Abstract
The year 2021 will mark 100 years since the discovery of insulin. Insulin, the first medication to be discovered for diabetes, is still the safest and most potent glucose-lowering therapy. The major challenge of insulin despite its efficacy has been the occurrence of hypoglycemia, which has resulted in sub-optimal dosages being prescribed in the vast majority of patients. Popular devices used for insulin administration are syringes, pens, and pumps. An artificial pancreas (AP) with a closed-loop delivery system with > 95% time in range is believed to soon become a reality. The development of closed-loop delivery systems has gained momentum with recent advances in continuous glucose monitoring (CGM) and computer algorithms. This review discusses the evolution of syringes, disposable, durable pens and connected pens, needles, tethered and patch insulin pumps, bionic pancreas, alternate controller-enabled infusion (ACE) pumps, and do-it-yourself artificial pancreas systems (DIY-APS).
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
2021 will mark 100 years since the discovery of insulin. |
Occurrence of hypoglycemia has resulted in sub-optimal use of insulin. |
Insulin delivery devices have rapidly advanced in the past 2 decades. |
A comprehensive review of the insulin delivery devices is presented in this article. |
Advances in the technologies from syringes and pens to pumps and a do-it-yourself (DIY) artificial pancreas aim to accomplish 100% TIR and 0% time in hypoglycemia. |
Introduction
All patients with type 1 diabetes mellitus (T1D) require insulin because of its absolute deficiency. With increasing longevity in type 2 diabetes mellitus (T2D) patients, they will require insulin because of progressive β-cell failure [1,2,3]. Even though insulin is the most powerful therapeutic option available to control hyperglycemia, patients with diabetes experience various challenges including, but not limited to, interference with daily living, financial constraints, complexity of regimens, injection discomfort, and public embarrassment for initiating and adhering to insulin therapy [2, 4]. Therefore, addressing such barriers with advanced and effective technologies for insulin delivery is essential to avoid the complications related to diabetes.
The origin of diabetes therapy dates back to the 1920s with the discovery of insulin and its applications [5]. The advent of diabetes technology, the term used to describe hardware, devices, and software used in diabetes therapy, has transformed patient care [6]. Starting with the syringe for injecting insulin, graduating to insulin pens, insulin pumps, and sensor-augmented pumps, the growth of diabetes technologies accelerated with the introduction of hybrid closed-loop systems, integration with consumer electronics, and cloud-based data systems [7, 8]. Further milestones in insulin therapy such as the development of slow-acting preparations, recombinant insulin, rapid-acting insulin analogs, and long-acting basal analogs have complemented the progress in diabetes technology [9, 10]. Figure 1 summarizes the landmark developments in the evolution of insulin delivery devices.
Notable drawbacks of the crude devices were the poor dose accuracy, lack of social acceptance, prolonged training period, and difficulty in conveyance. Continuous improvements and innovations in the design, technology, and accessibility of insulin delivery devices helped overcome these limitations [11]. The modern insulin delivery devices accomplish insulin delivery in a most precise manner with minimal invasiveness. These devices have favorably impacted patients’ perceptions about insulin therapy in addition to improving their quality of life [12]. However, the right choice and application of diabetes technologies are essential for positive results.
Here, we discuss the current literature on the evolution of insulin delivery devices with a focus on the pros and cons of technologies and anticipated improvements. Considering the vast number of technologic solutions available on the global market, only the most popular devices applicable to patient care are outlined here. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Insulin Delivery Devices
Insulin Syringes
Initially, big and heavy reusable syringes with plungers, barrels, and long large-bore needles were used for insulin delivery. These syringes and reusable needles had to be sterilized by boiling to ensure efficient reuse. The first specialized syringe for insulin injection was manufactured by Becton Dickinson (BD) in 1924 [13]. Novo Nordisk launched its first insulin syringe, the “Novo Syringe,” in 1925 [14]. In 1954, the first disposable glass syringe, the Hypak™ (BD), was launched. The all-plastic Monoject syringe (Roehr Products Inc) was introduced into the market in 1955. BD introduced the 1-ml Luer-Lok insulin syringe available with either a detachable needle or a permanently attached needle in the 1960s. By the mid-1960s, disposable plastic syringes from numerous vendors were available on the market [15]. These syringes reduced pain and the incidence of needle-associated infections [16]. In 1970, BD manufactured the first one-piece insulin syringe with an integral needle [17]. Early in 1983, the British Diabetic Association recommended a change from the commonly practiced two insulin strengths (40 units/ml and 80 units/ml) to single-strength insulin (100 units/ml). This transition initiated the use of glass syringes designated as BS 1619/2 specifically calibrated for U-100 insulin. However, these syringes had a significant drawback associated with the incorrect dosage due to the inherent ‘dead space’: the volume of a solution retained in the hub and the needle when the plunger of the syringe is completely depressed [18, 19].
Later, U-100 plastic insulin syringes with units marking down the side of the syringe came into use [15]. The BD Safety-Lok insulin syringe with advanced safety features was introduced in 1988. BD introduced the BD Veo insulin syringe with an Ultra-Fine 6-mm needle, offering less pain and reduced plunger force to ease the flow of large insulin doses in 2012 [20]. This syringe has been widely preferred since it lowers the risk of intramuscular injections [21]. In 2016, the FDA approved a U-500 specific insulin syringe designed by BD to address the dosing errors while administering doses from a U-500 vial with a U-100 insulin syringe [22]. In place of the long, large bore-sized and reusable needles used in earlier years, currently, small bore-sized and short-length needles (8 mm, 6 mm, and 5 mm) are used for insulin injection.
Even though “conventional” syringe technology has become less popular in the current era, vials and syringes have remained as the only option for insulin delivery for more than 50 years.
Limitations
Despite all the above-mentioned advances, most patients experienced difficulty in injecting insulin multiple times a day [16]. Besides, the use of syringes was associated with poor dose accuracy, a long training period, unpleasant psychologic impact, and difficulties in conveyance [11, 22, 23]. These negative impacts led to a lack of treatment persistence and nonadherence and created barriers to achieving glycemic control [24].
Injection Aids: I-Port Advance Injection Port
Injection aids to reduce the frequency of multiple injections and needle phobia in patients with diabetes are currently in practice. Medtronic launched the i-Port Advance Injection Port, a device that combines an injection port and inserter, in 2016. It is a small and discrete patch that can be attached to the skin. The device remains adhered to the skin up to 72 h and allows multiple injections. Thus, it eliminates direct injection on the skin and multiple punctures for each injection [25]. A study by Khan et al. reported that regular usage of i-Port Advance improved treatment compliance and reduced the frequency of hypoglycemic events and hospitalizations in 55 insulin-treated patients. However, the study could not reveal any significant difference in HbA1c reduction or patient satisfaction between regular and irregular users [25]. Although there was an initial excitement, this device remains unpopular probably because insulin shots are virtually painless with the newer needles.
Insulin Pen
The introduction of the insulin pens was a milestone in insulin delivery. The first insulin pen, the NovoPen, was launched by Novo Nordisk in 1985, followed by NovoPen 2 in 1988. NovoPen 2 has a characteristic dial-up setting to measure the required dose [26]. In general, pens offer more simple, accurate, and convenient insulin delivery over syringes. An insulin pen has three components: an insulin cartridge, a disposable short needle, and an incremental “one-click per unit” dosing. The device can be either reusable or disposable. Reusable insulin pens have a replaceable cartridge. Disposable pens have a prefilled cartridge and are discarded after the use. In 1989, Novo presented the world’s first disposable, prefilled insulin pen, ‘Novolet’ [27]. Insulin adsorbs onto the plastic surface of these prefilled pens over time and a precise concentration can be achieved by proper mixing. Therefore, these pens increased the dose accuracy and blood glucose (BG) stability between cartridge changes [28].
Compared with syringes, pens offer more flexibility, accuracy, discreetness, and long-term cost-effectiveness, contributing to improved treatment persistence and adherence. Therefore, the use of insulin pens demonstrates better glycemic control and has wider acceptance [29, 30].
Technologic refinements over the fundamental features of the earlier versions have produced more sophisticated insulin pens. Finer and safety needles that offer reduced pain perception have also been developed for use with insulin pens. First-generation insulin pens are available in the market from the 1990s. The most popular insulin pens in this category are multiple generations of durable pens of the NovoPen family, AllStar (Sanofi), and prefilled pens, such as FlexPen, FlexTouch (Novo Nordisk), Humalog Pen, Kwikpen (Eli Lilly), and SoloSTAR (Sanofi). NovoPen 3, a durable pen allowing a maximum dosage of 70 U, was launched in 1992. The characteristic features of this device were a dial and push-up button, which allowed less wastage of insulin while resetting the dose. This pen was more economical than its ancestors and was further refined for patient subsegments, such as NovoPen 1.5 and NovoPen Junior. NovoPen 1.5, a shorter version of NovoPen 3, which can hold smaller insulin cartridges, was launched in 1996. In 1999, NovoPen3 Demi, the first Novo family member to allow half-unit dose increments, was commercialized [31]. FlexPen, a prefilled insulin pen, was introduced in 2001. In 2003, NovoPen Junior, with vibrant colors, specifically designed for children with diabetes, was launched [31]. In 2005, the NovoPen 4 (dose increments of 1.0 U, maximum dose of 60 U) was launched. This device offers a more discreet design and requires reduced force to perform an injection [7]. Prefilled insulin pens, Kwikpen (Eli Lilly) and SoloSTAR (Sanofi), were launched in 2007 and 2008, respectively [32]. In 2008, the Next Generation FlexPen (Novo Nordisk), which requires 30% less injection force than the original Flexpen, was introduced. This pen features color-coded cartridge holders and labels, which increased the ease of use and convenience for diabetes patients [33].
In 2011, Novo Nordisk introduced FlexTouch, a re-engineered version of the original FlexPen. It is the single prefilled insulin pen with an easy touch button without an extension instead of a push-button extension. This feature improves the ease of use and device handling for the patients [34]. Sanofi India launched its first indigenously developed reusable insulin pen, AllStar, specifically designed for diabetes patients in India in 2012. The characteristic features of this pen are the slim and discreet design, clear dose magnification window, dose arrow on both sides, bayonet cartridge lock, short dial-out distance, penalty-free reverse dialing, audible click sound with every unit dialed and dispensed, and non-rotating dial button during dispense. This pen was designed to assure the convenience of international standards to Indian diabetes patients at a reasonable price [35]. In 2017, Junior KwikPen, a prefilled half-unit insulin pen, was approved and is considered to be lighter and smaller than other half-unit insulin pens on the market [36]. Besides insulin pens commonly used for years tailored to deliver insulin 100 U/ml, progress in the development of higher concentrated insulin has led to new insulin pens for 200 U/ml (Humalog, Tresiba) and 300 U/ml (Toujeo/Glargine). Humalog 200 U/ml KwikPen (Eli Lilly), Tresiba 200 U/ml Prefilled FlexTouch (Novo Nordisk), and Gla-300 SoloSTAR injector pen (Sanofi) have been in use since 2017 [37,38,39].
These modern pen devices have advanced safety features such as audible clicks with each dose as well as ergonomic features to reduce the physical effort of the injection and confer more user-friendliness, accuracy, and flexibility [40]. Pen needles of 4 mm, 5 mm, 6 mm, 8 mm, and 12.7 mm lengths are used with these insulin pens. The Nano 4-mm pen needle (BD), the shortest pen needle, is more comfortable and easier to use. These needles require low thumb force as well as allow higher flow rate and insulin absorption [41].
Next-Generation Insulin Pens
Second-generation pen devices or “smart pens” with a memory function have been on the scene since 2007. The multidose memory feature allows these devices to store the date, time, and amount of the previous doses [37, 38]. These devices are integrated with USB or Bluetooth features for efficient monitoring and data management. In 2007, Eli Lilly launched HumaPen MEMOIR, the world’s first digital insulin pen with memory, and HumaPen LUXURA HD, a reusable pen for people who need insulin dosing in half-unit increments from 0.5 to 30 units. NovoPen Echo, the first insulin pen with memory and half-unit dosing features, was launched by Novo Nordisk in 2010. This device has several child-friendly attributes and displays time elapsed since the last dose. A research study showed that NovoPen Echo offered a high level of satisfaction among pediatric patients over NovoPen Junior and HumaPen Luxura HD because of its simple memory function, half-increment units, ease of use, and design [42]. Later, in 2013, NovoPen Echo replaced NovoPen Junior because of its wider acceptance over the latter [43]. In 2012, NovoPen 5, a successor to NovoPen 4, with a simple memory function for use with the 3-ml Penfill cartridge, was launched [44].
Future refinements in this field include “smart pens” with in-built calculators to provide proper guidance to patients regarding the insulin dosage, memory functions to display the amount and time of injection, as well as automatic transmission through Bluetooth to produce computer-generated reports [16].
Connected Pens
Connected pens are next-generation insulin pens with features that go beyond the memory function. InPen System, a Bluetooth-enabled wireless insulin pen with a smartphone interface and bolus advisor, is the forerunner of this kind and was launched by Companion Medical in 2017 [45]. According to InPen’s website, this device is “a reusable injector pen plus an intuitive smartphone interface equals smart insulin delivery” [46].
Novo Nordisk’s "soon to be launched" NovoPen 6 and NovoPen Echo Plus also fall into this category of pens. These pens will automatically record the dose of insulin injected, and the data can be shared with collaborating CGM devices and Glooko’s Diasend digital diabetes management platforms. These pens are expected to sync with Roche’s mySugr app as well [47]. Connected pens are equipped with NFC (near-field communication) technology that allows scanning of these devices to transfer the data off to another device [48]. A Bluetooth/internet-connected insulin pen cap that supports the generation of smart dosing systems through a mobile app for the convenience of T1D patients who do not use an insulin pump is another forthcoming innovation in pen technology [49].
Limitations
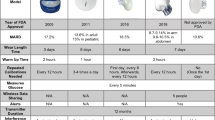
Although insulin pens offer the convenience of use, less pain, and better treatment adherence and health outcomes, they are not devoid of limitations. The disadvantages, such as difficulty in applying a mixture of insulins, higher cost, and lack of universal insurance coverage, have been major concerns [50]. Despite the ease of use, pens are mechanically more complex than insulin syringes [11]. When long-term cost-effectiveness is not considered, treatment with pen devices is more expensive than with insulin vials, especially in low- and middle-income countries [29, 51]. Table 1 summarizes the major advantages and disadvantages of insulin pens.
Insulin Pumps (Continuous Subcutaneous Insulin Infusion-CSII)
Pumps are advanced gadgets for the delivery of insulin and can be used for dispensing insulin in any patient who expresses the willingness to initiate pump therapy [1]. According to the Endocrine Society guidelines, the patients should be assessed for their psychologic status, prior compliance with diabetes self-care, willingness and motivation to try the device, and convenience of the required follow-up visits before suggesting CSII [52]. Typical components of an insulin pump are an insulin reservoir, infusion set, and tubing. The insulin reservoir is connected to the infusion set and a catheter to continuously deliver insulin to meet the daily requirement. The pump has user-specific in-built programs to dispense insulin at basal rates (slow, continuous) and in incremental (bolus) doses before meals [53]. This feature allows the removal of the inherent variations associated with the injection depth and multiple injection sites that are typical of conventional subcutaneous injections. The infusion site needs to be changed only once every 2–3 days. Therefore, insulin pumps eliminate the need for multiple injections on a daily basis resulting in less insulin variation [54, 55].
Continuous subcutaneous insulin infusion (CSII) or the insulin pump was introduced in the late 1970s, originally to treat T1D. The functioning of these devices closly resembles the physiologic method of insulin secretion by the pancreas. The prototype of an insulin pump was designed by Dr. Arnold Kadish in 1963. It was huge and had to be carried like a backpack. In 1974, Dr. Ernst Friedrich Pfeiffer developed the “Biostator,” an insulin pump with intravenous continuous glucose monitoring and closed-loop intravenous insulin infusion features. Even though its large size and complex operation were major limitations for outpatient use, the device proved the feasibility of closed-loop glucose control and facilitated further technology developments [56]. The first wearable insulin pump, known as the ‘blue brick’ and later the ‘autosyringe,’ was designed by Dean Kamen in 1976 and led to the introduction of insulin pump therapy in the same year [57]. In 1979, the first SOOIL insulin pump was clinically evaluated at Seoul National University Hospital [58]. Seven years later in 1983, MiniMed introduced their first insulin pump, MiniMed 502. This system soon underwent significant improvements in size and programmability and thus represented a major technologic breakthrough in the evolution of insulin pumps.
MiniMed introduced the implantable insulin pump to deliver insulin intraperitoneally in 1986. Insulin dispensed through this device was absorbed quickly and directly to the portal system. Studies in type 1 diabetes patients showed that the use of these pumps resulted in appreciable glycemic control with slighter glycemic fluctuations and fewer occurrences of hypoglycemia [59]. In 2000, new versions with improved memory and battery life were introduced. A study reported a large number of insulin under-delivery events with the MiniMed (MIP 2001) pump due to both pump- and catheter-related problems and suggested this is a limitation of extended peritoneal insulin infusion from implanted pumps [60]. Implantable insulin pump devices were discontinued in 2007 [61].
The new generation external pumps, released in the 1990s, are comparatively small, compact, handy, and effective. These “smart pumps” have features such as built-in bolus calculators, personal computer interfaces, and alarms [62]. The currently popular insulin pump models on the global market are Medtronic MiniMed, OmniPod (Insulet), T:Slim (Tandem), DANA R (SOOIL), Cellnovo, Accu-Chek Solo Micropump (Roche), and Ypsomed [63].
In 2003, Medtronic introduced the first-ever “intelligent” insulin pump. The system comprises a MiniMed Paradigm 512 insulin pump and a Paradigm Link® blood glucose monitor, co-developed with BD. Here, BG readings from the glucometer are wirelessly and automatically transmitted to the insulin pump, and the required insulin doses were suggested by a Bolus Wizard calculator [64].
Insulin pumps are mainly used for insulin replacement in T1DM patients, but it has now been widely accepted by T2DM patients as well [65]. Diabetes management with CSII provides better glycemic and metabolic control (reduces HbA1c, glycemic variation, and hypoglycemia) in patients with diabetes [66,67,68]. A clinical trial, the Exploratory CSII Randomized Controlled Trial on Erectile Dysfunction in T2DM Patients (ECSIITED), conducted by our group, revealed the improved efficiency of CSII in the treatment of erectile dysfunction and diabetic peripheral neuropathy in T2DM patients [69]. Advantages of CSII over other devices are the reduction in all grades of hypoglycemia, BG levels, HbA1c, and glucose variations with a low daily insulin dosage. Overall, the use of insulin pumps effectively contributes to the patients’ quality of life. However, the major drawbacks associated with the infusion sets are that they often exhibit handling issues and can detach, leak, or cause skin irritability, thus compromising the convenient use of insulin pumps [70]. The advantages and disadvantages of insulin pumps over insulin pens and syringes are summarized in Table 1.
Patch Pumps
The limitations of the infusion set have led to the development of “patch pumps”: pumps that are free of infusion sets, small, lightweight, and attached to the skin through an adhesive. Patch pumps offer additional comfort and flexibility to users, especially while traveling. In 2011, Insulet introduced OmniPod, the first tubeless insulin pump. It comprises an integrated infusion set and automated inserter that converses wirelessly with an integrated BG meter. The Omnipod patch pump allows complete freedom to the users to engage in routine activities [71]. V-Go (Valeritas) and PAQ (CeQur) are specific simplified patch pump models available on the market [72]. In 2013, the second-generation Omnipod, which is smaller and more compact than its predecessor, was launched. This version of the patch pump has advanced features such as “human factor screens” and improvements in both correction and meal boluses for insulin dose calculation [73].
Continuous Intraperitoneal Insulin Infusion (CIPII)
The intraperitoneal route of insulin delivery has been investigated since the 1970s. Continuous intraperitoneal insulin infusion (CIPII) is intended to enable the infusion of insulin into the peritoneal cavity. The advantage of this method is that it more closely resembles the physiology than the other conventional therapies [74]. Two different technologies have been developed in CIPII: implanted intraperitoneal pumps such as MiniMed MIP2007C (Medtronic) and a percutaneous port attached to an external pump such as the Accu-Chek® Diaport system (Roche Diabetes Care). The MIP 2007C is implanted beneath the subcutaneous tissue in the lower abdomen, and from this subcutaneous pocket, the peritoneum is opened, and the tip of the catheter is carefully inserted and directed toward the liver. After implantation, the pump reservoir is refilled in the outpatient clinic with concentrated insulin transcutaneously at least every 3 months. The Accu-Chek® Diaport system enables infusion of insulin into the peritoneal cavity through an Accu-Chek insulin pump and an infusion set. CIPII has been proven as a viable option for T1D patients with skin problems and unable to securely or efficiently control their diabetes with subcutaneous insulin [75]. The limitations of this route of insulin administration include the invasive nature, cannula blockage, higher cost, portal-vein thrombosis, and peritoneal infection.
In 2007, Medtronic announced the worldwide termination of the implantable insulin pump.
The Diaport system has relatively few side effects and has the potential to be integrated into closed-loop systems for insulin delivery. Now less than 500 people worldwide are on an implantable insulin pump.
Sensor-Augmented Pump Therapy (SAP)
In 2006, MiniMed introduced the first integrated diabetes management system: the MiniMed Paradigm REAL-Time system insulin pump and CGM system. The introduction of real-time, sensor-augmented insulin pumps is considered a major step toward the development of “closed-loop” insulin delivery or an artificial pancreas (AP) [1]. The use of CGM sensors to control insulin delivery through pumps by adjusting the basal rate has turned CSII into a new form of therapy, SAP therapy [76]. The SAP platform integrates two independent technologies into a single system [1]. SAP therapy produces superior outcomes in reducing hypoglycemia and achieving glycemic control to conventional therapies [77, 78]. In 2009, Medtronic launched the MiniMed Veo System, with a Low Glucose Suspend feature that automatically halts insulin delivery when sensor glucose levels hit a preset low threshold. This device has been considered the first stepping stone to an AP system [79]. SAP therapy provides room for potential innovations, particularly focusing on fully “closed-loop systems.”
Benefits and Limitations of Pump Therapy
It is undebatable that insulin pump users have lower A1c levels and fewer hypoglycemic events. In addition, the pump offers more accurate dosing, avoids the need for multiple daily injections, and thus provides convenience and a flexible lifestyle. Another potential benefit is that the pumps can store a plethora of data that can be transmitted to computer programs or bolus insulin calculators and further analyzed to make insulin dose adjustments.
Potential downsides of pump therapy are technical problems associated with the infusion set and higher acquisition costs. Patients often experienced skin irritations and infections at the insertion sites. Technical issues such as kinking, bending, or crimping of inserted cannulas and leakage of infusion sets have also been reported [70]. Initial acquisition and total annual costs are high for pump therapy compared with MDI [80].
Bolus Calculator Apps
Bolus calculator/bolus advisor mobile apps are platforms for insulin dose calculation available in smartphones. These can function independently or can be integrated into pumps to calculate the accurate insulin dose by incorporating expected carbohydrate intake, measured blood glucose values, and previous insulin doses [81]. Carbohydrate counting using bolus calculator apps has been found to improve glycemic control in MDI-treated diabetes patients [82]. Diabetes: M, mySugr (Roche), and PredictBGL are some of the most used bolus calculator apps. Bolus wizards are built-in automated bolus calculators specific to insulin pumps for insulin dose recommendations. The use of bolus wizards has been associated with better glycemic control and treatment satisfaction [83]. The 2016 Endocrine Society Clinical Practice Guidelines have strongly encouraged patients to use suitably adjusted built-in bolus calculators in CSII to enhance glycemic control [52].
Artificial Pancreas
Since the conception of CSII, the prime motive has been to design an artificial pancreas that mimics exquisite sugar control with minimal human interference. An artificial pancreas or a “closed-loop” is a combination of progressive technologies to engage automation to obtain glycemic targets. Generally, AP links three devices: (1) a sensor like CGM that measures BG and sends data to a computer algorithm, (2) a control algorithm to analyze the data and calculate the required insulin dose, and (3) an insulin infusion pump to deliver insulin as per the computer instructions [84].
MiniMed 530G with an Enlite sensor has been recognized as a first-generation artificial pancreas device system with Threshold Suspend automation. This device was approved by the FDA in 2013 for the use of diabetes patients > 16 years of age [64]. Medtronic introduced the MiniMed 640G system in 2015, taking one step closer to the artificial pancreas system. This system has integrated smart features such as active insulin tracking, a bolus progress bar, and predictive battery life [79, 85].
Safety and efficacy studies have been conducted on the combinational use of the predictive low-glucose suspension algorithm (PLGM) (commercially, “SmartGuard technology”) with the MiniMed 640G insulin pump that automatically suspends insulin delivery based on the prediction of low glucose levels; it has been used since 2016 [86]. Recent studies suggested that sensor-augmented pump therapy with the predictive low-glucose suspension algorithm (SAPT-PLGM) leads to a potential reduction in the metrics of hypoglycemia and post-exercise nocturnal hypoglycemia compared with SAP therapy alone [87,88,89].
In 2017, the first hybrid closed-loop system, the MiniMed 670G insulin pump with a Guardian 3 sensor, was licensed by the FDA for T1D therapy of children 7 years and older. When in auto mode, it functions as a hybrid closed-loop system that automatically controls basal insulin delivery every 5 min based on the CGM values to hold BG levels tightly to the specific target [8]. These systems have been reported to improve glycemic targets [BG, HbA1c, time-in-range (TIR)] and reduce the incidence of nocturnal hypoglycemia to ensure better safety, treatment satisfaction, sleep quality, and cognition in T1D patients [88, 90, 91]. Insulet’s Omnipod Dash System, a CSII system comprising a tubeless, waterproof, Bluetooth wireless technology pump with a capacity of 200 units of U-100 insulin and an advanced personal diabetes manager (PDM) that regulates the pump, obtained FDA approval in 2018. This has been recognized as the only insulin pump certified for cyber and information security. This system is expected to be expanded as the Omnipod Horizon hybrid closed-loop system in the near future [92].
The DBLG1 hybrid closed-loop system (Diabeloop) comprising Dexcom G6 CGM, Kaleido’s patch insulin pump, and the Diabeloop decision-making algorithm received the CE marking, an essential standard for marketing in 2018. A study by Benhamou et al. reported that the use of the DBLG1 system was associated with an increase in TIR (68.5%) compared with SAP (59.4%) in adults with T1D. Procedures required for the FDA clearance and commercial rollout of this system are on track [93, 94]. In 2019, Medtronic started the clinical trials on the MiniMed 780G system, which has novel features including automatic correction boluses, Bluetooth connectivity, and remote software updates. The project aims to achieve a TIR > 80% and a modifiable BG target level down to 100 mg/dl [95].
Alternate Controller Enabled Infusion (ACE) Pumps
Another recent technology in this area has been the emergence of alternate controller-enabled (ACE) infusion pumps. Unlike the conventional stand-alone pumps, ACE pumps can be interoperable: used jointly with different components of diabetes technologies, permitting custom-made diabetes management for patients according to individual device preferences. The ACE insulin pump can be combined with automated insulin dosing (AID) systems, CGMs, BG meters, and other electronics. The FDA authorized the first interoperable t:Slim X2 insulin pump in 2019 for subcutaneous insulin delivery for children and adults with diabetes [96]. In 2020, the FDA approved a new-generation, interoperable, control-IQ artificial pancreas system (tandem diabetes). A clinical trial that reported that the use of the control-IQ AP system was associated with a greater percentage of TIR, over the use of SAP, paved way for this approval [91]. The slow pace of innovations and highly unaffordable cost have been considered the major limitations of these technologies.
Do-It-Yourself Artificial Pancreas (DIY-APS)
The emergence of closed-loop systems has been a breakthrough development in diabetes treatment. However, the clinical trials and regulatory procedures mandatory for the commercialization of the AP systems are very complex and time-consuming. Frustrated by the slow pace and unaffordability of innovations, patients with diabetes (PWD) and their families/caregivers gathered online under the hashtag ‘#WeAreNotWaiting’ in 2013 to share knowledge of the open-source hardware and software solutions. This event marked the beginning of the DIY-APS movement. A major dimension of the #WeAreNotWaiting initiative was that the tech-savvy diabetes enthusiasts started self-building their closed-loop systems, also known as ‘looping.’ These automated insulin delivery systems are generally known as a ‘Do-it-yourself’ artificial pancreas (DIY-APS) [97, 98]. There are three types of DIY-APS: OpenAPS, AndroidAPS, and Loop. The diabetes community shared DIY diabetes device-related projects on digital and social media platforms such as Facebook, Twitter, NightScout, and GitHub, which led to the convergence of these projects. In 2014, Dana Lewis, Scott Leibrand, and Ben West launched the OpenAPS project, the first DIY-APS that provided the instructions and outline of a DIY patient-built APS [99]. DIY-APS uses individually made unauthorized algorithms to convert CGM data and calculate insulin doses, FDA approved communication devices, and insulin pumps. Since it involves the use of unauthorized algorithms, these systems are not FDA approved, commercialized, or regularized. Another innovation in the DIY-APS evolution is “RileyLink,” designed by Pete Schwamb for his daughter Riley, who had T1D, in 2017. It is a translator device that enables easy communication between the insulin pump and iPhone. This device is considered more user-friendly, and it is easy to set up and to maintain the procedures [100]. Real-life experiences from patients and caregivers, anecdotal data, and published reports from selected cohorts have highlighted the clinal benefits and reductions in self-management burden with DIY-APS [101].
Bionic Pancreas (BP)
The “bionic pancreas” is a type of closed-loop system consisting of two infusion pumps (separately for insulin and glucagon) and connected to a CGM via a smartphone app. The first bionic pancreas, ‘iLet’ (Beta Bionics), exclusively for T1D treatment, was invented by Dr. Edward Damiano in 2015. In this system, automated dosing assessments of insulin and glucagon levels are made every 5 min based on the appraised CGM data. These data are transmitted to pumps to regulate insulin or glucagon delivery [102]. Previous studies in home-use and outpatient settings indicated better glycemic regulation and positive psychosocial impacts associated with the use of the bionic pancreas [103, 104]. Another study noted that the insulin-only mode of the iLet significantly increased TIR in adults with type 1 diabetes to 70.1% compared with 61.5% in usual care therapy [105]. Ekhlaspour et al., using a population of T1D patients in the home-use setting, reported that the insulin-only version of the bionic pancreas delivered similar safety and performance outcomes to the other ‘insulin-only’ systems [106]. The iLet BP was granted the ‘breakthrough device designation’ by the FDA in 2019 [107].
D-Dads
Making use of their first-hand experiences with the triumphs and challenges of diabetes management, many D-Dads, parents of children with diabetes, have become the flagbearers of patient-led innovations and movements in the arena. The credit for the invention of the bionic pancreas goes to Dr. Edward R. Damiano, a professor of biomedical engineering at Boston University. He designed a BP to achieve automation for constant monitoring and adjustments of BG levels for his son, David, who was diagnosed with T1D at 11 months. He is the founder and CEO of the Beta Bionics firm, conducting research trials on iLet BP [108]. Pete Schwamb, a software engineer, made path-breaking contributions in the field of diabetes technologies. Pete’s effort to gain access to the insulin pump data of his 6-year-old daughter, Riley, led to the development of RileyLink, a translator device used to communicate between the insulin pump and iPhone. Later, he developed the first iOS-based automated insulin delivery system, ‘loop,’ in collaboration with Nathan Racklyeft [109]. Bryan Mazlish, a Wall Street quantitative analyst and one of the co-founders of Bigfoot Biomedical, made a fully functional homebrew artificial pancreas to manage his son’s T1D. Being a hacker by profession, he has been recognized as a standard-bearer for the DIY-APS hacking mission [108]. Jeffrey Brewer, a past president of the Juvenile Diabetes Research Foundation (JDRF), also known as “the father of the artificial pancreas,” has initiated research projects on automated insulin delivery systems. Later, he co-founded Bigfoot Biomedical along with Bryan Mazlish to develop its own closed-loop system, the Bigfoot smartloop™ system [110]. John Costik, the father of a 4-year-old boy, Evan, who had T1D, designed a code to hack his son’s CGM, to upload the values into the cloud and remotely access those data using a web-based or android interface. He later made the code available as open source and commenced ‘Nightscout CGM in the Cloud Project’ for wider dissemination of the technology [111, 112]. Nightscout CGM in the Cloud was co-developed by Lane Desborough, D-Dad of Hayden. He was a chief engineer at Medtronic and was one of the advocates of the #WeAreNotWaiting movement. Lane was the first person to get involved in the DIY-APS movement from the industry and later co-founded Bigfoot Biomedical [113]. Howard Look and Steve McCanne are D-Dads to their respective daughters with T1D and pursuing a vision to bring about innovations to reduce the management burden of T1D through their cofounded non-profit organization, Tidepool. Tidepool is currently on a venture to release a regulated version of the DIY-APS in collaboration with Omnipod and Dexcom [114, 115].
Implanted Pancreas
The implanted artificial pancreas, a fully implantable insulin delivery device, is another novel AP technology under development at De Montfort University. It is a gel-based system that responds to BG variation by altering the insulin delivery rate. The performance of this system in glycemic control is well tested in a diabetic domestic pig [116].
Regardless of category, the goal of the AP system is to improve glycemic outcomes with less hypoglycemia. It reduces hourly management and human interference to enhance user acceptance and quality of life in diabetes patients. The next step of AP would be exploiting engineering integration and validating the prototype systems with subsequent studies in large outpatient settings [117].
Insulin Inhalers
Insulin inhalers allow patients to breathe in fine-inhalable insulin (pulmonary insulin) (either dry powder-based formulations or solution) into their lungs. The pulmonary route of insulin administration was closer to physiologic portal delivery and therefore the first substitute for the subcutaneous route of insulin delivery [16]. When introduced to the market in 2006, inhalable insulin was considered a significant innovation to address needle phobia and incorrect insulin injection techniques pertained to systemic insulin delivery methods. The effectiveness of inhalable insulin in diabetes treatment, especially for postprandial hyperglycemia, has already been proven [118]. The first inhalable insulin, Exubera (Pfizer), was approved by the FDA in 2006 for the treatment of T1D and T2D. However, the use of Exubera was associated with an increased risk of hypoglycemia. The product was withdrawn from the market in 2007 because of its high cost and dose inaccuracy [119, 120]. The only surviving candidate in this category is Afrezza, a rapid-acting Technosphere insulin powder (MannKind Corp.). Afrezza got FDA approval for prandial insulin therapy in 2014 [121]. The delivery system of Afrezza is small, handy, and displays the dose in units [122]. The use of Afrezza has provided significant glycemic control and reduction of hypoglycemia in T1D patients [123, 124]. The acceptance of inhalable insulins is further limited by insurance barriers, safety concerns, and competing products [122].
Jet Injectors
Another possible entrant to the market could be jet injectors, a type of syringe that dispenses insulin subcutaneously with the aid of a high-pressure air mechanism. Pioneer jet injector technology was introduced in the 1860s. Later, it was reintroduced in the 1940s as the ‘Hypospray,’ focusing on patients’ self-management of insulin. The US military designed a high-speed system, ‘Ped-O-Jet’ (Keystone Industries), in the category of a multiuse nozzle jet injector (MUNJI), in the 1950s for mass-vaccination programs. In 1997, the Ped-O-Jet was discontinued as a result of contamination issues raised with the use of MUNJI [125]. The new-generation, disposable-syringe jet injectors (DSJIs) with disposable dose chambers (insulin cartridge) and nozzles were launched in the 1990s. Even though the idea is not first hand to the market, the wider acceptance of these devices has been stalled by the cost, low absorption with the repeated use, and high contamination rates of the previous systems [126]. Needless to say, the jet injectors are a solution for patients with needle phobia [127]. Recent safety and feasibility studies have evaluated the treatment efficiency and pharmacokinetic and pharmacodynamic (PK-PD) profiles of the insulin administered by the new-generation jet injectors [127, 128].
Conclusion
In the past decade, there has been a high-speed evolution in diabetes technologies to improve the quality of life and to extend the longevity of subjects with diabetes. Though there were commendable developments in the currently available devices, many of those were prohibitively expensive. In addition, there were serious issues associated with cannula blockages, infusion set handling, Bluetooth connectivity, and user-friendliness. As the hunt for more accurate and user-friendly methods continues, advances in pumps, CGMs, and predictive algorithms can make the closed-loop system as physiologic as possible with > 90–95% TIR and the least time spent in hypoglycemia. Some of the promising experiences are shared by subjects using DIY-APS. The DIY revolution has prompted all the device manufacturers to introduce ACE pumps and compatible sensors. The ultimate dream is to develop an artificial pancreas capable of 100% TIR and 0% time below range and affordable to everyone. Although the mission demands enormous commitment and time, it has the potential to transform diabetes therapy.
References
Kesavadev J, Das AK, Unnikrishnan R, et al. Use of insulin pumps in India: suggested guidelines based on experience and cultural differences. Diabetes Technol Ther. 2010;12:823–31.
Home P, Riddle M, Cefalu WT, et al. Insulin therapy in people with type 2 diabetes: opportunities and challenges? Diabetes Care. 2014;37:1499–1508. https://care.diabetesjournals.org/content/37/6/1499.abstract.
Garg SK, Rewers AH, Akturk HK. Ever-increasing insulin-requiring patients globally. Diabetes Technol Ther. 2018;20:S21–S2424. https://doi.org/10.1089/dia.2018.0101.
Knutsen PG, Voelker CQ, Nikkel CC. Clinical insights into a new, disposable insulin delivery device. Diabetes Spectr. 2015;28:209–213. https://spectrum.diabetesjournals.org/content/28/3/209.abstract.
Banting FG, Best CH. The internal secretion of the pancreas. J Lab Clin Med. 1972;80:465–80.
Alcántara-Aragón V. Improving patient self-care using diabetes technologies. Ther Adv Endocrinol Metab. 2019;10:2042018818824215–2042018818824215. https://www.ncbi.nlm.nih.gov/pubmed/30728941.
Rex J, Jensen KH, Lawton SA. A review of 20 years’ experience with the NovoPen family of insulin injection devices. Clin Drug Investig. 2006;26:367–401.
Weaver KW, Hirsch IB. The hybrid closed-loop system: evolution and practical applications. Diabetes Technol Ther. 2018;20:S216–S223223.
Group UKPDS (UKPDS). Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352:837–53.
Group DC and CTR. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–86.
Pearson TL. Practical aspects of insulin pen devices. J Diabetes Sci Technol. 2010;4:522–531. https://www.ncbi.nlm.nih.gov/pubmed/20513316.
Technology D. Standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S77–88.
BD. Diabetes products. BD diabetes prod. https://www.bd.com/en-uk/products/diabetes/diabetes-products (2019). Accessed 21 Nov 2019.
Nordisk N. History. https://www.novonordisk.com/media/photo-library-02/history.html (2019). Accessed 21 Nov 2019.
Fry A. Insulin delivery device technology 2012: where are we after 90 years? J Diabetes Sci Technol. 2012;6:947–53.
Shah RB, Patel M, Maahs DM, Shah VN. Insulin delivery methods: past, present and future. Int J Pharm Investig. 2016;6:1–9.
Exchange Supplies. The history of injecting, and the development of the syringe. https://www.exchangesupplies.org/article_history_of_injecting_and_development_of_the_syringe.php. Accessed 21 Nov 2019.
Bloom A. Syringes for diabetics. Br Med J (Clin Res Ed). 1985;290:727–728. https://pubmed.ncbi.nlm.nih.gov/3918730.
Hall GH, Thompson CJ, Palmer A. Danger of dead space in U100 insulin syringes. Br Med J (Clin Res Ed). 1984;288:284–5.
Aronson R, Gibney MA, Oza K, Berube J, Kassler-Taub K, Hirsch L. Insulin pen needles: effects of extra-thin wall needle technology on preference, confidence, and other patient ratings. Clin Ther. 2013;35(923.e4):933.e4.
BD. BD VeoTM insulin syringes with BD Ultra-FineTM 6mm × 31G needle. https://www.bd.com/en-us/offerings/capabilities/diabetes-care/insulin-syringes/bd-veo-insulin-syringe-with-ultra-fine-6mm-needle (2020). Accessed 15 Feb 2020.
Shaw KF, Valdez CA. Development and implementation of a U-500 regular insulin program in a federally qualified health center. Clin Diabetes. 2017;35:162–167. https://pubmed.ncbi.nlm.nih.gov/28761218.
Zambanini A, Newson RB, Maisey M, Feher MD. Injection related anxiety in insulin-treated diabetes. Diabetes Res Clin Pract. 1999;46:239–46.
Fu AZ, Qiu Y, Radican L. Impact of fear of insulin or fear of injection on treatment outcomes of patients with diabetes. Curr Med Res Opin. 2009;25:1413–20.
Khan AM, Alswat KA. Benefits of using the i-Port system on insulin-treated patients. Diabetes Spectr. 2019;32:30–5.
Novo Nordisk Blue sheet. Quarterly perspective on diabetes and chronic diseases. Novo Nord. Blue sheet. https://www.press.novonordisk-us.com/bluesheet-issue2/downloads/NovoNordisk_Bluesheet_Newsletter.pdf (2010). Accessed 21 Nov 2019.
Novo Nordisk History. Novo Nord. https://www.novonordisk.co.in/content/dam/Denmark/HQ/aboutus/documents/HistoryBook_UK.pdf (2020). Accessed 15 Feb 2020.
Dunne T, Whitaker D. Prefilled insulin syringes. Anaesthesia. 2016;71:349–50. https://doi.org/10.1111/anae.13389.
Singh R, Samuel C, Jacob JJ. A comparison of insulin pen devices and disposable plastic syringes - simplicity, safety, convenience and cost differences. Eur Endocrinol. 2018;14:47–51. https://www.ncbi.nlm.nih.gov/pubmed/29922352.
Guerci B, Chanan N, Kaur S, Jasso-Mosqueda JG, Lew E. Lack of treatment persistence and treatment nonadherence as barriers to glycaemic control in patients with type 2 diabetes. Diabetes Ther. 2019;10:437–49.
Hyllested-Winge J, Sparre T, Pedersen LK. NovoPen Echo(®) insulin delivery device. Med Devices. 2016;9:11–18. https://www.ncbi.nlm.nih.gov/pubmed/26793007.
Ignaut DA, Opincar M, Lenox S. FlexPen and KwikPen prefilled insulin devices: a laboratory evaluation of ergonomic and injection force characteristics. J Diabetes Sci Technol. 2008;2:533–7.
Davis EM, Sexson EL, Spangler ML, Foral PA. An evaluation of prefilled insulin pens: a focus on the Next Generation FlexPen(®). Med Devices. 2010;3:41–50. https://pubmed.ncbi.nlm.nih.gov/22915920.
Wielandt JO, Niemeyer M, Hansen MR, Bucher D, Thomsen NB. FlexTouch: a prefilled insulin pen with a novel injection mechanism with consistent high accuracy at low-(1 U), medium-(40 U), and high-(80 U) dose settings. J Diabetes Sci Technol 2011;5:1195–1199. https://pubmed.ncbi.nlm.nih.gov/22027317.
Sanofi. Sanofi launches specially designed ‘made in India’ re-usable insulin pen-AllStarTM Press Relaese. https://www.sanofi.in/-/media/Project/One-Sanofi-Web/Websites/Asia-Pacific/Sanofi-IN/Home/Media/press-release/2012/Sanofi-launches-specially-designed-made-in-India---Re-usable-insulin-pen---AllStar.pdf?la=en (2012). Accessed 15 Feb 2020.
Han DH. Humalog Junior KwikPen soon to be available. https://www.empr.com/home/news/humalog-junior-kwikpen-soon-to-be-available/ (2017). Accessed 16 Feb 2020.
Healthworld.com. Eli Lilly launches 200 U/mL pre-filled insulin pen. Econ Times. https://health.economictimes.indiatimes.com/news/pharma/eli-lilly-launches-200u/ml-pre-filled-insulin-pen/57685481 (2017). Accessed 19 Mar 2020.
Gudiksen N, Hofstätter T, Rønn BB, Sparre T. FlexTouch: an insulin pen-injector with a low activation force across different insulin formulations, needle technologies, and temperature conditions. Diabetes Technol Ther. 2017;19:603–607. https://pubmed.ncbi.nlm.nih.gov/28704062.
Pohlmeier H, Berard L, Brulle-Wohlhueter C, et al. Ease of use of the insulin glargine 300 U/mL pen injector in insulin-naïve people with type 2 diabetes. J Diabetes Sci Technol. 2017;11:263–269. https://pubmed.ncbi.nlm.nih.gov/27664062.
Chawla R, Shunmugavelu M, Bhansali A, et al. Practical guidance on insulin injection practice in diabetes self-management in the Indian setting: an expert consensus statement. 2019. pp. 176–194. https://journals.viamedica.pl/clinical_diabetology/article/view/DK.2019.0013.
Whooley S, Briskin T, Gibney MA, Blank LR, Berube J, Pflug BK. Evaluating the user performance and experience with a re-engineered 4 mm × 32G pen needle: a randomized trial with similar length/gauge needles. Diabetes Ther. 2019;10:697–712.
Olsen BS, Lilleøre SK, Korsholm CN, Kracht T. Novopen Echo® for the delivery of insulin: a comparison of usability, functionality and preference among pediatric subjects, their parents, and health care professionals. J Diabetes Sci Technol. 2010;4:1468–1475. https://pubmed.ncbi.nlm.nih.gov/21129343.
DiaTribeLearn. NovoPen Echo: a child-friendly variation of the insulin pen. https://diatribe.org/issues/20/new-now-next/3 (2010). Accessed 16 Feb 2020.
Review EP. Novo Nordisk’s award-winning NovoPen® 5 with easy-to-use memory function approved in China. https://www.europeanpharmaceuticalreview.com/news/17561/novo-nordisks-award-winning-novopen-5-with-easy-to-use-memory-function-approved-in-china/ (2013). Accessed 16 Feb 2020.
Bailey TS, Stone JY. A novel pen-based Bluetooth-enabled insulin delivery system with insulin dose tracking and advice. Expert Opin Drug Deliv. 2017;14:697–703.
Gildon BW. InPen smart insulin pen system: product review and user experience. Diabetes Spectr. 2018;31:354–358. https://spectrum.diabetesjournals.org/content/31/4/354.abstract.
Freed S. New smart pens hoped to change the way we treat diabetes. Diabetes Control. https://www.diabetesincontrol.com/new-smart-pens-hoped-to-change-the-way-we-treat-diabetes/ (2020). Accessed 2 Mar 2020.
DiaTribeLearn. NovoPen 6 and NovoPen Echo Plus: connected insulin pens to launch in early 2019. https://diatribe.org/novopen-6-and-novopen-echo-plus-connected-insulin-pens-launch-early-2019 (2018). Accessed 16 Feb 2020.
Sangave NA, Aungst TD, Patel DK. Smart connected insulin pens, caps, and attachments: a review of the future of diabetes technology. Diabetes Spectr. 2019;32:378–384. https://spectrum.diabetesjournals.org/content/32/4/378.abstract.
MedicalNewsToday. What are insulin pens and how do we use them? https://www.medicalnewstoday.com/articles/316607 (2019). Accessed 27 Mar 2019.
Ewen M, Joosse H-J, Beran D, Laing R. Insulin prices, availability and affordability in 13 low-income and middle-income countries. BMJ Glob Health. 2019;4:e001410. https://gh.bmj.com/content/4/3/e001410.abstract.
Peters AL, Ahmann AJ, Battelino T, et al. Diabetes technology-continuous subcutaneous insulin infusion therapy and continuous glucose monitoring in adults: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:3922–37.
Medtronic. What is insulin pump therapy. Medtronic. https://www.medtronicdiabetes.com/treatments/insulin-pump-therapy. Accessed 17 Feb 2020.
Al-Tabakha MM, Arida AI. Recent challenges in insulin delivery systems: a review. Indian J Pharm Sci. 2008;70:278–86.
Al Hayek AA, Robert AA, Babli S, Almonea K, Al Dawish MA. Fear of self-injecting and self-testing and the related risk factors in adolescents with type 1 diabetes: a cross-sectional study. Diabetes Ther. 2017;8:75–83. https://www.ncbi.nlm.nih.gov/pubmed/27995595.
Cobelli C, Renard E, Kovatchev B. Artificial pancreas: past, present, future. Diabetes. 2011;60:2672–2682. https://www.ncbi.nlm.nih.gov/pubmed/22025773.
Allen N, Gupta A. Current diabetes technology: striving for the artificial pancreas. Diagnostics. 2019;9:31. https://pubmed.ncbi.nlm.nih.gov/30875898.
SOOIL. SOOIL history. https://www.sooil.com/eng/about/history.php (2020). Accessed 2 Mar 2020.
Duckworth WC, Saudek CD, Henry RR. Why intraperitoneal delivery of insulin with implantable pumps in NIDDM? Diabetes. 1992;41:657–661. https://diabetes.diabetesjournals.org/content/41/6/657.abstract.
Renard E, Bouteleau S, Jacques-Apostol D, et al. Insulin underdelivery from implanted pumps using peritoneal route: determinant role of insulin pump compatibility. Diabetes Care. 1996;19:812–817. https://care.diabetesjournals.org/content/19/8/812.abstract.
Hoskins M. Implantable insulin pumps are near extinction, but still alive... Diabetes Mine. https://www.healthline.com/diabetesmine/implantable-insulin-pumps (2017). Accssed 20 Mar 2020.
Skyler JS, Ponder S, Kruger DF, Matheson D, Parkin CG. Is there a place for insulin pump therapy in your practice? Clin Diabetes. 2007;25:50–6.
Magennis C. The different types of insulin pumps available in 2019. https://www.dreambigtravelfarblog.com/blog/types-of-insulin-pumps (2019). Accssed 16 Feb 2020.
Medtronic. Innovation milestones. https://www.medtronicdiabetes.com/about-medtronic-innovation/milestone-timeline (2020). Accssed 16 Feb 2020.
Hieronymus Laura GS. Insulin delivery devices. https://www.diabetesselfmanagement.com/diabetes-resources/tools-tech/insulin-delivery-devices/ (2019). Accssed 22 Nov 2019.
Pickup JC, Reznik Y, Sutton AJ. Glycemic control during continuous subcutaneous insulin infusion versus multiple daily insulin injections in type 2 diabetes: individual patient data meta-analysis and meta-regression of randomized controlled trials. Diabetes Care. 2017;40:715–22.
Kesavadev J, Shankar A, Sadasrian Pillai PB, et al. CSII as an alternative therapeutic strategy for managing type 2 diabetes: adding the Indian experience to a global perspective. Curr Diabetes Rev. 2016;12:312–4.
Maiorino MI, Bellastella G, Casciano O, et al. The effects of subcutaneous insulin infusion versus multiple insulin injections on glucose variability in young adults with type 1 diabetes: the 2-year follow-up of the observational METRO study. Diabetes Technol Ther. 2018;20:117–26. https://doi.org/10.1089/dia.2017.0334.
Kesavadev J, Sadasivan Pillai PB, Shankar A, et al. Exploratory CSII randomized controlled trial on erectile dysfunction in T2DM patients (ECSIITED). J Diabetes Sci Technol. 2018;12(6):1252–3.
Heinemann L, Krinelke L. Insulin infusion set: the Achilles heel of continuous subcutaneous insulin infusion. J Diabetes Sci Technol. 2012;6:954–964. https://www.ncbi.nlm.nih.gov/pubmed/22920824.
Heinemann L, Waldenmaier D, Kulzer B, Ziegler R, Ginsberg B, Freckmann G. Patch pumps: are they all the same? J Diabetes Sci Technol. 2019;13:34–40. https://www.ncbi.nlm.nih.gov/pubmed/30132698.
Ginsberg BH. Patch pumps for insulin. J Diabetes Sci Technol. 2019;13:27–33. https://pubmed.ncbi.nlm.nih.gov/30070604.
DiaTribeLearn. Insulet’s second generation omnipod patch pump approved by FDA. https://diatribe.org/issues/50/new-now-next/1 (2012). Accessed 16 Feb 2020.
Garcia-Verdugo R, Erbach M, Schnell O. A new optimized percutaneous access system for CIPII. J Diabetes Sci Technol. 2017;11:814–21.
Gimenez M, Purkayajtha S, Moscardo V, Conget I, Oliver N. Intraperitoneal insulin therapy in patients with type 1 diabetes. Does it fit into the current therapeutic arsenal? Endocrinol diabetes y Nutr. 2018;65(3):182–4.
Steineck I, Ranjan A, Nørgaard K, Schmidt S. Sensor-augmented insulin pumps and hypoglycemia prevention in type 1 diabetes. J Diabetes Sci Technol. 2017;11:50–58. https://www.ncbi.nlm.nih.gov/pubmed/28264173.
Matsuoka A, Hirota Y, Urai S, et al. Effect of switching from conventional continuous subcutaneous insulin infusion to sensor augmented pump therapy on glycemic profile in Japanese patients with type 1 diabetes. Diabetol Int. 2018;9:201–207. https://www.ncbi.nlm.nih.gov/pubmed/30603368.
Oviedo S, Contreras I, Bertachi A, et al. Minimizing postprandial hypoglycemia in type 1 diabetes patients using multiple insulin injections and capillary blood glucose self-monitoring with machine learning techniques. Comput Methods Programs Biomed. 2019;178:175–180. https://www.ncbi.nlm.nih.gov/pubmed/31416546.
Medtronic. Innovation milestones. https://www.medtronicdiabetes.com/about-medtronic-innovation/milestone-timeline (2020). Accessed 11 Feb 2020.
Toresson Grip E, Svensson A-M, Miftaraj M, et al. Real-world costs of continuous insulin pump therapy and multiple daily injections for type 1 diabetes: a population-based and propensity-matched cohort from the swedish national diabetes register. Diabetes Care. 2019;42:545–552. https://care.diabetesjournals.org/content/42/4/545.abstract.
Huckvale K, Adomaviciute S, Prieto JT, Leow MK-S, Car J. Smartphone apps for calculating insulin dose: a systematic assessment. BMC Med. 2015;13:106. https://pubmed.ncbi.nlm.nih.gov/25943590.
Siavash M, Taherian M, Khorasgani MA. Efficacy of bolus insulin calculation by a mobile-based bolus advisor: an open label clinical trial. J Res Med Sci. 2015;20:1064–1069. https://pubmed.ncbi.nlm.nih.gov/26941810.
Shashaj B, Busetto E, Sulli N. Benefits of a bolus calculator in pre- and postprandial glycaemic control and meal flexibility of paediatric patients using continuous subcutaneous insulin infusion (CSII). Diabet Med. 2008;25:1036–42.
Story of discovery—artificial pancreas for managing type 1 diabetes: cutting-edge technology 50 years in the making. Natl Inst Diabetes Dig Kidney Dis. 2017. https://www.niddk.nih.gov/news/archive/2017/story-discovery-artificial-pancreas-managing-type1-diabetes.
Medtronic. Minimed TM 640G insulin pump system. Medtronic. https://www.medtronic-diabetes.com.au/products/minimed-640g-system (2020). Accessed 2 Mar 2020.
Biester T, Kordonouri O, Holder M, et al. “Let the Algorithm Do the Work”: reduction of hypoglycemia using sensor-augmented pump therapy with predictive insulin suspension (SmartGuard) in pediatric type 1 diabetes patients. Diabetes Technol Ther. 2017;19:173–182. https://www.ncbi.nlm.nih.gov/pubmed/28099035.
Petruzelkova L, Pickova K, Sumnik Z, Soupal J, Obermannova B. Effectiveness of SmartGuard technology in the prevention of nocturnal hypoglycemia after prolonged physical activity. Diabetes Technol Ther. 2017;19:299–304.
Garg SK, Weinzimer SA, Tamborlane W V, et al. Glucose outcomes with the in-home use of a hybrid closed-loop insulin delivery system in adolescents and adults with type 1 diabetes. Diabetes Technol Ther. 2017;19:155–163. https://www.ncbi.nlm.nih.gov/pubmed/28134564.
Gómez AM, Henao DC, Taboada LB, et al. Impact of sensor-augmented pump therapy with predictive low-glucose management on hypoglycemia and glycemic control in patients with type 1 diabetes mellitus: 1-year follow-up. Diabetes Metab Syndr. 2019;13:2625–2631. https://www.ncbi.nlm.nih.gov/pubmed/31405686.
Sharifi A, De Bock MI, Jayawardene D, et al. Glycemia, treatment satisfaction, cognition, and sleep quality in adults and adolescents with type 1 diabetes when using a closed-loop system overnight versus sensor-augmented pump with low-glucose suspend function: a randomized crossover study. Diabetes Technol Ther. 2016;18:772–783. https://www.ncbi.nlm.nih.gov/pubmed/27835037.
Brown SA, Kovatchev BP, Raghinaru D, et al. Six-month randomized, multicenter trial of closed-loop control in type 1 diabetes. N Engl J Med. 2019;381:1707–17. https://doi.org/10.1056/NEJMoa1907863.
Insulet’s Omnipod® HorizonTM Hybrid closed-loop system improves glycemic control in patients as young as two years old with type 1 diabetes. Insul Corp https://www.biospace.com/article/releases/insulet-s-omnipod-horizon-hybrid-closed-loop-system-improves-glycemic-control-in-patients-as-young-as-two-years-old-with-type-1-diabetes/ (2019). Accessed 2 Mar 2020.
Crabtree TSJ, Choudhary P, Hammond P, Lumb A, McLay A, Wilmot EG. Health-care professional opinions of DIY artificial pancreas systems in the UK. Lancet Diabetes Endocrinol. 2020;8:186–7. https://doi.org/10.1016/S2213-8587(19)30417-6.
Benhamou P-Y, Franc S, Reznik Y, et al. Closed-loop insulin delivery in adults with type 1 diabetes in real-life conditions: a 12-week multicentre, open-label randomised controlled crossover trial. Lancet Digit Health. 2019;1:e17–25. https://doi.org/10.1016/S2589-7500(19)30003-2.
DiaTribeLearn. ADA 2019: day 2 highlights. Diatribe Learn. https://diatribe.org/ada-2019-day-2-highlights (2019). Accessed 2 Mar 2020.
FDA. FDA authorizes first interoperable insulin pump intended to allow patients to customize treatment through their individual diabetes management devices. FDA. https://www.fda.gov/news-events/press-announcements/fda-authorizes-first-interoperable-insulin-pump-intended-allow-patients-customize-treatment-through (2019). Accessed 20 Jan 2020.
Omer T. Empowered citizen ‘health hackers’ who are not waiting. BMC Med. 2016;14:118. https://doi.org/10.1186/s12916-016-0670-y.
Marshall DC, Holloway M, Korer M, Woodman J, Brackenridge A, Hussain S. Do-it-yourself artificial pancreas systems in type 1 diabetes: perspectives of two adult users, a caregiver and three physicians. Diabetes Ther. 2019;10:1553–644. https://doi.org/10.1007/s13300-019-00679-y.
Lewis DM. Do-it-yourself artificial pancreas system and the openAPS movement. Endocrinol Metab Clin N Am. 2020;49:203–13.
Mine D. Homegrown closed loop technology: mom connects to RileyLink. https://www.healthline.com/diabetesmine/homegrown-diabetes-tool-rileylink#1 (2017). Accessed 17 Feb 2020.
Lewis D, Leibrand S. Real-world use of open source artificial pancreas systems. J Diabetes Sci Technol. 2016;10:1411. https://doi.org/10.1177/1932296816665635.
Bux Rodeman K, Hatipoglu B. Beta-cell therapies for type 1 diabetes: transplants and bionics. Cleve Clin J Med. 2018;85:931–937. https://www.ncbi.nlm.nih.gov/pubmed/30526754.
El-Khatib FH, Balliro C, Hillard MA, et al. Home use of a bihormonal bionic pancreas versus insulin pump therapy in adults with type 1 diabetes: a multicentre randomised crossover trial. Lancet. 2017;389:369–380. https://www.ncbi.nlm.nih.gov/pubmed/28007348.
Russell SJ, El-Khatib FH, Sinha M, et al. Outpatient glycemic control with a bionic pancreas in type 1 diabetes. N Engl J Med. 2014;371:313–325. https://www.ncbi.nlm.nih.gov/pubmed/24931572.
Jafri RZ, Balliro CA, Sherwood J, et al. 77-OR: first human study testing the ilet, a purpose-built bionic pancreas platform. Diabetes. 2019;68:77-OR. https://diabetes.diabetesjournals.org/content/68/Supplement_1/77-OR.abstract.
Ekhlaspour L, Nally LM, El-Khatib FH, et al. Feasibility studies of an insulin-only bionic pancreas in a home-use setting. J Diabetes Sci Technol. 2019;13:1001–7.
JDRF. FDA grants breakthrough device status: iLet bionic pancreas. https://www.jdrf.org/blog/2019/12/23/fda-grants-breakthrough-device-status-ilet-bionic-pancreas/ (2019).
Idlebrook C. The diabetes dads behind 3 type 1 breakthroughs. Insul. Nation. https://insulinnation.com/research/the-diabetes-dads-behind-3-type-1-breakthroughs/ (2015). Accessed 2 Mar 2020.
Racklyeft N. The history of Loop and LoopKit reflecting on the past in celebration of version 1.0. Medium. https://medium.com/@loudnate/the-history-of-loop-and-loopkit-59b3caf13805 (2016). Accessed 2 Mar 2020
Bevan A. “Not Good Enough”: how one dad led the change in diabetes devices through grassroots research and collaboration [Internet]. glu. https://myglu.org/articles/not-good-enough-how-one-dad-led-the-change-in-diabetes-devices-through-grassroots-research-and-collaboration (2017). Accessed 2 Mar 2020.
White K, Gebremariam A, Lewis D, et al. Motivations for participation in an online social media community for diabetes. J Diabetes Sci Technol. 2018;12:712–718. https://www.ncbi.nlm.nih.gov/pubmed/29310448.
Gavrila V, Garrity A, Hirschfeld E, Edwards B, Lee JM. Peer support through a diabetes social media community. J Diabetes Sci Technol. 2019;13:493–497. https://www.ncbi.nlm.nih.gov/pubmed/30600704.
Advancing Safety in Health Technology. In profile: lane Desborough. Adv. Saf. Heal. Technol. https://www.aami.org/news-resources/articledetail.aspx?ItemNumber=2536 (2015). Accessed 2 Mar 2020.
Glu. An interview with Tidepool CEO howard look. glu. https://myglu.org/articles/an-interview-with-tidepool-ceo-howard-look (2014). Accessed 2 Mar 2020.
Snider C. Tidepool loop, one year in: a development update. Tidepool. https://www.tidepool.org/blog/tidepool-loop-development-update (2020). Accessed 21 Feb 2020.
Taylor MJ, Gregory R, Tomlins P, Jacob D, Hubble J, Sahota TS. Closed-loop glycaemic control using an implantable artificial pancreas in diabetic domestic pig (Sus scrofa domesticus). Int J Pharm. 2016;500:371–378. https://www.ncbi.nlm.nih.gov/pubmed/26691655.
Peyser T, Dassau E, Breton M, Skyler JS. The artificial pancreas: current status and future prospects in the management of diabetes. Ann N Y Acad Sci. 2014;1311:102–123. https://www.ncbi.nlm.nih.gov/pubmed/24725149.
Santos Cavaiola T, Edelman S. Inhaled insulin: a breath of fresh air? A review of inhaled insulin. Clin Ther. 2014;36:1275–89.
Oleck J, Kassam S, Goldman JD. Commentary: why was inhaled insulin a failure in the market? Diabetes Spectr. 2016;29:180–184. https://pubmed.ncbi.nlm.nih.gov/27574374.
Bailey CJ, Barnett AH. Why is Exubera being withdrawn? BMJ Br Med J. 2007;335:1156 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2099527/.
Heinemann L, Baughman R, Boss A, Hompesch M. Pharmacokinetic and pharmacodynamic properties of a novel inhaled insulin. J Diabetes Sci Technol. 2017;11:148–56.
Oleck J, Kassam S, Goldman JD. Commentary: why was inhaled insulin a failure in the market? Diabetes Spectr. 2016;29:180–184. https://spectrum.diabetesjournals.org/content/29/3/180.abstract.
Seaquist ER, Blonde L, McGill JB, et al. Hypoglycaemia is reduced with use of inhaled Technosphere((R)) insulin relative to insulin aspart in type 1 diabetes mellitus. Diabet Med. 2019;37(5):752–9.
Akturk HK, Snell-Bergeon JK, Rewers A, et al. Improved postprandial glucose with inhaled technosphere insulin compared with insulin aspart in patients with type 1 diabetes on multiple daily injections: the STAT study. Diabetes Technol Ther. 2018;20:639–47.
Papania MJ, Zehrung D, Jarrahian C. Technologies to improve immunization. In: Plotkin SA, Orenstein WA, Offit PA, Edwards KMBT-PV (Seventh E, editors). Elsevier; 2018. pp. 1320.e17–1353.e17. https://www.sciencedirect.com/science/article/pii/B9780323357616000687.
Al-Tabakha M. Recent advances and future prospects of non-invasive insulin delivery systems. Int J Appl Pharm. 2019;11:16–24.
Guo L, Xiao X, Sun X, Qi C. Comparison of jet injector and insulin pen in controlling plasma glucose and insulin concentrations in type 2 diabetic patients. Medicine. 2017;96:e5482.
Hu J, Shi H, Zhao C, et al. Lispro administered by the QS-M needle-free jet injector generates an earlier insulin exposure. Expert Opin Drug Deliv. 2016;13:1203–7.
Acknowledgements
Funding
No funding or sponsorship was received for the publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
Jothydev Kesavadev, Banshi Saboo, Meera B. Krishna and Gopika Krishnan have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Digital Features
To view digital features for this article go to https://doi.org/10.6084/m9.figshare.12199748.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Kesavadev, J., Saboo, B., Krishna, M.B. et al. Evolution of Insulin Delivery Devices: From Syringes, Pens, and Pumps to DIY Artificial Pancreas. Diabetes Ther 11, 1251–1269 (2020). https://doi.org/10.1007/s13300-020-00831-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-020-00831-z