Abstract
Introduction
Diabetes mellitus (DM) is present in 10–15% of the surgical population. It is a known risk factor for adverse postoperative outcomes. UK perioperative guidance recommends optimizing glycemic control preoperatively, aiming for a target glycated hemoglobin (HbA1c) of < 69 mmol/mol. However, real-world compliance with this guidance remains unknown. The aim of our study was to determine how many patients with DM undergoing elective orthopedic and vascular surgery had a preoperative HbA1c of < 69 mmol/mol. We also reviewed the surgical reasons for non-concordance with the recommended preoperative HbA1c target.
Methods
This was a retrospective observational study of 1000 consecutive patients who had been referred for elective vascular and orthopedic surgery at a large tertiary center. Data were collected on these patients, both those with and without DM, between January 2016 and February 2017. Electronic databases were used to collect information on the patients’ preoperative HbA1c concentration and to determine whether there was a resulting delay in surgery when the preoperative HbA1c target of < 69 mmol/mol was exceeded.
Results
Of the 1000 patients referred for surgery (500 orthopedic and 500 vascular patients) included in the study, 201 (20%) had diabetes. Among these 201 people with DM, 155 (77%) had a preoperative HbA1c < 69 mmol/mol. Among the 46 people with DM whose HbA1c exceeded the recommended target, 41 were operated on despite the high HbA1c level, and only five had their surgery deferred or canceled due to suboptimal preoperative glycemic control.
Conclusions
Our data shows that the majority (77% ) of people undergoing elective vascular and orthopedic surgery were able to achieve a target HbA1c of < 69 mmol/mol. The current preoperative guidance is therefore achievable in a real-life setting. However, as is stated in the national guidance, this target should only be used where it is safe to do so and a degree of clinical discretion is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The prevalence of diabetes mellitus (DM) is increasing in the UK, where it has been estimated that there are currently 3.8 million adults with DM, equivalent to 8.6% of the adult population [1]. This is an increase from the estimate of 2.7 million (6% of the adult population) in 2013 [2]. Recent studies have shown that 8.8% of surgical referrals to all specialities are for persons with diabetes, and that 10–15% of those who ultimately undergo surgery have DM [3, 4]. This figure is expected to increase alongside increases in the prevalence of DM.
Poor perioperative diabetes control has been shown to be associated with adverse outcomes in almost every surgical speciality [5,6,7,8,9,10,11,12,13,14,15,16,17,18], although it is acknowledged that these data show an association and not causation. However, given the strength of the association, national guidelines recommend that glycemic control be optimized prior to elective surgery—i.e. the patient should achieve a glycated hemoglobin (HbA1c) of ≤ 69 mmol/mol (8.5%), where it is safe to do so [4, 19]. To date there are few data on how closely clinicians adhere to this standard at the preoperative assessment, or whether this target is achievable.
The aim of this single-center study was to determine how many orthopedic and vascular surgery patients with DM in a convenience sample had a preoperative HbA1c above the recommended target of 69 mmol/mol (8.5%), and how many ultimately underwent surgery despite having an HbA1c which exceeded the target.
Methods
We carried out a retrospective review of a convenience sample of 1000 consecutive vascular and orthopedic patients who had a preoperative assessment between 15 January 2016 and 20 February 2017 at the Norfolk and Norwich University Hospital (NNUH), a 1000-bed teaching hospital in the East of England.
All patients who require an elective vascular or orthopedic procedure are seen in a preoperative assessment clinic in the 2 weeks preceding their surgery. This clinic is run by experienced nursing staff with anaesthetic medical support. For those with significant co-morbidities, the assessments are undertaken by the anaesthetists themselves.
Patients attending their assessment were identified using the hospital’s patient administration system (PAS). Details of patients’ preoperative assessment were found using internal electronic databases (Orsos Web Periop [Allscripts, Manchester UK] and Bluespier [Droitwich, UK]). Sunquest ICE (Integrated Clinical Environment, an online pathology requesting and reporting system [Tucson, AZ]) and online outpatient clinic letters were then used to collect data on the patients’ HbA1c and any resulting delay in their elective surgery. Patients with and without DM were included in the study.
The study was registered as a local clinical audit (registration code DIAB-17-18-08) and as such ethical approval was not required. The study was registered with Researchregistry.com, registration number 4756. Reporting of this work followed the STROCSS (Strengthening the Reporting of Cohort Studies in Surgery) criteria. [20].
Results
Demographics and Type of Surgery
Of the 1000 consecutive patients reviewed, the median age was 69 (range 16–92) years, 42% were female and 20% had diabetes (Table 1). There was an even split between vascular and orthopedic surgery patients. The type of surgery performed is summarized in Table 2.
HbA1c Concentration
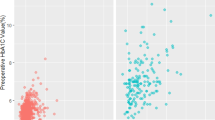
Overall there were 201 patients with DM, among whom 155 (77%) achieved an HbA1c below the target of 69 mmol/mol (8.5%) prior to their surgery. A total of 46 patients (23%) with DM did not meet the recommended preoperative HbA1c target.
Of the 46 individuals with DM who had a preoperative HbA1c ≥ 69 mmol/mol (8.5%), 41 underwent surgery irrespective of their preoperative glycemic control. The procedures carried out for these individuals are listed in Table 3. The remaining five individuals had their surgery deferred or canceled as a result of suboptimal preoperative glycemic control.
Deferred Surgeries
The details of the five individuals who had their surgery delayed or canceled due to a high HbA1c concentration are summarized in Table 4.
The surgery of one individual who was scheduled to have a vascular procedure for an occluded superior femoral artery stent, for which a femoro-distal bypass was indicated, was canceled due to high HbA1c. However, because the patient had continued poor glycemic control but the symptoms showed an improvement, surgery was no longer deemed urgent, and the decision was made to continue conservative treatment. This individual had the highest HbA1c readings of all the patients included in this study (134 and 140 mmol/mol [14.4 and 15%, respectively]).
Of the seven orthopedic patients with an HbA1c of ≥ 69 mmol/mol, only three ultimately had their respective surgery without delay. The HbA1c values of these three patients were 74, 72, and 69 mmol/mol (8.9, 8.7 and 8.5%), respectively. The patient with the HbA1c of 74 mmol/mol (8.9%) underwent an urgent foot amputation following a diagnosis of osteomyelitis.
No further preoperative assessments or admission details were found for the two patients with high HbA1c concentrations awaiting total hip replacements. These patients may have had their surgery elsewhere or had their surgery canceled altogether, thereby opting for conservative management.
Discussion
Our study shows that of 201 vascular and orthopedic patients with DM, only 46 (23%) had a pre-operative HbA1c ≥ 69 mmol/mol (8.5%). Of these latter 46 patients, only five individuals had their surgery deferred or canceled due to exceeding the target HbA1c concentration, while the majority (41/46) underwent surgery as planned.
Our institution is a 1000-bed tertiary teaching hospital that primarily serves the population of Norfolk, UK as well as neighboring counties. The prevalence of DM (diagnosed and undiagnosed) in Norfolk alone was estimated at 68,098 in 2015 [1]. At the time of the 2017 National Diabetes Inpatient Audit there were 140 inpatients with DM at the NNUH, accounting for 15.9% of the total number of beds included in the audit [21].
It is clear that if poor glycemic control was not picked up by the diabetes caregiver prior to the patient attending the the preoperative assessment clinic, then 2 weeks would be insufficient time to optimize glycemic control and the decision on whether to defer surgery would depend on the outcome of a discussion between the anaesthetist and the surgeon. The predominant factor in this discussion would be the urgency of the surgery. In line with UK national guidelines, the preoperative assessment clinic staff does not manage the diabetes care of individuals other than giving out instructions on how to manage their diabetes medications on the day prior to and on the day of surgery [19]. Among the patients reviewed here, those whose surgery could be safely deferred were asked to return to their primary diabetes caregiver who would then apply the current standard of care to improve glycemic control. These patients were sent to their diabetes caregiver with the information that the delay in surgery was due to poor glycemic control, and they were given additional information on the glycemic target. The vast majority of patients with type 1 diabetes (> 98%) in our study were looked after by secondary care services, while > 80% of those with type 2 diabetes were looked after by primary care services.
We believe that the sample size was large enough to allow for the primary analysis—i.e. to determine how many patients with DM had a pre-operative HbA1c below the target of 69 mmol/mol (8.5%) for elective orthopedic and vascular surgery. We were also able to review any patients who had a delay in their surgery due to high HbA1c. A strength of our study is that it was a single-center study which enabled us to comprehensively collect the data on HbA1c and on whether surgery went ahead or not.
A limitation in our data was that we did not collect information on interventions implemented to optimize glycemic control before the preoperative assessment, a task which may have been performed by primary or secondary care teams [4, 19]. Such data would have demonstrated whether patients with high HbA1c concentrations were being targeted for optimization of glycemic control before being referred for surgery. In addition, the aim of this study was not to look at any excess morbidity and mortality following surgery in patients with an HbA1c ≥ 69 mmol/mol. We are aware that the sample size was too small for such a study, and other work is ongoing to address this question. Further limitations to our study include not collecting data on the use of continuous glucose monitoring or insulin pump use nor on who was at high risk of developing hypoglycemia.
Data are available which show that post-operative outcomes worsen with worsening of preoperative glycemic control [5,6,7,8,9,10,11,12,13,14,15,16,17,18]. This increased postoperative complication rate is also associated with increased costs [22]. However, little data are currently available on whether various preoperative HbA1c targets are achievable for those undergoing elective surgery or whether clinicians adhere to these guidelines before proceeding with surgery. The data from the present study show that the orthopedic department adhered relatively closely to the target HbA1c of 69 mmol/mol. A previous study by Giori et al. focused on whether people with diabetes requiring total joint arthroplasty at a single center in the USA could achieve a pre-operative HbA1c goal of 53 mmol/mol [23]. These authors found that 94% of their patients ultimately did achieve the target HbA1c, but that 15% had their surgery delayed due to poor glycemic control, similar to our findings. These results led them to conclude that a goal designed to reduce perioperative risk should be achievable but also that it may not be possible for some patients with DM to achieve this target HbA1c of < 53 mmol/mol. However, Giori et al. [23] aimed for much tighter glycemic control than the UK current guidelines, which recommend an HbA1c of < 69 mmol/mol [19]. Furthermore, many individuals requiring joint arthroplasty are elderly, and such ‘tight’ glycemic control may be inappropriate and indeed harmful in this patient population [24, 25]. Some authors from the USA have shown that risks of excess postoperative complications first occur when the HbA1c rises to > 58 mmol/mol [26], and thus a target of < 58 mmol/mol may be inappropriate.
The recommended threshold for preoperative HbA1c differs between studies, ranging between 53 and 75 mmol/mol [6, 26,27,28,29,30]. When investigating joint infections following total knee arthroplasty [31] and hip arthroplasty [29], Cancienne et al. calculated that a target HbA1c of 64 or 58 mmol/mol, respectively, could be used. However, for both studies the authors suggested that HbA1c had poor sensitivity as an independent predictor of infection.
There are data to suggest that those people who are hyperglycemic, but not previously known to have diabetes preoperatively, have poorer postoperative outcomes than those known to have diabetes [32,33,34]. These data suggest that for those who are at risk of developing hyperglycemia, pre-operative HbA1c testing may be beneficial [35]. Those people who may benefit from preoperative testing of HbA1c are listed in Table 5.
Conclusions
In summary, our data show that the majority (77%) of patients in our convenience sample of 1000 consecutive patients undergoing elective vascular and orthopedic surgery were able to achieve a target HbA1c of < 69 mmol/mol. The current preoperative guidance is therefore achievable in a real-life setting. However, as is stated in the national guidance, this target should only be used where it is safe to do so and that a degree of clinical discretion is necessary.
References
Public Health England. Diabetes prevalence model. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/612306/Diabetesprevalencemodelbriefing.pdf. 2016. Accessed 13 Aug 2019.
Public Health England. Adult obesity and type 2 diabetes. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/338934/Adult_obesity_and_type_2_diabetes_.pdf. 2014. Accessed 13 Aug 2019.
Pournaras DJ, Photi ES, Barnett N, et al. Assessing the quality of primary care referrals to surgery of patients with diabetes in the East of England: a multi-centre cross-sectional cohort study. Int J Clin Pract. 2017;71(7):e12971.
Barker P, Creasey PE, Dhatariya K, et al. Peri-operative management of the surgical patient with diabetes 2015: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2015;70(12):1427–40.
Walid MS, Newman BF, Yelverton JC, et al. Prevalence of previously unknown elevation of glycosylated hemoglobin in spine surgery patients and impact on length of stay and total cost. J Hosp Med. 2010;5(1):E10–4.
O’Sullivan CJ, Hynes N, Mahendran B, et al. Haemoglobin A1c (HbA1C) in non-diabetic and diabetic vascular patients. Is HbA1C an independent risk factor and predictor of adverse outcome? Eur J Vasc Endovasc Surg. 2006;32(2):188–97.
Gustafsson UO, Thorell A, Soop M, Ljungqvist O, Nygren J. Haemoglobin A1c as a predictor of postoperative hyperglycaemia and complications after major colorectal surgery. Br J Surg. 2009;96(11):1358–64.
Halkos ME, Lattouf OM, Puskas JD, et al. Elevated preoperative hemoglobin A1c level is associated with reduced long-term survival after coronary artery bypass surgery. Ann Thorac Surg. 2008;86(5):1431–7.
Kreutziger J, Schlaepfer J, Wenzel V, Constantinescu MA. The role of admission blood glucose in outcome prediction of surviving patients with multiple injuries. J Trauma. 2009;67(4):704–8.
Vilar-Compte D, de Iturbe IA, Martin-Onraet A, et al. Hyperglycemia as a risk factor for surgical site infections in patients undergoing mastectomy. Am J Infect Control. 2008;36(3):192–8.
Park C, Hsu C, Neelakanta G, et al. Severe intraoperative hyperglycemia is independently associated with surgical site infection after liver transplantation. Transplantation. 2009;87(7):1031–6.
Ambiru S, Kato A, Kimura F, et al. Poor postoperative blood glucose control increases surgical site infections after surgery for hepato-biliary-pancreatic cancer: a prospective study in a high-volume institute in Japan. J Hosp Infect. 2008;68(3):230–3.
Chuang SC, Lee KT, Chang WT, et al. Risk factors for wound infection after cholecystectomy. J Formos Med Assoc. 2004;103(8):607–12.
Shibuya N, Humphers JM, Fluhman BL, Jupiter DC. Factors associated with nonunion, delayed union, and malunion in foot and ankle surgery in diabetic patients. J Foot Ankle Surg. 2013;52(2):207–11.
Sadoskas D, Suder NC, Wukich DK. Perioperative glycemic control and the effect on surgical site infections in diabetic patients undergoing foot and ankle surgery. Foot Ankle Spec. 2016;9(1):24–30.
Domek N, Dux K, Pinzur M, Weaver F, Rogers T. Association between hemoglobin A1c and surgical morbidity in elective foot and ankle surgery. J Foot Ankle Surg. 2016;55(5):939–43.
Jehan F, Khan M, Sakran JV, et al. Perioperative glycemic control and postoperative complications in patients undergoing emergency general surgery: what is the role of plasma hemoglobin A1c? J Trauma Acute Care Surg. 2018;84(1):112–7.
Martin ET, Kaye KS, Knott C, et al. Diabetes and risk of surgical site Infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2016;37(1):88–99.
Dhatariya K, Levy N, Kilvert A, et al. NHS Diabetes guideline for the perioperative management of the adult patient with diabetes. Diabet Med. 2012;29(4):420–33.
Agha RA, Borrelli MR, Vella-Baldacchino M, Thavayogan R, Orgill DP. The STROCSS statement: strengthening the reporting of cohort studies in surgery. Int J Surg. 2017;49:198–202.
NHS Digital. National Diabetes Inpatient Audit (NaDIA)—2017. https://digital.nhs.uk/data-and-information/publications/statistical/national-diabetes-inpatient-audit/national-diabetes-inpatient-audit-nadia-2017. 2018. Accessed 23 Aug 2019.
Kurowicki J, Rosas S, Khlopas A, et al. Impact of perioperative HbA1c on reimbursements in diabetes mellitus patients undergoing total hip arthroplasty: a nationwide analysis. J Arthroplasty. 2017;33(7):2038–42.
Giori NJ, Ellerbe LS, Bowe T, Gupta S, Harris AH. Many diabetic total joint arthroplasty candidates are unable to achieve a preoperative hemoglobin A1c goal of 7% or less. J Bone Joint Surg Am. 2014;96(6):500–4.
Dhatariya K. Pharmacotherapy for type 2 diabetes in very elderly patients: practicing nihilism or pragmatism? Age Ageing. 2015;44(4):540–2.
The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Eng J Med. 2008;358(24):2545–59.
Underwood P, Askari R, Hurwitz S, Chamarthi B, Garg R. Preoperative A1C and clinical outcomes in patients with diabetes undergoing major noncardiac surgical procedures. Diabetes Care. 2014;37(3):611–6.
Cancienne JM, Miller MD, Browne JA, Werner BC. Not all patients with diabetes have the same risks: perioperative glycemic control Is associated with postoperative infection following knee arthroscopy. Arthroscopy. 2018;34(5):1561–9.
Kallio PJ, Nolan J, Olsen AC, et al. Anesthesia preoperative clinic referral for elevated HbA1c reduces complication rate in diabetic patients undergoing total joint arthroplasty. Anesth Pain Med. 2015;5(3):e24376.
Cancienne JM, Werner BC, Browne JA. Is there a threshold value of hemoglobin A1c that predicts risk of infection following primary total hip arthroplasty? J Arthroplasty. 2017;32(9):S236–40.
Cheisson G, Jacqueminet S, Cosson E, et al. Perioperative management of adult diabetic patients. Preoperative period. Anaesth Crit Care Pain Med. 2018;37[Suppl 1]:S9–19.
Cancienne JM, Werner BC, Browne JA. Is there an association between hemoglobin A1C and deep postoperative infection after TKA? Clin Orthop Relat Res. 2017;457(6):1642–9.
Blaha J, Mraz M, Kopecky P, et al. Perioperative tight glucose control reduces postoperative adverse events in nondiabetic cardiac surgery patients. J Clin Endocrinol Metab. 2015;100(8):3081–9.
Kwon S, Thompson R, Dellinger P, et al. Importance of perioperative glycemic control in general surgery: a report from the surgical care and outcomes assessment program. Ann Surg. 2013;257(1):8–14.
Kotagal M, Symons RG, Hirsch IB, et al. Perioperative hyperglycemia and risk of adverse events among patients with and without diabetes. Ann Surg. 2016;261(1):97–103.
Dhatariya KK, Wiles MD. Pre-operative testing guidelines: a NICE try but not enough. Anaesthesia. 2016;71(12):1403–7.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Celina Uppal and Andrew Blanshard collected and analyzed the data and wrote the initial draft of the manuscript. Rupa Ahluwalia supervised the project and helped draft the final manuscript. Ketan Dhatariya conceived the study and wrote the final draft of the manuscript. All authors saw and approved the final draft.
Disclosures
Ketan Dhatariya is a member of the journal’s Editorial Board. Celina Uppal, Andrew Blanshard and Rupa Ahluwalia have nothing to disclose.
Compliance with Ethics Guidelines
The study was registered as a local clinical audit (registration code DIAB-17-18-08) and as such ethical approval was not required. The study was registered with Researchregistry.com, registration number 4756. This work has been reported in line with the STROCSS criteria [20].
Data Availability
The datasets during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.9667592.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Uppal, C., Blanshard, A., Ahluwalia, R. et al. Achieving a Preoperative Target HbA1c of < 69 mmol/mol in Elective Vascular and Orthopedic Surgery: A Retrospective Single Center Observational Study. Diabetes Ther 10, 1959–1967 (2019). https://doi.org/10.1007/s13300-019-00688-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-019-00688-x