Abstract
The nucleocapsid (N) protein of SARS-CoV-2 has been reported to have a high ability of liquid-liquid phase separation, which enables its incorporation into stress granules (SGs) of host cells. However, whether SG invasion by N protein occurs in the scenario of SARS-CoV-2 infection is unknow, neither do we know its consequence. Here, we used SARS-CoV-2 to infect mammalian cells and observed the incorporation of N protein into SGs, which resulted in markedly impaired self-disassembly but stimulated cell cellular clearance of SGs. NMR experiments further showed that N protein binds to the SG-related amyloid proteins via non-specific transient interactions, which not only expedites the phase transition of these proteins to aberrant amyloid aggregation in vitro, but also promotes the aggregation of FUS with ALS-associated P525L mutation in cells. In addition, we found that ACE2 is not necessary for the infection of SARS-CoV-2 to mammalian cells. Our work indicates that SARS-CoV-2 infection can impair the disassembly of host SGs and promote the aggregation of SG-related amyloid proteins, which may lead to an increased risk of neurodegeneration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ongoing pandemic of coronavirus disease 2019 (COVID-19) caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an international public health emergency. SARS-CoV-2 infection typically causes a contagious respiratory tract illness and occasionally gastrointestinal symptoms (Lee et al., 2020; Mao et al., 2020; Zhou et al., 2020; Zhu et al., 2020). These immediate symptoms would disappear in several weeks as the patients recover from the infection (Soresina et al., 2020; Thevarajan et al., 2020). In the meantime, many evidence have shown that SARS-CoV-2 can also infect human central nervous system (Mao et al., 2020; Zhou et al., 2020; Song et al., 2021) and cause neuroinflammation (Bostanciklioglu, 2020; Gatto and Fernandez Boccazzi, 2020; Hascup and Hascup, 2020; Heneka et al., 2020; Singal et al., 2020), which raise worries about potential long-term effects of COVID-19 especially on the development of neurodegenerative diseases (Gatto and Fernandez Boccazzi, 2020; Heneka et al., 2020; Li et al., 2020; Paniz-Mondolfi et al., 2020; Serrano-Castro et al., 2020). Indeed, virus invasion in neurological system has been linked to the pathogenesis of several neurodegenerative disorders such as Parkinson’s disease (PD), Alzheimer’s disease (AD), and amyotrophic lateral sclerosis (ALS) (Jang et al., 2009; Eimer et al., 2018; Readhead et al., 2018; Bellmann et al., 2019; Marreiros et al., 2020). PD diagnosed after SARS-CoV-2 infection has been also reported (Cohen et al., 2020). However, the relationship between SARS-CoV-2 infection and neurodegeneration requires a lot more evidence to reveal.
SARS-CoV-2 belonging to SARS-related coronaviruses, is an enveloped, positive-sense single-stranded RNA virus with a 30-kb genome (Wu et al., 2020; Zhou et al., 2020; Zhu et al., 2020). Its genomic RNA packages with the nucleocapsid (N) protein to form the so-called nucleocapsid (Lai and Cavanagh, 1997; Saikatendu et al., 2007), which is important for the viral replication and transcription (McBride et al., 2014). The genome of SARS-CoV-2 consists of 14 open reading frames (Orfs) encoding 16 non-structural proteins (Nsp1–16), four structural proteins (spike (S), envelope (E), membrane (M) and nucleocapsid (N)) and nine putative accessory factors (Chan et al., 2020; Wu et al., 2020). A recent mass spectrometry study expressed 26 out of the 29 SARS-CoV-2 proteins in human cells and identified broad interactions between the viral and human proteins involved in biological processes including protein trafficking, translation, transcription and ubiquitination regulation (Gordon et al., 2020). Bioinformatics analysis predicted that the disordered domains of SARS-CoV-2 N protein can engage in π-π intermolecular interactions with host stress granule (SG) proteins, which is crucial for the viral hijacking of host machineries (Moosa and Banerjee, 2020). Recombinant N protein of SARS-CoV-2 exhibits a high ability of liquid-liquid phase separation in vitro (Carlson et al., 2020; Chen et al., 2020; Iserman et al., 2020; Savastano et al., 2020; Luo et al., 2021b; Zhao et al., 2021), overexpression of which in human cell lines showed its incorporation into SGs (Savastano et al., 2020; Luo et al., 2021a). These studies indicate the association of N protein with host SGs, while a real scenario of virus infection is lacking. Neither do we know the consequence of the potential invasion of host SGs by SARS-CoV-2.
In this work, we infected mammalian cells with SARS-CoV-2, and observed that N protein but not the other monitored viral proteins incorporated into host SGs. Consequently, the invaded SGs are less dynamic and resistant to disassemble after the removal of stress, but are promoted for clearance upon continuous stress. In vitro observations showed cooperative liquid-liquid phase separation (LLPS) of N protein with SG-related amyloid proteins and stimulation of their amyloid aggregation. NMR experiments further characterized the non-specific transient interactions between N protein and SG-related amyloid proteins. The enhancement of amyloid aggregation by SARS-CoV-2 infection was further shown by the exacerbated aggregation of an ALS-associated FUS mutant in cells. In addition, we found that cells without the ACE2 receptor can still be infected by SARS-CoV-2, with a decreased efficiency though. These molecular evidences support that SARS-CoV-2 infection might increase the risk of neurodegenerative diseases.
Results
ACE2 is not necessary for SARS-CoV-2 to infect mammalian cells
To investigate the impact of SARS-CoV-2 infection on host SGs, we first treated mammalian cells including monkey Vero cells and human HeLa cells with SARS-CoV-2 for 30 min (Fig. 1A). Vero cells have the ACE2 receptor (Fig. S1A), which can help the entry of SARS-CoV-2 (Li et al., 2003). After two days for virus replication, expression of viral proteins in Vero cells was detected (Fig. S1A). Although HeLa cells lack ACE2 (Zhou et al., 2020), at a high multiplicity of infection (MOI) of 0.75, SARS-CoV-2 can still infect HeLa cells and the expression of the viral N protein was detected by Western blot (Fig. S1B). However, the expression of Spike was not observed (Fig. S1B), which may reflect poor replication of the virus in HeLa cells. To increase the virus entry efficiency, we also treated HeLa cells overexpressing human ACE2 (ACE2-HeLa cells) with the virus. After 2 days for viral replication, expression of the viral proteins was detected (Fig. S1B). These results indicate that ACE2 is not necessary for SARS-CoV-2 to infect mammalian cells, although it can increase the efficiency.
SARS-CoV-2 infection results in the incorporation of N protein with SGs in mammalian cells. (A) Schematic workflow of the virus infection and SG induction. (B) Confocal images of mammalian cells infected by SARS-CoV-2. Infected cells were stressed with 100 μmol/L sodium arsenite for 1 h, and stained with DAPI, antibodies for N protein and SG marker proteins G3BP1. Arrows indicate SGs. Scale bar, 5 µm. (C) Confocal images of HeLa cells transfected with Flag-tagged N protein (Flag-N). Cells were stressed with 100 μmol/L sodium arsenite for 1 h, and stained with DAPI, anti-flag, and anti-G3BP1. Arrows indicate SGs. Scale bar, 5 µm
N protein enters the host SGs upon SARS-CoV-2 infection
Next, we stressed the infected cells with 100 μmol/L sodium arsenite to induce SGs, and then used immunofluorescence microscopy to monitor the cellular localization of different viral proteins including N protein, S protein, Nsp1, Nsp8 and ORF7α (Fig. 1A). The result showed that N protein but not the others is recruited into the SGs of the mammalian cells (Figs. 1B and S2).
It has been reported that overexpressed N protein of either SARS-CoV-2 or SARS-CoV can invade cellular SGs (Peng et al., 2008; Savastano et al., 2020; Luo et al., 2021a). We confirmed this result by overexpressing recombinant Flag-tagged N protein in HeLa cells, and consistently observed the overexpressed N protein co-localizing with SGs (Fig. 1C). The overexpression results indicate that N protein can incorporate into SGs independent of viral components.
SARS-CoV-2 infection impairs the self-disassembly of SGs
To investigate the influence of SARS-CoV-2 invasion on SG dynamics, we relieved the cellular stress by washing out sodium arsenite in the culture medium (Fig. 2A). Before washout, similar amounts of SGs formed in SARS-CoV-2 infected cells and control cells (not treated with virus) (Fig. 2B), indicating no significant influence of SARS-CoV-2 infection on the assembly of SGs. However, the self-disassembly of SGs was significantly slowed down in the infected cells monitored 60 min post washout (Fig. 2B). Similar phenomena were observed in both HeLa cells and ACE2-overexpressed HeLa cells (Figs. 2B and S3A). We also performed the washout experiment by directly overexpressing N protein in HeLa cells and obtained consistent results with that infected by the virus (Fig. S3B). These results indicate that upon SARS-CoV-2 infection, the invasion of N protein can impair the dynamics, specifically the self-disassembly of SGs.
SARS-CoV-2 infection impairs the disassembly but enhances the cellular clearance of host SGs. (A) Schematic workflow of the experiment of SG self-disassembly. (B) Confocal images of ACE2-HeLa cells with or without (control) infection of SARS-CoV-2. Cells were stressed with 100 μmol/L sodium arsenite for 1 h, followed by washing out sodium arsenite. Cells were stained with antibodies for viral N protein and SG marker protein G3BP1. Arrows indicate SGs. Scale bar, 5 µm. Quantitative analysis of the images is shown on the right as the area of SGs per cell. Values are means ± SD, n > 150 cells from 3 replicates. Student’s t-test, *P < 0.05, **P < 0.01; ns, not significant. (C) Schematic workflow of the experiment of cellular SG clearance. (D) Confocal images of ACE2-HeLa cells with or without (control) SARS-CoV-2 infection. Cells were stressed with 100 μmol/L sodium arsenite for 1 h or 5 h. Cells were stained with antibodies for N and G3BP1 proteins. Arrows indicate SGs. Scale bar, 5 µm. Quantitative analysis of the images is shown on the right as the area of SGs per infected cell. Values are means ± SD, n > 150 cells from 3 replicates. Student’s t-test, *P < 0.05, **P < 0.01; ns, not significant. (E) In situ FRAP for SGs in HeLa cells overexpressing RFP-tagged N protein. Cells overexpressing RFP-tag were performed as a control. mEGFP-tagged G3BP1 was co-overexpressed with RFP or RFP-N to fluorescently label SGs. Scale bar, 5 µm. FRAP montages of an SG for each sample are shown. The arrows indicate the action of bleaching. (F) Fluorescent recovery curves of the SGs. Data shown are means ± S.D., n = 3 individual SGs. Student’s t-test
SARS-CoV-2 infection promotes cellular clearance of SGs
Previous studies suggest autophagy as a second SG clearance system in addition to self-disassembly (Buchan et al., 2013; Protter and Parker, 2016), and persistent SGs induced by chronic stress are eliminated by autophagy-dependent degradation (Gwon et al., 2021). Indeed, as we stressed the cells for extra h (5 h), we also observed disappearance of SGs (Fig. 2C and 2D), although the involvement of autophagy is not confirmed here. Notably, SARS-CoV-2 infected cells exhibited more severe SG disappearance than the control cells (Fig. 2D). Similar phenomena were observed when overexpressing N protein in HeLa cells (Fig. S4). These results indicate that abnormal SGs due to the incorporation of the viral N protein may be more potent to trigger cellular degradation systems.
N protein incorporation impairs the liquid-like state of host SGs
To further investigate the influence of N protein incorporation on the liquid-like state of SGs, we performed in situ fluorescence recovery after photobleaching (FRAP). We overexpressed G3BP1 with an mEGFP tag as a fluorescent marker of SGs in HeLa cells. FRAP experiment showed that the fluorescent intensity of SGs rapidly recovered about 80% within 2 min after photobleaching reflecting high mobility and liquid-like property of SGs (Fig. 2E). In contrast, as N protein co-overexpressed in the cells, the recovery of fluorescent intensity significantly slowed down to ~50% recovery within 2 min (Fig. 2F). This result indicates that N protein incorporation disrupts the liquid-like state of SGs.
N protein expedites the maturation of the LLPS of SG-related amyloid proteins
It has been reported that N protein of SARS-CoV-2 has a high ability of LLPS under various conditions (Carlson et al., 2020; Cubuk et al., 2020; Iserman et al., 2020; Luo et al., 2020; Perdikari et al., 2020; Savastano et al., 2020). The LLPS property of N protein has been suggested to play an important role in the viral genome packing in other viruses (Guseva et al., 2020; Monette et al., 2020). We also observed that N protein readily underwent LLPS in the presence of synthetic single-stranded RNA (polyU) (Fig. S5).
Several RNA-binding proteins of SGs including FUS, hnRNPA1, and TDP43 are meanwhile prone to undergo amyloid aggregation, which is closely associated with neurodegenerative diseases such as ALS and frontotemporal dementia (FTD). These proteins also have a high ability of LLPS (Molliex et al., 2015; Patel et al., 2015). To investigate the influence of SARS-CoV-2 N protein on the phase transition of these SG-related amyloid proteins, we added the viral N protein to the LLPS solution of human FUS, hnRNPA1, and TDP43, respectively. Fluorescent microscopic imaging showed that N protein spontaneously condenses in the droplets formed by the SG proteins (Fig. 3A), which is consistent with a previous report showing that N protein can co-phase separate with FUS, TDP43, and hnRNPA2 (Perdikari et al., 2020).
SARS-CoV-2 N protein co-phase separates with SG proteins and solidifies their liquid-like droplets. (A) Fluorescence images of co-phase separation of N protein with SG proteins hnRNPA1, FUS, and TDP43, respectively. SG protein concentrations and the molar ratio of SG proteins to N protein are indicated. LLPS buffer: 50 mmol/L Tris-HCl, pH 7.5, 100 mmol/L NaCl, 10% PEG 3,350 (no PEG for FUS). EGFP is a fluorescence tag. Alexa-488 and QSY7 are fluorescence dyes. Scale bar, 5 µm. (B) FRAP montages of FUS-EGFP droplets (left). The arrows indicate the action of bleaching. Protein concentrations are indicated. Buffer: 50 mmol/L Tris-HCl, pH 7.5, 100 mmol/L NaCl. The droplets are incubated for 0 h and 12 h, respectively. Scale bar, 2 µm. The graphs (right) show the recovery fraction as the function of time. Data shown are means ± SD, n = 3. (C) Representative images of the morphological changes of FUS-EGFP droplets in the absence or presence of N protein over time. The phase separation condition is the same as (B). A FUS droplet with fibrils growing out is enlarged in the inset. Scale bar, 10 µm
Moreover, we observed that in the presence of N protein, the fluorescent intensity of EGFP-tagged FUS (FUS-EGFP) recovered markedly slower than that in the absence of N protein (Fig. 3B). After incubation for 12 h, the shape of the droplets was apparently less round than that at 0 h (Fig. 3B). FRAP showed that these droplets nearly lost the mobility and were hardly recovered after bleaching (Fig. 3B). Similarly, N protein also impairs the liquid-like nature of the hnRNPA1 and TDP43 droplets by FRAP experiments (Fig. S6). These data indicate that the involvement of N protein accelerates the liquid-to-solid maturation process of these SG proteins, which is in line with the impaired dynamics of SGs in cells stated above.
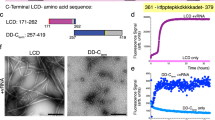
Non-specific transient interactions between N protein and the LC domains of SG-related proteins
We next used NMR spectroscopy to study the molecular mechanism underlying the interaction between N protein and the SG proteins. The 2D 1H-15N HSQC spectra of 15N-labeled FUS low complex domain (FUS-LC) and 15N-labeled TDP43-LC showed that both proteins adopted an intrinsically disordered conformation with a narrow chemical shift dispersion in the 1H dimension (backbone amide resonances within 7.8–8.8 ppm) (Fig. S7), which is consistent with the previous reports (Burke et al., 2015; Conicella et al., 2016; Liu et al., 2020; Gu et al., 2021a). We then used unlabeled N protein to titrate 15N-labeled FUS-LC. The HSQC spectra of FUS-LC showed a global decrease of signal intensities in a concentration-dependent manner (Figs. 4A, 4B and S7B), indicating direct interaction between N protein and FUS-LC. However, no specific region or residue type showed significant intensity decrease compared to others, and residues of FUS-LC suffered an overall ~40% intensity decrease at the substoichiometric molar ration of 1:0.5 (FUS-LC:N) (Fig. 4A), implying that the interaction between N protein and FUS-LC is non-specific. Similarly, titration of N protein to TDP43-LC resulted in concentration-dependent attenuations of the signal intensities in the HSQC spectra of TDP43-LC (Figs. 4C, 4D and S7D). The interaction between N protein and TDP43-LC also appears non-specific, since the residues of TDP43-LC generally showed a ~20% intensity decrease at the molar ratio of 1:5 (TDP43-LC:N) (Figs. 4C, 4D and S7D). Unfortunately, we did not get a good NMR spectrum of hnRNPA1-LC, in which only a few broadening crosspeaks could be detected at our conditions. Taken together, these results indicate that N protein may commonly bind the SG proteins via nonspecific weak interactions to the LC domains of the SG proteins.
SARS-CoV-2 N protein non-specifically interacts with LC domains of FUS and TDP-43. (A) Residue-specific intensity changes of signals in the 2D 1H-15N HSQC spectra of 25 μmol/L 15N-labeled FUS-LC in the presence of N protein at molar ratios (FUS-LC : N) of 1:0.5 (green) and 1:2 (orange). The x axis for the spectra on the top is shown according to the residue numbers; that at the bottom is according to the amino acid composition. Residue signals that dropped over 70% are shown in (B). (C) Residue-specific intensity changes of signals in the 2D 1H-15N HSQC spectra of 20 μmol/L 15N-labeled TDP43-LC in the presence of N protein at molar ratios (TDP43-LC : N) of 1:2.5 (pink) and 1:5 (grey). Residue signals that dropped over 30% are shown in (B)
N protein stimulates the aggregation of SG-related amyloid proteins
As we incubated N protein with FUS for 12 h, we observed that some LLPS droplets became spiky with fibrils growing out of the droplets (Fig. 3B and 3C). FRAP experiment showed that the fluorescence of these spiky droplets can hardly recover after bleaching, which confirms the solid nature of these droplets (Fig. 3B).
To further examine the influence of N protein on the amyloid fibril formation of FUS, hnRNPA1, and TDP43, we performed the ThT fluorescence assay and negative-staining transmission electron microscopy (TEM). Since the LC domains of FUS, hnRNPA1, and TDP43 are the amyloid-forming core sequences of these proteins (Johnson et al., 2009; Kato et al., 2012; Kim et al., 2013), we incubated N protein with the LC domains of these three SG proteins, respectively. The result showed that the presence of N protein markedly enhanced the ThT intensities of the fibril-forming samples, and shortened the lag time of the ThT kinetic curves in a dose-dependent manner (Fig. 5A). TEM imaging confirmed amyloid fibril formation in these samples (Fig. 5B). In addition, we confirmed that N protein under the examined conditions does not form amyloid fibrils (Fig. S8). These results indicate that N protein can generally stimulate the phase transition of the SG-related amyloid proteins into amyloid aggregation.
SARS-CoV-2 N protein promotes the amyloid aggregation of SG proteins. (A) ThT kinetic assays for amyloid fibril formation of the LC domains of FUS, TDP43, and hnRNPA1. Protein concentrations and molar ratios are indicated. Buffer for FUS-LC and hnRNPA1-LC amyloid formation: 50 mmol/L Tris-HCl, pH 7.5 and 100 mmol/L NaCl. Buffer for TDP43-LC amyloid formation: 50 mmol/L Bis-Tris, pH 6.5 and 100 mmol/L NaCl. Data correspond to mean ± SD, n = 3 independent replicates. (B) TEM images of samples in (A) at the end time point. Scale bar, 500 nm. (C) Confocal images of CFP-FUS P525L aggregation puncta in ACE2-HeLa cells infected by SARS-CoV-2. Cells without treatment of the virus are used as a control. FUS P525L is visualized by CFP fluorescence. N protein is immunostained with anti-N. The arrows indicate FUS P525L aggregates. Scale bar, 5 μm. Quantitative analysis of the aggregation area per cell in the imaging data is shown on the right. Values are means ± SD, n > 150 cells from 3 replicates. Student’s t-test
SARS-CoV-2 infection promotes amyloid aggregation of ALS-related FUS mutant in cells
We next sought to investigate SARS-CoV-2 infection on protein amyloid aggregation in cells. We used a cell model that overexpresses FUS with P525L mutation, a mutation found in ALS that disrupts the nuclear localization of FUS and results in FUS accumulation in the cytoplasm (Kwiatkowski et al., 2009; Dormann et al., 2010; De Santis et al., 2019). We first transfected ACE2-overexpressed HeLa cells with CFP-fused FUS P525L. Aggregation of FUS P525L in cells can be probed CFP fluorescence and an amyloid dye—pFTAA (Klingstedt et al., 2013; Qamar et al., 2018). Next, we treated the cells with SARS-CoV-2 and observed that the viral N protein colocalizes with FUS P525L aggregates (Fig. 5C). Notably, comparing with the control cells (no virus infection), the aggregation of FUS P525L significantly increased upon virus infection (Fig. 5C). We also observed the same enhancement of FUS P525L aggregation by using SARS-CoV-2 infected HeLa cells (Fig. S9A) and HeLa cells with overexpressed N protein (Fig. S9B). These data strengthen the potential consequence of SARS-CoV-2 infection in stimulating protein amyloid aggregation in the host cells.
Discussion
Virus infection has been found to play an important role in the pathogenesis and clinical onset of human neurodegenerative diseases (Jang et al., 2009; Eimer et al., 2018; Readhead et al., 2018; Bellmann et al., 2019; Marreiros et al., 2020). Recent studies have shown that proteins of SARS-CoV-2 accumulate in the brain tissues of both transgenic mice and patients who died from COVID-19 (Matschke et al., 2020; Song et al., 2021). It has also been reported that SARS-CoV-2 can infect and replicate in astrocytes (Crunfli et al., 2021). Clinical correlation of SARS-CoV-2 infection and PD onset has also been reported. These observations raise the concern of neurodegeneration as a long-term consequence of COVID-19 (Bostanciklioglu, 2020; Gatto and Fernandez Boccazzi, 2020; Hascup and Hascup, 2020; Heneka et al., 2020; Singal et al., 2020). The answer for this concern is important for our treatment and policy to COVID-19. Our work demonstrates that as SARS-CoV-2 infects the host cells, it has a strong potential to stimulate the amyloid aggregation of host proteins, which provides molecular evidence for the role of SARS-CoV-2 in triggering neurodegeneration (Fig. 6). During this process, the viral N protein is a major player. N protein can interact with a wide spectrum of SG proteins including FUS, TDP43, hnRNPA1, hnRNPA2, G3BP1, and G3BP2 as reported previously and in this work (Kaur and Lal, 2020; Luo et al., 2020; Moosa and Banerjee, 2020; Perdikari et al., 2020). Our NMR data showed that N protein non-specifically interacts with the LC domains of FUS and TDP43. Given that the SG-related RNA-binding proteins generally contain intrinsically disordered sequences, N protein may interact with other SG proteins via a similar mechanism. Direct interactions with various SG proteins underlie the partition of N protein into SGs; however, whether this process is active or passive is obscure. SG formation is part of the antiviral responses of cells, which can assemble in response to viral infection and function to sequester host and viral mRNAs and proteins (Onomoto et al., 2012; Jain et al., 2016). On the other hand, N protein incorporation may hijack host SGs and alter their attributes. In addition, the viral genomic RNA, that assembles with N protein to form nucleocapsid, may facilitate the SG incorporation of N protein. Indeed, we observed that single-stranded RNA lowered the critical concentration of N protein for LLPS (Fig. S5). Note that in our experiments, we did not observe viral infection-triggered SG formation in either human HeLa cells or monkey Vero cells, which may be caused by reasons such as cell sensitivity, virus infection titer and time.
Schematic diagram for the interplay between SARS-CoV-2 and host SGs. During SARS-CoV-2 replication in host cells, the viral N protein enters the host SGs and directly interacts with SG-related amyloid-forming proteins (e.g., FUS, hnRNPA1 and TDP43), which stimulates the liquid to solid phase transition (amyloid formation) of these host proteins. Inefficient maintenance of proteostasis may result in accumulation of the pathological amyloid fibrils and development of neurodegeneration
Many evidences have indicated that disruption of SG dynamics is closely associated with neurodegenerative diseases such as ALS and FTD (Molliex et al., 2015; Duan et al., 2019; Wolozin and Ivanov, 2019; Zhang et al., 2020). Our work demonstrates that SARS-CoV-2 infection can impair the dynamics of SGs and promote amyloid aggregation of SG-related proteins. In addition, our data show that HeLa cells, that same as neurons, lack the ACE2 receptor, can be infected by SARS-CoV-2 (Fig. S1B). Consistently, recent studies have identified several other receptors that may contribute to ACE2-independent cell entry of SARS-CoV-2 (Gao et al., 2020; Amraei et al., 2021; Chen et al., 2021; Gu et al., 2021b). These indicate that neurons are likely to be infected by SARS-CoV-2 as the virus invades the human brain. Our work provides molecular evidence for the increased risk of neurodegeneration after SARS-CoV-2 infection, and suggests paying a special attention to the incidence of neurodegenerative diseases in aged people under the current circumstances of ongoing widespread of SARS-CoV-2.
References
Amraei R, Yin W, Napoleon MA, Suder EL, Berrigan J, Zhao Q, Olejnik J, Chandler K, Xia C, Feldman J, et al (2021) CD209L/L-SIGN and CD209/DC-SIGN act as receptors for SARS-CoV-2. bioRxiv
Bellmann J, Monette A, Tripathy V, Sojka A, Abo-Rady M, Janosh A, Bhatnagar R, Bickle M, Mouland AJ, Sterneckert J (2019) Viral infections exacerbate FUS-ALS phenotypes in iPSC-derived spinal neurons in a virus species-specific manner. Front Cell Neurosci 13:480
Bostanciklioglu M (2020) Severe acute respiratory syndrome coronavirus 2 is penetrating to dementia research. Curr Neurovasc Res.
Buchan JR, Kolaitis RM, Taylor JP, Parker R (2013) Eukaryotic stress granules are cleared by autophagy and Cdc48/VCP function. Cell 153:1461–1474
Burke KA, Janke AM, Rhine CL, Fawzi NL (2015) Residue-by-residue view of in vitro FUS granules that bind the C-terminal domain of RNA polymerase II. Mol Cell 60:231–241
Carlson CR, Asfaha JB, Ghent CM, Howard CJ, Hartooni N, Safari M, Frankel AD, Morgan DO (2020) Phosphoregulation of phase separation by the SARS-CoV-2 N protein suggests a biophysical basis for its dual functions. Mol Cell 80:1092–1103
Chan JF, Kok KH, Zhu Z, Chu H, To KK, Yuan S, Yuen KY (2020) Genomic characterization of the 2019 novel human-pathogenic coronavirus isolated from a patient with atypical pneumonia after visiting Wuhan. Emerg Microbes Infect 9:221–236
Chen H, Cui Y, Han X, Hu W, Sun M, Zhang Y, Wang PH, Song G, Chen W, Lou J (2020) Liquid-liquid phase separation by SARS-CoV-2 nucleocapsid protein and RNA. Cell Res 30:1143–1145
Chen J, Fan J, Chen Z, Zhang M, Peng H, Liu J, Ding L, Liu M, Zhao C, Zhao P et al (2021) Nonmuscle myosin heavy chain IIA facilitates SARS-CoV-2 infection in human pulmonary cells. Proc Natl Acad Sci USA 118:e2111011118
Cohen ME, Eichel R, Steiner-Birmanns B, Janah A, Ioshpa M, Bar-Shalom R, Paul JJ, Gaber H, Skrahina V, Bornstein NM et al (2020) A case of probable Parkinson’s disease after SARS-CoV-2 infection. Lancet Neurol 19:804–805
Conicella AE, Zerze GH, Mittal J, Fawzi NL (2016) ALS mutations disrupt phase separation mediated by alpha-helical structure in the TDP-43 low-complexity C-terminal domain. Structure 24:1537–1549
Crunfli F, Carregari VC, Veras FP, Vendramini PH, Fragnani Valença AG, Marcelo Antunes ASL, Brandão-Teles C, da Silva Zuccoli G, Reis-de-Oliveira G, Silva-Costa LC, et al (2021) SARS-CoV-2 infects brain astrocytes of COVID-19 patients and impairs neuronal viability. medRxiv
Cubuk J, Alston JJ, Incicco JJ, Singh S, Stuchell-Brereton MD, Ward MD, Zimmerman MI, Vithani N, Griffith D, Wagoner JA, et al (2020) The SARS-CoV-2 nucleocapsid protein is dynamic, disordered, and phase separates with RNA. bioRxiv
De Santis R, Alfano V, de Turris V, Colantoni A, Santini L, Garone MG, Antonacci G, Peruzzi G, Sudria-Lopez E, Wyler E et al (2019) Mutant FUS and ELAVL4 (HuD) aberrant crosstalk in amyotrophic lateral sclerosis. Cell Rep 27:3818–3831
Dormann D, Rodde R, Edbauer D, Bentmann E, Fischer I, Hruscha A, Than ME, Mackenzie IR, Capell A, Schmid B et al (2010) ALS-associated fused in sarcoma (FUS) mutations disrupt transportin-mediated nuclear import. EMBO J 29:2841–2857
Duan Y, Du A, Gu J, Duan G, Wang C, Gui X, Ma Z, Qian B, Deng X, Zhang K et al (2019) PARylation regulates stress granule dynamics, phase separation, and neurotoxicity of disease-related RNA-binding proteins. Cell Res 29:233–247
Eimer WA, Vijaya Kumar DK, Navalpur Shanmugam NK, Rodriguez AS, Mitchell T, Washicosky KJ, Gyorgy B, Breakefield XO, Tanzi RE, Moir RD (2018) Alzheimer’s disease-associated beta-amyloid is rapidly seeded by herpesviridae to protect against brain infection. Neuron 99:56–63
Gao C, Zeng J, Jia N, Stavenhagen K, Matsumoto Y, Zhang H, Li J, Hume AJ, Muhlberger E, van Die I, et al (2020) SARS-CoV-2 spike protein interacts with multiple innate immune receptors. bioRxiv
Gatto EM, Fernandez Boccazzi J (2020) COVID-19 and neurodegeneration: what can we learn from the past? Eur J Neurol. https://doi.org/10.1111/ene.14311
Gordon DE, Jang GM, Bouhaddou M, Xu J, Obernier K, White KM, O’Meara MJ, Rezelj VV, Guo JZ, Swaney DL et al (2020) A SARS-CoV-2 protein interaction map reveals targets for drug repurposing. Nature 583:459–468
Gu J, Wang C, Hu R, Li Y, Zhang S, Sun Y, Wang Q, Li D, Fang Y, Liu C (2021a) Hsp70 chaperones TDP-43 in dynamic, liquid-like phase and prevents it from amyloid aggregation. Cell Res 31:1024–1027
Gu Y, Cao J, Zhang X, Gao H, Wang Y, Wang J, He J, Jiang X, Zhang J, Shen G, et al (2021b) Receptome profiling identifies KREMEN1 and ASGR1 as alternative functional receptors of SARS-CoV-2. Cell Res
Guseva S, Milles S, Jensen MR, Salvi N, Kleman JP, Maurin D, Ruigrok RWH, Blackledge M (2020) Measles virus nucleo- and phosphoproteins form liquid-like phase-separated compartments that promote nucleocapsid assembly. Sci Adv 6:eaaz7095
Gwon Y, Maxwell BA, Kolaitis RM, Zhang P, Kim HJ, Taylor JP (2021) Ubiquitination of G3BP1 mediates stress granule disassembly in a context-specific manner. Science 372:eabf6548
Hascup ER, Hascup KN (2020) Does SARS-CoV-2 infection cause chronic neurological complications? Geroscience 42:1083–1087
Heneka MT, Golenbock D, Latz E, Morgan D, Brown R (2020) Immediate and long-term consequences of COVID-19 infections for the development of neurological disease. Alzheimers Res Ther 12:69
Iserman C, Roden CA, Boerneke MA, Sealfon RSG, McLaughlin GA, Jungreis I, Fritch EJ, Hou YJ, Ekena J, Weidmann CA et al (2020) Genomic RNA elements drive phase separation of the SARS-CoV-2 nucleocapsid. Mol Cell 80:1078–1091
Jain S, Wheeler JR, Walters RW, Agrawal A, Barsic A, Parker R (2016) ATPase-modulated stress granules contain a diverse proteome and substructure. Cell 164:487–498
Jang H, Boltz D, Sturm-Ramirez K, Shepherd KR, Jiao Y, Webster R, Smeyne RJ (2009) Highly pathogenic H5N1 influenza virus can enter the central nervous system and induce neuroinflammation and neurodegeneration. Proc Natl Acad Sci USA 106:14063–14068
Johnson BS, Snead D, Lee JJ, McCaffery JM, Shorter J, Gitler AD (2009) TDP-43 is intrinsically aggregation-prone, and amyotrophic lateral sclerosis-linked mutations accelerate aggregation and increase toxicity. J Biol Chem 284:20329–20339
Kato M, Han TW, Xie S, Shi K, Du X, Wu LC, Mirzaei H, Goldsmith EJ, Longgood J, Pei J et al (2012) Cell-free formation of RNA granules: low complexity sequence domains form dynamic fibers within hydrogels. Cell 149:753–767
Kaur R, Lal SK (2020) The multifarious roles of heterogeneous ribonucleoprotein A1 in viral infections. Rev Med Virol 30:e2097
Kim HJ, Kim NC, Wang YD, Scarborough EA, Moore J, Diaz Z, MacLea KS, Freibaum B, Li S, Molliex A et al (2013) Mutations in prion-like domains in hnRNPA2B1 and hnRNPA1 cause multisystem proteinopathy and ALS. Nature 495:467–473
Klingstedt T, Shirani H, Aslund KO, Cairns NJ, Sigurdson CJ, Goedert M, Nilsson KP (2013) The structural basis for optimal performance of oligothiophene-based fluorescent amyloid ligands: conformational flexibility is essential for spectral assignment of a diversity of protein aggregates. Chemistry 19:10179–10192
Kwiatkowski TJ Jr, Bosco DA, Leclerc AL, Tamrazian E, Vanderburg CR, Russ C, Davis A, Gilchrist J, Kasarskis EJ, Munsat T et al (2009) Mutations in the FUS/TLS gene on chromosome 16 cause familial amyotrophic lateral sclerosis. Science 323:1205–1208
Lai MM, Cavanagh D (1997) The molecular biology of coronaviruses. Adv Virus Res 48:1–100
Lee IC, Huo TI, Huang YH (2020) Gastrointestinal and liver manifestations in patients with COVID-19. J Chin Med Assoc 83:521–523
Li W, Moore MJ, Vasilieva N, Sui J, Wong SK, Berne MA, Somasundaran M, Sullivan JL, Luzuriaga K, Greenough TC et al (2003) Angiotensin-converting enzyme 2 is a functional receptor for the SARS coronavirus. Nature 426:450–454
Li H, Xue Q, Xu X (2020) Involvement of the nervous system in SARS-CoV-2 infection. Neurotox Res 38:1–7
Liu Z, Zhang S, Gu J, Tong Y, Li Y, Gui X, Long H, Wang C, Zhao C, Lu J et al (2020) Hsp27 chaperones FUS phase separation under the modulation of stress-induced phosphorylation. Nat Struct Mol Biol 27:363–372
Luo L, Li Z, Ma P, Zou Y, Li P, Liang A, Jin Z, Chi T, Huang C, Zhang Y, et al (2020). SARS-CoV-2 Nucleocapsid protein impairs SG assembly by partitioning into G3BP condensate. SSRN Electron J
Luo L, Li Z, Zhao T, Ju X, Ma P, Jin B, Zhou Y, He S, Huang J, Xu X et al (2021a) SARS-CoV-2 nucleocapsid protein phase separates with G3BPs to disassemble stress granules and facilitate viral production. Sci Bull 66:1194–1204
Luo L, Li Z, Zhao T, Ju X, Ma P, Jin B, Zhou Y, He S, Huang J, Xu X et al (2021b) SARS-CoV-2 nucleocapsid protein phase separates with G3BPs to disassemble stress granules and facilitate viral production. Sci Bull 66(12):1194–1204
Mao L, Jin H, Wang M, Hu Y, Chen S, He Q, Chang J, Hong C, Zhou Y, Wang D et al (2020) Neurologic manifestations of hospitalized patients with coronavirus disease 2019 in Wuhan. China. JAMA Neurol 77(6):683–690
Marreiros R, Muller-Schiffmann A, Trossbach SV, Prikulis I, Hansch S, Weidtkamp-Peters S, Moreira AR, Sahu S, Soloviev I, Selvarajah S et al (2020) Disruption of cellular proteostasis by H1N1 influenza A virus causes alpha-synuclein aggregation. Proc Natl Acad Sci USA 117:6741–6751
Matschke J, Lutgehetmann M, Hagel C, Sperhake JP, Schroder AS, Edler C, Mushumba H, Fitzek A, Allweiss L, Dandri M et al (2020) Neuropathology of patients with COVID-19 in Germany: a post-mortem case series. Lancet Neurol 19:919–929
McBride R, van Zyl M, Fielding BC (2014) The coronavirus nucleocapsid is a multifunctional protein. Viruses 6:2991–3018
Molliex A, Temirov J, Lee J, Coughlin M, Kanagaraj AP, Kim HJ, Mittag T, Taylor JP (2015) Phase separation by low complexity domains promotes stress granule assembly and drives pathological fibrillization. Cell 163:123–133
Monette A, Niu M, Chen L, Rao S, Gorelick RJ, Mouland AJ (2020) Pan-retroviral nucleocapsid-mediated phase separation regulates genomic RNA positioning and trafficking. Cell Rep 31:107520
Moosa MM, Banerjee PR (2020) Subversion of host stress granules by coronaviruses: potential roles of pi-rich disordered domains of viral nucleocapsids. J Med Virol. https://doi.org/10.1002/jmv.26195
Onomoto K, Jogi M, Yoo JS, Narita R, Morimoto S, Takemura A, Sambhara S, Kawaguchi A, Osari S, Nagata K et al (2012) Critical role of an antiviral stress granule containing RIG-I and PKR in viral detection and innate immunity. PLoS ONE 7:e43031
Paniz-Mondolfi A, Bryce C, Grimes Z, Gordon RE, Reidy J, Lednicky J, Sordillo EM, Fowkes M (2020) Central nervous system involvement by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Med Virol 92:699–702
Patel A, Lee HO, Jawerth L, Maharana S, Jahnel M, Hein MY, Stoynov S, Mahamid J, Saha S, Franzmann TM et al (2015) A liquid-to-solid phase transition of the ALS protein FUS accelerated by disease mutation. Cell 162:1066–1077
Peng TY, Lee KR, Tarn WY (2008) Phosphorylation of the arginine/serine dipeptide-rich motif of the severe acute respiratory syndrome coronavirus nucleocapsid protein modulates its multimerization, translation inhibitory activity and cellular localization. FEBS J 275:4152–4163
Perdikari TM, Murthy AC, Ryan VH, Watters S, Naik MT, Fawzi NL (2020) SARS-CoV-2 nucleocapsid protein phase-separates with RNA and with human hnRNPs. EMBO J 39:e106478
Protter DSW, Parker R (2016) Principles and properties of stress granules. Trends Cell Biol 26:668–679
Qamar S, Wang G, Randle SJ, Ruggeri FS, Varela JA, Lin JQ, Phillips EC, Miyashita A, Williams D, Strohl F et al (2018) FUS phase separation is modulated by a molecular chaperone and methylation of arginine cation-pi interactions. Cell 173:720–734
Readhead B, Haure-Mirande JV, Funk CC, Richards MA, Shannon P, Haroutunian V, Sano M, Liang WS, Beckmann ND, Price ND et al (2018) Multiscale analysis of independent Alzheimer’s cohorts finds disruption of molecular, genetic, and clinical networks by human herpesvirus. Neuron 99:64–82
Saikatendu KS, Joseph JS, Subramanian V, Neuman BW, Buchmeier MJ, Stevens RC, Kuhn P (2007) Ribonucleocapsid formation of severe acute respiratory syndrome coronavirus through molecular action of the N-terminal domain of N protein. J Virol 81:3913–3921
Savastano A, Ibanez de Opakua A, Rankovic M, Zweckstetter M (2020) Nucleocapsid protein of SARS-CoV-2 phase separates into RNA-rich polymerase-containing condensates. Nat Commun 11:6041
Serrano-Castro PJ, Estivill-Torrus G, Cabezudo-Garcia P, Reyes-Bueno JA, Ciano Petersen N, Aguilar-Castillo MJ, Suarez-Perez J, Jimenez-Hernandez MD, Moya-Molina MA, Oliver-Martos B et al (2020) Impact of SARS-CoV-2 infection on neurodegenerative and neuropsychiatric diseases: a delayed pandemic? Neurologia 35:245–251
Singal CMS, Jaiswal P, Seth P (2020) SARS-CoV-2, more than a respiratory virus: its potential role in neuropathogenesis. ACS Chem Neurosci 11:1887–1899
Song E, Zhang C, Israelow B, Lu-Culligan A, Prado AV, Skriabine S, Lu P, Weizman OE, Liu F, Dai Y et al (2021) Neuroinvasion of SARS-CoV-2 in human and mouse brain. J Exp Med 218:e20202135
Soresina A, Moratto D, Chiarini M, Paolillo C, Baresi G, Foca E, Bezzi M, Baronio B, Giacomelli M, Badolato R (2020) Two X-linked agammaglobulinemia patients develop pneumonia as COVID-19 manifestation but recover. Pediatr Allergy Immunol 31(5):565–569
Thevarajan I, Nguyen THO, Koutsakos M, Druce J, Caly L, van de Sandt CE, Jia X, Nicholson S, Catton M, Cowie B et al (2020) Breadth of concomitant immune responses prior to patient recovery: a case report of non-severe COVID-19. Nat Med 26:453–455
Wolozin B, Ivanov P (2019) Stress granules and neurodegeneration. Nat Rev Neurosci 20:649–666
Wu F, Zhao S, Yu B, Chen YM, Wang W, Song ZG, Hu Y, Tao ZW, Tian JH, Pei YY et al (2020) A new coronavirus associated with human respiratory disease in China. Nature 579:265–269
Zhang X, Wang F, Hu Y, Chen R, Meng D, Guo L, Lv H, Guan J, Jia Y (2020) In vivo stress granule misprocessing evidenced in a FUS knock-in ALS mouse model. Brain 143:1350–1367
Zhao D, Xu W, Zhang X, Wang X, Ge Y, Yuan E, Xiong Y, Wu S, Li S, Wu N et al (2021) Understanding the phase separation characteristics of nucleocapsid protein provides a new therapeutic opportunity against SARS-CoV-2. Protein Cell 12:734–740
Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, Si HR, Zhu Y, Li B, Huang CL et al (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 579:270–273
Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, Zhao X, Huang B, Shi W, Lu R et al (2020) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382:727–733
Acknowledgements
This work was supported by the National Natural Science Foundation (NSF) of China (32170683, 82188101, 32171236, 31872716, 32070049, 82041016), the Major State Basic Research Development Program (2019YFE0120600), the Science and Technology Commission of Shanghai Municipality (STCSM) (20XD1425000 and 2019SHZDZX02), CAS project for Young Scientists in Basic research (YSBR-009), the Eastern Scholar project supported by Shanghai Municipal Education Commission, National Key R&D Program of China (2021YFC2301700, 2021YFA1301900), Yunnan Key Research and Development project (202103AQ100001), CAMS Innovation Fund for Medical Sciences(2021-I2M-1-038), special research fund on COVID-19 of Sichuan Province (2020YFS0010).
Abbreviations
ACE2, angiotensin converting enzyme 2; AD, Alzheimer’s disease; ALS, amyotrophic lateral sclerosis; COVID-19, coronavirus disease 2019; E, envelope; FRAP, fluorescence recovery after photobleaching; FTD, frontotemporal dementia; LC, low complexity; LLPS, liquid-liquid phase separation; M, membrane; MOI, multiplicity of infection; N protein, nucleocapsid protein; NMR, nuclear magnetic resonance; Nsp; non-structural proteins; Orfs, open reading frames; PD, Parkinson’s disease; S, spike; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2; SG, stress granule; TEM, transmission electron microscopy.
Author contributions
D.L. and C.L. designed the project. Y.L., S.L., J.Y. and X.P. performed virus-infected cellular experiments. Y.L., S.Z., Y.W., C.Z., Z.S. and J.L. prepared N protein, J.G., Y.S. and Y.L. prepared the TDP43, hnRNPA1 and FUS samples. Y.L., W.X and J.G. performed the in vitro biochemical characterization of protein LLPS. Y.L. and S.Z. performed NMR experiments. Y.L. and J.G. performed all cellular experiments. W.X. performed the TEM measurement. All of the authors are involved in analyzing the data and contributed to manuscript discussion and editing. D.L. and Y.L. wrote the manuscript.
Compliance with ethics guidelines
Yichen Li, Shuaiyao Lu, Jinge Gu, Wencheng Xia, Shengnan Zhang, Shenqing Zhang, Yan Wang, Chong Zhang, Yunpeng Sun, Jian Lei, Cong Liu, Zhaoming Su, Juntao Yang, Xiaozhong Peng and Dan Li declare that they have no conflict of interest. This article does not contain any studies with human or animal subjects performed by the any of the authors. All the participants agreed to the publication.
Author information
Authors and Affiliations
Corresponding authors
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, Y., Lu, S., Gu, J. et al. SARS-CoV-2 impairs the disassembly of stress granules and promotes ALS-associated amyloid aggregation. Protein Cell 13, 602–614 (2022). https://doi.org/10.1007/s13238-022-00905-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13238-022-00905-7