Abstract
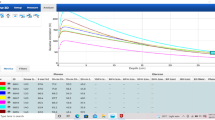
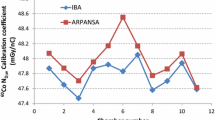
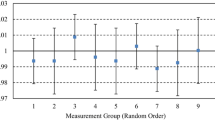
For safe and accurate dose delivery in brachytherapy, associated equipment is subject to commissioning and ongoing quality assurance (QA). Many centres depend on the use of a well-type chamber (‘well chamber’) for performing brachytherapy dosimetry. Documentation of well chamber commissioning is scarce despite the important role the chamber plays in the whole brachytherapy QA process. An extensive and structured commissioning of the HDR 1000 plus well chamber (Standard Imaging Inc, Middleton WI) for HDR and LDR dosimetry was undertaken at Sir Charles Gairdner Hospital. The methodology and outcomes of this commissioning is documented and presented as a guideline to others involved in brachytherapy. The commissioning tests described include mechanical integrity, leakage current, directional dependence, response, length of uniform response, the influence of insert holders, ion collection efficiency, polarity effect, accuracy of measured air kerma strength (S K ) or reference air kerma rate (K R ) and baseline setting (for ongoing constancy checks). For the HDR 1000 plus well chamber, some of the insert holders modify the response curve. The measured sweet length was 2.5 cm which is within 0.5 % of that specified by the manufacturer. Correction for polarity was negligible (0.9999) and ion recombination was small (0.9994). Directional dependence was small (less than 0.2 %) and leakage current was negligible. The measured K R for 192Ir agreed within 0.11 % compared with a second well chamber of similar model and was within 0.5 % of that determined via a free-in-air measurement method. Routine constancy checks over a year agreed with the baseline within 0.4 %.





Similar content being viewed by others
References
International Atomic Energy Agency (IAEA) (2002) IAEA TECDOC 1274; calibration of photon and beta ray sources used in brachytherapy. IAEA, Vienna, pp 1–58
Dempsey C, Smith R, Nyathi T et al (2013) ACPSEM brachytherapy working group recommendations for quality assurance in brachytherapy. Australas Phys Eng Sci Med 36(4):387–396
International Atomic Energy Agency (IAEA) (1999) IAEA TECDOC 1079; calibration of brachytherapy sources. IAEA, Vienna, pp 1–47
Swiss Society of radiobiology and Medical Physics (SSRMP) (2005) Dosimetry and quality assurance in high dose rate brachytherapy with iridium-192. SSRMP, Switerland, pp 1–18
DeWerd LA, Micka JA, Holmes SM et al (2006) Calibration of multiple LDR brachytherapy sources. Med Phys 33(10):3804–3813
Standard Imaging Inc (2011) HDR 1000 plus well chamber REF 90008. Standard Imaging Inc, Middleton, pp 1–20
Kutcher GJ, Coia L, Gillin M et al (1994) Comprehensive QA for radiation oncology: report of AAPM Radiation Therapy Committee Task Group 40. Med Phys 21(4):581–618
Mellenberg DE Jr, Kline RW (1995) Verification of manufacturer-supplied 125I and 103Pd air-kerma strengths. Med Phys 22(9):1495–1997
Suntharalingam N, Podgorsak EB, Tolli H (2005) Brachytherapy: physical and clinical aspects. In: Podgorsak EB (ed) Radiation oncology physics: a handbook for teachers and students. IAEA, Vienna
Vandana S, Sharma SD (2010) Long term response stability of a well-type ionization chamber used in calibration of high dose rate brachytherapy sources. J Med Phys 35(2):100–103
Mayles WPM, Lake R, Mckenzie A et al (1999) Physics aspects of quality control in radiotherapy: IPEM Report 81. England, pp 1–303
Van Dyk J (1999) The modern technology of radiation oncology: a compendium for medical physicists and radiation oncologists, vol 2. Medical Physics Publishing, Madison
Mayles WPM, Nahum AE, Rosenwald JC (2007) Handbook of radiotherapy physics: theory and practice. CRC Press, Boca Raton
Butler WM, Bice WS, DeWerd LA et al (2008) Third-party brachytherapy source calibrations and physicist responsibilities: report of the AAPM Low Energy Brachytherapy Source Calibration Working Group. Med Phys 35(9):3860–3865
Hayes E (2012) Introduction of IPEM code of practice for determination of reference air kerma rate for HDR 192Ir brachytherapy sources based on the NPL air kerma standard. Phys Med: Eur J Med Phys 28(4):336
Yu Y, Anderson LL, Zuofeng L et al (1999) Permanent prostate seed implant brachytherapy: report of the American Association of Physicists in Medicine Task Group No. 64. Med Phys 26(10):2054–2076
Kudo HD, Glasgow GP, Pethel PD et al (1998) High Dose Rate brachytherapy treatment delivery: report of the AAPM Radiation Therapy Committee Group No 59. Med Phys 25(4):375–404
Venselarr J, Perez-Calatayud J (2004) European guidelines for quality assurance in radiotherapy, ESTRO Booklet No 8, a practical guide to quality control of brachytherapy equipment. ESTRO, Belgium, pp 1–270
Nath R, Anderson LL, Meli JA et al (1997) Code of practice for brachytherapy physics: report of the AAPM Radiation Therapy Committee Task Group No. 56. American Association of Physicists in Medicine. Med Phys 24(10):1557–1598
Morgan AM, Arid EGA, Aukett AJ et al (2000) IPEM guidelines on dosimeter systems for use as transfer instruments between the UK primary dosimetry standards laboratory (NPL) and radiotherapy centres. Phys Med Biol 45(9):2445–2457
International Atomic Eneragy Agency (IAEA) (2007) Appendix to IAEA calibration certificate: well type chamber and electrometer calibration procedure at the IAEA dosimetry laboratory. IAEA, Vienna, pp 1–4
International Atomic Energy Agency (IAEA) (2006) IAEA TRS 398; absolute dose determination in external beam radiotheraphy: an international code of practice for dosimetry based on stanadrds of absorbed dose to water. IAEA, Vienna, pp 1–183
Standard Imaging Inc (2000) Technical note: calibration of the 125I rapid strand. Standard Imaging Inc, Middleton, pp 1–2
Canadian Association of Provincial Cancer Agencies (CAPCA) (2007) Quality control standards: major dosimetry equipment. CAPCA, Canada, pp 1–28
Standard Imaging Inc (2007) Specifications of HDR 1000 plus well type chamber. Standard Imaging Inc, Middleton, pp 1–2
Acknowledgments
The authors would like to acknowledge assistance from fellow Medical Physicists at Sir Charles Gairdner Hospital. We would like to thank the hospital for the facility and environment that is conducive for such endeavours.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mukwada, G., Neveri, G., Alkhatib, Z. et al. Commissioning of a well type chamber for HDR and LDR brachytherapy applications: a review of methodology and outcomes. Australas Phys Eng Sci Med 39, 167–175 (2016). https://doi.org/10.1007/s13246-015-0415-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-015-0415-9