Abstract
Introduction
Patients with diabetes and familial hypercholesterolaemia (FH) are at very high risk of cardiovascular events, but rates of FH detection are very low in most countries, including Bulgaria. Given the lack of relevant data in the literature, we conducted a retrospective observational study to (1) identify individuals with previously undiagnosed FH among patients being treated at Bulgarian diabetes centres, and (2) gain insight into current management and attainment of low-density lipoprotein cholesterol (LDL-C) goals in such patients.
Methods
From a database of diabetes centres across Bulgaria we retrieved medical records from patients aged ≥ 18 years with type 1/2 diabetes mellitus (T1DM/T2DM) who were being treated with insulin/insulin analogues, dipeptidyl peptidase 4 inhibitors, glucagon-like peptide 1 receptor agonists and/or sodium-glucose co-transporter-2 inhibitors. Patients with FH (Dutch Lipid Clinic Network score ≥ 3) were identified, and their data analyzed (lipid-modifying therapy (LMT), diabetes treatment, cardiovascular events and glycaemic and lipid parameters).
Results
A total of 450 diabetic patients with FH (92.0% with T2DM; 52.4% receiving insulin/insulin analogues) were included in the analysis. LMT consisted of statin monotherapy (86% of patients; 18% receiving high-intensity statin monotherapy), statin-based combination therapy (13%) or fenofibrate (< 1%). Median LDL-C was 4.4 mmol/L. Although 30% of patients had a glycated haemoglobin level of ≤ 7%, only one patient (< 1%) achieved the LDL-C target recommended in 2016 European guidelines for very high-risk patients (< 1.8 mmol/L). Previous cardiovascular events were documented in 40% of patients.
Conclusion
To our knowledge, this is the first study to specifically explore lipid target achievement in diabetic patients with FH. In this preselected Bulgarian population, < 1% of patients achieved the 2016 European guideline-defined LDL-C target. These data highlight the importance of identifying FH in diabetic patients as early as possible so that they can receive appropriate treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Patients with diabetes and familial hypercholesterolaemia (FH) are at very high risk of cardiovascular events due to multiple comorbid risk factors. |
Since published data are lacking, the aim of this retrospective observational study was to (1) identify individuals with previously undiagnosed FH among patients attending diabetes centres across Bulgaria and (2) gain insight into the management of these patients. |
What was learned from the study? |
To our knowledge, this is the first study to specifically evaluate lipid target achievement in diabetic patients with FH. |
Only one patient of the 450 included in the analysis (< 1%) achieved the 2016 LDL-C target recommended by The European Society of Cardiology/European Atherosclerosis Society for very high-risk patients (< 1.8 mmol/L). |
These data highlight the importance of identifying underlying FH in diabetic patients so that they can receive appropriate treatment. |
Introduction
Atherosclerotic cardiovascular disease (ASCVD) is the leading cause of death in patients with diabetes mellitus (DM) [1]. Indeed, those with type 1 or type 2 DM (T1DM or T2DM) have an approximately twofold higher risk of both myocardial infarction and stroke than nondiabetic individuals, as shown by a meta-analysis of 102 prospective studies conducted by the Emerging Risk Factors Collaboration [2]. Addressing major risk factors, including dyslipidaemia and hypertension, as well as the disturbed carbohydrate metabolism, is key to reducing the risk of CVD events in diabetic patients [3].
Reducing elevated total cholesterol (TC), non-high-density lipoprotein cholesterol (non-HDL-C) and, most importantly, low-density lipoprotein cholesterol (LDL-C), via lipid-modifying therapy (LMT), lowers the risk of CV events [4,5,6]. The degree of risk reduction is proportional to the degree of LDL-C reduction [7], and the European Society of Cardiology/European Atherosclerosis Society (ESC/EAS) have set stringent LDL-C goals for patients with dyslipidaemia [8, 9]. However, it is well established that a substantial proportion of patients do not manage to achieve these goals despite receiving LMT [8,9,10,11].
The presence of undiagnosed familial hypercholesterolaemia (FH) is a potential reason for failure to attain guideline lipid targets. Characterized by very high levels of LDL-C and early CVD, this disorder is caused by mutations in genes governing the LDL pathway, including the LDL-receptor (LDLR), apolipoprotein B or proprotein convertase subtilisin/kexin type 9 (PCSK9). While reported prevalences of FH in various populations range from approximately 1:500 to 1:200, detection rates are very low in most countries [12, 13]. In Bulgaria, FH has only recently (in 2017) been added to the list of International Statistical Classification of Diseases and Related Health Problems (ICD) codes for diseases reimbursed with public funds. The EUROASPIRE IV survey estimated the age-standardized prevalence of potential FH in coronary patients in Bulgaria to be 9% (3.7–14.2%) [14]. It is important that individuals with FH are identified as early as possible and treated appropriately, since if left untreated, they are estimated to have an up to eightfold higher CVD risk versus unaffected relatives [15]. The odds of developing CVD have been reported to be threefold higher in diabetic patients with FH versus nondiabetic patients with FH [16] and 22-fold higher in mutation-positive FH patients with LDL-C ≥ 190 mg/dL (4.91 mmol/L) versus non-FH individuals with LDL-C < 130 mg/dL (3.36 mmol/L) [17].
To date, no real-life data on the management of FH in diabetes populations are available in the literature. Moreover, healthcare data from Eastern Europe are somewhat limited, reflecting a general lack of patient registries and limited access to public/health insurance data. There is no registry of diabetic patients in Bulgaria. Accordingly, we conducted a retrospective observational study to (1) identify individuals with previously undiagnosed FH among patients being treated at Bulgarian diabetes centres, and (2) gain insight into current management and attainment of ESC/EAS-defined LDL-C goals in such patients.
Methods
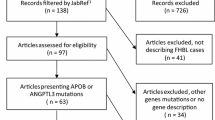
We reviewed electronic medical records from a database of Bulgarian diabetes centres that routinely treat patients with diabetes and are authorized by the National Health Insurance Fund to prescribe insulin, insulin analogues, dipeptidyl peptidase 4 (DPP4) inhibitors, glucagon-like peptide 1 receptor agonists (GLP-1 RA) and sodium-glucose co-transporter-2 (SGLT2) inhibitors. Patient records were screened to identify those with pre-treatment LDL-C levels of ≥ 4.1 mmol/L and/or TC levels of ≥ 8 mmol/L, and Dutch Lipid Clinic Network (DLCN) criteria were applied to the retrieved records to identify patients with FH (see study flow diagram in Electronic Supplementary Material [ESM]). If pretreatment LDL-C was not available it was calculated from the most current LDL-C measurement and statin dose using a regression coefficient approved by the Bulgarian Society of Cardiology and National Health Insurance Fund [18].
Inclusion Criteria
The medical records of patients aged ≥ 18 years with T1DM or T2DM on LMT who were being treated with insulin, insulin analogues, DPP-4 inhibitors, GLP-1 RA and/or SGLT2 inhibitors and attending a participating centre for a routine visit between 1 January 2014 and 1 September 2018 were eligible for analysis in phase 1 of this study. All eligible patients were required to have available data on LDL-C values, LMT (type and dose of medication) and documented family history. Patients identified with a DLCN score ≥ 3 (i.e. possible/probable/definite FH) were eligible for inclusion in the main analysis (phase 2). Patients with secondary dyslipidaemia were excluded, as were those with a normal lipid profile. Investigators started from the most recent eligible records and continued backwards until the required sample size of 450 patients with FH was reached.
The study was conducted in accordance with all local legal and regulatory requirements and followed generally accepted research practices. In agreement with national law, the study protocol was approved by the Central Ethics Committee of the Bulgarian Regulatory Medicines Agency. Due to the retrospective nature of this study informed consent was not required.
Data Collection
For patients identified as having FH as per DLCN criteria, baseline characteristics collected in phase 2 included medical status at the date of enrolment and all relevant clinical history up to that date. The following data were collected:
Demographic and clinical characteristics, including age, gender, employment status, waist circumference, body mass index (BMI), systolic and diastolic blood pressure (SBP and DBP, respectively), height, weight, alcohol intake, smoking and dietary habits and physical activity.
Diagnosis and treatment of hyperlipidaemia (e.g. date of diagnosis, LMT since diagnosis): primary/secondary prevention.
Relevant medical history, including concomitant hypertension; type of diabetes; first-degree relatives with known dyslipidaemia and CV events; history of CVD, stroke, transient ischaemic attacks, peripheral artery disease; FH score based on DLCN; CV risk category; LMT details (type, dose, starting date).
Lipid profile (LDL-C, TC, HDL-C and non-HDL-C)]: most recent measurements. LDL-C was either measured directly or calculated using the Friedewald formula: LDL-C (mmol/L) = (TC [mmol/L] − HDL-C [mmol/L] − triglycerides [mmol/L]/2.19) [19], which is reasonably accurate if total triglyceride levels are < 4.5 mmol/L, but unreliable when triglycerides are elevated due to the effects of very low- and intermediate-density lipoproteins. In such situations, LDL-C was measured directly. Non-HDL-C was calculated by subtracting HDL-C from TC.
Glycaemic parameters (fasting blood glucose and glycated haemoglobin [HbA1c]), other relevant laboratory assessments (e.g. glucose, estimated glomerular filtration rate [eGFR], creatinine).
Hospitalization events, with reasons.
Study Endpoints
The primary objective was to estimate the proportion of patients with FH and diabetes who achieved LDL-C levels < 1.8 mmol/L, i.e. the ESC/EAS goal applicable to very high risk (VHR) patients at the time [9], based on the most recent LDL-C value available. Secondary objectives included (1) describing the clinical characteristics of patients with FH and diabetes; (2) identifying the parameters of clinical management of patients, including statin dose and intensity and use of statin-based combination treatments; (3) determining absolute LDL-C levels and (4) analyzing hospitalizations for CVD. Moderate-intensity statin therapy was defined as atorvastatin 10 or 20 mg, fluvastatin 80 mg, lovastatin 40 mg, rosuvastatin 5 or 10 mg or simvastatin 20 or 40 mg; high-intensity statin therapy was defined as atorvastatin 40 or 80 mg, rosuvastatin 20 or 40 mg or simvastatin 80 mg.
Study Sample Size
A large Swedish survey found that approximately 30% of diabetes patients with a history of CVD reached their ESC/EAS target for LDL-C [11]. As our primary endpoint (achievement of 2016 LDL-C targets) was based on subjects with diabetes and previously undiagnosed FH (and therefore very high pretreatment LDL-C levels), it was anticipated that the proportion of patients reaching the endpoint would be much lower than 30%. Based on the Wilson method [20], we calculated that a target sample size of 453 patients with FH would enable the primary outcome measure to be estimated with 3% precision, if 5–20% of patients achieved the LDL-C target.
Although the EUROASPIRE IV survey calculated a 9.0% overall prevalence of FH (age-standardized prevalence of potential FH by gender and centre) among coronary patients in Bulgaria [14], we did not expect to find the same prevalence of FH in our diabetes population. Patients with heterozygous FH are reported to be at much lower risk of T2DM (approx. 50% lower) than are individuals without FH [21, 22], as well as being at lower risk of statin-associated incident T2DM [23]. There are an estimated 95,000 patients with T1DM or T2DM in Bulgaria being treated with insulin/insulin analogues, DPP-4 inhibitors, GLP-1 RA and/or SGLT2 inhibitors, Thus, we planned to initially include 15 large diabetes centres across the country, with the option to increase this number to a maximum of 20 centres if required to meet our target of 453 FH patients. During the study, it became apparent that the proportion of patients with FH in our study population was much lower than anticipated and the sample size was rounded down from 453 to 450 in the course of site data verification. This made little change to the study precision (3.007 vs 2.997%).
Statistical Analysis
This study was primarily descriptive in nature. Categorical variables were summarized as the number and percentage of patients in each category. For continuous variables, the number of observations, mean, median, standard deviation, quartiles 1 and 3 (Q1, Q3), range (minimum and maximum) and number of patients with missing data were reported.
All data collected during the observation period were used in the analysis and there was no imputation for missing values. To assess whether sites were representative of sites across Bulgaria, summary statistics of site characteristics and the number of patients enrolled in the study by site were analyzed.
Data were managed using GoResearch™, a platform that incorporates a data validation module and is compliant with the requirements of the USA (US Food and Drug Administration document 21 CFR part 11; https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=11) and the European Union (EudraLex Vol. 4 annex 11 for Computerized Systems; https://ec.europa.eu/healthsites/healthfiles/eudralex/vol-4/annex11_01-2011_en.pdf) regulations.
Results
Study Population
A total of 16 diabetes centres participated in the study, providing > 30,000 patient records (500–8000 per centre) in phase 1. Review of these records identified 450 patients with FH who were included in phase 2 of the study as planned; of these patients, 36 (8.0%) had T1DM and 414 (92.0%) had T2DM. The characteristics of these 450 patients are shown in Table 1 and ESM Table 1. Mean age was 60.6 (range 20–84) years, with the majority of patients (n = 314; 69.8%) aged between 50 and 69 years. Mean BMI was 31.7 (range 17.7–60.4) kg/m2. All 450 patients were categorized as VHR, and 271 (60.2%) were primary prevention patients. The majority (n = 280; 62.2%) had DLCN score 3–5 (probable/possible FH). Hypertension (SBP > 140 or DBP > 90 mmHg) was present in 374 patients (83.1%).
Approximately one-half of the patients (236; 52.4%) were receiving insulin or insulin analogues, with DPP4 inhibitors (n = 117; 26.0%) being the next most common antidiabetic treatment among this pre-selected group of patients (Table 1). Lifestyle factors are summarized in ESM Table 2. Approximately half (230; 51.1%) were nonsmokers, and only a minority (26; 5.8%) reported consuming ≥ 3 units of alcohol/day, while approximately one-third reported following a low-calorie or cholesterol-lowering diet. However, it should be noted that lifestyle data were not available for a sizeable proportion of patients (approximately 30–40%; see ESM Table 2).
Lipid-Modifying Therapy
With the exception of three patients (0.6%) who were being treated with fenofibrate alone, all patients were receiving statins, with 389 (86.4%) on statin monotherapy and 58 (12.9%) on statin combinations (Table 2). Dosage details for the 389 patients receiving statin monotherapy are summarized in ESM Table 3. Rosuvastatin and simvastatin were the most commonly used statins. Overall, 79 patients (17.6% of all patients) were on high-intensity statin monotherapy, 34/229 in the primary prevention subgroup (14.8%) and 45/163 (27.6%) in the secondary prevention subgroup.
LDL-C Levels and Goal Achievement, Other Lipids
The lipid profile (most recent measurement) by DLCN score is summarized in Table 3. Overall, median (Q1, Q3) LDL-C was 4.4 (3.6, 5.2) mmol/L, with LDL-C values increasing with DLCN score: 4.03 (3.4, 4.6), 5.1 (4.3, 6.2) and 5.2 (4.7, 6.2) mmol/L in patients with DLCN scores of 3–5, 6–8 and ≥ 9, respectively (Table 3; Fig. 1). A post-hoc analysis conducted using Dunn’s method (with Bonferroni’s correction) after the Kruskal–Wallis test revealed significant differences in LDL-C in DLCN score subgroups 6–8 and ≥ 9 versus 3–5 (both p < 0.001, adjusted) that was reflected by both means and medians. However, there was no significant difference between subgroups with DLCN scores 6–8 and ≥ 9 (data not shown). A similar pattern was seen for TC. Kendall’s procedure revealed that LDL-C (τ = 0.463, p < 0.001) and non-HDL-C (τ = 0.323; p < 0.001) were significantly correlated with DLCN score. HDL-C and triglycerides did not appear to be related to DLCN score. Mean LDL-C levels were only weakly correlated with the intensity of statin monotherapy (high vs. non-high intensity).
Based on the most recent test values, only one patient (with DLCN score 6–8; 0.2% of all patients with FH; 95% confidence interval 0.04–1.25%) had achieved the 2016 ESC-defined target of LDL-C < 1.8 mmol/L, while 15 patients (3.3%) had achieved levels between 1.8 and 2.6 mmol/L (Fig. 2).
HbA1c, serum glucose and creatinine and eGFR (most recent measurements) are summarized in ESM Table 4. Dunn’s method (after Kruskal–Wallis test) did not reveal any significant differences in these laboratory values between the three DLCN score strata. Overall, median (Q1, Q3) HbA1c was 8.0% (6.9.0, 9.4%), with 137 patients (30.4%) having HbA1c ≤ 7% (Fig. 2).
Cardiovascular Events and Hospitalizations
The most common CV events (total 325) recorded among the 179 secondary prevention patients were myocardial infarction/unstable angina (n = 100/325; 30.8% of events), coronary revascularization (60; 18.5%) and stroke (n = 49; 27.4%; ESM Fig. 1a). The number of CV events was not correlated with DLCN score in individual patients.
There were 93 hospitalizations recorded in total; all except for one (pyelonephritis) were for CV events (ESM Fig. 1b). The most common reasons for hospitalizations were unstable angina, coronary revascularization, ischaemic stroke and myocardial infarction, each accounting for approximately 20% of hospitalizations.
Discussion
This national retrospective observational study was based on data retrieved from clinical records of over 30,000 patients with T1DM and T2DM who were being treated with insulin/insulin analogues, GLP1 RA and/or DPP4/SGLT2 inhibitors at diabetes centres across Bulgaria. By applying the widely accepted DLCN criteria to individuals with pretreatment LDL-C ≥ 4.1 mmol/L and/or TC ≥ 8.0 mmol/L, we identified 450 patients with previously undiagnosed possible/probable/definite FH (DLCN score ≥ 3), representing approximately 1.5% of the records studied.
As noted previously, patients with heterozygous FH are reported to be at much lower risk of developing T2DM (approximately 50% lower) than are individuals without FH [21, 22], although the risk may depend on the specific type of FH-associated gene mutation involved [21, 24, 25]. This apparent protective effect of FH might reflect impaired intracellular cholesterol uptake [16, 21]. FH is characterized by reduced LDLR production or function and reduced cholesterol uptake by pancreatic beta cells. Conversely, statin treatment leads to increased LDLR expression and increased cholesterol uptake in beta cells [26, 27].
Almost all (> 99%) of our 450 patients were receiving statin-based therapy, with approximately 18% receiving high-intensity statin monotherapy and 13% on statin combinations. Almost one-third had good glycaemic control (HbA1c ≤ 7%), but only one patient (< 1%) achieved the 2016 ESC/EAS LDL-C goal of < 1.8 mmol/L recommended for VHR patients [9], based on their most recent values. Moreover, patients with the highest DLCN scores were found to have the worst glycaemic control, although HbA1c was not correlated with DLCN score. Previous cardiovascular events were documented in 40% of patients.
Given that lowering of LDL-C to levels well below 1.8 mmol/L has been shown in recent years to confer additional CV risk reduction, updated 2019 European guidelines now advocate an LDL-C target of < 1.4 mmol/L for VHR patients and < 1.8 mmol/L for HR patients, along with a minimum LDL-C reduction from baseline of 50% [28]. For patients with ASCVD with a second vascular event within 2 years while taking maximally tolerated statin-based therapy, the updated guidelines recommend considering an LDL-C target of 1.0 mmol/L [28]. None of our patients achieved LDL-C levels within the new VHR target, since the lowest value recorded was 1.75 mmol/L. Patients with diabetes benefit from aggressive control of dyslipidaemia at least as much as do nondiabetic patients with other risk factors according to data from the Cholesterol Treatment Trialists’ Collaboration meta‐analysis of 14 randomized statin trials [7] and the IMPROVE‐IT (Improved Reduction of Outcomes: Vytorin Efficacy International Trial) trial, which evaluated the addition of ezetimibe to statin therapy [29].
There are multiple factors that can contribute to poor lipid control in patients with dyslipidaemia. Underdosing and statin discontinuation/poor adherence to therapy, which may reflect concerns surrounding actual or anticipated statin intolerance, are acknowledged as key factors and have been linked to poorer clinical outcomes [9, 30]. Moreover, in patients with diabetes, physicians may prioritize glycaemic control over lipid control and be reluctant to prescribe higher statin doses because of potential adverse effects on glucose metabolism [26, 27]. Reimbursement issues in Bulgaria may present a financial barrier to intensive statin therapy, as well as to newer and alternative treatments for patients with inadequate response or statin intolerance. Only 25% of the cost of statins are reimbursed, and simvastatin is the only statin reimbursed by the National Health Insurance Fund for diabetic patients, with atorvastatin and rosuvastatin being paid for out of pocket. Only cardiologists are authorized to prescribe statins as secondary prevention with public funds. Healthcare systems in the Eastern Europe region are based on the reference pricing principle and are, therefore, relatively restrictive in permitting newer treatments.
Even at high intensity, statins may not be able to sufficiently reduce the very elevated baseline LDL-C levels that characterize patients with FH. Monotherapy with atorvastatin 40–80 mg or rosuvastatin 10–20 mg daily can typically lower LDL-C by approximately 50%, while adding ezetimibe to either of these treatment regimens can reduce levels by a further 15–20% [9]. Statins cannot reduce LDL-C in patients with homozygous FH with no residual LDLR function and produce only modest reductions in those with low residual LDLR activity [31]. The availability (since 2015) of the PCSK9 inhibitors (PCSK9i) evolocumab and alirocumab has provided alternative options for the treatment of dyslipidaemia. These agents improve LDLR recycling and increase LDLR availability on hepatocyte cell surfaces [32] and can lower LDL-C by a further 60% in patients already receiving maximal statin therapy [33,34,35,36,37], thereby significantly reducing the risk of CV events [35, 38, 39]. European dyslipidaemia guidelines have recommended that PCSK9i may be considered for VHR patients with ASCVD, including those with progressive ASCVD or diabetes with target organ damage or a major CV risk factor, or for patients with severe FH without ASCVD but severely elevated LDL-C despite maximal statin/ezetimibe therapy [40]. Evolocumab was reported to be effective in reducing LDL-C and other atherogenic lipids, without compromising glycaemic control, in patients with T2DM and dyslipidaemia on statin treatment (n = 981) [41]; in this study, approximately 90% of patients attained LDL-C < 1.8 mmol/L.
In Bulgaria, the treatment of T1DM and T2DM is initiated by endocrinologists, who also follow up patients on insulin, insulin analogues, DPP-4 inhibitors, GLP-1 RA and/or SGLT-2 inhibitors. Such patients visit a diabetes centre every 6 months for follow-up, and once-yearly lipid profile tests are recommended for those receiving LMT. National treatment guidelines ensure that treatment lines are harmonized across diabetes centres. The study sites were chosen based on the National Health Insurance Fund list of diabetes centres authorized to prescribe insulin, insulin analogues, DPP-4 inhibitors, GLP-1 RA and SGLT-2 inhibitors. All patients attending the participating sites who met the inclusion criteria were considered eligible for inclusion in the analysis.
The current study has a number of limitations. Data were captured retrospectively from patient records and are limited to patients treated with insulin, insulin analogues, DPP-4 inhibitors, GLP-1 RA and SGLT-2 inhibitors. It is expected that our results are generalizable to Bulgaria as a whole, but they may not necessarily be directly transferable to other regions. Lifestyle data were missing for approximately 30–40% of patients, perhaps reflecting patient reluctance to disclose such information. The number of hospitalizations may have been underestimated, as patients without hospitalization data could be included in the study. We did not evaluate compliance with LMT. LDL-C was determined by a number of different local laboratories (direct measurement or calculated using the Friedewald formula). Our estimate of the proportion of patients within glycaemic and lipid goals is based only on their most recent available test results. Nevertheless, our observational data provide a useful snapshot of real-life patient management of this population in Bulgaria.
Conclusions
To our knowledge, this is the first study to specifically evaluate lipid management in diabetic patients with FH. Based on the most recent LDL-C measurements for these 450 patients, < 1% who were being treated in diabetes clinics throughout Bulgaria achieved the ESC-defined goal of LDL-C < 1.8 mmol/L. These data highlight the importance of identifying underlying FH in diabetic patients so that they can receive appropriate treatment.
References
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17:83.
Emerging Risk Factors Collaboration, Sarwar N, Gao P, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Authors/Task Force Members, Rydén L, Grant PJ, et al. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: The Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J. 2013;34:3035–87.
Kannel WB. The Framingham Study: an epidemiological investigation of cardiovascular disease, section 30. Some characteristics related to the incidence of cardiovascular disease and death: The Framingham Study 18-year follow-up. Publication No. (NIH) 74-599. Washington DC: Department of Health, Education, and Welfare, Washington; 1974.
Kannel WB. Range of serum cholesterol values in the population developing coronary artery disease. Am J Cardiol. 1995;76:69C–77C.
Kannel WB, Castelli WP, Gordon T. Cholesterol in the prediction of atherosclerotic disease: new perspectives based on the Framingham study. Ann Intern Med. 1979;90:85–91.
Cholesterol Treatment Trialists’ Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376:1670–81.
Reiner Z, Catapano AL, De Backer G, et al. ESC/EAS guidelines for the management of dyslipidaemias: the Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and the European Atherosclerosis Society (EAS). Eur Heart J. 2011;32:1769–818.
Catapano AL, Graham I, De Backer G, et al. 2016 ESC/EAS guidelines for the Management of Dyslipidaemias: the Task Force for the Management of Dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS) developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis. 2016;253:281–344.
Gitt AK, Lautsch D, Ferrieres J, et al. Low-density lipoprotein cholesterol in a global cohort of 57,885 statin-treated patients. Atherosclerosis. 2016;255:200–9.
Eliasson B, Svensson AM, Miftaraj M, et al. Clinical use and effectiveness of lipid lowering therapies in diabetes mellitus—an observational study from the Swedish National Diabetes Register. PLoS ONE. 2011;6:e18744.
Nordestgaard BG, Chapman MJ, Humphries SE, et al. Familial hypercholesterolaemia is underdiagnosed and undertreated in the general population: guidance for clinicians to prevent coronary heart disease Consensus Statement of the European Atherosclerosis Society. Eur Heart J. 2013;34:3478–90.
Akioyamen LE, Genest J, Shan SD, et al. Estimating the prevalence of heterozygous familial hypercholesterolaemia: a systematic review and meta-analysis. BMJ Open. 2017;7:e016461.
De Backer G, Besseling J, Chapman J, et al. Prevalence and management of familial hypercholesterolaemia in coronary patients: an analysis of EUROASPIRE IV, a study of the European Society of Cardiology. Atherosclerosis. 2015;241:169–75.
Alonso R, Mata N, Castillo S, et al. Cardiovascular disease in familial hypercholesterolaemia: influence of low-density lipoprotein receptor mutation type and classic risk factors. Atherosclerosis. 2008;200:315–21.
Paquette M, Bernard S, Ruel I, et al. Diabetes is associated with an increased risk of cardiovascular disease in patients with familial hypercholesterolemia. J Clin Lipidol. 2019;13:123–8.
Khera AV, Won HH, Peloso GM, et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J Am Coll Cardiol. 2016;67:2578–89.
Anonymous. Supplement A: Correction factors lipid-lowering drugs. Available at https://www.danina-g.com/documents/04-Prilojenie-2006-23-01-2006.pdf. Accessed 9 Dec 2019.
Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502.
Valliant R, Dever J, Kreuter F. Statistics for social and behavioral sciences, practical tools for designing and weighting survey samples. New York: Springer; 2018.
Besseling J, Kastelein JJ, Defesche JC, et al. Association between familial hypercholesterolemia and prevalence of type 2 diabetes mellitus. JAMA. 2015;313:1029–36.
Climent E, Perez-Calahorra S, Marco-Benedi V, et al. Effect of LDL cholesterol, statins and presence of mutations on the prevalence of type 2 diabetes in heterozygous familial hypercholesterolemia. Sci Rep. 2017;7:5596.
Vuorio A, Strandberg TE, Schneider WJ, Kovanen PT. Statins and new-onset diabetes mellitus—a risk lacking in familial hypercholesterolaemia. J Intern Med. 2016;279:358–61.
Xu H, Ryan KA, Jaworek TJ, et al. Familial Hypercholesterolemia and type 2 diabetes in the old order Amish. Diabetes. 2017;66:2054–8.
Saavedra YL, Dufour R, Baass A. PCSK9 InsLEU genetic variant is associated with pre-diabetes and diabetes*. J Clin Lipidol. 2015;9:419.
Sattar N, Preiss D, Murray HM, et al. Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials. Lancet. 2010;375:735–42.
Sirtori CR. Pharmacology and mechanism of action of the new HMG-CoA reductase inhibitors. Pharmacol Res. 1990;22:555–63.
Mach F, Baigent C, Catapano AL, et al. 2019 ESC/EAS guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J. 2019;ehz455. https://doi.org/10.1093/eurheartj/ehz455.
Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe added to statin therapy after acute coronary syndromes. N Engl J Med. 2015;372:2387–97.
Banach M, Stulc T, Dent R, Toth PP. Statin non-adherence and residual cardiovascular risk: there is need for substantial improvement. Int J Cardiol. 2016;225:184–96.
Cuchel M, Bruckert E, Ginsberg HN, et al. Homozygous familial hypercholesterolaemia: new insights and guidance for clinicians to improve detection and clinical management. A position paper from the consensus panel on familial hypercholesterolaemia of the European Atherosclerosis Society. Eur Heart J. 2014;35:2146–57.
Seidah NG, Awan Z, Chrétien M, Mbikay M. PCSK9. A key modulator of cardiovascular health. Circ Res. 2014;114:1022–36.
Lipinski MJ, Benedetto U, Escarcega RO, et al. The impact of proprotein convertase subtilisin-kexin type 9 serine protease inhibitors on lipid levels and outcomes in patients with primary hypercholesterolaemia: a network meta-analysis. Eur Heart J. 2016;37:536–45.
Navarese EP, Kolodziejczak M, Schulze V, et al. Effects of proprotein convertase subtilisin/kexin type 9 antibodies in adults with hypercholesterolemia: a systematic review and meta-analysis. Ann Intern Med. 2015;163:40–51.
Sabatine MS, Giugliano RP, Keech AC, et al. Evolocumab and clinical outcomes in patients with cardiovascular disease. N Engl J Med. 2017;376:1713–22.
Sabatine MS, Giugliano RP, Pedersen TR. Evolocumab in patients with cardiovascular disease. N Engl J Med. 2017;377:787–8.
Sabatine MS, Giugliano RP, Wiviott SD, et al. Efficacy and safety of evolocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1500–9.
Robinson JG, Farnier M, Krempf M, et al. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1489–99.
Guedeney P, Giustino G, Sorrentino S et al. Efficacy and safety of alirocumab and evolocumab: a systematic review and meta-analysis of randomized controlled trials. Eur Heart J. 2019. https://doi.org/10.1093/eurheartj/ehz430.
Landmesser U, Chapman MJ, Stock JK, et al. 2017 Update of ESC/EAS Task Force on practical clinical guidance for proprotein convertase subtilisin/kexin type 9 inhibition in patients with atherosclerotic cardiovascular disease or in familial hypercholesterolaemia. Eur Heart J. 2018;39(14):1131–43.
Lorenzatti AJ, Eliaschewitz FG, Chen Y, et al. Randomised study of evolocumab in patients with type 2 diabetes and dyslipidaemia on background statin: primary results of the BERSON clinical trial. Diabetes Obes Metab. 2019;21:1455–63.
Acknowledgements
Funding
Amgen (Europe) GmbH participated in the design/concept of the study and provided funding for the study, preparation of the manuscript and Rapid Service Fee for publication.
Medical Writing Assistance
Julia Balfour of Northstar Medical Writing and Editing, Dundee, UK, provided medical writing support, with financial support from Amgen.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
TT and VL contributed to conception and/or design of the study. AO conducted the statistical analysis. All authors contributed to acquisition, analysis, and/or interpretation of data for the work, critically revised the manuscript, gave final approval and agree to be accountable for all aspects of work ensuring integrity and accuracy.
Disclosures
Tsvetalina Tankova has received consulting fees from MSD, Sanofi, Boehringer Ingelheim, Eli Lilly, Novo Nordisk, Astra Zeneca and speakers bureau fees from MSD, Sanofi, Boehringer Ingelheim, Eli Lilly, Novo Nordisk, Astra Zeneca, Servier, Merck and Amgen. Anna-Maria Borissova has received consulting fees from Boehringer Ingelheim, Astra Zeneca, Mundipharma, Sanofi, Eli Lilly, MSD, Amgen and speakers bureau fees from Novo Nordisk, Eli Lilly, Sanofi, Boehringer Ingelheim, Astra Zeneca, MSD, Servier, Novartis, Amgen, Merck and Roche. Roumyana Dimova has received consulting fees from Amgen and Speakers Bureau fees from Boehringer Ingelheim, Astra Zeneca and Novo Nordisk. Adrian Olszewski is an employee of 2KMM, a contract research organization. Vasil Lachev and Reneta Petkova are employees and shareholders of Amgen. Atanaska Elenkova and Ralitsa Robeva have nothing to disclose.
Compliance with Ethics Guidelines
The study was conducted in accordance with all local legal and regulatory requirements and followed generally accepted research practices. In agreement with national law, the study protocol was approved by the Central Ethics Committee of the Bulgarian Regulatory Medicines Agency. Due to the retrospective nature of this study informed consent was not required.
Data Availability
Qualified researchers may request data from Amgen clinical studies. Complete details are available at the following: http://www.amgen.com/datasharing.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11342132.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Tankova, T., Elenkova, A., Robeva, R. et al. Familial Hypercholesterolaemia in a Bulgarian Population of Patients with Dyslipidaemia and Diabetes: An Observational Study. Diabetes Ther 11, 453–465 (2020). https://doi.org/10.1007/s13300-019-00748-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-019-00748-2