Abstract
Introduction
Guidelines for self-treatment of hypoglycaemia specify initial treatment with quick-acting carbohydrate until blood glucose levels normalize and then follow-up with longer-acting carbohydrate. The few studies investigating follow-up show 29–57% omission or undertreatment with follow-up carbohydrate but do not investigate the association of this with repeat hypoglycaemia. This study aimed to develop, validate and administer a questionnaire to delineate this association. The timeframe targeted was 2 h post primary hypoglycaemic event (PPHE), the time influenced by long-acting carbohydrate.
Methods
A questionnaire was generated, test–retest reliability assessed, and it was piloted on convenience samples from the target population. The final version was administered to all insulin-treated individuals attending an outpatient diabetes clinic over 4 weeks (169).
Results
Questionnaire development: readability (69.6—standard/easy), test–retest reliability (Cohen’s kappa 0.57–0.91) and return rate (72.2%) were all acceptable. Questionnaire data: questionnaires were returned by 122 participants (63 males/59 females). Method of insulin administration was subcutaneous insulin injections (91%) and continuous subcutaneous insulin infusion (CSII) (9%). Repeat hypoglycaemia within 2 h PPHE was reported by 8.2% of respondents. There was no significant difference for age, gender and diabetes duration between those reporting repeat hypoglycaemia and those without. Consumption of follow-up longer-acting carbohydrate was reported by 58.2% of responders with 48% of these using long-acting and 52% medium-acting carbohydrate foods. Method of insulin administration and consumption of follow-up food were significantly associated with repeat hypoglycaemia (P = 0.015, 0.039) but presence or absence of symptoms and duration of action of carbohydrate were not significantly associated (P = 0.103, 0.629). Hierarchical logistic regression analysis showed omission of follow-up food PPHE was not a significant predictor of increased likelihood of repeat hypoglycaemia within 2 h PPHE, irrespective of method of insulin administration (P = 0.085).
Conclusion
This study supports guidelines that recommend judicious, rather than routine use of follow-up longer-acting carbohydrate PPHE.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hypoglycaemia is a common complication of insulin treatment resulting from relative insulin excess and suboptimal glucose counterregulation [1]. Mean rates of hypoglycaemia in insulin-treated diabetes are reported as 42.89 (type 1) and 16.37 (type 2) events per person per year (population-based study) [2] and 29.0 (type 1 >15 years duration) and 10.2 (type 2 >5 years duration) events per person-year (secondary health based study) [3]. Hypoglycaemia is cited as the main impediment to euglycemia [4] and the most feared complication of insulin-treated diabetes [5].
It has been reported that 90.8% of adults with type 1 and 84.5% with type 2 diabetes self-treat their hypoglycaemia [6]. Recommendations for self-treatment advise ingestion of quick-acting carbohydrate, reassessment of blood glucose and repeat treatment until blood glucose levels normalise. Subsequent ingestion of longer-acting carbohydrate is then recommended [7–14] as quick-acting carbohydrate used for initial treatment peaks at 30 min and may return to baseline by 90–120 min [15], theoretically increasing the possibility of a repeat hypoglycaemic event within this timeframe. Longer-acting carbohydrate potentially stays above baseline to 210 min post-ingestion [16].
There are few reports in the literature on the extent of adherence to recommendations for follow-up treatment with longer-acting carbohydrate [17–19]. Sommerfield et al. in a survey of 101 insulin-treated individuals reported 29% undertreating with long-acting follow-up food [17], defining undertreatment as less than 10–20 g of long-acting carbohydrate (Diabetes UK Treatment Guidelines For Hypoglycaemia) [13]. Sumner et al. surveyed 125 individuals with type 1 diabetes reporting 57% omitted long-acting follow-up carbohydrate [18], and Vindedzis et al. reported 44.2% omitted follow-up carbohydrate in a survey of 119 insulin-treated individuals [19]. The association of omission or inadequate ingestion of follow-up food with repeat hypoglycaemia was not investigated in any of these studies.
Repeat hypoglycaemia per se does not have a formal definition, and the term is sometimes used interchangeably with recurrent hypoglycaemia [20] and multiple episodes of hypoglycaemia [21]. Current literature on repeat/recurrent hypoglycaemia examines a longer timeframe than would be affected by lack of follow-up food post-primary hypoglycaemic event (PPHE). Reports on paramedic treatment of hypoglycaemia identify repeat hypoglycaemia as occurring within 24–72 h PPHE [22], and reviews of mechanisms and prevention of hypoglycaemia identify repeat hypoglycaemia over 24 h PPHE, or longer [23, 24]. This timescale for recurrence in the insulin-treated individual will be largely influenced by insulin status and also defective counterregulation, clinically indicated by reduced awareness of hypoglycaemic symptoms [23]. Method of insulin administration may be a modifier of hypoglycaemia within a shorter timeframe; there is mixed evidence of the association of continuous subcutaneous insulin infusion (CSII) with reduction in severe hypoglycaemia as compared with multiple daily injections [25, 26].
It could be reasonably assumed that the effect of follow-up longer-acting carbohydrate on blood glucose levels would be confined to 2–3 h PPHE depending on the source of the carbohydrate [16]. We therefore hypothesized that omission of follow-up longer-acting carbohydrate would increase the frequency of repeat hypoglycaemia within 2 h PPHE in free-living insulin-treated individuals. The aim of this study was therefore, first, to develop and validate a questionnaire to obtain data on treatment of primary hypoglycaemia, the presence or absence of symptoms of hypoglycaemia, and the frequency of repeat hypoglycaemia within 2 h PPHE and second, to administer this questionnaire to free-living insulin-treated individuals to assess the likelihood of repeat hypoglycaemia with and without follow-up food while controlling for other significant modifiers of hypoglycaemia.
Materials and Methods
Development of the Questionnaire
The one-page questionnaire was couched in simple language with explanation of technical terms and aimed at completion within 10 min. It commenced with a brief preamble assuring anonymity and explaining the aim was investigation of individual experience of hypoglycaemia. Contact and ethics approval details were provided. Questionnaire items were generated from the literature, patient education material and clinical experience and were a mixture of multichoice and numeric and text open-ended questions. Readability of the questionnaire was assessed by the Flesch Reading Ease Formula and Flesch–Kincaid Grade Level Formula, which are considered suitable for use in health care settings [27]. Content validity was assessed qualitatively by a diabetologist, two diabetes educators and a dietitian. A convenience sample of 19 insulin-treated people from the population to be tested were recruited to assess test–retest reliability of the questionnaire, which was conducted by comparing self-administered responses with interview responses to the same questionnaire items. Interviews were carried out by one of five experienced diabetes educators blinded to the original responses. The questionnaire was then piloted on a convenience sample of nine people with insulin-treated diabetes (7% of sample size) to gain insight into item comprehension; this resulted in several minor rewordings. The return rate of the questionnaire was calculated by number of returned questionnaires against number distributed.
Administration of the Questionnaire
The questionnaire was distributed to all insulin-treated adults attending routine outpatient diabetes clinic appointments over a period of 4 weeks (n = 169). Treatment of diabetes was by either subcutaneous insulin injection (SII) or CSII. All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Study information was given and consent presumed on return of questionnaire. Ethics approval was obtained from Curtin University Human Research Ethics Committee and the project was registered as a clinical audit at Royal Perth Hospital. The questionnaire was designed for self-administration but was initially given to insulin-treated individuals, with a brief explanation, by one of five credentialled diabetes educators. The questionnaire was anonymous, filled out while waiting to see the doctor and consent was presumed on return of the questionnaire to a designated sealed box.
Statistical Methods
Questionnaire Development
Test–retest reliability of the questionnaire was evaluated by percent agreement and also using the kappa statistic (κ), which measures the amount by which agreement exceeds that expected by chance. Kappa was calculated for the self administered—interview data with 95% confidence intervals based on 1,000 bootstraps.
Data from Questionnaire
Descriptive statistics were used for participant characteristics and hypoglycaemic frequency. The Chi-square test (χ 2) was used to compare categorical variables and extended Fisher’s exact test for age and duration of diabetes (>2 × 2 contingency table with some cells <5). Glycaemic index (GI) was used to assess duration of action of follow-up carbohydrate with GI of ≤55 categorized as long-acting and 56–69 as medium-acting carbohydrate [28]. Hierarchical logistic regression analysis was performed to predict the likelihood of repeat hypoglycaemia with respect to consumption/non-consumption of follow-up food while controlling for other significant variables. Analysis was performed using SPSS Statistics—version 21 (IBM Corporation, Somers, NY, USA) and extended Fisher’s exact test by Gunma online database [29].
Results
Development of Questionnaire
Readability of the questionnaire was assessed as 69.6 on Flesch Reading Ease Formula (standard—easy level) and 6.2 on Flesch–Kincaid Grade Level Formula consistent with a grade 6 level, thus theoretically understandable by 85–90% of the population [27]. Test–retest reliability and response rate for individual items are shown in Table 1. Response rates and percent agreement were uniformly high. Values for κ exceeded 0.61, indicating substantial agreement for six of the seven questions, with moderate agreement for the other [30].
Data from Questionnaire
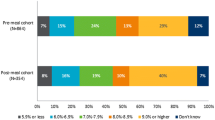
Questionnaires were returned by 122 out of 169 participants (63 males, 59 females) giving a return rate of 72.2%, well above the estimated acceptable rate of 65% for self-completed postal questionnaires [31]. Participant characteristics are shown in Table 2 and self-reported frequency, symptoms and treatment of hypoglycaemia in Table 3. Repeat hypoglycaemia was reported by 8.2% (n = 10) of participants and correlated well with a separate question on self-reported frequency of repeat hypoglycaemia (P < 0.001). There was no significant difference in the distribution of age, gender and duration of diabetes between those reporting repeat hypoglycaemia and those without (P = 0.343, 1.00, 0.458 respectively). All participants reported consuming initial treatment food. Follow-up food ingestion was reported by 58.2% of item responders with 48% of these using long-acting and 52% medium-acting carbohydrate. Ninety percent of those using medium-acting carbohydrate chose food sources in the lower half of this category, i.e. GI <62 (Fig. 1).
Both method of insulin administration and consumption/non-consumption of follow-up food PPHE were significantly associated with presence/absence of repeat hypoglycaemia (χ 2: P = 0.015, 0.039) but presence/absence of hypoglycaemic symptoms and duration of action of carbohydrate were not significantly associated (χ 2: P = 0.103, 0.629). Hierarchical logistic regression analysis was then conducted to predict the likelihood of repeat hypoglycaemia using consumption/non-consumption of follow-up food PPHE as a predictor variable while controlling for method of insulin administration. A test of the full model against a constant only model was statistically significant, indicating that the predictor variables should distinguish between those with and without repeat hypoglycaemia (χ 2 = 4.445, P = 0.035 with df = 1), the Hosmer–Lemeshow goodness of fit test was not significant (P = 0.838) indicating the model prediction was not significantly different from the observed values; however, the Wald criterion demonstrated that consumption/non-consumption of follow-up food PPHE was not a significant predictor of repeat hypoglycaemia (P = 0.085). All standard errors <2 indicated no multicollinearity between variables.
Discussion
Insulin-treated individuals in the target population are routinely taught to ingest follow-up food post-hypoglycaemia; therefore, it might be presumed they may be reluctant to admit they do not carry this out. In view of this, the data collection method considered optimal for this study was an anonymous self-administered questionnaire. This mode has been shown to decrease biased responses and result in more accurate and less ‘socially desirable’ responses to sensitive health-related questions than information obtained by interview [32]. A negative aspect of self-administered questionnaires is a possible decrease in reliability for open and more complex questions [33], but this was not demonstrated in this study. Advanced notification ahead of self-administration of a questionnaire has been shown to raise response rates and credibility without affecting questionnaire response type [33], and the initial contact by diabetes educators with potential participants may partly account for the relatively high response rate.
Potentially many factors influence repeat hypoglycaemia [23]. We have investigated one of these (follow-up food) and sought to control for the other factor (method of insulin administration) that showed a significant association within the specified timeframe. Perhaps surprisingly, lack of symptoms of hypoglycaemia was not a modifier, possibly a function of the inclusion of individuals with insulin-treated type 2 diabetes and the associated lower rate of compromised counterregulation [34].
A limitation of this study was the inability to differentiate between type 1 and insulin-treated type 2 diabetes. It was considered that self-reported data on this may be inaccurate. Similarly, we collected no data on alcohol consumption, a modifier of hypoglycaemia, as this requires strategies to obtain accurate information outside the scope of this study [35].
Hierarchical binary logistic regression was the statistical test of choice as it assesses the likelihood of an event occurring given a set of conditions and does not require the statistical presumption of normality, which was not fulfilled in this data as all variables were categorical. Although only 10 participants reported repeat hypoglycaemia, the sample size (122) was considered adequate according to the rule of thumb N − k − 1 ≥ 50 (N = sample size, k = number of predictor variables) [36]. The questionnaire item yes/no to experiencing repeat hypoglycaemia was used as the outcome variable, but only exhibited moderate test–retest reliability. It did, however, show excellent correlation with the separate questionnaire item on frequency of repeat hypoglycaemia, which exhibited high test–retest reliability, and was therefore taken as robust data.
The high reported rate (40.2%) of omission of follow-up food in this study is consistent with two other comparable studies [17, 19]. The use of medium-acting foods for follow-up is consistent with some recommendations [9, 13, 14], but notably, in this study, the majority of respondents selecting medium-acting follow-up foods tended towards those that were slower-acting in this category and this may account for the lack of association of duration of action of carbohydrate with incidence of repeat hypoglycaemia.
The relative percentages of reported repeat hypoglycaemia and omission of follow-up longer-acting carbohydrate PPHE suggest many individuals do omit follow-up food with impunity. The situation is rather complex, with some guidelines recommending routine consumption of follow-up food [7, 9, 12] and others stating follow-up food may be required [10, 13, 14]. CSII treatment is cited as one instance where follow-up food may be unnecessary as short-term insulin status is more controllable [14]; however, in this study omission of follow-up food PPHE did not significantly increase the likelihood of repeat hypoglycaemia irrespective of method of insulin administration.
Conclusion
The results of this study support guidelines recommending judicious, rather than routine use of follow-up longer-acting carbohydrate PPHE.
References
Cryer PE, Davis SN, Shamoon H. Hypoglycemia in diabetes. Diabetes Care. 2003;26:1902–12.
Donnelly LA, Morris AD, Frier BM, et al. Frequency and predictors of hypoglycaemia in Type 1 and insulin-treated Type 2 diabetes: a population-based study. Diabet Med. 2005;22:749–55.
UK Hypoglycaemia Study Group. Risk of hypoglycaemia in types 1 and 2 diabetes: effects of treatment modalities and their duration. Diabetologia. 2007;50:1140–7.
Cryer PE. Elimination of hypoglycemia from the lives of people affected by diabetes. Diabetes. 2011;60:24–7.
Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Education Couns. 2007;68:10–5.
Leiter L, Yale J, Chiasson J, Harris S, Kleinstiver P, Sauriol L. Assessment of the impact of fear of hypoglycemic episodes on glycemic and hypoglycemia management. Can J Diab. 2005;29:186–92.
American Diabetes Association. Standards of medical care in diabetes—2013. Diabetes Care. 2013;36(Suppl 1):S11–66.
Canadian Diabetes Association [Homepage on the Internet]. Hypoglycemia. Canada: Canadian Diabetes Association. Available at: http://www.diabetes.ca/. Accessed 23 Jan 2013.
Diabetes Australia. [Homepage on the Internet]. Hypoglycemia. Canberra: Diabetes Australia. Available at: http://www.diabetesaustralia.com.au/. Accessed 16 Jan 2013.
Diabetes Education Study Group of The European Association for the Study of Diabetes [Homepage on the Internet]. Teaching letter 2, hypoglycemia. Available at: http://www.desg.org/. Accessed Jan 23 2013.
Asian-Pacific Type 2 Diabetes Policy Group. [Homepage on the Internet]. Type 2 diabetes practical targets and treatments. International Diabetes Federation. Available at: http://www.idf.org/idf-wpr-type-2-diabetes-pratical-targets-and-treatments. Accessed Jan 23 2013.
Singapore Diabetes Society [Homepage on the Internet]. Diabetes and hypoglycemia. Singapore: Diabetic Society of Singapore. Available at: http://www.diabetes.org.sg/. Accessed 23 Jan 2013.
Diabetes UK [Homepage on the Internet]. Treatment of hypoglycaemia. London: Diabetes UK. Available at: http://www.diabetes.org.uk/. Accessed Jan 23 2013.
National Health and Medical Research Council. National Evidence-Based Clinical Care Guidelines for Type 1 Diabetes for Children, Adolescents and Adults 2011. Department of Health and Aging. Available at: http://www.nhmrc.gov.au/_files_nhmrc/publications/attachments/cp102.pdf. Accessed 13 Dec 2012.
Brand-Miller J, McMillan-Price J, Steinbeck K, Caterson I. Carbohydrates—the good, the bad and the whole grain. Asia Pac J Clin Nutr. 2008;17(Suppl 1):16–9.
Chlup R, Peterson K, Zapletalova J, Kudlova P, Seckar P. Extended prandial glycemic profiles of foods as assessed using continuous glucose monitoring enhance the power of the 120-minute glycemic index. J Diabetes Sci Technol. 2010;4:615–24.
Sommerfield AJ, Ewing FME, Strachan MWJ, Deary IJ, Aitken G, Frier BM. Self-treatment of mild symptomatic hypoglycaemia by people with insulin-treated diabetes. Diabet Med. 2003;20:686–7.
Sumner J, Baber C, Williams V. What do patients with type 1 diabetes know about hypoglycaemia? Pract Diabetes Int. 2000;17:187–90.
Vindedzis SA, Marsh B, Sherriff JL, Dhaliwal SS, Stanton KG. Food selection for treatment of hypoglycaemia in insulin-treated diabetes: what happens in real life? Practical Diabetes. 2012;29:271–4.
Cryer PE, Axelrod L, Grossman AB, et al. Evaluation and management of adult hypoglycemic disorders: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2009;94:709–28.
Kilpatrick ES, Rigby AS, Goode K, Atkin SL. Relating mean blood glucose and glucose variability to the risk of multiple episodes of hypoglycaemia in type 1 diabetes. Diabetologia. 2007;50:2553–61.
Roberts K, Smith A. Outcome of diabetic patients treated in the prehospital arena after a hypoglycaemic episode, and an exploration of treat and release protocols: a review of the literature. Emerg Med J. 2003;20:274–6.
Amiel S. Hypoglycemia: from the laboratory to the clinic. Diabetes Care. 2009;32:1364–71.
Kinsley BT, Weinger K, Bajaj M, et al. Blood glucose awareness training and epinephrine responses to hypoglycemia during intensive treatment in type 1 diabetes. Diabetes Care. 1999;22:1022–8.
Fatourechi MM, Kudva YC, Murad MH, Elamin MB, Tabini CC, Montori VM. Clinical review: hypoglycemia with intensive insulin therapy: a systematic review and meta-analyses of randomized trials of continuous subcutaneous insulin infusion versus multiple daily injections. J Clin Endocrinol Metab. 2009;94:729–40.
Pickup JC, Sutton AJ. Severe hypoglycaemia and glycaemic control in Type 1 diabetes: meta-analysis of multiple daily insulin injections compared with continuous subcutaneous insulin infusion. Diabet Med. 2008;25:765–74.
Ley P, Florio T. The use of readability formulas in health care. Psychol Health Med. 1996;1:7–28.
Atkinson FS, Foster-Powell K, Brand-Miller JC. International tables of glycemic index and glycemic load values: 2008. Diabetes Care. 2008;31:2281–3.
Statistics database. Gumna University Website. Available at: http://aoki2.si.gunma-u.ac.jp/exact/exact.html. Accessed 16 Jan 2013.
Saw SM, Ng TP. The design and assessment of questionnaires in clinical research. Singapore Med J. 2001;42:131–5.
Kelley K, Clark B, Brown V, Sitzia J. Good practice in the conduct and reporting of survey research. Int J Qual Health Care. 2003;15:261–6.
Okamoto K, Ohsuka K, Shiraishi T, Hukazawa E, Wakasugi S, Furuta K. Comparability of epidemiological information between self- and interviewer-administered questionnaires. J Clin Epidemiol. 2002;55:505–11.
de Leeuw E. To mix or not to mix data collection modes in surveys. J Off Stat. 2005;21:233–55.
de Galan BE, Schouwenberg BJ, Tack CJ, Smits P. Pathophysiology and management of recurrent hypoglycaemia and hypoglycaemia unawareness in diabetes. Neth J Med. 2006;64:269–79.
Beck F, Peretti-Watel P. The impact of data collection methodology on the reporting of illicit drug use by adolescents. Population-E. 2002;57:571–92.
Peng CY, So TS, Stage FK, St. John EP. The use and interpretation of logistic regression in higher education journals: 1988–1999. Res High Education. 2002;43:259–93.
Acknowledgments
The authors wish to thank all participants. Thanks also to Angela Sun, BeeChoo Lim, Anne Perry, and A.G. Tan for their help during the study. Sally Vindedzis is the guarantor for this article, and takes responsibility for the integrity of the work as a whole. No funding or sponsorship was received for this study or publication of this article.
Conflict of interest
Sally Vindedzis, Beryl Marsh, Jill Sherriff, Satvinder Dhaliwal, and Kim Stanton declare no conflicts of interest.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Study information was given and consent presumed by return of questionnaire.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Vindedzis, S., Marsh, B., Sherriff, J. et al. Omitting Follow-up Food After Initial Hypoglycaemic Treatment Does not Increase the Likelihood of Repeat Hypoglycaemia. Diabetes Ther 4, 67–75 (2013). https://doi.org/10.1007/s13300-013-0019-x
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-013-0019-x