Abstract
Introduction
FreeStyle Libre® 2 system is a sensor-based flash-monitoring system that measures interstitial fluid glucose. The study aimed to compare cost of FreeStyle Libre 2 system and self-monitoring of blood glucose (SMBG) in the type 2 diabetes mellitus (T2DM) population from the Spanish Health System perspective.
Methods
On the basis of data collected from a literature review, the cost of glucose monitoring was modelled for patients with T2DM on a basal-bolus insulin regimen. The cost estimate included annual consumption for glucose monitoring (strips, lancets and sensors) and severe hypoglycaemic events (SHE) management. A published rate of SHE (2.5 episodes/patient-year) was considered. A reduction of SHE (− 48.8%) associated with FreeStyle Libre 2 system, derived from the REPLACE trial, was applied. Hospital attendance for 20.5% of SHEs (with subsequent hospitalization in 16.0%) was applied. Consumption of strips and lancets was set at 6/day for SMBG (derived from national monitoring recommendations), and 0.2/day for FreeStyle Libre 2 system users, with 26 FreeStyle Libre 2 sensors/year. Unitary costs (€, year 2020 excluding VAT) were derived from literature (€0.28/strip; €0.09/lancet; €3.09/daily FM sensor; €3804/hospitalized SHE; €1794/hospital-attended non-admitted SHE; €389/community-attended SHE).
Results
Costs were €2700 and €2120/year/patient using SMBG or FreeStyle Libre 2 system, respectively. For 1000 patients with T2DM using basal-bolus insulin, 1220 SHEs/year (with 48 hospitalizations) could be prevented and FreeSytle Libre 2 system could generate cost savings of up to €580,953/year versus SMBG (− 21.5%).
Conclusion
FreeStyle Libre 2 system is a potential cost-saving strategy in patients with T2DM in Spain on a basal-bolus insulin regimen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
A flash monitoring system for glucose monitoring in patients with diabetes mellitus has been demonstrated to be effective and cost savings in some healthcare settings. |
The present analysis estimates the economic impact related to the use of a flash monitoring system, FreeStyle Libre 2, in an adult population with type 2 diabetes (T2DM) treated with basal-bolus insulin in Spain. |
What was learned from the study? |
Use of FreeStyle Libre 2 system in patients with T2DM treated with basal-bolus insulin could be associated with annual savings for the Spanish National System. Savings linked to avoided hypoglycaemic episodes are the main contributor to these savings. |
Using the FreeStyle Libre 2 system in this population could avoid severe hypoglycaemic episodes (up to 1220 in a 1000 patients annually). |
In Spain, the FreeStyle Libre 2 system could be associated with annual savings of up to €581 per patient for the National Health System. |
These results could be useful in the decision-making process related to public reimbursement and resource allocation in the diabetes mellitus field. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14447457.
Introduction
The latest report of the International Diabetes Federation (IDF) estimated that nearly 463 million adults are diagnosed with diabetes mellitus (DM) worldwide [1], and this figure is expected to rise to 578 million and 700 million in 2030 and 2045, respectively [1]. Type 2 DM (T2DM) accounts for the clear majority (around 90.0%) of diabetes cases [1]. The most recent update of a larger epidemiological study on DM (Di@bet.es study) [2] confirmed that known T2DM prevalence in Spain is at 7.8%.
In addition to the increasing clinical burden [3], DM and its complications are associated with an important economic impact. The cost of care for people with diabetes can be up to four times higher than in those without diabetes [4, 5]. Annual global health expenditure on diabetes is estimated to be USD 760 billion [1].
In Spain, DM was ranked as the 15th most common cause of mortality in both sexes in 2016 [6], and the 9th most frequently treated health problem in the public primary care health system [7], and it has been estimated that the direct costs associated with the disease may reach €5100 million, representing 8.0% of global public health expenditure [8].
The therapeutic cornerstone for patients with T2DM lies in the promotion of a healthy lifestyle including a balanced diet, regular physical activity, smoking cessation and maintenance of a healthy body weight. When attempts to change lifestyle are insufficient in controlling blood glucose levels, oral medication with metformin should be the first-line treatment. Beyond this, a range of combination therapy options are now available, but if oral medications are insufficient to maintain blood glucose within the recommended ranges, insulin-based regimens may be required.
Insulin concentration elevations in blood inevitably involve the risk of all types of hypoglycaemia so the use of insulin secretagogues and insulin-based regimens are risk factors for the development of hypoglycaemic episodes [9]. The incidence of hypoglycaemia is higher among insulin-treated patients with T2DM [10, 11], primarily those with complex insulin regimens following the use of basal insulin, who also required personalized treatment adjustments with several types of insulin.
Hypoglycaemia is a major contributing factor to long-term complications and reduced survival in patients with DM, in addition to its detrimental impact on health-related quality of life and increased overall associated costs [12].
Glucose monitoring is a useful tool for controlling glycosylated haemoglobin (HbA1c) levels; however, monitoring based on the self-monitoring of blood glucose (SMBG) has significant limitations [13], because it is cumbersome, painful and costly. Several barriers (physical, such as pain and discomfort; psychological, such as fear and frustration; social, such as interference with lifestyle) are directly related to low patient adherence to the monitoring recommendations established by national [14] and international scientific societies [15, 16].
Monitoring of glucose in interstitial fluid poses an alternative to the traditional SMBG, and is associated with better HbA1c levels, less glucose variability, better quality of life and more lifestyle flexibility [17,18,19].
The FreeStyle Libre® 2 system is an interstitial fluid glucose flash monitoring system with optional alarms, marketed and available in Spain, fully reimbursed under the Basic Services Portfolio of the Spanish National Health System (Sistema Nacional de Salud [SNS]) for the type 1 DM population (T1DM) [20]. The FreeStyle Libre system is fully or partially reimbursed in 36 markets across the world for T1DM and T2DM; in most European countries (France, UK, Germany, Austria, Italy, Portugal, etc.), reimbursement for patients with T2DM has started with patients with T2DM treated with three or more insulin doses a day, including premixed and basal-bolus insulin regimens. The latter is considered a preferred subgroup in national [21] and international [22] guidelines.
The FreeStyle Libre 2 system is accompanied by a digital ecosystem with free mobile applications (FreeStyle Libre Link and FreeStyle LibreLinkUp) and virtual software (Libre View) that simplify glucose monitoring, allowing better management of the disease and facilitating communication between professionals and patients.
The clinical evidence of the FreeStyle Libre 2 system has been evaluated in many randomised clinical trials, like the IMPACT study [23, 24] for T1DM and the REPLACE trial [25, 26] in patients with T2DM and several real-world data studies. Treatment satisfaction with the FreeStyle Libre 2 system has been also tested in the T2DM population [27].
The findings in the REPLACE study showed that patients in the FreeStyle Libre 2 system arm experienced a decrease in the number and mean duration of hypoglycaemic episodes compared with those in the SMBG-only arm [25]. Moreover, the FreeStyle Libre 2 system users reduced their need for finger-prick blood glucose measurements by up to 95.0% versus SMBG.
The overall cost for management in patients with T2DM treated with insulin regimens is expected to be reduced following the lower consumption of SMBG supplies and the decreased need for healthcare resources due to the reduced incidence of hypoglycaemic episodes associated with the use of the FreeStyle Libre 2 system.
In this study a cost analysis was conducted of the FreeStyle Libre 2 system compared to SMBG in adults with T2DM treated with basal-bolus insulin in Spain, which complements a previous analysis published for T1DM [28].
Methods
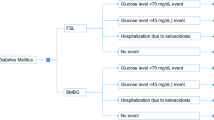
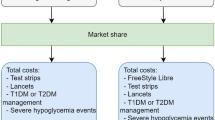
A cost analysis model previously developed for T1DM [28] was used to estimate the economic impact associated with glucose monitoring and the management of hypoglycaemic events in a hypothetical cohort of 1000 adult (> 18 years) patients with T2DM treated with basal-bolus insulin regimen, using the FreeStyle Libre 2 system as compared to standard practice based on SMBG only. The FreeStyle Libre 2 system has been considered in the analysis, as this version of the FreeStyle Libre system will be available in Spain as of early 2020.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors. All the inputs for the model were derived from a literature review, so they were not directly collected from any study.
The perspective of the Spanish National Health System was used to estimate the annual costs derived from the consumption of resources associated with glucose monitoring (strips and lancets, plus FreeStyle Libre sensors in FreeStyle Libre 2 system users) and the management of severe hypoglycaemia.
The values of the parameters, obtained from the published literature, were validated by a panel of eight experts (three endocrinologists, two primary care physicians and three specialists in internal medicine) with expertise in the management of patients with diabetes.
A review of the scientific literature was performed to identify the available evidence on hypoglycaemia rates in the T2DM population.
In line with the widely accepted definition, severe hypoglycaemic episodes were regarded as those requiring help from another person [29, 30].
A wide variation of severe hypoglycaemia rates per patient-year was found during the literature review. The Hypoglycaemia Assessment Tool (HAT) study, an observational study conducted in 24 countries, was initially chosen in view of its robustness (sample size, multicentric nature and representativeness of the Spanish population) [31] to obtain base case results. In the aforementioned study an annual incidence of 2.5 severe hypoglycaemic episodes was reported per patient for the T2DM population [31].
The efficacy of the FreeStyle Libre system in T2DM was evaluated by the REPLACE study [25], a phase III, randomized, multicentre clinical trial that included 224 patients under intensive insulin therapy from 26 diabetes centres in three European countries (France, Germany and UK). A reduction in hypoglycaemia associated with the use of the FreeStyle Libre system (− 48.8% for episodes with glucose level < 2.5 mmol/L [45 mg/dL]) was reported [25].
A proposal for reporting hypoglycaemia events in clinical trials (based on three levels) has been issued by the International Hypoglycaemia Study Group [32]. However, in the REPLACE trial [25] severe hypoglycaemia episodes (requiring third-party assistance) were not specifically reported. For the purpose of this analysis, level 1 episodes according to the American Diabetes Association (ADA) proposed classification were equated to severe hypoglycaemic episodes with glucose level < 2.5 mmol/L (45 mg/dL) (Table 1).
For the management of hypoglycaemic events, the information source was the Emergency Care of the Person with Diabetes Project (PAUEPAD, for its initials in Spanish) [33]. This is a retrospective study of all registered hypoglycaemia-related emergency calls taken by the emergency medical services in Andalusia, Spain (8.5 million inhabitants). Hospital attendance was considered necessary in 20.5% of the episodes of severe hypoglycaemia. The rate of subsequent hospital admission (15.6% of them) comes from a survey in people with insulin-treated T2DM who have experienced severe hypoglycaemic events in Germany, Spain or the UK [34].
A daily consumption of six strips was considered for patients with T2DM treated with a basal-bolus insulin regimen, estimated as the average of national recommendations for glucose monitoring in these patients according to their level of blood glucose control [14], and in line with FL2 reimbursement criteria in Spain for patients with T1DM with the same insulin and glucose monitoring requirements. The use of one lancet per SMBG measurement was also assumed.
The REPLACE showed a frequency of 0.2 ± 0.6 tests a day in FreeStyle Libre users [26], meaning a daily consumption of 0.2 strips and lancets which was used for calculations in the present analysis.
Considering the labelling requirements about sensor replacement [35] (one every 14 days), an annual consumption of 26 FreeStyle Libre 2 system sensors was applied in the cohort of patients with T2DM using the FreeStyle Libre 2 system.
The unit costs (in € year 2020 and excluding VAT) were obtained from the reviewed literature (€0.28 /strip [28], €0.09/lancet [28], €3.09/daily FreeStyle Libre 2 sensor [28], €3804.17/severe hypoglycaemic episode with hospital admission [36], €1793.74/severe hypoglycaemic episode with emergency hospital care but no admission [33], €388.83/severe hypoglycaemic episode without hospital care [37]).
Sensitivity Analysis
Sensitivity analyses (SAs) were conducted to assess the model’s robustness by modifying the parameters with the greatest uncertainty. The following one-way SA were carried out: alternative severe hypoglycaemia rate (1.3 episodes per patient-year as indicated in the HAT study for the Northern European and Canadian population) [38] (SA1); reduction of consumption of strips and lancets in patients with SMBG to 3 daily (SA2); variation of consumption of strips and lancets in FreeStyle Libre 2 users to 0.66 per day based on recently published real-world data in Spain [39] (SA3); alternative daily consumption of strips and lancets (3 for SMBG only patients and 0.66 for FreeStyle Libre 2 users) (SA4); theoretical consumption of strips and lancets in patients with SMBG only estimated by assuming equivalence to the monitoring frequency with FreeStyle Libre system observed in a real-world study [39] (13 daily) (SA5).
An additional scenario was also tested, considering non-severe hypoglycaemia events (SA6), equated to those episodes with glucose level ≥ 2.5 mmol/L (45 mg/dL) and < 3.9 mmol/L (70 mg/dL). A rate of 17.02 non-severe hypoglycaemia episodes per patient-year reported on the HAT study [31] was considered. A reduction of 27.7% for episodes with a glucose level < 3.9 mmol/L (70 mg/dL) reported in the REPLACE trial [25] for FreeStyle Libre system users was applied to the non-severe hypoglycaemic events rate. A unitary cost of €15.07/non-severe hypoglycaemia episode [40] was used in calculations.
Results
The total annual cost estimated in this analysis for the SMBG-only arm was €2700 per patient with T2DM receiving basal-bolus insulin. In the FreeStyle Libre 2 user arm, the total annual cost was €2120 per patient.
The costs associated with glucose monitoring in SMBG were €811 per patient. The glucose monitoring cost in patients using the FreeStyle Libre 2 system was €1152 per patient-year. Savings derived from the reduction in the use of daily strips and lancets were €783 (− 96.7%) per patient with T2DM receiving basal-bolus insulin, which offset the FreeStyle Libre 2 system sensor acquisition cost, estimated to be €1125 per patient-year.
The management of severe hypoglycaemic episodes represented an annual cost of €1890 per SMBG patient. In patients with FreeStyle Libre 2 system, the annual cost was €967 per patient. The hypoglycaemic episodes prevented annually with the FreeStyle Libre 2 system would result in a cost saving of €922 (− 48.8%).
The use of the FreeStyle Libre 2 system as compared to SMBG would be associated with an annual total cost saving of €581 (− 21.5%) per patient with basal-bolus insulin (Fig. 1).
In a cohort of 1000 patients with T2DM with intensive insulin therapy (basal-bolus regimen), a total of 2500 severe hypoglycaemic episodes would occur using SMBG versus 1280 with the FreeStyle Libre 2 system. Thus, the FreeStyle Libre 2 system would annually prevent 1220 severe hypoglycaemic episodes (48.8% reduction), and among them 48 cases of hospitalizations due to severe hypoglycaemia (Table 2).
The use of the FreeStyle Libre 2 system would generate total annual savings per 1000 patients of up to €580,953 compared with SMBG in patients with T2DM treated with basal-bolus insulin (Table 3), thus representing a 21.5% reduction in overall costs.
SA results confirmed the model robustness for the 1000 patients with T2DM receiving basal-bolus insulin.
The SA using the alternative severe hypoglycaemia rate (1.3 episodes per patient-year) [38] showed that FreeStyle Libre 2 system use would be related to annual cost savings of €138,323 (− 7.7%), derived from the reduction of 634 severe hypoglycaemic episodes yearly (Table 4).
The modifications in daily use of strips and lancets also produced savings associated with the use of the FreeStyle Libre 2 system versus SMBG that ranged between €113,360 (− 4.9%) with a daily consumption of 3 strips and lancets in SMBG and 0.66 for FreeStyle Libre 2 users and €1,526,950 (− 41.9%) for 13 strips and 3 lancets a day in SBMG (Table 4).
In the additional scenario considering severe and non-severe hypoglycaemic episodes, the total annual cost reached €2,951,884 and €2,309,089 for the cohort with SMBG and the FreeStyle Libre 2 system, respectively. In this scenario it was shown that the use of the FreeStyle Libre 2 system would prevent 5407 hypoglycaemic episodes a year. Of these avoided hypoglycaemic events 1220 would correspond to severe episodes (− 48.8%), and 4187 to non-severe episodes (− 24.6%). Cost savings with the use of the FreeStyle Libre 2 system as compared to SMBG would be up to €642,795 per year (− 21.8%) (Table 4).
Discussion
The efficacy of the FreeStyle Libre 2 system in the T2DM population has been proven in clinical trials [25, 26], and corroborated by real-world studies which have revealed reductions in hospitalizations due to DM complications, such as hypoglycaemic events [41] or ketoacidosis [42].
The present analysis proves the FreeStyle Libre 2 system to be a strategy that results in savings for the clinical management of patients with T2DM treated with basal-bolus insulin in Spain. On the basis of the assumptions described throughout the paper, the present model showed that the FreeStyle Libre 2 system would decrease the total annual cost by up to €580 (− 21.5%) per patient with T2DM treated with basal-bolus insulin, generating annual savings for the Spanish National Health System of more than half a million euros per cohort of 1000 treated patients.
The cost savings associated with the use of the FreeStyle Libre 2 system have also been observed in other settings such as the USA [43], where annual reductions of $1682 per patient with T2DM receiving intensive insulin therapy were estimated in relation to the use of the FreeStyle Libre 2 system in comparison to SBMG (with a use of six strips and lancets per day), in terms of glucose monitoring. Additionally, reductions in the cost of severe hypoglycaemia events management were also shown (− $852 per patient/year).
At the European level, cost savings following the use of theFreeStyle Libre 2 system have been demonstrated for the UK setting in analyses comprising patients with T1DM [44], as well as in models focused on patients with T2DM [45]. The latter one showed annual savings of £191/patient associated with the use of the FreeStyle Libre 2 system in the T2DM population when considering three daily SMBG measurements.
One main limitation of this model involves the incidence of hypoglycaemia. There are a wide range of values available in the literature, very likely because of differences in the methodology and criteria used in the different studies. For the purpose of the present analysis, the expert panel selected a multicentre (2004 healthcare centres), multinational (24 countries), large-scale study (27,585 patients with diabetes; 19,563 patients with T2DM) [31] as the most robust data source. To reduce uncertainty about this parameter a SA was performed with an alternate hypoglycaemia rate, which also presented savings with the FreeStyle Libre 2 system. Additionally, a SA including non-severe hypoglycaemic events was also performed.
Reductions of biochemical hypoglycaemia episodes associated with use of the FreeStyle Libre 2 system reported in the REPLACE study [25] were applied to the incidence of clinical hypoglycaemia in this analysis. This is a controversial issue, because evidence on the relationship between low glucose levels and symptomatic hypoglycaemic episodes is limited, although a recent publication has concluded that the occurrence of biochemical hypoglycaemia (< 3.9 mmol/L or 3 mmol/L) is associated with an increased risk of severe hypoglycaemia [46].
To the better address the issue of hypoglycaemia risk, the International Hypoglycaemia Study Group issued a recommendation to the diabetes community to adopt common glucose levels when reporting outcomes about hypoglycaemic episodes in studies [32]. However, since hypoglycaemic events were not specifically reported in the trial used in this analysis as efficacy source, an assumption was needed to equate those episodes with glucose levels < 2.5 mmol/L (45 mg/dL) to hypoglycaemic episodes requiring external care. Given the results of the REPLACE trial, this assumption represents a conservative scenario, as the proposed definition for severe hypoglycaemic episodes could also be applied to events with glucose levels ≥ 2.5 mmol/L (45 mg/dL).
As a result of the short time horizon of the cost analysis, the long-term benefits of FreeStyle Libre 2 system related to the prevention of other diabetes complications such as cardiovascular disease, renal failure, blindness, amputations, etc. owing to the improved glycaemic control were not included, so these results should be considered as representative of a conservative scenario in this sense.
This analysis assumed that the findings from the REPLACE study are fully transferable to FreeStyle Libre 2 system, but with FreeStyle Libre 2’s optional alarms and the most recent improvements in accuracy, the use of the FreeStyle Libre 2 system could result in an even greater reduction of severe hypoglycaemia events, which could result in higher savings due to the prevention of hypoglycaemic events (especially in patients with hypoglycaemia unawareness).
In addition to the prevented hypoglycaemic episodes, the use of the FreeStyle Libre 2 system was associated with a decrease in the number of SMBG measurements required by the patients. Frequency of SMBG and therefore the daily consumption of strips and lancets is the second critical issue of the present model. The SA corroborated that even in scenarios with a lower number of SMBG measurements, the use of FreeStyle Libre 2 system would be associated with cost reductions of 7.6% as compared to the use of SMBG alone, generating direct cost savings of €175,525 per 1000 patients/year. In a theoretical scenario where the number of finger-prick blood glucose measurements would total 13 a day, which is the number of daily scans with the FreeStyle Libre 2 systems observed in a Spanish real-world study [39], the reduction of total cost would be 41.9% (− €1,526,950 per 1000 patients with T2DM, yearly).
The value of glucose monitoring in the control of diabetes and the strong association between higher SMBG frequency and lower HbA1c levels are undeniable [47]; however, several scientific publications [17, 48] revealed poor adherence to the recommendations set out in the current clinical guidelines [14]. Considering possible low adherence to these monitoring recommendations, SAs with variations in optimum consumption were performed. Although the daily number of SMBG measurements in patients with T2DM was lower than recommended, the savings derived from the prevented hypoglycaemic episodes would offset the costs of purchasing FreeStyle Libre 2 sensors.
Patients’ reasons for poor adherence to the monitoring vary greatly and include lack of time, invasiveness and needle phobia [48, 49]. The features of the FreeStyle Libre 2 system could eliminate some of these barriers [50], thereby increasing the daily number of glucose determinations as has been proven by all the clinical studies and real-world data on the FreeStyle Libre system (like the study from Spain that found a mean number of 13 daily scans) [39].
The savings identified in this cost study are a conservative estimate, as savings linked to hyperglycaemic events prevention by the FreeStyle Libre 2 system have not been included. A Spanish study calculated that the mean cost of a hospital admission for hyperglycaemic crisis was €3364.6 [36]. Another study found that the mean cost per episode involving emergency room care would add an additional cost of €1476.80 per episode [51]. Given that the FreeStyle Libre 2 system now has an optional alarm for high glucose values, the FreeStyle Libre 2’s contribution to the prevention of hyperglycaemic events cannot be disregarded, with its associated savings owing to events prevented.
Furthermore, savings linked to the use of the FreeStyle Libre 2 system and LibreView as a telemedicine tool have not been considered in the present analysis. A literature review revealed a study in which patients in the telemedicine group showed a substantial reduction in their HbA1c levels compared to their counterparts in conventional care, with patients with T2DM being the most favoured (Hedges g = − 0.48) compared to T1DM (Hedges g = − 0.26) [52]. Another meta-analysis [53] of randomized clinical trials identified that the telemedicine, compared to conventional care, reduces hypoglycaemia (odds ratio = 0.42%). Although not specifically referring to patients with DM, a local study has shown that telemedicine could save up to €15 per visit. Patients are the greatest beneficiaries of these savings (owing to shorter waiting time and travel costs) but it is also more efficient from the healthcare perspective [54]. The added benefits of telemedicine in the era of the COVID-19 crisis and lockdown, for patients, healthcare professional and the healthcare system, cannot be disregarded, even though they are not the focus of this analysis. This analysis showed savings from the National Health System perspective, but in addition to the direct medical resources, hypoglycaemic events often entail pain, suffering and work absenteeism which could also impact on the glucose monitoring cost. FreeStyle Libre 2 has been shown to improve quality of life and work productivity [55, 56]. The FreeStyle Libre 2 system has been positively evaluated in patients with T1DM and T2DM by health technology agencies in a number of countries and regions (France, Norway, Scotland, Sweden, England, Wales, etc.), and published cost-effectiveness analyses have shown the efficiency of the FreeStyle Libre 2 system in several settings [57,58,59,60,61,62].
Previous analysis in Spain showed annual cost savings of nearly €2 million (euros year 2019) per 1000 adults patients associated with the use of the FreeStyle Libre 2 system in T1DM populations treated with multiple daily doses of insulin [28].
The use of the FreeStyle Libre 2 system as a substitute for test strips in SMBG may result in savings for the National Health System, while simultaneously improving disease control and patient quality of life. It would be particularly interesting to conduct future studies and/or registries on the use of this technology in real life, with a view to obtaining information on the clinical, economic and quality of life repercussions for patients in our setting—particularly considering that the digital ecosystem accompanying the FreeStyle Libre 2 system (LibreView, FreeStyle Libre Link, FreeStyle Libre LinkUp) can also have an impact on patients, their relatives and healthcare professionals.
Conclusions
The use of FreeStyle Libre 2 flash glucose monitoring system for patients with T2DM treated with basal-bolus insulin therapy is an efficient strategy for the Spanish National Health System thanks to the savings it can generate, owing to both the decrease in hypoglycaemia episodes and to the direct cost savings in blood glucose monitoring.
Considering the assumptions and costs described, in comparison with SMBG, the FreeStyle Libre 2 system would potentially allow cost savings of up to €580,953 per year in a cohort of 1000 patients with T2DM receiving basal-bolus insulin.
Change history
09 July 2021
A Correction to this paper has been published: https://doi.org/10.1007/s13300-021-01093-z
References
International Diabetes Federation. IDF Diabetes Atlas. 9th edition 2019. https://www.diabetesatlas.org/en/resources/. Accessed Feb 2021.
Soriguer F, Goday A, Bosch-Comas A, et al. Prevalence of diabetes mellitus and impaired glucose regulation in Spain: the Di@bet.es study. Diabetologia. 2012;55:88–93. https://doi.org/10.1007/s00125-011-2336-9.
Lovic D, Piperidou A, Zografou I, Grassos H, Pittaras A, Manolis A. The growing epidemic of diabetes mellitus. Curr Vasc Pharmacol. 2020;18:104–9. https://doi.org/10.2174/1570161117666190405165911.
Bruno G, Picariello R, Petrelli A, et al. Direct costs in diabetic and non diabetic people: the population-based Turin study. Italy Nutr Metab Cardiovasc Dis. 2012;22:684–90. https://doi.org/10.1016/j.numecd.2011.04.007.
Mata-Cases M, Casajuana M, Franch-Nadal J, et al. Direct medical costs attributable to type 2 diabetes mellitus: a population-based study in Catalonia. Spain Eur J Health Econ. 2016;17:1001–10. https://doi.org/10.1007/s10198-015-0742-5.
Soriano JB, Rojas-Rueda D, Alonso J, et al. The burden of disease in Spain: results from the global burden of disease 2016. Med Clin (Barc). 2018;151:171–90. https://doi.org/10.1016/j.medcli.2018.05.011.
Díaz S, Dilla T, Reviriego J. Observational studies with type 2 diabetes mellitus treatments in Spain: a systematic literature review. Endocrinol Diabetes Nutr. 2019;66:254–70. https://doi.org/10.1016/j.endinu.2018.09.002.
Lopez-Bastida J, Boronat M, Moreno JO, Schurer W. Costs, outcomes and challenges for diabetes care in Spain. Global Health. 2013;9:17. https://doi.org/10.1186/1744-8603-9-17.
UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50:1140–7. https://doi.org/10.1007/s00125-007-0599-y.
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53 (Erratum in: Lancet 1999;354:602).
Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736–47. https://doi.org/10.1056/NEJMoa0905479.
Amiel SA, Dixon T, Mann R, Jameson K. Hypoglycaemia in type 2 diabetes. Diabet Med. 2008;25:245–54. https://doi.org/10.1111/j.1464-5491.2007.02341.x.
Karter AJ, Parker MM, Moffet HH, et al. Longitudinal study of new and prevalent use of self-monitoring of blood glucose. Diabetes Care. 2006;29:1757–63. https://doi.org/10.2337/dc06-2073.
Menéndez-Torre E, Tarón García T, Ortega Millán C, Fornos Pérez JA, García Mayor R, López Fernández ML. Recomendaciones 2012 de la Sociedad Española de Diabetes sobre la utilización de tiras reactivas para la medición de la glucemia capilar en personas con diabetes [Recommendations of the Spanish Diabetes Society on the use of reagent strips for measuring capillary blood glucose in diabetic patients]. Av Diabetol. 2012;28:3–9. https://doi.org/10.1016/j.avdiab.2012.01.002.
Buse JB, Wexler DJ, Tsapas A, et al. 2019 Update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43:487–93. https://doi.org/10.2337/dci19-0066.
National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. NICE guideline [NG28]. https://www.nice.org.uk/guidance/ng28#:~:text=Guidance,-NICE%20interactive%20flowchart&text=This%20guideline%20covers%20the%20care,and%20managing%20long%2Dterm%20complications. Accessed Sept 2020.
Vincze G, Barner JC, Lopez D. Factors associated with adherence to self-monitoring of blood glucose among persons with diabetes. Diabetes Educ. 2004;30:112–25. https://doi.org/10.1177/014572170403000119.
Vidal Flor M, Jansà Morató M, Galindo Rubio M, Penalba MM. Factors associated to adherence to blood glucose self-monitoring in patients with diabetes treated with insulin. The dapa study. Endocrinol Diabetes Nutr. 2018;65:99–106.
Mian Z, Hermayer KL, Jenkins A. Continuous glucose monitoring: review of an innovation in diabetes management. Am J Med Sci. 2019;358:332–9. https://doi.org/10.1016/j.amjms.2019.07.003.
Ministerio de Sanidad, Consumo y Bienestar Social. Nota de prensa. Ministerio y CC.AA. han aprobado el Plan de Abordaje de Terapias Avanzadas y la priorización de cinco colectivos para la inclusión del sistema flash de monitorización de glucosa para adultos con diabetes tipo1. https://www.mscbs.gob.es/gabinete/notasPrensa.do?id=4430. Accessed Sep 2020.
Gomez-Peralta F, Escalada San Martín FJ, Menéndez Torre E, et al. Spanish Diabetes Society (SED) recommendations for the pharmacologic treatment of hyperglycemia in type 2 diabetes: 2018 update. Endocrinol Diabetes Nutr. 2018;65:611–24. https://doi.org/10.1016/j.endinu.2018.08.004.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S90–102. https://doi.org/10.2337/dc19-S009.
Bolinder J, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R. Novel glucose-sensing technology and hypoglycemia in type 1 diabetes: a multicentre, non-masked, randomised controlled trial. Lancet. 2016;388:2254–63. https://doi.org/10.1016/S0140-6736(16)31535-5.
Oskarsson P, Antuna R, Geelhoed-Duijvestijn P, Kröger J, Weitgasser R, Bolinder J. Impact of flash glucose monitoring on hypoglycemia in adults with type 1 diabetes managed with multiple daily injection therapy: a pre-specified subgroup analysis of the IMPACT randomised controlled trial. Diabetologia. 2018;61:539–50. https://doi.org/10.1007/s00125-017-4527-5.
Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G. Flash glucose-sensing technology as a replacement for blood glucose monitoring for the management of insulin-treated type 2 diabetes: a multicentre, open-label randomized controlled trial. Diabetes Ther. 2017;8:55–73. https://doi.org/10.1007/s13300-016-0223-6.
Haak T, Hanaire H, Ajjan R, Hermanns N, Riveline JP, Rayman G. Use of flash glucose-sensing technology for 12 months as a replacement for blood glucose monitoring in insulin-treated type 2 diabetes. Diabetes Ther. 2017;8:573–86. https://doi.org/10.1007/s13300-017-0255-6.
Yaron M, Roitman E, Aharon-Hananel G, et al. Effect of flash glucose monitoring technology on glycemic control and treatment satisfaction in patients with type 2 diabetes. Diabetes Care. 2019;42:1178–84. https://doi.org/10.2337/dc18-0166.
Oyagüez I, Merino-Torres JF, Brito M, et al. Cost analysis of the flash monitoring system (FreeStyle Libre 2) in adults with type 1 diabetes mellitus. BMJ Open Diabetes Res Care. 2020;8:e001330. https://doi.org/10.1136/bmjdrc-2020-001330.
Seaquist ER, Anderson J, Childs B, et al. Hypoglycemia and diabetes: a report of a workgroup of the American Diabetes Association and the Endocrine Society. Diabetes Care. 2013;36:1384–95. https://doi.org/10.2337/dc12-2480.
Mezquita-Raya P, Reyes-García R, Moreno-Pérez O, et al. Grupo de trabajo de Diabetes mellitus de la Sociedad Española de Endocrinología y Nutrición (SEEN). Documento de posicionamiento: evaluación y manejo de la hipoglucemia en el paciente con diabetes mellitus. Grupo de Trabajo de Diabetes Mellitus de la Sociedad Española de Endocrinología y Nutrición. Endocrinol Nutr. 2013;60:517.e1-517.e18. https://doi.org/10.1016/j.endonu.2013.04.005.
Khunti K, Alsifri S, Aronson R, et al. HAT Investigator Group. Rates and predictors of hypoglycemia in 27 585 people from 24 countries with insulin-treated type 1 and type 2 diabetes: the global HAT study. Diabetes Obes Metab. 2016;18:907–15. https://doi.org/10.1111/dom.12689.
International Hypoglycaemia Study Group. Glucose concentrations of less than 3.0 mmol/l (54 mg/dl) should be reported in clinical trials: a joint position statement of the American Diabetes Association and the European Association for the Study of Diabetes. Diabetologia. 2017;60:3–6. https://doi.org/10.2337/dc16-2215.
Barranco RJ, Gomez-Peralta F, Abreu C, et al. Incidence and care-related costs of severe hypoglycemia requiring emergency treatment in Andalusia (Spain): the PAUEPAD project. Diabet Med. 2015;32:1520–6. https://doi.org/10.1111/dme.12843.
Lammert M, Hammer M, Frier BM. Management of severe hypoglycemia: cultural similarities, differences and resource consumption in three European countries. J Med Econ. 2009;12:269–80. https://doi.org/10.3111/13696990903310501.
Abbott Diabetes Care. FreeStyle Libre 2. User manual. https://freestyleserver.com/Payloads/IFU/2020/q2/ART41007-004_rev-A-Web.pdf. Accessed Jul 28, 2020.
Crespo C, Brosa M, Soria-Juan A, Lopez-Alba A, López-Martínez N, Soria B. Costes directos de la diabetes mellitus y de sus complicaciones en España (Estudio SECCAID: Spain estimated cost Ciberdem-Cabimer in Diabetes). Av Diabetol. 2013;29:186–9.
Hammer M, Lammert M, Mejías SM, Kern W, Frier BM. Costs of managing severe hypoglycemia in three European countries. J Med Econ. 2009;12:281–90. https://doi.org/10.3111/13696990903336597.
Khunti K, Cigrovski Berković M, Ludvik B, et al. Regional variations in definitions and rates of hypoglycemia: findings from the global HAT observational study of 27 585 people with type 1 and insulin-treated type 2 diabetes mellitus. Diabet Med. 2018;35:1232–41. https://doi.org/10.1111/dme.13662.
Gomez-Peralta F, Dunn T, Landuyt K, Xu Y, Merino-Torres JF. Flash glucose monitoring reduces glycemic variability and hypoglycemia: real-world data from Spain. BMJ Open Diabetes Res Care. 2020;8:e001052. https://doi.org/10.1136/bmjdrc-2019-001052.
Parekh W, Hoskins N, Baker-Knight J, Ramirez de Arellano A, Mezquita Raya P. The economic burden of insulin-related hypoglycemia in Spain. Diabetes Ther. 2017;8:899–913. https://doi.org/10.1007/s13300-017-0285-0.
Bergenstal R, Kerr M, Roberts G, Souto D, Nabutovsky Y, Hirsch I. FreeStyle Libre® system use is associated with reduction in inpatient and outpatient emergency acute diabetes events and all-cause hospitalizations in patients with type 2 diabetes. American Diabetes Association. 80th Scientific Sessions – Virtual. 12–14 June 2020.
Roussel R, Guerci B, Vicaut E, Depouvourville G, Detournay B, Emery C. Dramatic drop in ketoacidosis rate after FreeStyle Libre™ system initiation in type 1 and type 2 diabetes in France, especially in people with low self-monitoring of blood glucose (SMBG): a nationwide study. American Diabetes Association. 80th Scientific Sessions – Virtual. 12–14 June 2020.
Shi L, Hellmund R. Cost comparison of flash continuous glucose monitoring with self-monitoring of blood glucose in adults with type 1 or type 2 diabetes using intensive insulin—from a US Private Payer Perspective. US Endocrinol. 2020;16:20–30.
Hellmund R, Weitgasser R, Blissett D. Cost calculation for a flash glucose monitoring system for UK adults with type 1 diabetes mellitus receiving intensive insulin treatment. Diabetes Res Clin Pract. 2018;138:193–200. https://doi.org/10.1016/j.diabres.2018.01.028.
Hellmund R, Weitgasser R, Blissett D. Cost calculation for a flash glucose monitoring system for adults with type 2 diabetes mellitus using intensive insulin—a UK perspective. Eur Endocrinol. 2018;14:86–92. https://doi.org/10.17925/EE.2018.14.2.86.
Beck RW, Bergenstal RM, Riddlesworth TD, Kollman C. The association of biochemical hypoglycemia with the subsequent risk of a severe hypoglycemic event: analysis of the DCCT data set. Diabetes Technol Ther. 2019;21:1–5. https://doi.org/10.1089/dia.2018.0362.
Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36:2009–14. https://doi.org/10.2337/dc12-1770.
Wagner J, Malchoff C, Abbott G. Invasiveness as a barrier to self-monitoring of blood glucose in diabetes. Diabetes Technol Ther. 2005;7:612–9. https://doi.org/10.1089/dia.2005.7.612.
Zambanini A, Feher MD. Needle phobia in type 1 diabetes mellitus. Diabet Med. 1997;14:321–3.
Rittmeyer D, Schmid C, Haug C, Freckmann G. A novel glucose monitoring system versus a conventional SMBG system: time and step analysis. Poster ATTD-0466. 8th International conference on advanced technologies and treatments for diabetes, 18–21 February 2015. Paris, France.
Barranco RJ, Gomez-Peralta F, Abreu C, et al. Incidence, recurrence and cost of hyperglycaemic crises requiring emergency treatment in Andalusia. Spain Diabet Med. 2017;34:966–72. https://doi.org/10.1111/dme.13355.
Tchero H, Kangambega P, Briatte C, Brunet-Houdard S, Retali GR, Rusch E. Clinical effectiveness of telemedicine in diabetes mellitus: a meta-analysis of 42 randomized controlled trials. Telemed J E Health. 2019;25:569–83. https://doi.org/10.1089/tmj.2018.0128.
Hu Y, Wen X, Wang F, et al. Effect of telemedicine intervention on hypoglycaemia in diabetes patients: a systematic review and meta-analysis of randomised controlled trials. J Telemed Telecare. 2019;25:402–13. https://doi.org/10.1177/1357633X18776823.
López Seguí F, Franch Parella J, Gironès García X, et al. A cost-minimization analysis of a medical record-based, store and forward and provider-to-provider telemedicine compared to usual care in Catalonia: more agile and efficient, especially for users. Int J Environ Res Public Health. 2020;17:2008. https://doi.org/10.3390/ijerph17062008.
Charleer S, De Block C, Van Huffel L, et al. Quality of life and glucose control after 1 year of nationwide reimbursement of intermittently scanned continuous glucose monitoring in adults living with type 1 diabetes (FUTURE): a prospective observational real-world cohort study. Diabetes Care. 2020;43:389–97. https://doi.org/10.2337/dc19-1610.
Fokkert M, van Dijk P, Edens M, et al. Improved well-being and decreased disease burden after 1-year use of flash glucose monitoring (FLARE-NL4). BMJ Open Diabetes Res Care. 2019;7:e000809. https://doi.org/10.1136/bmjdrc-2019-000809.
Bilir SP, Hellmund R, Wehler B, Li H, Munakata J, Lamotte M. Cost-effectiveness analysis of a flash glucose monitoring system for patients with type 1 diabetes receiving intensive insulin treatment in Sweden. Eur Endocrinol. 2018;14:73–9. https://doi.org/10.17925/EE.2018.14.2.73.
Gil-Ibáñez MT, Aispuru GR. Análisis de coste-efectividad de control glucémico con FreeStyle Libre® en pacientes diabéticos tipo 1 en atención primaria de salud de Burgos. [Cost-effectiveness analysis of glycaemic control of a glucose monitoring system (FreeStyle Libre®) for patients with type 1 diabetes in primary health care of Burgos]. Enferm Clin. 2019. https://doi.org/10.1016/j.enfcli.2019.07.011 (pii:S1130-8621(19)30295-5).
Vellopoulou K, Kourlaba G, Ntoupis I, Maniadakis N. Economic evaluation of flash glucose monitoring compared to self-monitoring of blood glucose for the management of patients receiving intensive insulin with diabetes type 1 and type 2 in Greece [Abstract]. Value Health. 2017;20:A-585.
Wehler E, Li H, Bilir SP, et al. Cost effectiveness analysis of a flash continuous glucose monitoring system for type 2 diabetes (T2DM) patients receiving intensive insulin treatment in the UK [Abstract]. Value Health. 2017;20:A-246.
Bilir SP, Hellmund R, Wehler E, Li H, Munakata J, Lamotte M. The cost-effectiveness of a flash glucose monitoring system for management of patients with type 2 diabetes receiving intensive insulin treatment in Sweden. Eur Endocrinol. 2018;14:80–5. https://doi.org/10.17925/EE.2018.14.2.80.
Li H, Bilir SP, Donga P, et al. Cost effectiveness analysis of flash glucose monitoring for type 2 diabetes patients receiving insulin treatment in the UK [Abstract]. Value Health. 2014;17:A-351.
Acknowledgements
Funding
Abbott Diabetes Care provided unconditional financial support to performing the analysis, medical writing and the journal’s Rapid Service Fee.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, assume responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authors’ Contribution
Itziar Oyagüez developed the model, reviewed the scientific literature, performed the analyses and drafted the manuscript. Fernando Gómez-Peralta, Sara Artola, Francisco J Carrasco, Juana Carretero-Gómez, Javier García-Soidán, Ricardo Gómez-Huelgas, Juan F Merino-Torres, and Antonio Perez validated the model structure and the inputs and provided information about clinical management of patients with diabetes mellitus in Spain. All the authors contributed to interpretation of the results and reviewed and approved the final version of the manuscript.
Prior Presentation
Preliminary results of this work were submitted XXXI annual congress of the Diabetes Spanish Association (Sociedad Española de Diabetes), held on June 22–24, 2020.
Disclosures
Itziar Oyagüez is an employee of Pharmacoeconomics & Outcomes Research Iberia (PORIB), a consultant specialized in the economic evaluation of healthcare interventions, which provided technical and editorial support to conduct the study. Fernando Gómez-Peralta, Sara Artola, Francisco J Carrasco, Juana Carretero-Gómez, Javier García-Soidán, Ricardo Gómez-Huelgas, Juan F Merino-Torres, and Antonio Perez received payment from Abbott Diabetes Care for consulting activities related to validation of the parameters and results. None of them received financial compensation for reviewing or their co-authorship of this manuscript.
Compliance with Ethics Guidelines
No ethics approval by an ethics committee was required, as no patient-level data were used in the analysis.
This article is based on previously conducted studies and does not contain any new studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Additional information
The shape of the circle sensor unit, FreeStyle, Libre, and related brand marks are owned by Abbott.
The original online version of this article was revised: The original publication was revised due to update in Table 4.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Oyagüez, I., Gómez-Peralta, F., Artola, S. et al. Cost Analysis of FreeStyle Libre® 2 System in Type 2 Diabetes Mellitus Population. Diabetes Ther 12, 2329–2342 (2021). https://doi.org/10.1007/s13300-021-01064-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01064-4