Abstract
The fetal heart rate (FHR) signal is used to assess the well-being of a fetus during labor. Manual interpretation of the FHR is subject to high inter- and intra-observer variability, leading to inconsistent clinical decision-making. The baseline of the FHR signal is crucial for its interpretation. An automated method for baseline determination may reduce interpretation variability. Based on this claim, we present the Auto-Regressed Double-Sided Improved Asymmetric Least Squares (ARDSIAsLS) method as a baseline calculation algorithm designed to imitate expert obstetrician baseline determination. As the FHR signal is prone to a high rate of missing data, a step of gap interpolation in a physiological manner was implemented in the algorithm. The baseline of the interpolated signal was determined using a weighted algorithm of two improved asymmetric least squares smoothing models and an improved symmetric least squares smoothing model. The algorithm was validated against a ground truth determined from annotations of six expert obstetricians. FHR baseline calculation performance of the ARDSIAsLS method yielded a mean absolute error of 2.54 bpm, a max absolute error of 5.22 bpm, and a root mean square error of 2.89 bpm. In a comparison between the algorithm and 11 previously published methods, the algorithm outperformed them all. Notably, the algorithm was non-inferior to expert annotations. Automating the baseline FHR determination process may help reduce practitioner discordance and aid decision-making in the delivery room.





Similar content being viewed by others
References
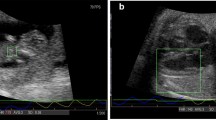
Jezewski J, Kupka T, Horoba K (2008) Extraction of fetal heart-rate signal as the time event series from evenly sampled data acquired using doppler ultrasound technique. IEEE Trans Biomed Eng 55:805–810. https://doi.org/10.1109/TBME.2007.903532
Rochard F, Schifrin BS, Goupil F et al (1976) Nonstressed fetal heart rate monitoring in the antepartum period. Am J Obstet Gynecol 126:699–706. https://doi.org/10.1016/0002-9378(76)90523-8
Trimbos JB, Keirse MJNC (1978) Observer variability in assessment of antepartum cardiotocograms. BJOG 85:900–906. https://doi.org/10.1111/J.1471-0528.1978.TB15851.X
Rooth G, Huch A, Huch R (1987) Figo news. Int J Gynecol Obstet 25:159–167. https://doi.org/10.1016/0020-7292(87)90012-9
Ayres-De-Campos D, Spong CY, Chandraharan E (2015) FIGO consensus guidelines on intrapartum fetal monitoring: cardiotocography. Int J Gynecol Obstet 131:13–24. https://doi.org/10.1016/J.IJGO.2015.06.020
Moss AJ (1993) Measurement of the QT interval and the risk associated with QTc interval prolongation: a review. Am J Cardiol 72:B23–B25. https://doi.org/10.1016/0002-9149(93)90036-C
Jadeja NM (2021) How to Read an EEG. Cambridge University Press, Cambridge
Tankisi H, Burke D, Cui L et al (2020) Standards of instrumentation of EMG. Clin Neurophysiol 131:243–258. https://doi.org/10.1016/J.CLINPH.2019.07.025
Stålberg E, van Dijk H, Falck B et al (2019) Standards for quantification of EMG and neurography. Clin Neurophysiol 130:1688–1729. https://doi.org/10.1016/J.CLINPH.2019.05.008
Creel DJ (2012) The electroretinogram and electro-oculogram: clinical applications. In: Kolb Helga, Fernandez E, Nelson R (eds) Webvision: the Organization of the retina and visual system. University of Utah Health Sciences Center, Salt Lake City
Ayres-De-Campos D, Arulkumaran S (2015) FIGO consensus guidelines on intrapartum fetal monitoring: introduction. Int J Gynecol Obstet 131:3–4. https://doi.org/10.1016/J.IJGO.2015.06.017
Schneider KTM, Beckmann MW, German Society of Gynecology et al (2014) S1-Guideline on the use of CTG during pregnancy and labor: long version – AWMF Registry No. 015/036. Geburtshilfe Frauenheilkd 74:721. https://doi.org/10.1055/S-0034-1382874
Das S, Roy K, Saha CK (2011) A novel approach for extraction and analysis of variability of baseline. 2011 International conference on recent trends in information systems, ReTIS 2011. IEEE, New York, pp 336–339. https://doi.org/10.1109/RETIS.2011.6146892
Ayres-de-campos D, Bernardes J, Garrido A et al (2000) SisPorto 2.0: a program for automated analysis of Cardiotocograms. J Maternal-Fetal Neonatal Med 9:311–318. https://doi.org/10.3109/14767050009053454
Pardey J, Moulden M, Redman CWG (2002) A computer system for the numerical analysis of nonstress tests. Am J Obstet Gynecol 186:1095–1103. https://doi.org/10.1067/MOB.2002.122447
Mongelli M, Dawkins R, Chung T et al (1997) Computerised estimation of the baseline fetal heart rate in labour: the low frequency line. BJOG 104:1128–1133. https://doi.org/10.1111/J.1471-0528.1997.TB10935.X
K Maeda (1980) Computer-aided fetal heart rate analysis and automatic fetal-distress diagnosis during labor and pregnancy utilizing external technique in fetal monitoring. MEDINFO 80.
Lu Y, Wei S (2012) Nonlinear baseline estimation of FHR signal using empirical mode decomposition. International Conference on Signal Processing Proceedings ICSP 3:1645–1649. https://doi.org/10.1109/ICOSP.2012.6491896
Wei SY, Lu YS, Liu XL (2012) Fetal heart rate analysis using a non-linear baseline and variability estimation method. 2012 5th International Conference on Biomedical Engineering and Informatics BMEI 2012 532:536. https://doi.org/10.1109/BMEI.2012.6513082
Taylor GM, Mires GJ, Abel EW et al (2000) The development and validation of an algorithm for real-time computerised fetal heart rate monitoring in labour. BJOG 107:1130–1137. https://doi.org/10.1111/J.1471-0528.2000.TB11112.X
Boudet S, Houzé de l’Aulnoit A, Demailly R et al (2019) Fetal heart rate baseline computation with a weighted median filter. Comput Biol Med 114:103468. https://doi.org/10.1016/J.COMPBIOMED.2019.103468
Cazares SM (2002) Automated identification of abnormal patterns in the intrapartum cardiotocogram. Doctoral dissertation, University of Oxford
Cazares S, Tarassenko L, Impey L et al (2001) Automated identification of abnormal cardiotocograms using neural network visualization techniques. Annual International Conference of the IEEE Engineering in Medicine and Biology-Proceedings. IEEE, New York, pp 1629–1632. https://doi.org/10.1109/IEMBS.2001.1020526
Yaosheng L, Xiaodong L, Shouyi W, Xiaolei L (2014) Fetal heart rate baseline estimation with analysis of fetal movement signal. Biomed Mater Eng 24:3763–3769. https://doi.org/10.3233/BME-141205
Li X, Lu Y (2015) [An Algorithm for correcting fetal heart rate Baseline]. Sheng Wu Yi Xue Gong Cheng Xue Za Zhi 32:1106–1112
Jiménez L, González R, Gaitán MJ et al (2002) Computerized algorithm for baseline estimation of fetal heart rate. Comput Cardiol 29:477–480. https://doi.org/10.1109/CIC.2002.1166813
Houze de L’Auinoit DL, Beuscart RJ, Brabant G et al (2005) Real-time analysis of the fetal heart rate. [1990] Proceedings of the Twelfth Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE, New York, pp 1994–1995. https://doi.org/10.1109/IEMBS.1990.692125
Houzé de l’Aulnoit A, Boudet S, Demailly R et al (2019) Automated fetal heart rate analysis for baseline determination and acceleration/deceleration detection: a comparison of 11 methods versus expert consensus. Biomed Signal Process Control 49:113–123. https://doi.org/10.1016/J.BSPC.2018.10.002
He S, Zhang W, Liu L et al (2014) Baseline correction for Raman spectra using an improved asymmetric least squares method. Anal Methods 6:4402–4407. https://doi.org/10.1039/C4AY00068D
Ye J, Tian Z, Wei H, Li Y (2020) Baseline correction method based on improved asymmetrically reweighted penalized least squares for the Raman spectrum. Appl Opt 59:10933. https://doi.org/10.1364/AO.404863
Yang G, Dai J, Liu X et al (2020) Multiple constrained reweighted penalized least squares for spectral baseline correction. Appl Spectrosc 74:1443–1451. https://doi.org/10.1177/0003702819885002
Jiang X, Li F, Wang Q et al (2021) Baseline correction method based on improved adaptive iteratively reweighted penalized least squares for the x-ray fluorescence spectrum. Appl Opt 60:5707. https://doi.org/10.1364/AO.425473
Zhang F, Tang X, Tong A et al (2020) An automatic baseline correction method based on the penalized least squares Method. Sensors 20:2015. https://doi.org/10.3390/S20072015
Baek S-J, Park A, Ahn Y-J, Jaebum Choo (2014) Baseline correction using asymmetrically reweighted penalized least squares smoothing. Analyst 140:250–257. https://doi.org/10.1039/C4AN01061B
Zhang ZM, Chen S, Liang YZ (2010) Baseline correction using adaptive iteratively reweighted penalized least squares. Analyst 135:1138–1146. https://doi.org/10.1039/B922045C
Barzideh F, Urdal J, Engan K et al (2018) Estimation of missing data in fetal heart rate signals using shift-invariant dictionary. European Signal Processing Conference 2018-September. IEEE, New York, pp 762–766. https://doi.org/10.23919/EUSIPCO.2018.8553110
Spilka J, Chudáček V, Koucký M et al (2012) Using nonlinear features for fetal heart rate classification. Biomed Signal Process Control 7:350–357. https://doi.org/10.1016/J.BSPC.2011.06.008
Spilka J, Georgoulas G, Karvelis P et al (2014) Discriminating normal from “abnormal” pregnancy cases using an automated FHR evaluation method. Lecture Notes in Computer Science (including subseries Lecture Notes in Artificial Intelligence and Lecture Notes in Bioinformatics) 8445 LNCS:521–531. https://doi.org/10.1007/978-3-319-07064-3_45/COVER
Feng G, Quirk JG, Djuric PM (2017) Recovery of missing samples in fetal heart rate recordings with Gaussian processes. 25th European Signal Processing Conference, EUSIPCO. IEEE, New York, pp 261–265. https://doi.org/10.23919/EUSIPCO.2017.8081209
Oikonomou VP, Spilka J, Stylios C, Lhostka L (2013) An adaptive method for the recovery of missing samples from FHR time series. CBMS. IEEE, New York, pp 337–342. https://doi.org/10.1109/CBMS.2013.6627812
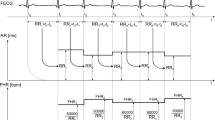
Singstad B (2022) Norwegian Endurance Athlete ECG Database (version 1.0.0). PhysioNet
Goldberger AL, Amaral LAN, Glass L et al (2000) Physiobank, physiotoolkit, and physionet: components of a new research resource for complex physiologic signals. Circulation 101:e215–e220
von Steinburg SP, Boulesteix AL, Lederer C et al (2013) What is the normal fetal heart rate? PeerJ 1:e82. https://doi.org/10.7717/PEERJ.82
Stock JH (2001) Time series: economic forecasting. International encyclopedia of the social & behavioral sciences. Elsevier, Amsterdan, pp 15721–15724
PHC Eilers, HFM Boelens (2005) Baseline correction with asymmetric least squares smoothing. Leiden University Medical Centre report
Erb D (2021) Pybaselines: a python library of algorithms for the baseline correction of experimental data
Laszuk D (2017) Python implementation of Empirical Mode Decomposition algorithm. GitHub Repository.
Miller RG (1981) Simultaneous Statistical Inference. Springer, Berlin
Mittelhammer RC, Judge GG, Miller DJ (2002) The multivariate normal linear regression model: inference. Econometric Foundations. Cambridge University Press, Cambridge, pp 61–85
Bonferroni CE (1936) Teoria statistica delle classi e calcolo delle probabilità. Pubblicazioni del R Istituto Superiore di Scienze Economiche e Commerciali di Firenze. 8:3–62
PHILIPS (2011) Instructions for Use Avalon Fetal Monitor FM20/30, FM40/50
Spilka J, Chudáček V, Janků P et al (2014) Analysis of obstetricians’ decision making on CTG recordings. J Biomed Inform 51:72–79. https://doi.org/10.1016/J.JBI.2014.04.010
Sabiani L, le Dû R, Loundou A et al (2015) Intra- and interobserver agreement among obstetric experts in court regarding the review of abnormal fetal heart rate tracings and obstetrical management. Am J Obstet Gynecol 213:856-e1-856-e8. https://doi.org/10.1016/J.AJOG.2015.08.066
Alkan A, Akben SB (2011) Use of K-means clustering in migraine detection by using EEG records under flash stimulation. Int J Phys Sci 6:641–650. https://doi.org/10.5897/IJPS11.174
Oğuz FE, Alkan A, Schöler T (2023) Emotion detection from ECG signals with different learning algorithms and automated feature engineering. Signal Image Video Process 17:1–9. https://doi.org/10.1007/S11760-023-02606-Y/TABLES/3
Muhammed Sünnetci K, Alkan A, Kubilay Muhammed Sünnetci C (2022) Lung cancer detection by using probabilistic majority voting and optimization techniques. Int J Imaging Syst Technol 32:2049–2065. https://doi.org/10.1002/IMA.22769
Sunnetci KM, Kaba E, Celiker FB, Alkan A (2023) Deep Network-Based comprehensive parotid gland tumor detection. Acad Radiol. https://doi.org/10.1016/J.ACRA.2023.04.028
Mulder EJH, Visser GHA, Bekedam DJ, Prechtl HFR (1987) Emergence of behavioural states in fetuses of type-1-diabetic women. Early Hum Dev 15:231–251. https://doi.org/10.1016/0378-3782(87)90082-X
Acknowledgements
Special thanks to Dr. Mordechai Bardicef, Dr. Amit Damti, Dr. Yael Goldberg, Dr. Eliyahu Gutterman, and Dr. Maayan Lahav-Sher for annotating the clinical FHR signals.
Funding
This work was supported by the Mark S. Kahn Family Fund.
Author information
Authors and Affiliations
Contributions
NK, RS and YY conceived and designed the research. RS performed the experiments and the analysis. RS and NK designed the algorithm. RS drafted the manuscript. NK, YY and RK edited and revised the manuscript. RS, NK, YY and RK approved the final version.
Corresponding authors
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Carmel Hospital Institutional Review Board (0001-22-CMC).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shapira, R., Kedar, R., Yaniv, Y. et al. Double-sided asymmetric method for automated fetal heart rate baseline calculation. Phys Eng Sci Med 46, 1779–1790 (2023). https://doi.org/10.1007/s13246-023-01337-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-023-01337-1