bolus insulin dose subgroup with faster aspart versus IAsp (faster aspart 9.3 events/patient years of exposure [PYE] versus IAsp 13.7 events/PYE; ETR 0.68 [95% CI 0.48; 0.95]; p = 0.024). No significant differences were observed in the other subgroups (Fig. 2c).
Similar daily bolus, basal insulin, and total daily doses were used by participants using faster aspart compared with IAsp at week 1 and week 16 (ESM Table 3b).
Efficacy and Safety of Faster Aspart Compared with IAsp at Week 16 by BMI
Baseline characteristics were similar across BMI subgroups (ESM Table 2c). Generally, comparable glycaemic control, PPG control, and rates of severe or BG-confirmed hypoglycaemia were observed between treatment arms across the BMI subgroups (Fig. 3).
Analysis by BMI: a change from baseline in HbA1c, b change from baseline in 1-h PPG increment, c rates of severe or BG-confirmed hypoglycaemia and estimated treated ratios, at week 16. aChange from baseline in HbA1c was analysed using an analysis of covariance model after multiple imputation assuming treatment according to randomisation. The model included treatment, region, and metformin use at baseline (yes/no) as factors, and an interaction between treatment and subgroup, with baseline HbA1c and earlier changes from baseline in HbA1c as covariates. Multiple imputation is used to sequentially impute missing values. bChange from baseline in PPG increment (meal test) was analysed using an analysis of variance model after multiple imputation assuming patients on faster aspart switch to insulin aspart. The model included treatment, region, and metformin use at baseline (yes/no) as factors, and an interaction between treatment and subgroup, with PPG increments as a covariate. Multiple imputation is used to impute missing values. cSevere or BG-confirmed hypoglycaemia was defined according to the American Diabetes Association classification [27] or BG-confirmed by a plasma glucose value < 3.1 mmol/L (56 mg/dL), and were treatment-emergent. Number of hypoglycaemic episodes is analysed using a negative binomial regression model with a log-link function and the logarithm of the time period in which a hypoglycaemic episode is considered treatment-emergent as offset. The model includes treatment, region, and metformin use at baseline (yes/no) as factors, and the interaction between treatment and subgroup. The p value for homogeneity of treatment differences across levels of the covariate is from a Wald test. BG blood glucose, BMI body mass index, CI confidence interval, ETD estimated treatment difference, ETR estimated treatment ratio, faster aspart fast-acting insulin aspart, HbA1c glycated haemoglobin, IAsp insulin aspart, LS least squares, PPG postprandial glucose, PYE patient-years of exposure
Change from baseline in 1-h PPG increment (meal test) significantly favoured faster aspart over IAsp in the BMI ≥ 30 to < 35 kg/m2 subgroup, ETD − 0.55 mmol/L (95% CI − 1.00; − 0.10), but was not significantly different for the other BMI subgroups (Fig. 3b).
Daily bolus insulin doses were similar between treatment groups within each BMI subgroup. Bolus and basal insulin doses increased gradually for each treatment group with increasing baseline BMI (ESM Table 3c).
Efficacy and Safety of Faster Aspart Compared with IAsp at Week 16 by Age
Baseline HbA1c was similar between treatment arms in the < 65 and ≥ 65 years subgroups (ESM Table 2d). Similar reductions from baseline in HbA1c were observed with both faster aspart and IAsp in participants aged < 65 years and those aged ≥ 65 years (Fig. 4a). Change from baseline in 1-h PPG increment (meal test) favoured faster aspart over IAsp in the < 65 years subgroup, ETD − 0.47 mmol/L (95% CI − 0.82; − 0.13), and was similar between treatments in the ≥ 65 years subgroup (Fig. 4b).
Analysis by age: a change from baseline in HbA1c, b change from baseline in 1-h PPG increment, c rates of severe or BG-confirmed hypoglycaemia and estimated treated ratios, at week 16. For definitions of the superscript letters a–c, see Fig. 3
Severe or BG-confirmed hypoglycaemic episodes for age subgroups are shown in Fig. 4c. The rate of severe or BG-confirmed hypoglycaemia was similar between treatments in the < 65 years subgroup and was statistically significantly lower for faster aspart compared with IAsp in the ≥ 65 years subgroup (faster aspart 11.0 events/PYE versus IAsp 16.3 events/PYE; ETR: 0.68 [95% CI 0.52;0.88]; p = 0.004).
Daily bolus and basal insulin doses were similar between treatment arms for both the < 65 years and ≥ 65 years subgroups (ESM Table 3d).
Discussion
In this post hoc analysis of onset 9 trial data, we analysed whether there were differences between various subgroups of patients in their responses to faster aspart and IAsp, in order to optimise the management of diabetes. Overall, faster aspart provided reductions in HbA1c comparable with IAsp across all subgroups, with improved 1-h PPG control compared with IAsp in several subgroups. Faster aspart was shown to improve rates of severe or BG-confirmed hypoglycaemia compared with IAsp in participants at glycaemic target after basal insulin optimisation (HbA1c < 7.0%), in the elderly (≥ 65 years old), and in those requiring higher bolus insulin doses (> 20 U meal test actual bolus insulin dose). It is clinically relevant that, in elderly participants (≥ 65 years old), faster aspart provided a similar reduction in HbA1c versus IAsp with a reduced risk of severe or BG-confirmed hypoglycaemia.
The results of the current study are supported by those of previous post hoc analyses. In the onset 2 trial, in patients with inadequately controlled T2D on basal insulin, faster aspart was non-inferior compared with IAsp in a basal–bolus regimen in terms of change in baseline HbA1c, and overall hypoglycaemia rates were similar between treatments [19]. In the post hoc analysis, there was improved PPG control with faster aspart compared with IAsp for patients in the > 20 U bolus insulin dose subgroup and no significant treatment differences in favour of faster aspart in the ≤ 10 and > 10–20 U dose subgroups [29]. In another post hoc analysis, the association between baseline characteristics HbA1c and BMI and treatment differences (faster aspart versus IAsp) were investigated [30]. The change from baseline in HbA1c was similar across baseline HbA1c (≤ 7.5%, > 7.5 to < 8.0%, ≥ 8.0%) and BMI (< 25 kg/m2, 25 to < 30 kg/m2, ≥ 30 kg/m2) subgroups in onset 2, and statistically significantly in favour of faster aspart compared with IAsp in onset 3 [30]. Overall, baseline HbA1c and BMI subgroups did not have a clinically relevant effect on treatment outcomes.
In terms of real-world relevance, patients and physicians have reported better PPG control using faster aspart compared with other mealtime insulins [31]. As per the guidelines, treatment should be tailored towards the patient, as part of a patient-centred model of diabetes management [32, 33]. The results of the current analysis show that effective glycaemic control can be achieved with faster aspart when used by patients of a variety of different characteristics. This had been demonstrated in previous post hoc analyses in patients with T2D uncontrolled on basal insulin therapy (duration of diabetes 12.7 years [19]) [29, 30]. In the current post hoc analysis, this has now also been demonstrated in patients with long-standing T2D not optimally controlled with a basal–bolus insulin regimen (duration of diabetes 19.4 years [20]).
The strengths of this post hoc analysis included that the data were from a large, double-blind randomised controlled trial (onset 9). A breadth of patient characteristics was assessed, providing information that may help guide clinical decisions based on patient’s baseline HbA1c, BMI, and age. In the analysis, the subgroup data were analysed using the same statistical method (ANCOVA), allowing for consistency when comparing subgroups.
This study also has some limitations. As with all studies carried out post hoc, the interpretation of the results requires caution. The number of participants in each of the meal test bolus insulin dose subgroups was relatively small, and each subgroup was defined individually without combining any of the subgroups to observe the effect this may have had on the outcomes. For example, some patients in clinical practice may be both elderly and in a higher BMI category, with HbA1c < 7.0%. Additionally, the bolus insulin dose that was used to categorise the patients into subgroups was calculated using the meal test at baseline. However, during the 16-week treatment period, the bolus insulin dose was titrated using a bolus-dosing algorithm. Therefore, the actual bolus insulin requirement might have differed from that calculated at baseline. A limitation of the primary study design is the relatively short follow-up period (16 weeks) compared with other trials in the onset clinical programme.
Conclusions
The results of this post hoc analysis indicate that faster aspart provides effective overall glycaemic control, with improved early PPG control compared with IAsp across a range of baseline characteristic categories. In addition, certain subgroups of patients, including those using higher insulin doses, patients ≥ 65 years old, and patients with HbA1c < 7.0%, may benefit from a lower risk of severe or BG-confirmed hypoglycaemia with the use of faster aspart compared with IAsp.
References
Mauricio D, Meneghini L, Seufert J, et al. Glycaemic control and hypoglycaemia burden in patients with type 2 diabetes initiating basal insulin in Europe and the USA. Diabetes Obes Metab. 2017;19:1155–64.
Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycaemia in type 2 diabetes. Diabet Med. 2008;25:245–54.
Wami WM, Buntinx F, Bartholomeeusen S, Goderis G, Mathieu C, Aerts M. Influence of chronic comorbidity and medication on the efficacy of treatment in patients with diabetes in general practice. Br J Gen Pract. 2013;63:e267–73.
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;(41):2669–701.
Mearns ES, Sobieraj DM, White CM, et al. Comparative efficacy and safety of antidiabetic drug regimens added to metformin monotherapy in patients with type 2 diabetes: a network meta-analysis. PLoS ONE. 2015;10: e0125879.
Lipska KJ, Warton EM, Huang ES, et al. HbA1c and risk of severe hypoglycemia in type 2 diabetes: the diabetes and aging study. Diabetes Care. 2013;36:3535–42.
Garg SK, Aurand LA, Rimler MS, Dailey GE. Diabetes duration and the efficacy and safety of insulin glargine versus comparator treatment in patients with type 2 diabetes mellitus. Endocr Pract. 2014;20:120–8.
Geller AI, Shehab N, Lovegrove MC, et al. National estimates of insulin-related hypoglycemia and errors leading to emergency department visits and hospitalizations. JAMA Intern Med. 2014;174:678–86.
Bramante CT, Lee CJ, Gudzune KA. Treatment of obesity in patients with diabetes. Diabetes Spectr. 2017;30:237–43.
Huang ES, Laiteerapong N, Liu JY, John PM, Moffet HH, Karter AJ. Rates of complications and mortality in older patients with diabetes mellitus: the diabetes and aging study. JAMA Intern Med. 2014;174:251–8.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2019. Diabetes Care. 2019;42:S90–102.
Hinnen DA. Therapeutic options for the management of postprandial glucose in patients with type 2 diabetes on basal insulin. Clin Diabetes. 2015;33:175–80.
Riddle MC, Rosenstock J, Vlajnic A, Gao L. Randomized, 1-year comparison of three ways to initiate and advance insulin for type 2 diabetes: twice-daily premixed insulin versus basal insulin with either basal-plus one prandial insulin or basal-bolus up to three prandial injections. Diabetes Obes Metab. 2014;16:396–402.
Home PD. The pharmacokinetics and pharmacodynamics of rapid-acting insulin analogues and their clinical consequences. Diabetes Obes Metab. 2012;14:780–8.
Jain SM, Seshadri K, Unnikrishnan AG, et al. Best practices and tools for titrating basal insulins: expert opinion from an Indian panel via the modified Delphi consensus method. Diabetes Ther. 2020;11:621–32.
Owens DR, Traylor L, Dain MP, Landgraf W. Efficacy and safety of basal insulin glargine 12 and 24 weeks after initiation in persons with type 2 diabetes: a pooled analysis of data from treatment arms of 15 treat-to-target randomised controlled trials. Diabetes Res Clin Pract. 2014;106:264–74.
Kildegaard J, Buckley ST, Nielsen RH, et al. Elucidating the mechanism of absorption of fast-acting insulin aspart: the role of niacinamide. Pharm Res. 2019;36:49.
Pieber TR, Svehlikova E, Brunner M, Halberg IB, Due Thomsen KM, Haahr H. Fast-acting insulin aspart in people with type 2 diabetes: earlier onset and greater initial exposure and glucose-lowering effect compared with insulin aspart. Diabetes Obes Metab. 2019;21:2068–75.
Bowering K, Case C, Harvey J, et al. Faster aspart versus insulin aspart as part of a basal-bolus regimen in inadequately controlled type 2 diabetes: the onset 2 trial. Diabetes Care. 2017;40:951–7.
Lane WS, Favaro E, Rathor N, et al. A randomized trial evaluating the efficacy and safety of fast-acting insulin aspart compared with insulin aspart, both in combination with insulin degludec with or without metformin, in adults with type 2 diabetes (onset 9). Diabetes Care. 2020;43:1710–6.
Gradel AKJ, Porsgaard T, Lykkesfeldt J, et al. Factors affecting the absorption of subcutaneously administered insulin: effect on variability. J Diabetes Res. 2018:1205121.
Derraik JG, Rademaker M, Cutfield WS, et al. Effects of age, gender, BMI, and anatomical site on skin thickness in children and adults with diabetes. PLoS ONE. 2014;9: e86637.
American Diabetes Association. 6. Glycemic targets: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S66–76.
World Health Organization. Obesity and overweight. https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight. Accessed Nov 2020.
American Diabetes Association. 12. Older adults: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S152–62.
Enander R, Gundevall C, Strömgren A, Chaplin J, Hanas R. Carbohydrate counting with a bolus calculator improves post-prandial blood glucose levels in children and adolescents with type 1 diabetes using insulin pumps. Pediatr Diabetes. 2012;13:545–51.
Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. J Clin Endocrinol Metab. 2013;98:1845–59.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley and Sons; 2004.
Bowering K, Harvey J, Kolaczynski JW, Snyder JW, Bode BW. Mealtime fast-acting insulin aspart versus insulin aspart for controlling postprandial hyperglycaemia in people with insulin-resistant type 2 diabetes. Diabet Med. 2019;36:771–5.
Bowering K, Rodbard HW, Russell-Jones D, et al. Investigating the association between baseline characteristics (HbA1c and body mass index) and clinical outcomes of fast-acting insulin aspart in people with diabetes: a post hoc analysis. Diabetes Ther. 2019;10:177–88.
Baru A, Amir S, Ekelund M, Montagnoli R, Da Fernandes JD. A survey of physician experience and treatment satisfaction using fast-acting insulin aspart in people with type 1 or type 2 diabetes. Postgrad Med. 2020;132:320–7.
American Diabetes Association. 1. Improving care and promoting health in populations: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S7–13.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes—2020. Diabetes Care. 2020;43:S98–110.
Acknowledgements
Funding
The onset 9 trial, including study design, data collection, post hoc analysis, interpretation and the journal’s Rapid Service Fee was funded by Novo Nordisk A/S.
Authorship
All authors confirm that they meet the International Committee of Medical Journal Editors (ICMJE) uniform requirements for authorship.
Author Contributions
All authors were involved at all stages of manuscript development, and approved the final version. Furthermore, all authors share final responsibility for the content of the manuscript and the decision to submit it for publication. Wendy Lane is the guarantor of this work and, as such, had full access to all data in the study and takes responsibility for the integrity of the data.
Medical Writing, Editorial and Other Assistance
Medical writing and editorial support for the development of this manuscript, under the direction of the authors, was provided by Matthew Robinson, Amy Hepple and Malgorzata Urbacz of Ashfield MedComms, an Ashfield Health company, funded by Novo Nordisk A/S.
Disclosures
Wendy Lane has served on advisory boards for Novo Nordisk, has received honoraria for serving on speakers’ bureaus for Novo Nordisk and Dexcom, and has received research grant support from Novo Nordisk. Ramsathish Sivarathinasami and Pranav Kelkar are employees of Novo Nordisk A/S. Elena Favaro was an employee of Novo Nordisk A/S at the time of the study. Esteban Jódar reports receiving grants and personal fees from Novo Nordisk for the work for publication; grants and personal fees from Novo Nordisk, MSD, FAES, Eli Lilly, Janssen, Pfizer, AstraZeneca, Boehringer Ingelheim, Sanofi, UCB, Amgen, and personal fees from Mundipharma. Alejandra Oviedo has received research support from Novo Nordisk and is on the speakers’ bureau for Novo Nordisk. Peter A. Senior has received research support to his institution from Novo Nordisk, and serves on an independent data monitoring committee for a clinical trial sponsored by Vertex. Giorgio Sesti has received speaker/consulting honoraria from Novo Nordisk, Eli Lilly, AstraZeneca, Boehringer Ingelheim, MSD, Sanofi, Amgen, GlaxoSmithKline, Theras, L-Nutra, Omikron, Daiichi Sankyo, Sobi, Novartis, and Servier. Edward Franek has participated in advisory panels for AstraZeneca, Bioton, Boehringer Ingelheim and Novo Nordisk, and has received honoraria for serving on speakers’ bureaus for AstraZeneca, Bioton, Boehringer Ingelheim, Eli Lilly, Merck, Merck Sharp & Dohme, Novo Nordisk, and Servier.
Compliance with Ethics Guidelines
The trial was conducted in accordance with the Declaration of Helsinki (64th amendment) and International Conference on Harmonization of Good Clinical Practice. The protocol of the onset 9 trial and patient consent forms were approved by research ethics boards/institutional review boards for all sites. The committee names and reference numbers of all research ethics boards/institutional review boards are provided in ESM Table 1. Informed consent was obtained in writing from all participants prior to any trial-related activities.
Data Availability
The data sets generated and/or analysed during the current study are available from the corresponding author on reasonable request.
Thanking the Participants
We thank all investigators, trial staff and participants of this study.
Prior Presentation
Some data from this study were presented at the American Diabetes Association, 80th Scientific Sessions in 2020 and at the 56th EASD Annual Meeting in 2020.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lane, W., Favaro, E., Jódar, E. et al. Effective Overall Glycaemic Control with Fast-Acting Insulin Aspart Across Patients with Different Baseline Characteristics: A Post Hoc Analysis of the Onset 9 Trial. Diabetes Ther 13, 761–774 (2022). https://doi.org/10.1007/s13300-022-01213-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01213-3