Abstract
The need to develop an insulin delivery system that can closely mimic physiologically induced changes in prandial insulin release has been a major research target since the discovery of insulin. The challenges facing existing insulin delivery systems, related to relatively slow pharmacokinetics and pharmacodynamics, have been further highlighted by rapid advances in diabetes technology and progress in artificial pancreas research. Despite the growing interest in alternative routes of insulin administration, the subcutaneous route remains—at least for now—the preferred route for insulin administration. In this article, we review efforts aimed at developing subcutaneously injected ultrafast-acting insulin and measures aimed at enhancing insulin absorption, focusing on local warming devices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In people with normal glucose tolerance, the endogenous insulin profile combines constant pulsatile basal insulin production with prandial insulin secretion. The main role of basal insulin is to limit hepatic glucose production while maintaining adequate glucose for cerebral function. Following a mixed meal, the rise in blood glucose is rapidly sensed by beta cells in the pancreas, resulting in insulin release, over two phases, into the portal circulation and a rapid rise in circulating insulin levels. This results in suppression of hepatic glucose production followed by stimulation of glucose utilisation in the main insulin-dependent tissues (e.g. skeletal muscle and adipose tissue), preventing a postprandial rise in blood glucose levels [1].
In healthy nonobese adults, insulin is secreted at a basal rate of 0.5–1 U per hour, resulting in plasma concentrations of 5–15 mU/L in fasting conditions [1]. Following a mixed meal, plasma insulin levels reach half of the maximal concentration in approximately 16–18 min and peak at 60–80 mU/L within 45 min before returning to baseline 2–4 h later [2].
Since the discovery of insulin in 1922, there have been continuous advances in the field of insulin therapy, with the aim being to develop insulin delivery systems that can mimic physiological insulin secretion. However, several factors affect the pharmacokinetics (PK) and pharmacodynamics (PD) of exogenously administered insulin. These include insulin formulation, dose and concentration, as well as mode of administration, injection site, injection depth, infusion site age, exercise, local massage, temperature and individual variation in obesity, age, and smoking [2–7]. The subcutaneous tissue structure limits the spread of injectable insulin and its absorption into the systemic circulation. This impacts insulin PK and PD with delayed onset, a delayed peak and a longer duration of insulin action, making postprandial glucose optimisation challenging, with early postprandial glycaemic (PPG) excursions and a risk of late postprandial hypoglycaemia, negatively affecting the overall glycaemic control as assessed by HbA1c [8]. This increase in glycaemic variability may also contribute to diabetes-related complications, independently of HbA1c [9, 10].
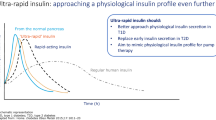
The introduction in the 1990s of rapid-acting insulin analogues (RAIAs), with insulin absorption and a metabolic effect that are accelerated compared to regular human insulin (RHI), has resulted in improved diabetes management. The faster onset and peak of action allow the time interval between insulin injection and meals to be shortened and postprandial glycaemic excursions to be reduced [11]. The shorter duration of action also reduces the risk of hypoglycaemia [12]. Evidence from meta-analyses also shows the beneficial effect of RAIAs compared to RHI in reducing HbA1c in both type 1 and type 2 diabetes [13, 14]. Moreover, the earlier rise in insulin levels obtained with RAIAs, simulating the first-phase insulin response, may have a more pronounced impact on the suppression of hepatic glucose production with a subsequent significant reduction in PPG [15]. Current RAIAs (lispro, aspart and glulisine) have similar PK/PD profiles, with the onset of insulin exposure occurring in 5–15 min, a peak at 45–60 min and an overall duration of about 3–4 h [11]. Despite the benefits provided by RAIAs, these formulations remain slower than physiological insulin secretion since their glucose-lowering effect can take 2–3 h to peak and can last for 5–6 h [16]. Several studies have demonstrated that an injection to meal time interval of 15–20 min was required to shift the action profile of RAIAs to achieve a better overlap with the postprandial glucose profile and optimally reduce PPG excursions without increasing the risk of hypoglycaemia [17–19]. However, inconvenience and the increased risk of periprandial hypoglycaemia are likely to be a barrier to an early injection to meal interval in reality. Furthermore, the relatively slow PK/PD of RAIAs represent a challenge to artificial pancreas algorithms. The delay between the start of a meal and rise of interstitial fluid glucose, which triggers automatic insulin delivery, is exacerbated by the slow PK/PD of existing insulin formulations, resulting in large PPG excursions. Therefore, the development of novel formulations and methods that modify insulin PK/PD to mimic the endogenous insulin profile remains a major research target.
Euglycaemic glucose-clamp studies are frequently used to assess PK (insulin exposure) and PD (insulin action) of insulins. The serum insulin concentration reflects insulin exposure, while glucose infusion rate (GIR) reflects insulin action. The onset, time to peak and offset are represented by early t 50%, t max and late t 50%, respectively. Other important parameters include maximum insulin concentration (C max), maximum GIR (GIRmax) and area under the curve (AUC). The AUC for insulin represents the overall bioavailability of injected insulin, while the AUC for GIR represents the overall glucose-lowering effect [1].
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Innovations Aiming to Enhance Absorption of Subcutaneously Injected Insulin
Several methods that are aimed at enhancing prandial insulin delivery to the systemic circulation have been studied. These include studies to investigate alternative routes of insulin administration to the traditional subcutaneous route, such as inhaled Technosphere insulin (Afrezza), buccal spray insulin (Oral-lyn), intraperitoneal and intradermal delivery [2, 20–23]. Innovations aimed at enhancing the absorption of subcutaneous insulin include the development of novel formulations that contain excipients such as citrate and disodium ethylenediaminetetraacetic acid in VIAject [24] or nicotinamide and arginine in faster-acting insulin aspart (FIAsp) [25].
BioChaperone Lispro (Adocia, Lyon, France) is a novel insulin formulation that comprises the proprietary BioChaperone platform. This is a library of polysaccharide derivatives that are designed to form a reversible molecular complex with therapeutic proteins, e.g. insulin. This protects insulin from enzymatic degradation and enhances its stability and solubility, with subsequent enhancement of absorption and bioavailability [26, 27].
A recent study has demonstrated the effect of the addition of recombinant human hyaluronidase (rHuPH20) on enhancing PK/PD profiles of co-injected RAIAs [28]. The FDA-approved Hylenex® recombinant human hyaluronidase (Halozyme Therapeutics, San Diego, CA, USA) transiently and reversibly degrades hyaluronan to enhance the diffusion and absorption of co-injected insulin.
The use of jet spray injectors has also been investigated as a method to enhance insulin absorption [29, 30]. Initially designed for people with needle phobia, jet spray injectors work by sending a fine spray of insulin through the skin into subcutaneous tissue using a high-velocity jet, allowing insulin delivery without the need to use a needle to puncture the skin. They enhance insulin absorption by mechanically dispersing insulin into a large area of the subcutaneous tissue. The use of jet injectors is limited by the need for training, their cost and the potential discomfort caused by the high-velocity jet.
This article reviews evidence relating to the use of local warming devices (InsuPatch and InsuPad) as tools to increase the absorption of subcutaneously injected insulin and enhance its PK/PD profile. A literature review was performed using PubMed, the Cochrane Library database and Web of Science to identify relevant studies. Search terms used were “insulin absorption”, “insulin pharmacokinetics” and “insulin pharmacodynamics” followed by a keyword search for “local warming” and “local heating”. Other search terms used were “InsuPad” and “InsuPatch”.
Local Warming Devices
Principle and Mechanism of Action
The effect of ambient temperature on insulin PK has been recognised. Exposure to a sauna at 85 °C for 50 min resulted in an increase in insulin absorption of 110% and a reduction in postprandial glycaemic excursions compared to a control environment of 22 °C [31]. This effect on insulin PK is produced through an increase in local blood flow and was demonstrated in another study in which a rise in ambient temperature from 20 to 35 °C resulted in a 25% increment in skin temperature, a two- to threefold increase in skin blood flow and 50–60% increases in insulin absorption over a 4-h period in people with diabetes [32]. At normal ambient room temperature (22–24 °C), a wide range of local skin temperatures occur (30–37 °C), with a positive correlation observed between serum insulin 45 min after injection and temperature [33].
InsuPatch and InsuPad (InsuLine Medical, Israel) are devices that employ the concept of elevating the local skin temperature at the time of subcutaneous prandial insulin injection to modify insulin PK/PD. InsuPatch (Fig. 1) is designed for insulin pump users. It consists of a heating pad attached to the insulin pump infusion set and a unit that controls and monitors the temperature of the heating pad. The heating pad is a flat circular patch with a 2-cm inner diameter and a 5-cm outer diameter that incorporates battery-powered heating coils. Following the delivery of an insulin bolus, InsuPatch warms the tissue surrounding the infusion set to 38.5 °C for 30 min.
InsuPad (Fig. 2) consists of two units: a warming electronic pad and a disposable plastic frame. One part of the plastic frame houses the warming unit whilst the other part of the frame attaches to the skin with adhesive tape to provide a window (42 × 60 mm) through which prandial insulin doses can be injected over 24 h. Following insulin administration, closure of the plastic frame exposes the injection site to the warming unit, which is automatically activated. The unit works for 50 min to apply three 10-min warming intervals that increase the local skin temperature to 40 °C. There is a 10-min break following each warming interval. At the end of the day, removal of the warming unit destroys the disposable frame and the unit is charged. InsuPad is CE marked and is currently approved for marketing in a few countries, including Israel, Canada and Germany. However, it is not FDA approved yet.
Studies Evaluating the Effects of Local Warming Devices
Evaluation of InsuPatch
The effects of InsuPatch on the PK and PD of insulin were evaluated in 17 adults with type 1 diabetes (using insulin lispro or aspart). In this open-label randomised crossover study, subjects were randomised to InsuPatch or control (using an infusion set without InsuPatch) arms before crossover and underwent a meal tolerance test glucose clamp. This 4-h study demonstrated that the use of InsuPatch resulted in significant acceleration of insulin absorption with earlier onset of insulin exposure (early t 50%max decreased by 30%), acceleration of time to insulin peak (t max decreased by 43%), a significant increase in maximum insulin concentration (C max increased by 37%) and significant increases in the AUC for insulin at 0–30, 0–60 and 0–90 min. The effect of the device on the glucose profile showed significant reductions in PPG excursions at 60 and 90 min by 36% and 39%, respectively (Table 1). Although the study demonstrated the potential advantages of improving insulin PK/PD using InsuPatch, it is limited by its small data set: data on PK were obtained from only 9 of the 17 subjects [34].
Aiming to evaluate the effects of InsuPatch on the PK and PD of insulin in a real-life setting where subjects received continental breakfast and dinner, a 4-day study was conducted in 24 adults with type 1 diabetes. The study demonstrated that the use of InsuPatch resulted in reductions in PPG of 14% and 40% after breakfast and dinner, respectively [35].
In a larger study, a euglycaemic glucose clamp technique was used to evaluate the effects of InsuPatch. In this randomised crossover study, 56 subjects with type 1 diabetes were randomised to either an intervention phase or a control phase before crossover. Compared to the control, the use of InsuPatch resulted in a 30% increase in the AUC of serum insulin in the first 60 min following insulin bolus and a greater insulin peak concentration (C max 57 vs 47.6 mU/L). Despite the enhanced PK, this did not translate into significant PD benefits [36].
The effect of InsuPatch was evaluated in two studies in adolescents with type 1 diabetes. In the first study, a euglycaemic glucose clamp technique was used to evaluate the PK/PD of insulin aspart with the use of the InsuPatch device in 13 adolescents. Subjects underwent two euglycaemic clamp procedures on separate occasions: one with and one without InsuPatch activation, in random order. During studies where the InsuPatch was active, the infusion site was warmed to 38.5 °C 15 min prior to bolus administration and remained warmed for 60–90 min after bolus administration. PK data showed that the use of InsuPatch resulted in a 30% increase in maximal insulin increment (ΔC max 106 vs 81 uU/mL) and a shorter time to reach this maximum increment (t max 41 vs 67 min). It also resulted in 35% and 28% increases in AUC for insulin increment over the first 90 min and over the full 5 h, respectively. This translated into enhanced PD with a 28% acceleration of the peak of insulin action (mean GIR t max 90 vs 125 min) and a 36% increase in the overall glucose-lowering effect for the first 90 min (GIR AUC0–90) [37]. The second study, which recruited 17 adolescents with type 1 diabetes, aimed to evaluate the effect of InsuPatch at a higher temperature (40 °C). This resulted in a similar PD effect on GIR t max and an 85% increase in the overall glucose-lowering effect for the first 30 min (GIR AUC0–30) with InsuPatch activation. This study also demonstrated that the use of InsuPatch resulted in an acceleration of the disappearance of the insulin bolus. The time for the insulin level to return to baseline was reduced from 200 to 183 min with InsuPatch use. This implies a potential benefit of InsuPatch use in reducing the risk of late postprandial hypoglycaemia, resulting from the effect of insulin stacking. The device was well tolerated by all subjects despite the use of the higher temperature [38]. It was not clear whether the two most important unique observations in this study (85% increase in GIR AUC0–30 and the faster-out effect) were related to the higher temperature (40 °C), as neither of those two variables were reported in the earlier study [37]. Other PK/PD variables were similar for the two studies. It is also important to note that, in these two studies, InsuPatch was activated 15 min before insulin bolus and remained active for 60 min afterwards. Despite the value of earlier administration of RAIAs before mealtime, it is difficult to consistently undertake this task, and the pre-activation of the InsuPatch device before mealtime could be similarly challenging. These two studies are limited by the small populations involved and the inability to extrapolate the results beyond the study populations.
A study of the effect of the InsuPatch on automated closed-loop glucose control in type 1 diabetes is currently underway [39].
Evaluation of InsuPad
The InsuPad device was evaluated in a number of meal tolerance studies that demonstrated the potential benefits of InsuPad in lowering PPG excursions in subjects with type 2 diabetes [40]. In an open-label randomised crossover meal tolerance study, the effect of InsuPad on PPG excursions was evaluated in subjects with type 2 diabetes treated with basal-bolus insulin therapy. Glucose profiles demonstrated a 40% reduction in the AUC of the PPG excursion during the first 2 h following the meal when InsuPad was used (Fig. 3). Insulin PK (Fig. 4) showed that the use of InsuPad resulted in an earlier insulin peak (t max 52 vs 80 min), a shorter duration (151 vs 190 min) and a significantly higher AUC of insulin concentration in the first hour after the meal (Table 2). The study also demonstrated the effect of InsuPad in reducing intersubject variability in relation to the time to insulin peak. The use of InsuPad did not result in skin irritation or inflammation in any of the subjects [41].
Effect of InsuPad on postprandial glucose (black circles) compared to the control (white squares) following a liquid mixed meal in subjects with type 2 diabetes. Figure reproduced with permission from SAGE publications Inc. [41]
Effect of InsuPad use on insulin pharmacokinetics (black circles) compared to the control (white squares) following a liquid mixed meal in subjects with type 2 diabetes. Figure reproduced with permission from SAGE publications Inc. [41]
Further evaluation of the device was conducted in another study under more real-life conditions. An open-label randomised crossover study was conducted in 20 subjects (14 with type 2 diabetes and 6 with type 1 diabetes) with insulin resistance (mean total daily insulin dose of 0.97 U/kg body weight). Subjects were randomised to either 4 weeks of InsuPad use with breakfast and dinner or to standard care before crossing over to the other phase for 4 weeks. Capillary blood glucose was monitored at least five times daily and insulin doses were documented. PPG excursions between 75 and 135 min after the meal were analysed. Despite a significant reduction in PPG excursions with InsuPad use, there was no statistically significant difference in overall mean glucose or biochemical hypo- and hyperglycaemia. The study is limited by the method of assessing PPG excursions. Valid pairs of pre- and postprandial blood glucose measurements were available for only 50% of breakfasts and dinners [42].
The device was also evaluated in a larger study under real conditions of daily life over a period of 3 months. The Barmer study was performed with 145 subjects (13 with type 1 diabetes and 132 with type 2 diabetes, aged 61.1 ± 8.4 years, BMI 35.5 ± 6.1 kg/m2). All patients were on a basal bolus regimen using RAIAs. Subjects underwent a 4-week run-in period before randomisation to InsuPad (intervention, n = 73) or not (control, n = 72). Results showed an initial improvement in HbA1c during the 4-week optimisation phase in the whole study cohort [drop from 7.2 to 6.8% (P < 0.001)]. At the end of the 3-month study, the two groups showed similar improvements in glycaemic control, with a further significant drop of HbA1c to 6.3% observed in the two groups. However, the prandial insulin requirement in the intervention group was 19% lower than baseline (drop from 70 to 55 U). In comparison, subjects in the control group needed an 8.1% increase in their prandial insulin requirements. There was an increase of 3.4% in basal insulin requirements in the intervention group. The total daily dose of insulin was increased by 3.7% in the control group, while it was reduced by 8.6% in the intervention group (P < 0.001). The study also evaluated the number of hypoglycaemic events (CBG < 3.5 mmol/L) in each group. This was 46% lower in the intervention group (3.3 vs 6.2 episodes/patient). However, there was no statistically significant difference in the number of severe hypoglycaemic events. There was also no statistically significant difference in change in body weight or number of hyperglycaemic events. While the study demonstrates the potential clinical value of InsuPad, it is limited by its open-label design, mixed diabetes cohort, and by the inability to extrapolate the result beyond the study population [43].
One of the acknowledged limitations of the Barmer study was the reliability of self-reported prandial insulin dose information. Aiming to confirm the findings of the Barmer study and to demonstrate the noninferiority of the reduced prandial insulin dose observed in the intervention group, a substudy of the original Barmer study involving all subjects from one study site was performed. Thirty-two subjects underwent a 5-h meal tolerance test with a standardised insulin dose at baseline and at the end of 3 months of randomisation to InsuPad use or control. Baseline and 3-month data were similar to those in the original Barmer study. Despite reduction of prandial insulin dose by almost 20% in the InsuPad group at 3 months, insulin PK showed enhanced insulin absorption, with a 40% reduction in the time to reach maximal insulin concentration (t max reduced from 99 min at baseline to 60 min at 3 months). In comparison, t max in the control group remained around 70 min. C max and PPG at 3 months were similar in the two groups [44].
To evaluate the effect of delayed prandial insulin administration with the use of the InsuPad device on the postprandial glucose profile, a 5-h meal tolerance study was conducted in 15 subjects with type 2 diabetes. Subjects consumed standardised liquid meals and the study was conducted twice: with the InsuPad device (0.2 U/kg injected 30 min post meal) and without the InsuPad device (0.2 U/kg injected before meal). The use of InsuPad with delayed prandial insulin administration showed an earlier rise in glucose level. However, it resulted in a lower mean maximum glucose excursion (129 vs 142 mg/dL) and lower AUC for postprandial glucose excursion over the 5-h study (54 vs 70 mg/dL) [45, 46].
One of the secondary objectives of the Barmer study was to evaluate the psychosocial effect of the InsuPad. This was assessed using the Diabetes Treatment Satisfaction Questionnaire (DTSQ) and the Problem Areas in Diabetes (PAID) questionnaire at the end of the 3-month study. Despite the technical demands associated with the use of the InsuPad, the overall diabetes treatment satisfaction was comparable between the intervention and control groups. Similarly, diabetes-related distress was comparable in the two groups. In keeping with the reduction in the frequency of nonsevere hypoglycaemia in the intervention group, subjects in this group reported lower unacceptably low blood glucose levels (1.4 vs 1.9 in the control group; P < 0.05). Furthermore, 34.4% of the subjects in the intervention group reported reduced pain intensity in relation to insulin injections. This should be compared to only 4.2% who reported increased pain intensity with the use of the InsuPad. More than 95% of the subjects in the intervention group accepted an offer to continue InsuPad use after the end of the study [47].
A long-term follow-up open-label extension of the Barmer study was performed in 52 patients who could be contacted after a minimum of 13 months (mean usage time: 17.8 months, range: 13–21 months). In those subjects, the initial benefits observed with InsuPad use were maintained over 18 months. HbA1c was stable at 6.4%, as was body weight. However, the total daily insulin dose was further reduced compared to baseline. Only 2 people stopped using the device because of a persistent skin reaction to the adhesive [48].
Conclusion
Local warming devices (InsuPatch and InsuPad) represent a simple method of enhancing the PK/PD of subcutaneously injected insulin. Existing evidence demonstrates the potential benefits of using these devices in reducing PPG excursions, improving metabolic control, reducing doses of prandial insulin and decreasing nonsevere hypoglycaemic events in obese insulin-resistant subjects with well-controlled diabetes. Moreover, the evidence suggests that these devices are well tolerated and accepted by users. Warming devices also provide the potential to be combined with other methods that enhance insulin absorption to further augment their effect. However, existing studies are small and heterogeneously designed and some of them include heterogeneous participants. Before these devices are approved by different regulatory bodies and widely adopted by clinicians and patients, more appropriately designed large-scale longitudinal studies are needed to demonstrate the effects of these devices on clinical and patient-reported outcomes in other subjects with different types of diabetes and different baseline characteristics, and to assess the health economics of these devices.
References
Arnolds S, et al. How pharmacokinetic and pharmacodynamic principles pave the way for optimal basal insulin therapy in type 2 diabetes. Int J Clin Pract. 2010;64(10):1415–24.
Heinemann L, Muchmore DB. Ultrafast-acting insulins: state of the art. J Diabetes Sci Technol. 2012;6(4):728–42.
ter Braak EW, et al. Injection site effects on the pharmacokinetics and glucodynamics of insulin lispro and regular insulin. Diabetes Care. 1996;19(12):1437–40.
de la Pena A, et al. Pharmacokinetics and pharmacodynamics of high-dose human regular U-500 insulin versus human regular U-100 insulin in healthy obese subjects. Diabetes Care. 2011;34(12):2496–501.
Gagnon-Auger M, et al. Dose-dependent delay of the hypoglycemic effect of short-acting insulin analogs in obese subjects with type 2 diabetes: a pharmacokinetic and pharmacodynamic study. Diabetes Care. 2010;33(12):2502–7.
Bott S, et al. Impact of smoking on the metabolic action of subcutaneous regular insulin in type 2 diabetic patients. Horm Metab Res. 2005;37(7):445–9.
Dillon RS. Improved serum insulin profiles in diabetic individuals who massaged their insulin injection sites. Diabetes Care. 1983;6(4):399–401.
Monnier L, Lapinski H, Colette C. Contributions of fasting and postprandial plasma glucose increments to the overall diurnal hyperglycemia of type 2 diabetic patients: variations with increasing levels of HbA(1c). Diabetes Care. 2003;26(3):881–5.
Ceriello A, et al. Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes. 2008;57(5):1349–54.
Brownlee M, Hirsch IB. Glycemic variability: a hemoglobin A1c-independent risk factor for diabetic complications. JAMA. 2006;295(14):1707–8.
Home PD. The pharmacokinetics and pharmacodynamics of rapid-acting insulin analogues and their clinical consequences. Diabetes Obes Metab. 2012;14(9):780–8.
Heller SR, et al. Hypoglycaemia with insulin aspart: a double-blind, randomised, crossover trial in subjects with Type 1 diabetes. Diabet Med. 2004;21(7):769–75.
Mannucci E, Monami M, Marchionni N. Short-acting insulin analogues vs. regular human insulin in type 2 diabetes: a meta-analysis. Diabetes Obes Metab. 2009;11(1):53–9.
Plank J, et al. Systematic review and meta-analysis of short-acting insulin analogues in patients with diabetes mellitus. Arch Intern Med. 2005;165(12):1337–44.
Bruttomesso D, et al. Restoration of early rise in plasma insulin levels improves the glucose tolerance of type 2 diabetic patients. Diabetes. 1999;48(1):99–105.
Homko C, et al. Comparison of insulin aspart and lispro: pharmacokinetic and metabolic effects. Diabetes Care. 2003;26(7):2027–31.
Luijf YM, et al. Premeal injection of rapid-acting insulin reduces postprandial glycemic excursions in type 1 diabetes. Diabetes Care. 2010;33(10):2152–5.
Cobry E, et al. Timing of meal insulin boluses to achieve optimal postprandial glycemic control in patients with type 1 diabetes. Diabetes Technol Ther. 2010;12(3):173–7.
Scaramuzza AE, et al. Timing of bolus in children with type 1 diabetes using continuous subcutaneous insulin infusion (TiBoDi Study). Diabetes Technol Ther. 2010;12(2):149–52.
Santos Cavaiola T, Edelman S. Inhaled insulin: a breath of fresh air? A review of inhaled insulin. Clin Ther. 2014;36(8):1275–89.
Rini CJ, et al. Intradermal insulin infusion achieves faster insulin action than subcutaneous infusion for 3-day wear. Drug Deliv Transl Res. 2015;5(4):332–45.
Heinemann L, Jacques Y. Oral insulin and buccal insulin: a critical reappraisal. J Diabetes Sci Technol. 2009;3(3):568–84.
Sousa F, et al. How to overcome the limitations of current insulin administration with new non-invasive delivery systems. Ther Deliv. 2015;6(1):83–94.
Heinemann L, et al. U-100, pH-neutral formulation of VIAject((R)): faster onset of action than insulin lispro in patients with type 1 diabetes. Diabetes Obes Metab. 2012;14(3):222–7.
Heise T, et al. Faster-acting insulin aspart: earlier onset of appearance and greater early pharmacokinetic and pharmacodynamic effects than insulin aspart. Diabetes Obes Metab. 2015;17:682–8.
Adocia. HinsBet: “Human insulin is better”. http://www.adocia.fr/WP/products/hinsbet-ultra-fast-acting-human-insulin/. Accessed 3 June 2015.
Andersen G, et al. The ultra-rapid biochaperone insulin lispro (BC LIS) shows a faster onset of action and stronger early metabolic effect than insulin lispro (LIS). In: Abstracts from ADA2014, 13–17 June 2014, San Francisco, CA, USA.
Morrow L, et al. Comparative pharmacokinetics and insulin action for three rapid-acting insulin analogs injected subcutaneously with and without hyaluronidase. Diabetes Care. 2013;36(2):273–5.
Engwerda EE, et al. Improved pharmacokinetic and pharmacodynamic profile of rapid-acting insulin using needle-free jet injection technology. Diabetes Care. 2011;34(8):1804–8.
Engwerda EE, Tack CJ, de Galan BE. Needle-free jet injection of rapid-acting insulin improves early postprandial glucose control in patients with diabetes. Diabetes Care. 2013;36(11):3436–41.
Koivisto VA. Sauna-induced acceleration in insulin absorption from subcutaneous injection site. Br Med J. 1980;280(6229):1411–3.
Koivisto VA. Sauna-induced acceleration in insulin absorption. Br Med J. 1980;281(6240):621–2.
Sindelka G, et al. Effect of insulin concentration, subcutaneous fat thickness and skin temperature on subcutaneous insulin absorption in healthy subjects. Diabetologia. 1994;37(4):377–80.
Raz I, et al. Effect of a local heating device on insulin and glucose pharmacokinetic profiles in an open-label, randomized, two-period, one-way crossover study in patients with type 1 diabetes using continuous subcutaneous insulin infusion. Clin Ther. 2009;31(5):980–7.
Freckmann G, et al. Clinical performance of a device that applies local heat to the insulin infusion site: a crossover study. J Diabetes Sci Technol. 2012;6(2):320–7.
Landau Z, et al. Improved pharmacokinetic and pharmacodynamic profiles of insulin analogues using InsuPatch, a local heating device. Diabetes Metab Res Rev. 2014;30(8):686–92.
Cengiz E, et al. Acceleration of insulin pharmacodynamic profile by a novel insulin infusion site warming device. Pediatr Diabetes. 2013;14(3):168–73.
Cengiz E, et al. Faster in and faster out: accelerating insulin absorption and action by insulin infusion site warming. Diabetes Technol Ther. 2014;16(1):20–5.
US NIH. ClinicalTrials.gov: Effect of the InsuPatch on automated closed-loop glucose control in type 1 diabetes (IPCL). https://clinicaltrials.gov/ct2/show/NCT01787318. Accessed 13 July 2015.
Pfützner A, et al. Effect of the InsuPad device on postprandial glucose excursion in type II diabetic subjects. Diabetes Technol Ther. 2013;15(suppl 1):A167.
Raz I, et al. Improved postprandial glucose control using the InsuPad device in insulin-treated type 2 diabetes: injection site warming to improve glycemic control. J Diabetes Sci Technol. 2015;9(3):639–43. doi:10.1177/1932296815578881.
Hermanns N, et al. Effect of local heating on postprandial blood glucose excursions using the InsuPad device: results of an outpatient crossover study. J Diabetes Sci Technol. 2014;8(6):1126–32.
Pfutzner A, et al. The Barmer study: impact of standardized warming of the injection site to enhance insulin absorption and reduce prandial insulin requirements and hypoglycemia in obese patients with diabetes mellitus. Curr Med Res Opin. 2014;30(5):753–60.
Pfutzner A, et al. Standardized modulation of the injection site allows for insulin dose reduction without deterioration of metabolic control. Curr Med Res Opin. 2014;30(10):2001–8.
Bitton G, et al. Effect of the Insupad device on post meal glucose and insulin levels with delayed insulin injections. Diabetes Technol Ther. 2014;16(P-216):A-83.
Pfutzner A, et al. Improved insulin absorption by means of standardized injection site modulation results in a safer and more efficient prandial insulin treatment. A review of the existing clinical data. J Diabetes Sci Technol. 2015;9(1):116–22.
Pfutzner A, et al. The impact of local warming at the insulin injection site by the use of the InsuPad device on treatment satisfaction and diabetes related distress. Diabetes Technol Ther. 2014; 16(P-226):A-88.
Pfutzner A, et al. Long-term use of InsuPad is associated with high treatment adherence, maintenance of excellent glycemic control and further reduction of prandial insulin requirements. Diabetes Technol Ther. 2015;17:A102.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
Ahmed H. El-Laboudi has no conflict of interest to declare. Nick Oliver has received honoraria for consultancy from Abbotts Diabetes Care and Roche.
Compliance with ethics guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
El-Laboudi, A.H., Oliver, N. Towards a Physiological Prandial Insulin Profile: Enhancement of Subcutaneously Injected Prandial Insulin Using Local Warming Devices. Diabetes Ther 6, 257–272 (2015). https://doi.org/10.1007/s13300-015-0125-z
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-015-0125-z