Abstract
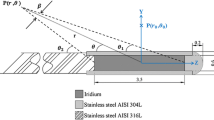
The purpose of this research is to study the effect of various applicator compositions on dosimetric parameters and dose distribution of 192Ir, 137Cs, and 60Co sources, using Monte Carlo simulation techniques. To study the effect of applicators on source dosimetry, the dose rate constant, and radial dose function and isodose curves for the above noted sources were calculated in the presence and absence of plastic, titanium, and a stainless steel applicators. The effects of the applicators on the dosimetric parameters and isodose curves of these sources were dependent of the source type and materials of the applicator. The 192Ir source with the stainless steel applicator has the maximum difference of dose rate (4.2 %) relative to the without applicator case. The 60Co source with plastic applicator has the minimum dose variation. Moreover, this effect is higher for lower energy sources. Ignoring the effect of applicator composition and geometry on dose distribution may cause discrepancies in treatment planning. Plastic applicators have the least radiation attenuation compared to the other applicators, therefore, they are recommended for use in brachytherapy. A table of correction factors has been introduced for different sources and applicators with different materials for the clinical applications.





Similar content being viewed by others
References
Papagiannis P, Baltas D, Granero D, Pérez-Calatayud J, Gimeno J, Ballester F et al (2008) Radiation transmission data for radionuclides and materials relevant to brachytherapy facility shielding. Med Phys 35(11):4898–4906
Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W et al (2010) SEER cancer statistics review SEER cancer statistics review, 1975–2007. National Cancer Institute, Bethesda. http://seer.cancer.gov/csr/1975_2007. Accessed 17 Jan 2016
Wu CH, Shiau AC, Liao YJ, Lin HY, Liu YW, Hsu SM et al (2014) Influence of metal of the applicator on the dose distribution during brachytherapy. PLoS One 9(8):1–7
Kirisits C, Lang S, Dimopoulos J, Berger D, Georg D, Pötter R (2006) The Vienna applicator for combined intracavitary and interstitial brachytherapy of cervical cancer: design, application, treatment planning, and dosimetric results. Int J Radiat Oncol Biol Phys 65(2):624–630
Hu Y, Esthappan J, Mutic S, Richardson S, Gay HA, Schwarz JK et al (2013) Improve definition of titanium tandems in MR-guided high dose rate brachytherapy for cervical cancer using proton density weighted MRI. Radiat Oncol 8(1):16
Haack S, Nielsen SK, Lindegaard JC, Gelineck J, Tanderup K (2009) Applicator reconstruction in MRI 3D image-based dose planning of brachytherapy for cervical cancer. Radiother Oncol 91(2):187–193
Wills R, Lowe G, Inchley D, Anderson C, Beenstock V, Hoskin P (2010) Applicator reconstruction for HDR cervix treatment planning using images from 0.35 T open MR scanner. Radiother Oncol 94(3):346–352
Kim Y, Muruganandham M, Modrick JM, Bayouth JE (2011) Evaluation of artifacts and distortions of titanium applicators on 3.0-Tesla MRI: feasibility of titanium applicators in MRI-guided brachytherapy for gynecological cancer. Int J Radiat Oncol Biol Phys 80(3):947–955
Williamson JF (1990) Dose calculations about shielded gynecological colpostats. Int J Radiat Oncol Biol Phys 19(1):167–178
Kim JS, Lee YS, Lim YK, Park SY, Kim JY (2010) Reconstruction of a fletcher-type applicator with a CT/MR compatible catheter using MR imaging for cervical cancer brachytherapy. J Korean Phys Soc 56(3):880–886
Yu PC, Chao TC, Lee CC, Wu CJ, Tung CJ (2010) A Monte Carlo dosimetry study using Henschke applicator for cervical brachytherapy. Nucl Instrum Meth A 619(1):411–414
Sina S, Faghihi R, Meigooni A, Mehdizadeh S, Zehtabian M, Mosleh Shirazi MA (2009) Simulation of the shielding effects of an applicator on the AAPM TG-43 parameters of CS-137 Selectron LDR Brachytherapy sources. Iran J Radiat Res 7(3):135–140
Ye SJ, Brezovich IA, Shen S, Duan J, Popple RA, Pareek PN (2004) Attenuation of intracavitary applicators in 192Ir-HDR brachytherapy. Med Phys 31(7):2097–2106
Sina S, Faghihi R, Soleimani Meigooni A, Siavashpour Z, Mosleh Shirazi MA (2013) Developing a treatment planing software based on TG-43U1 formalism for Cs-137 brachytherapy. Iran Red Crescent Med J 15(8):712–717
Gaudreault M, Reniers B, Landry G, Verhaegen F, Beaulie L (2014) Dose perturbation due to catheter materials in high-dose-rate interstitial 192Ir brachytherapy. Brachytherapy 13(6):627–631
Kim SM, Kim MH (2014) A study on MCNPX-CINDER90 system for activation analysis. 2014 Fall Meeting of the Korean Nuclear Society, Pyeongchang, Republic of Korea. 29–31 Oct 2014
Nuclear Energy Agency. http://www.oecd-nea.org/tools/abstract/detail/ccc-0746. Accessed 17 Jan 2016
Rivard MJ, Coursey BM, DeWerd LA, Hanson WF, Huq MS, Ibbott GS et al (2004) Update of AAPM task group No. 43 report: a revised AAPM protocol for brachytherapy dose calculations. Med Phys 31(3):633–674
Mathews B, Price M (2011) SU-E-T-379: development of a Monte Carlo based correction strategy for a TG-43 based brachytherapy treatment planning system to account for applicator inhomogeneities. Med Phys 38(6):3575
Chandola R, Tiwari S, Kowar M, Choudhary V (2010) Effect of inhomogeneities and source position on dose distribution of nucletron high dose rate Ir-192 Brachytherapy source by Monte Carlo simulation. J Cancer Res Ther 6(1):54–57
López JF, Donaire JT, Alcalde RG (2011) Monte Carlo dosimetry of the most commonly used 192Ir high dose rate brachytherapy sources. Rev Fis Med 12(3):159–168
Vijande J, Granero D, Perez Calatayud J, Ballester F (2012) Monte Carlo dosimetric study of the Flexisource Co-60 high dose rate source. J Contemp Brachyther 4(1):34–44
Medich DC, Munro J (2007) Monte Carlo characterization of the M-19 high dose rate Iridium-192 brachytherapy source. Med Phys 34(6):1999–2006
Perez Calatayud J, Ballester F, Das RK, DeWerd LA, Ibbott GS, Meigooni AS et al (2012) Dose calculation for photon-emitting brachytherapy sources with average energy higher than 50 keV: report of the AAPM and ESTRO. Med Phys 39(5):2904–2929
Otal A, Martínez-Fernández JM, Granero D (2011) Revision of the dosimetric parameters of the CSM11 LDR Cs-137 source. J Contemp Brachyther 3(1):36–39
Nath R, Anderson LL, Luxton G, Weaver KA, Williamson JF, Meigooni AS (1995) Dosimetry of interstitial brachytherapy sources: recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. Med Phys 22(2):209–234
National Institute of Standards and Technology. http://physics.nist.Gov/PhysRefData/XrayMassCoef/ComTab/water.html. Accessed 17 Jan 2016
Nucletron, Fletcher CT/MR applicator set 189.730, Fletcher CT/MR applicator set XS 110.216 user manual. Doc. No. 090.713ENG-06
Soni N (2012) Quantitative assessment of the source attenuation for the new CT compatible titanium Fletcher-Suit-Delclos (FSD) gynecologic applicator. M Sc thesis on Medical Physics, University of Toledo. http://etd.Ohiolink.Edu/ap/10?0::NO:10:P10_ACCESSION_NUM:mco1353080695. Accessed 17 Jan 2016
Aestrospace Specification Metals Inc. http://asm.matweb.com/search/SpecificMaterial.asp?bassnum=MQ316A.Accessed. Accessed 17 Jan 2016
Selvam TP, Sahoo S, Vishwakarma RS (2009) EGSnrc-based Monte Carlo dosimetry of CSA1 and CSA2 137Cs brachytherapy source models. Med Phys 36(9):3870–3879
NIST.Guidelines for evaluating and expressing the uncertainty of NIST measurement results (1994). http://physics.nist.gov/Pubs/guidelines/contents.html. Accessed 17 Jan 2016
Pelowitz DB (2008). MCNPX user’s manual, LA-CP-07-1473, Version 2.6.0. Los Alamos National Laboratory
National Institute of Standards and Technology. http://physics.nist.Gov/PhysRefData/XrayMassCoef/ComTab/a150.html. Accessed 17 Jan 2016
National Institute of Standards and Technology. http://physics.nist.gov/PhysRefData/XrayMassCoef/ElemTab/z22.html. Accessed 17 Jan 2016
National Institute of Standards and Technology. http://physics.nist.gov/PhysRefData/XrayMassCoef/ElemTab/z26.html. Accessed 17 Jan 2016
National Institute of Standards and Technology. http://physics.nist.gov/PhysRefData/XrayMassCoef/ElemTab.html. Accessed 17 Jan 2016
Ahmadi Moghaddas T, Ghorbani M, Haghparast A, Flynn RT, Eivazi MT (2014) Monte Carlo study on dose enhancement effect of various paramagnetic nanoshells in Brachytherapy. J Med Biol Eng 34(6):559–567
Ghorbani M, Behmadi M (2016) Evaluation of hypothetical 153Gd source for use in brachytherapy. Rep Pract Oncol Radiother 21(1):17–24
Beaulieu L, Carlsson Tedqren A, Carrier JF, Davis SD, Mourtada F, Rivard MJ et al (2012) Report of the task group 186 on model-based dose calculation methods in brachytherapy beyond the TG-43 formalism: current status and recommendations for clinical implementation. Med Phys 39(10):6208–6236
White SA, Landry G, Fonseca GP, Holt R, Rusch T, Beaulieu L et al (2014) See comment in PubMed Commons below Comparison of TG-43 and TG-186 in breast irradiation using a low energy electronic brachytherapy source. Med Phys 41(6):6208–6236
ICRU report No. 24 (1976) Determination of absorbed dose in a patient irradiated by beams of X or gamma rays in radiotherapy procedures. International Commission on Radiation Units and Measurements (ICRU), Washington
Acknowledgments
The authors would like to thank Nucletron Company for providing the useful information on the geometry of the plastic applicator. We are also grateful for the financial support provided by Mashhad University of Medical Sciences.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ghorbani, M., Hashempour, M., Azizi, M. et al. Evaluating the effect of various intracavitary applicators on dosimetric parameters of 192Ir, 137Cs, and 60Co sources. Australas Phys Eng Sci Med 39, 477–491 (2016). https://doi.org/10.1007/s13246-016-0441-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-016-0441-2