Abstract
Introduction
Basal-bolus (BB) and premixed insulin regimens may lower fasting plasma glucose (FPG) and postprandial plasma glucose (PPG), but are complex to use and associated with weight gain and hypoglycaemia. Although randomized controlled trials and prospective observational studies in insulin-naïve Japanese patients with type 2 diabetes (T2D) inadequately controlled with oral antidiabetic drugs (OADs) initiating these regimens have been conducted, real-world data are lacking. This study describes the characteristics of patients initiating these regimens in routine clinical practice and identifies the course and outcomes of therapy in the year following initiation.
Methods
Adults with T2D initiating BB or premixed regimens following OAD therapies held in a Japanese electronic medical record database were identified (2010–2019). Subcohorts were determined by treatment changes during ≤ 12 months of follow-up (no change, intensified, switched, discontinued). Outcomes included change in glycated haemoglobin levels (HbA1c), probability of first reaching HbA1c < 7% (stratified by baseline OAD number, HbA1c and age), and hypoglycaemia incidence.
Results
The main cohorts comprised 1315 BB and 1195 premixed therapy initiators. Most individuals (67.9%) initiated BB as inpatients; 50.8% switched at a mean of 47.6 days. Mean HbA1c lowering was – 2.5% for BB and – 1.4% for premixed regimens (no change cohorts). Overall, a greater proportion achieved HbA1c < 7% if they were (at baseline) taking fewer OADs, in a lower HbA1c category, and aged ≥ 65 years. Hypoglycaemia incidence (< 70 mg/dl) was higher with BB than premixed regimens and lower in patients aged < 65 years.
Conclusion
Greater HbA1c reductions, but a higher incidence of hypoglycaemia, were reported with BB versus premixed regimens, while both cohorts demonstrated clinically meaningful reductions in HbA1c during follow-up. After initiation, most premixed regimens remained unchanged, whereas switches from BB to less intensive regimens were numerous, in accordance with the use of BB for a limited duration to improve FPG and PPG control.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Japanese people with T2D have a specific pathophysiology that directly influences the choice and potential success of insulin-based therapy. |
Both RCTs and prospective observational studies have previously examined the efficacy and safety of basal-bolus or premixed regimens in insulin-naïve Japanese patients with T2D inadequately controlled on OADs. |
This study is the first retrospective real-world analysis of these insulin regimens in Japanese clinical practice and provides insight into the demographics of the patients and effectiveness of these interventions in routine practice. |
What did the study ask? |
What are the clinical characteristics and glycaemic outcomes of insulin-naïve patients initiating basal-bolus and premixed regimens in routine Japanese clinical practice? |
Does the clinical setting of care impact on the initiation, durability, and effectiveness of these therapeutic regimens? |
What was learned from the study? |
Mean HbA1c was markedly elevated from generally accepted HbA1c targets at the point of initiation of both basal-bolus and premixed regimens. |
Both cohorts demonstrated clinically meaningful reductions in HbA1c over the 12-months of follow-up; larger reductions were observed in the basal-bolus cohort; however, patients on basal-bolus regimens were generally more likely to experience hypoglycaemia. |
Premixed regimens were most commonly commenced in an outpatient setting with therapy being maintained throughout the 12-month observation period, while basal-bolus regimens were more often, but not exclusively, initiated in a hospital setting. |
We also observed that in many cases, complex basal-bolus regimens were only implemented for a relatively short period of treatment, indicating a planned approach to hyperglycaemia alleviation before deintensifying insulin therapy. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14061143.
Introduction
Many people with type 2 diabetes (T2D), despite increasing numbers of oral antidiabetic drugs (OADs), cannot reach or maintain target glycated haemoglobin (HbA1c). Intensification to injectable therapies, especially insulin, although clinically indicated, is often delayed. There are a number of complex and interrelated reasons underlying this delay, which has been termed clinical or therapeutic inertia [1, 2]. Delays in insulin initiation and optimization of glycaemic control lead to both an increased duration of glycaemic exposure with increased risk of diabetic complications and a lower likelihood of reaching glycaemic targets with any single-therapy intervention, such as basal insulin or a glucagon-like peptide-1 receptor agonist (GLP-1 RA) [3, 4]. This reduced response to therapeutic intervention may reflect greater β-cell loss due to progression of the underlying pathophysiological mechanisms or reduced β-cell function as a consequence of hyperglycaemia-mediated glucotoxicity [5, 6]. This decline in β-cell effectiveness leads to a loss of both baseline and prandial insulin secretion, resulting in a rise of both fasting and postprandial glucose levels [7, 8].
Basal insulin may help control high fasting plasma glucose (FPG) levels by suppressing hepatic gluconeogenesis, but it does not address high postprandial plasma glucose (PPG) levels, which can contribute significantly to overall HbA1c and daily glycaemic variability, which may lead to an increased risk of diabetic complications [8, 9]. Basal-bolus (BB) and premixed insulin (premixed) regimens that provide basal and prandial insulins may lower FPG and PPG levels. However, both BB and premixed regimens are complex to use, involving multiple injections aligned to mealtimes, and generally require numerous blood glucose tests and a high degree of patient education for dose adjustments to optimize therapy [10]. As a result, this may require additional costs in terms of ongoing healthcare resource utilization to deliver the required patient education [11, 12]. Compared with basal insulin, these regimens are also associated with more weight gain and a greater risk of hypoglycaemia as doses are increased [13] and, paradoxically, may increase glycaemic variability by inducing a cycle of hypoglycaemia and hyperglycaemia, further undermining patient well-being and adherence. It has been argued that these issues are major determinants underlying patient selection and the therapeutic success of these regimens in real-world clinical settings [14].
Japanese people with T2D have a specific pathophysiology that directly influences the choice and potential success of therapy. They tend to be thinner than Western patients and, although they do accumulate visceral fat, reduced insulin secretion rather than insulin resistance has been proposed as the major metabolic abnormality in this patient population [15, 16]. Japanese patients have a reduced β-cell mass leading to a loss in first-phase insulin secretion and a progressive loss of β-cell mass amplified by reduced β-cell activity due to glucotoxicity necessitates insulin replacement therapy [17, 18]. The requirement for both postprandial and fasting glucose control is well recognized in Japanese patients based on the underlying pathophysiology [17].
Studies examining the use of BB and premixed regimens in insulin-naïve Japanese patients with T2D inadequately controlled on OADs have included randomized controlled trials and prospective observational studies [19,20,21,22]. The current study, which is the first retrospective analysis of routine clinical practice data, provides additional insights into this patient population. The objectives of this real-world observational study were to describe the characteristics of Japanese patients with T2D initiating BB or premixed regimens following OAD therapies and to evaluate the glycaemic outcomes.
Methods
Study Design and Cohort Selection
This population-based, retrospective, observational cohort study used data from the RWD database (RWD-DB) that is maintained by the Health, Clinic, and Education Information Evaluation Institute (HCEI, Kyoto, Japan) with support from Real World Data Co., Ltd. (Kyoto, Japan). The HCEI authorized the use of data for the current study. The database contains the electronic medical records (EMRs) and claims data for about 20 million patients from approximately 160 medical institutions across Japan (dating back to 2000). The stored information includes demographic data, diagnoses, prescriptions, procedures, and laboratory results from both inpatient and outpatient services. The data are automatically extracted from EMRs at each institution; patient records are kept by allocating unique identifiers for each individual, which are valid within the same institution, to ensure anonymity.
Data from 1 January 2010 to 30 June 2019 were used in this analysis. The inclusion criteria for the study were as follows: individuals aged ≥ 18 years with a confirmed diagnosis of T2D (identified using International Statistical Classification of Diseases and Related Health Problems [ICD]-10 codes) receiving OAD therapy who initiated BB (the BB cohort) or premixed (the premixed cohort) regimens either in hospital (inpatients) or in the outpatient setting. The index date was defined as the date of BB or premixed therapy initiation. To be included in the analysis, patient data had to extend ≥ 1 year prior to the index date during which no previous insulin injectable therapies had been prescribed (Fig. 1). In addition, ≥ 1 HbA1c measurement in the 90 days prior to the index date and ≥ 1 HbA1c measurement up to 360 days following the index date had to be available. All individuals were followed up to 360 days after the index date. Patients with type 1 diabetes, gestational diabetes, or polycystic ovarian syndrome (identified from ICD-10 codes in the EMRs or claims data) were excluded.
The main cohort consisted of two groups of patients: those who initiated BB therapy (basal insulin plus separate prandial insulin injections) and those who initiated premixed therapy (insulin that combines a basal and prandial insulin in a single injection) after receiving OADs. The analysis was conducted by examining subcohorts of patients in each group determined by whether treatment changed during the follow-up period. These subcohorts included no change, intensification, switch, and discontinuation groups. Definitions and study designs for the subcohorts are shown in Fig. 1.
This study was approved by the Research Institute of Healthcare Data Science (RIHDS) ethics committee (no. RI2019008). This article is based on an existing EMR database and does not contain any studies with human participants or animals. The manuscript was prepared in line with the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines [23].
Outcomes
The main objectives of the study were to describe the use of premixed and BB insulin regimens at initiation of insulin to include baseline characteristics, influence of clinical setting, duration of therapy, and effectiveness of the intervention after 360 days of treatment. The period used to collect baseline characteristics was over 180 days prior to and up to the index date. The baseline HbA1c value was defined as the last observation within 90 days prior to and including the index date. Glycaemic control was determined by the change in HbA1c level over time. Other outcome measures included the cumulative probability of first reaching glycaemic control (HbA1c < 7%) over 360 days following the index date. The cumulative probability of reaching glycaemic control was also analysed in the subcohorts of patients stratified by the number of OADs used at baseline, HbA1c at baseline, and age on the index date. Safety-related outcomes included hypoglycaemia incidence, defined as the percentage of patients who experienced more than one hypoglycaemia event (blood glucose < 70 mg/dl).
Statistical Analyses
Baseline characteristics and change in HbA1c over time from baseline were analysed using descriptive statistics. The cumulative probability of first reaching glycaemic control over time was estimated using the Kaplan-Meier method, and log-rank tests were used for comparison between subcohort categories. A P value < 0.05 was considered statistically significant.
Results
A total of 957,411 people with T2D were identified in the RWD-DB; of these, 227,664 had received ≥ 1 OAD prescription. The main cohorts analysed consisted of 1315 BB and 1195 premixed initiators who fulfilled the inclusion criteria. A flowchart for patient inclusion is shown in Fig. 2.
Flow diagram of patient cohort selection. BB basal-bolus insulin therapy, EMR electronic medical record, GLP-1 RA glucagon-like peptide-1 receptor agonist, HbA1c glycated haemoglobin, OAD oral antidiabetic drug, PCOS polycystic ovarian syndrome, Premixed premixed insulin therapy, T1D type 1 diabetes, T2D type 2 diabetes. aApplies to BB cohort only. bApplies to premixed cohort only
The baseline demographic and clinical characteristics of the main BB and premixed cohorts are shown in Table 1. The two cohorts were similar in terms of age: mean 64.6 (standard deviation [SD] 12.0) years for BB and 65.4 (11.5) years for premixed initiators, with 53.9% and 55.0% aged ≥ 65 years, respectively. A total of 34.8% of the BB cohort and 40.7% of the premixed cohort were female. Mean (SD) HbA1c at baseline was 9.8% (2.1%) in the BB cohort and 9.0% (1.8%) in the premixed cohort. The observed proportions of relevant comorbidities were generally higher in the BB cohort than in the premixed cohort, with rates of hypertension, dyslipidaemia, obesity, renal impairment, and atherosclerotic cardiovascular disease being higher in the BB cohort (hypertension was 36.0% vs. 25.2%, dyslipidaemia was 32.2% vs. 21.5%, obesity was 4.3% vs. 1.1%, renal impairment was 8.0% vs. 6.6%, and atherosclerotic cardiovascular disease was 36.0% vs. 26.3% in the BB vs. premixed cohorts, respectively). A higher proportion of people commencing BB therapy was taking ≥ 2 OADs at baseline than those commencing premixed therapy (53.8% of those on BB were receiving ≥ 2 OADs compared with 46.9% of those on premixed regimens). The type of OAD that patients were taking differed between the two cohorts; those initiating BB regimens were most commonly taking a dipeptidyl peptidase-4 inhibitor (DPP-4) or sulfonylurea compared with those commencing premixed regimens, who were more likely to be taking a sulfonylurea or an alpha-glucosidase inhibitor.
The baseline demographic and clinical characteristics of the no change and change subcohorts are shown in Table S1 in the electronic supplementary material. In the BB cohort, 45.8% had no change, 3.5% intensified, 45.9% switched, and 4.9% discontinued therapy. In the premixed cohort, 79.7% had no change, 6.8% intensified, 4.9% switched, and 8.5% discontinued therapy.
The baseline demographic and clinical characteristics by the inpatient and outpatient setting of initiation are shown in the supplementary material in Table S2 for the BB cohort and Table S3 for the premixed cohort. The setting of BB and premixed therapy initiation and treatment patterns following initiation are shown in Fig. 3. Of the BB initiators, 67.9% initiated therapy as inpatients and 32.1% initiated therapy as outpatients (Table S2). Among the inpatients, 50.8% switched therapy, 41.0% had no change in therapy, and rates of intensification (3.2%) and discontinuation (4.9%) were low. Among the outpatients, 35.3% switched therapy, 55.9% had no change in therapy, and, again, rates of intensification (4.0%) and discontinuation (4.7%) were low. Individuals initiating BB as inpatients were older than those receiving BB as outpatients, with a mean (SD) age of 65.6 (11.7) years for inpatients compared with 62.5 (12.3) years for outpatients (main cohorts), and a higher percentage of inpatients were aged ≥ 65 years (57.4% of the inpatients and 46.4% of the outpatients). Of the premixed therapy initiators (Table S3), 30.3% initiated therapy as inpatients and 69.7% initiated therapy as outpatients. Among the inpatients, 79.0% had no change in therapy, and rates of intensification (6.1%), switch (4.7%), and discontinuation (10.2%) were low. Among the outpatients, 80.1% had no change in therapy, and rates of intensification (7.1%), switch (5.0%), and discontinuation (7.8%) were also low. Individuals initiating premixed regimens as inpatients were older than those initiating premixed regimens as outpatients (66.6 ± 11.5 years vs. 64.9 ± 11.4 years, respectively), and a higher percentage of inpatients vs. outpatients were aged ≥ 65 years (61.0% vs. 52.3%, respectively).
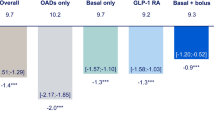
Changes in HbA1c for the BB and premixed therapy subcohorts are shown in Table 2. For those who remained on therapy throughout the follow-up period (the no change subcohorts), mean HbA1c lowering was – 2.5% for BB and – 1.4% for premixed therapy. Kaplan-Meier curves representing the cumulative probability during the follow-up period of first reaching HbA1c < 7% in the no change subcohorts are shown in Fig. 4a and b. The cumulative probability of first reaching HbA1c < 7% in the no change cohorts by baseline characteristics is shown in Fig. 4c–h. After receiving 1, 2, or ≥ 3 OADs at baseline, an HbA1c target < 7% was achieved by 74%, 69%, and 61% of patients who initiated BB, and 66%, 60%, and 50% of patients who initiated premixed regimens, respectively. With a baseline HbA1c ≥ 7 to < 8%, ≥ 8 to < 9%, or ≥ 9%, an HbA1c target < 7% was achieved by 78%, 69%, and 65% of patients who initiated BB and 75%, 59%, and 51% of patients who initiated premixed regimens, respectively. In both the BB and premixed cohorts, a greater proportion of people achieved HbA1c < 7% if they were taking fewer OADs (Fig. 4c, d), were in a lower HbA1c category (Fig. 4e, f), and were older (aged ≥ 65 years; Fig. 4g, h) at baseline. An HbA1c target < 7% was achieved by 63% of patients aged < 65 years and 75% of those aged ≥ 65 years who initiated BB regimens and 55% of patients aged < 65 years and 67% of those aged ≥ 65 years who initiated premixed regimens. For the subcohorts that included a change to therapy, the cumulative probability of first reaching HbA1c < 7% from the index date to the change date is shown in the supplementary material in Fig. S1a and b.
Overall cumulative probability of first reaching HbA1c < 7% within 12 months following the index date in the no change cohorts (a, b), by number of OADs (c, d), by HbA1c groups (e, f), by age (g, h). BB basal-bolus insulin, HbA1c glycated haemoglobin, OAD oral antidiabetic drug, Premixed premixed insulin
The overall incidence of hypoglycaemia (the percentage of patients who had ≥ 1 hypoglycaemia event based on available recorded blood glucose level < 70 mg/dl) in the main cohorts was 20.0% with BB and 15.7% with premixed therapy. The overall incidence of hypoglycaemia was generally lower in those aged < 65 years (16.0% with BB and 11.8% with premixed regimens) compared with those aged ≥ 65 years (23.4% with BB and 18.8% with premixed regimens). The highest incidence of hypoglycaemia was seen in patients aged ≥ 65 years receiving BB (23.4%), and the lowest incidence was seen in patients aged < 65 years receiving premixed regimens (11.8%). The incidence of hypoglycaemia in the subcohorts (from the index date to the end of follow-up in the no change subcohort, and from the index date to the change date in the intensification, switch and discontinuation subcohorts) and by age (< 65 and ≥ 65 years) is shown in Fig. 5.
Incidence of hypoglycaemia according to available recorded blood glucose < 70 mg/dla in a the subcohorts and b by age (< 65 and ≥ 65 years) in the subcohorts. BB basal-bolus insulin, Premixed premixed insulin. aMeasurement of fasting, non-fasting, and unknown blood glucose values are included in the analysis
Discussion
This population-based, retrospective, observational cohort study used real-world data from EMRs and claims to explore the characteristics and glycaemic responses, over a 12-month period of Japanese people with T2D who commenced BB or premixed regimens following OAD therapies. The present study is the first retrospective analysis of these regimens in this population and provides insight into their effectiveness and safety in a real-world setting.
BB and premixed regimens were initiated for Japanese patients with T2D when baseline HbA1c was significantly elevated compared with Japan Diabetes Society (JDS) and American Diabetes Association (ADA)/European Association for the Study of Diabetes (EASD) recommended targets [24, 25]. Despite basal insulin being typically recommended as the first-line insulin therapy in T2D, data from the current study suggest that there is a proportion of Japanese patients where a clinical decision is made (possibly based on high HbA1c levels) that basal insulin may be inadequate treatment and will not deliver target HbA1c. For these patients, a more aggressive dual intervention using basal and prandial insulin that targets both fasting and postprandial glucose levels is selected by clinicians. It has been recommended that BB or premixed regimens should be considered in insulin-naïve patients with T2D when HbA1c is > 8.5% [26].
A recently published study of basal insulin and GLP-1 RA therapy in the same database population showed 3477 patients commencing basal insulin over the same time period. Based on the present study, BB and premixed regimens are relatively common in insulin-naïve Japanese people with T2D [27].
In this study, compared with people receiving premixed regimens, those receiving BB therapy had a higher baseline HbA1c (mean HbA1c was 9.8% with BB vs. 9.0% with premixed regimens) and a shorter disease duration (mean duration was 5.1 years with BB vs. 6.2 years with premixed regimens). We observed that those in the BB cohort were more likely to have comorbidities of interest, representing a higher cardiovascular risk, and that those commencing BB regimens were more likely to be on multiple OADs at baseline. Furthermore, the predominant types of OADs varied considerably between the cohorts, with the use of newer oral therapies such as DPP-4 inhibitors being more prevalent in the BB cohort. This suggests that the clinicians managing these patients may be working in different settings (e.g., hospital vs. primary care) and/or may have different biases for certain medication types. We observed relatively low rates of metformin use across both cohorts, despite this generally being recommended as a first-line oral agent in T2D internationally [25, 28]. This may not be the case in Japanese practice [29]. The variance between the two cohorts in baseline characteristics may indicate that BB regimens tend to be used where disease progression is more aggressive (i.e., with higher HbA1c over a similar duration of disease) and the patient is at greater risk of complications.
While both BB and premixed regimens resulted in impressive and clinically meaningful HbA1c reductions, patients receiving BB therapy experienced greater HbA1c reductions and achieved an HbA1c < 7% more quickly than those receiving premixed therapy; furthermore, a higher proportion of those initiated on BB regimens reached an HbA1c target < 7% (69% of those receiving BB vs. 62% of those receiving premixed regimens). The highest probability of reaching target HbA1c was in the first 3 months of treatment. However, a higher incidence of hypoglycaemia was typically observed with BB than with premixed regimens, as would be expected with the more aggressive glucose-lowering approach [13]. We observed that the incidence of hypoglycaemia was higher in patients aged ≥ 65 years than in those aged < 65 years.
Predictably, patients were more likely to reach an HbA1c < 7% with either BB or premixed regimens if they were taking fewer OADs or had a lower HbA1c at baseline. Perhaps unexpectedly, we observed that patients who were aged ≥ 65 years at baseline also had an increased chance of reaching HbA1c < 7% compared with those aged < 65 years, irrespective of the treatment cohort. This is of interest as guidelines recommend individualization of HbA1c targets and less aggressive targets would generally be considered in older people with T2D given the increased risk of hypoglycaemia-related complications. This result may reflect that older people have better treatment adherence relative to their younger counterparts. However, it is important in all clinical situations that the benefits in effective glycaemic control with any regimen must always be weighed against the risk of hypoglycaemia, regimen complexity, and patient acceptability.
In Japanese clinical practice, it is well described that BB treatment is often initiated as an inpatient intervention, with the patient admitted for 1–2 weeks to stabilize and adjust insulin doses and provide patient education [6, 30]. The initiation of BB therapy is also described as a therapeutic intervention designed to reduce glucotoxicity and improve β-cell function with the specific intention that this be a transient intervention, which will be de-escalated at an appropriate time to a less complex insulin-based regimen. The results of this study challenge the generality of these observations and suggest that real-world clinical practice is somewhat different to the accepted narrative. A majority of patients (68%) were initiated on BB regimens as inpatients, but a significant proportion of patients (32%) were still initiated on BB therapy as outpatients. By contrast, among patients initiating premixed regimens, 70% were outpatients and 30% were inpatients, possibly reflecting the belief that premixed therapy is a simpler alternative to BB therapy. Overall, among those who initiated BB therapy as inpatients, 41% did not change therapy, 51% went on to switch, 3% intensified and 5% discontinued. Of the patients initiating BB therapy in an outpatient setting, the majority (56%) remained on BB therapy unchanged, 35% switched, 4% intensified, and 5% discontinued. Irrespective of where BB treatment was commenced, among patients who did switch (46%), the switch was at a mean (median) of 47.6 (17.0) days following initiation. This confirms that BB therapy is utilized as a transient intervention but its use in this manner is inconsistent and this approach is not operating as a population intervention strategy. This means that a large proportion (46%) remains unintentionally on a BB regimen for the long term. By contrast, the majority of the premixed cohort (80%) had no change in therapy throughout the follow-up period, suggesting that premixed therapy, despite its well-known limitations, is seen as an accepted ongoing intervention. Importantly, switching/de-escalating therapy was not associated with deterioration in glycaemic control over the course of our follow-up period, which would support the approach of an aggressive reduction in glucose to reduce β-cell glucotoxicity and improve β-cell function.
The data in this study suggest that a possible determinant of an effective BB treatment strategy may require access to an inpatient facility. Such high levels of intensive intervention may, in the future, be inconsistent with patterns of healthcare, patient choice, or sustainable care. Treatments that can be more readily and reliably delivered in an outpatient setting may be more acceptable for patients and healthcare systems alike.
Future directions for real-world research in this space should also examine the relative effectiveness, safety, and use of the recently introduced once-daily fixed-ratio combinations (FRCs) in Japan, which combine basal insulin and GLP-1 RAs into a single formulation that targets fasting and postprandial hyperglycaemia. While we observed that BB and premixed therapies produce meaningful reductions in HbA1c, the risk of hypoglycaemia and complexity of these regimens may make them undesirable for some patients. FRC products, therefore, could be considered in similar populations following inadequate control using increasing OADs to reduce hypoglycaemia or promote weight loss [31, 32] in both inpatient and outpatient settings. Furthermore, given the frequent but inconsistent strategy of short-duration BB therapy, FRCs may also be a suitable alternative for patients to de-escalate to simple regimens with a low injection burden following a reduction in glucotoxicity.
Limitations
A number of limitations should be taken into account when considering the findings from this analysis. The database consists of a limited number of hospitals and clinics and does not cover all regions of Japan, and patients who were not part of the participating facilities were not captured in this study. Furthermore, patients who transferred to other institutions could not be followed up. While a large number of patients were identified in the database, the sample size was diminished, possibly because of errors in coding (e.g. patients coded as having prediabetes rather than T2D) or the exclusion of those who had their OADs prescribed in, or were lost to follow-up by transferring to, non-participating centres. Data were based on prescriptions written, and imperfect adherence could have reduced the effects of treatment. The reporting of hypoglycaemia incidence alone provides only limited information; as the characteristics of those who experienced hypoglycaemia are unknown, it is unclear whether high-risk factors were present, and there is no analysis of the effects of hypoglycaemia on individuals. We acknowledge that the hypoglycaemia incidence results may have been influenced by different time exposure in the various change subcohorts. While it is common knowledge that Japanese patients with T2D are often admitted to an inpatient facility to commence insulin therapy, reasons for admission were not analysed in this study so it is possible that this might have been for other medical reasons. It should be noted that this study was not intended to be an efficacy comparison between BB and premixed therapies, and we expected to observe underlying differences in the patient populations for which these regimens were used.
Conclusions
In Japanese people with T2D, insulin was initiated after OAD failure when HbA1c was markedly elevated. Compared with premixed therapy initiators, BB therapy initiators were younger with higher HbA1c levels and a shorter disease duration at baseline. They experienced greater HbA1c reductions but a higher incidence of hypoglycaemia. BB regimens were commenced more frequently in inpatient settings. By contrast, premixed regimens were mostly initiated in outpatients. Changes or de-intensification of BB regimens were common, often after relatively short periods of exposure, and these occurred more frequently in patients who commenced BB therapy as inpatients. This suggests a predetermined strategy to reduce glucotoxicity quickly and efficiently by targeting FPG and PPG before commencing less intensive injectable regimens.
References
Harris SB, Kapor J, Lank CN, Willan AR, Houston T. Clinical inertia in patients with T2DM requiring insulin in family practice. Can Fam Physician. 2010;56:e418–24.
Khunti S, Davies MJ, Khunti K. Clinical inertia in the management of type 2 diabetes mellitus: a focused literature review. Br J Diabetes. 2015;15:65–9.
Blonde L, Meneghini L, Peng XV, et al. Probability of achieving glycemic control with basal insulin in patients with type 2 diabetes in real-world practice in the USA. Diabetes Ther. 2018;9:1347–58.
Rosenstock J, Aronson R, Grunberger G, et al. Benefits of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide versus insulin glargine and lixisenatide monocomponents in type 2 diabetes inadequately controlled on oral agents: the LixiLan-O randomized trial. Diabetes Care. 2016;39:2026–35.
Campos C. Chronic hyperglycemia and glucose toxicity: pathology and clinical sequelae. Postgrad Med. 2012;124:90–7.
Del Prato S. Loss of early insulin secretion leads to postprandial hyperglycaemia. Diabetologia. 2003;46(Suppl 1):M2-8.
Kahn SE. Clinical review 135: the importance of beta-cell failure in the development and progression of type 2 diabetes. J Clin Endocrinol Metab. 2001;86:4047–58.
Fonseca V. Clinical significance of targeting postprandial and fasting hyperglycemia in managing type 2 diabetes mellitus. Curr Med Res Opin. 2003;19:635–41.
Nalysnyk L, Hernandez-Medina M, Krishnarajah G. Glycaemic variability and complications in patients with diabetes mellitus: evidence from a systematic review of the literature. Diabetes Obes Metab. 2010;12:288–98.
van Brunt K, Curtis B, Ivanyi T, et al. Basal-bolus therapy in patients with type 2 diabetes mellitus in the UK: patient characteristics, treatment patterns and the effect of switching to premixed insulin. Diabetes Ther. 2016;7:793–807.
Iqbal A, Heller SR. The role of structured education in the management of hypoglycaemia. Diabetologia. 2018;61:751–60.
Walker GS, Chen JY, Hopkinson H, Sainsbury CAR, Jones GC. Structured education using Dose Adjustment for Normal Eating (DAFNE) reduces long-term HbA1c and HbA1c variability. Diabet Med. 2018;35:745–9.
Holman RR, Farmer AJ, Davies MJ, et al. Three-year efficacy of complex insulin regimens in type 2 diabetes. N Engl J Med. 2009;361:1736–47.
Giugliano D, Sieradzki J, Stefanski A, Gentilella R. Personalized intensification of insulin therapy in type 2 diabetes—does a basal-bolus regimen suit all patients? Curr Med Res Opin. 2016;32:1425–34.
Fukushima M, Suzuki H, Seino Y. Insulin secretion capacity in the development from normal glucose tolerance to type 2 diabetes. Diabetes Res Clin Pract. 2004;66(Suppl 1):S37–43.
Lee S, Yabe D, Nohtomi K, et al. Intact glucagon-like peptide-1 levels are not decreased in Japanese patients with type 2 diabetes. Endocr J. 2010;57:119–26.
Kohei KAKU. Pathophysiology of type 2 diabetes and its treatment policy. JMAJ. 2010;53:41–6.
Sakuraba H, Mizukami H, Yagihashi N, Wada R, Hanyu C, Yagihashi S. Reduced beta-cell mass and expression of oxidative stress-related DNA damage in the islet of Japanese type II diabetic patients. Diabetologia. 2002;45:85–96.
Masuda H, Sakamoto M, Irie J, et al. Comparison of twice-daily injections of biphasic insulin lispro and basal-bolus therapy: glycaemic control and quality-of-life of insulin-naïve type 2 diabetic patients. Diabetes Obes Metab. 2008;10:1261–5.
Domeki N, Matsumura M, Monden T, Nakatani Y, Aso Y. A randomized trial of step-up treatment with premixed insulin lispro-50/50 vs. aspart-70/30 in patients with type 2 diabetes mellitus. Diabetes Ther. 2014;5:403–13.
Wenying Y, Benroubi M, Borzi V, et al. Improved glycaemic control with BIAsp 30 in insulin-naïve type 2 diabetes patients inadequately controlled on oral antidiabetics: subgroup analysis from the IMPROVE study. Curr Med Res Opin. 2009;25:2643–54.
Nezu U, Nakamura A, Aoki K, Kimura M, Terauchi Y. Comparative study of effectiveness of multiple-daily injections of insulin versus twice-daily injections of biphasic insulin in patients with type 2 diabetes. Endocr J. 2009;56:193–200.
STROBE. STrengthening the reporting of observational studies in epidemiology 2014. https://www.strobe-statement.org/index.php?id=strobe-home. Accessed Oct 02, 2020.
Araki E, Goto A, Kondo T, et al. Japanese clinical practice guideline for diabetes 2019. J Diabetes Investig. 2020;11:1020–76.
Davies MJ, D’Alessio DA, Fradkin J, et al. Management of hyperglycemia in type 2 diabetes, A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2018;2018(41):2669–701.
National Institute for Health and Care Excellence. Type 2 diabetes in adults: management. 2015. https://www.nice.org.uk/guidance/ng28/resources/type-2-diabetes-in-adults-management-1837338615493. Accessed Oct 02, 2020.
Baxter M, Morimoto Y, Tamiwa M, et al. A real-world observational study evaluating the probability of glycemic control with basal insulin or glucagon-like peptide-1 receptor agonist in Japanese patients with type 2 diabetes. Diabetes Ther. 2020;11:1481–96.
Haneda M, Noda M, Origasa H, et al. Japanese Clinical Practice Guideline for Diabetes 2016. Diabetol Int. 2018;9:1–45.
Seino Y, Kuwata H, Yabe D. Incretin-based drugs for type 2 diabetes: Focus on East Asian perspectives. J Diabetes Investig. 2016;7(Suppl 1):102–9.
Ikeda S, Crawford B, Sato M. Utilization patterns of insulin therapy and healthcare services among Japanese insulin initiators during their first year: a descriptive analysis of administrative hospital data. BMC Health Serv Res. 2016;16:6.
Moreira RO, Cobas R, Lopes Assis Coelho RC. Combination of basal insulin and GLP-1 receptor agonist: is this the end of basal insulin alone in the treatment of type 2 diabetes? Diabetol Metab Syndr. 2018;10:26.
Kaneto H, Koshida R, Baxter M. Fixed-ratio combination of basal insulin and glucagon-like peptide-1 receptor agonists in the treatment of Japanese people with type 2 diabetes: an innovative solution to a complex therapeutic challenge. Diabetes Obes Metab. 2020. https://doi.org/10.1111/dom.14095 (Online ahead of print).
Acknowledgements
The authors thank Shiro Hinotsu, the representative director of the Health, Clinic, and Education Information Evaluation Institute, for database development for the study and Asuka Ozaki (Sanofi) for advice on data interpretation and critical review of the manuscript.
Funding
Sponsorship for this study was funded by Sanofi. The Rapid Service Fee was funded by Sanofi.
Medical Writing Assistance
Medical writing assistance was provided by Sarah Smith, PhD, of Caudex (Oxford, UK), funded by Sanofi.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Prior Presentation
Data from this study were presented at the 56th European Association for the Study of Diabetes (EASD) Virtual Meeting, 21–25 September 2020 (poster 668).
Disclosures
Hideaki Miyoshi has received honoraria for lectures from Astellas Pharma, Eli Lilly K.K., Kowa Pharmaceutical, Mitsubishi Tanabe Pharma, MSD K.K., Nippon Boehringer Ingelheim, Novartis, Novo Nordisk, Ono Pharmaceutical, Sanofi, AstraZeneca K.K., and Sumitomo Dainippon Pharma; and research funding from Abbott Japan, Astellas Pharma, Daiichi Sankyo, Eli Lilly K.K., Kowa Pharmaceutical, Mitsubishi Tanabe Pharma, Nippon Boehringer Ingelheim, Novo Nordisk, Ono Pharmaceutical, Sumitomo Dainippon Pharma, LifeScan Japan K.K., and Taisho Pharmaceutical. Mike Baxter is a medical therapy expert for Sanofi UK, and a non-executive director of Ashford and St. Peter’s NHS Foundation Trust, and Frimley Health NHS Foundation Trust. Takeshi Kimura and Masakatsu Hattori are employees of Real World Data, Co., Ltd. Yukiko Morimoto and Masami Tamiwa are employees of Sanofi K.K. Dion Marinkovich is an employee of Sanofi Australia & New Zealand. Takahisa Hirose has received honoraria from AstraZeneca K.K., Eli Lilly K.K., Kowa Pharmaceutical, Mitsubishi Tanabe Pharma, MSD K.K., Nippon Boehringer Ingelheim, Novartis K.K., Novo Nordisk, Ono Pharmaceutical, Sanofi K.K., Sumitomo Dainippon Pharma, and Takeda; research funding from AstraZeneca K.K. and Mitsubishi Tanabe Pharma; and subsidies/donations from Astellas Pharma, Bayer Yakuhin, Daiichi Sankyo, Eli Lilly K.K., Mitsubishi Tanabe Pharma, MSD K.K., Nippon Boehringer Ingelheim, Novartis K.K., Novo Nordisk, Ono Pharmaceutical, Sanofi K.K., Soiken, Taisho Pharmaceutical, and Takeda.
Compliance with Ethics Guidelines
This study was approved by the Research Institute of Healthcare Data Science (RIHD) ethics committee (no. RI2019008). This article is based on an existing EMR database and does not contain any studies with human participants or animals.
Data Availability
These analyses were conducted on medical records data provided under a commercial license, which the authors are unable to share.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Miyoshi, H., Baxter, M., Kimura, T. et al. A Real-World, Observational Study of the Initiation, Use, and Effectiveness of Basal-Bolus or Premixed Insulin in Japanese People with Type 2 Diabetes. Diabetes Ther 12, 1341–1357 (2021). https://doi.org/10.1007/s13300-021-01041-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-021-01041-x