Abstract
Background
Despite ample evidence of high depression rates among women with high-risk pregnancies, there is limited information available regarding the effectiveness of Internet-based psychotherapies in this population. This study aimed to assess the effectiveness of internet-based psychotherapy in treating depression and anxiety in pregnant women with high-risk pregnancies admitted to the hospital.
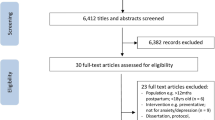
Methods
In a quasi-experimental study, 60 inpatient women with high-risk pregnancies exhibiting mild to moderate depression were allocated to either the experimental (n = 30) or control (n = 30) group. The experimental group received medical therapy with Internet-based Synchronous Individualized Therapy for six sessions, each lasting 50–60 min, conducted over six weeks. The control group solely received medical therapy. All participants completed questionnaires, including the Brief Symptom Inventory (BSI-18) and Edinburgh Postnatal Depression Scale, at both baseline and the post-trial stage (6 weeks after the study commencement).
Results
The mean scores for depression and anxiety in both groups were elevated (experimental group: M = 11.36, SD = 4.84; M = 13.82, SD = 4.78; control group: M = 11.4, SD = 4.8; M = 13.6, SD = 4.6). Symptom severity decreased more significantly in the group receiving internet psychotherapy in addition to medical treatment than in the control group, with medium effect sizes observed for depression symptoms (η2 = 0.145, P = 0.003) and anxiety symptoms (η2 = 0.238, P < 0.001). Furthermore, the reduction in anxiety and depression scores in the internet psychotherapy group was notably more significant than in the control group, with a moderate effect size (η2 = 0.177, P = 0.041).
Conclusion
Augmenting medical therapy with therapist-guided internet-based psychotherapy may effectively reduce depression, anxiety, and psychological distress in pregnant women experiencing high-risk pregnancies and comorbid depression. These findings suggest that hospitalized, depressed pregnant women with high-risk pregnancies should be offered internet-based psychotherapy as an adjunctive treatment option.

Similar content being viewed by others
References
Queenan JT, Spong CY, Lockwood CJ. Queenan’s management of high-risk pregnancy: an evidence-based approach. Wiley; 2012.
Mirzakhani K, Ebadi A, Faridhosseini F, Khadivzadeh T. Well-being in high-risk pregnancy: an integrative review. BMC Pregnancy Childbirth. 2020;20:526.
Rodrigues PB, Zambaldi CF, Cantilino A, Sougey EB. Special features of high-risk pregnancies as factors in development of mental distress: a review. Trends Psychiatry Psychother. 2016;38:136–40.
Tsakiridis I, Bousi V, Dagklis T, Sardeli C, Nikolopoulou V, Papazisis G. Epidemiology of antenatal depression among women with high-risk pregnancies due to obstetric complications: a scoping review. Arch Gynecol Obstet. 2019;300:849–59.
Obrochta CA, Chambers C, Bandoli G. Psychological distress in pregnancy and postpartum. Women Birth. 2020;33:583–91.
Soteriou M, Naar H, Teroni F. The ontology of emotion. The Ontology Of Emotions. 2018:71–89.
Basirat Z, Ramaezani F, Sepidarkish M, Kashifard M, Faramarzi M. Psychiatric Symptoms in Women with High-risk Pregnancy in the Postpartum Period: A Case-control Study. Revista Brasileira de Ginecologia e Obstetricia/RBGO-Gynecology and Obstetrics. 2023;45:186–91.
Simmons HA, Goldberg LS. ‘High-risk’pregnancy after perinatal loss: understanding the label. Midwifery. 2011;27:452–7.
Roomaney R, Andipatin MG, Naidoo A. The psychological experience of women who survived HELLP syndrome in Cape Town. South Africa Health SA Gesondheid. 2014;19:1–9.
Yedid Sion M, Harlev A, Weintraub AY, Sergienko R, Sheiner E. Is antenatal depression associated with adverse obstetric and perinatal outcomes? J Matern Fetal Neonatal Med. 2016;29:863–7.
Logsdon MC, Wisner KL, Pinto-Foltz MD. The impact of postpartum depression on mothering. J Obstet Gynecol Neonatal Nurs. 2006;35:652–8.
Lépine J-P, Briley M. The increasing burden of depression. Neuropsychiatr Dis Treat. 2011;7:3–7.
Kazdin AE, Blase SL. Rebooting psychotherapy research and practice to reduce the burden of mental illness. Perspect Psychol Sci. 2011;6:21–37.
Schröder J, Berger T, Westermann S, Klein JP, Moritz S. Internet interventions for depression: new developments. Dialogues Clin Neurosci. 2016;18:203–12.
Kingston D, Janes-Kelley S, Tyrrell J, Clark L, Hamza D, Holmes P, et al. An integrated web-based mental health intervention of assessment-referral-care to reduce stress, anxiety, and depression in hospitalized pregnant women with medically high-risk pregnancies: a feasibility study protocol of hospital-based implementation. JMIR Res Protocols. 2015;4:e4037.
Goetz M, Schiele C, Müller M, Matthies LM, Deutsch TM, Spano C, et al. Effects of a brief electronic mindfulness-based intervention on relieving prenatal depression and anxiety in hospitalized high-risk pregnant women: exploratory pilot study. J Med Internet Res. 2020;22:e17593.
McCabe-Beane JE, Segre LS, Perkhounkova Y, Stuart S, O’Hara MW. The identification of severity ranges for the Edinburgh Postnatal Depression Scale. J Reprod Infant Psychol. 2016;34:293–303.
Kharaghani R, Shariati M, Yunesian M, Keramat A, Moghisi A. The Iranian integrated maternal health care guideline based on evidence-based medicine and American guidelines: a comparative study. Mod Care J. 2016;13.
Hamidia A, Kheirkhah F, Faramarzi M, Basirat Z, Ghadimi R, Chehrazi M, et al. Depressive symptoms and psychological distress from antenatal to postnatal period in women with high-risk pregnancy: a prospective study during the COVID-19 pandemic. Indian J Psychiatry. 2021;63:536–42.
Mazhari S, Nakhaee N. Validation of the Edinburgh Postnatal depression scale in an Iranian sample. Arch Womens Ment Health. 2007;10:293–7.
Jaremko M, Meichenbaum D. Stress reduction and prevention. Springer; 2013.
Vahidi A, Shaker DA. The role of caregiver burden, marital stress, and mindfulness in predicting psychosocial adjustment to illness in people with coronary artery disease. Iran J Cardiovasc Nurs. 2018;7:50–9.
Meichenbaum D. Roadmap to resilience: a guide for military. Trauma Victims and Their Families: Institute Press; 2012.
Cohen J. Statistical power analysis for the behavioral sciences. 2nd ed. New York: Routledge; 1988.
Grassi L, Caruso R, Mitchell AJ, Sabato S, Nanni MG. Screening for emotional disorders in patients with cancer using the Brief Symptom Inventory (BSI) and the BSI-18 versus a standardized psychiatric interview (the World Health Organization Composite International Diagnostic Interview). Cancer. 2018;124:2415–26.
Akhavan Abiri F, Shairi MR. Short forms of symptom checklist (SCL): investigation of validity & reliability. Clin Psychol Personal. 2020;18:137–62.
ForsellBendixHolländareSzymanska von SchultzNasiellBlomdahl-Wetterholm EMFBJM, et al. Internet delivered cognitive behavior therapy for antenatal depression: a randomised controlled trial. J Affect Disord. 2017;221:56–64.
Heller HM, Hoogendoorn AW, Honig A, Broekman BF, van Straten A. The effectiveness of a guided internet-based tool for the treatment of depression and anxiety in pregnancy (MamaKits Online): randomized controlled trial. J Med Internet Res. 2020;22:e15172.
Milgrom J, Danaher BG, Seeley JR, Holt CJ, Holt C, Ericksen J, et al. Internet and face-to-face cognitive behavioral therapy for postnatal depression compared with treatment as usual: randomized controlled trial of MumMoodBooster. J Med Internet Res. 2021;23:e17185.
Acknowledgements
The authors would like to express their gratitude to The National Institute for Medical Research Development (NIMAD) for supporting the funding (Grant Number: 973413). The funder reviewed the project plan and rewarded a small grant for implementation of the project. The Ethical Committee of the National Institute for Medical Research Development (NIMAD) approved the study (IR.NIMAD.REC.1398.015). Also, we would like to thank Noushin Fatri for helping us to invite the patients
Funding
This study was supported by the. National Institute for Medical Research Development (NIMAD) Grant No. 973413.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares no conflict of interest.
Ethical Approval
This project was approved by Ethic Committee of National Institute for Medical Research Development (NIMAD) (IR.NIMAD.REC.1398.015).
Informed Consent
Informed written consent was obtained from each participant before participating in the study. Anonymity and confidentiality for participants were guaranteed. All methods were carried out in accordance with Declaration of Helsinki guidelines and regulations.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Shirin Shahrokhi is a MsC Student; Zahra Basirat is a Professor; Shahnaz Barat is a Associate Professor; Farzan Kheirkhah is a Professor; Elizabeth O’Connor is a Investigator; Seyyedeh Mahboubeh Mirtabar is a PhD candidate; Mahbobeh Faramarzi is a Professor.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shahrokhi, S., Basirat, Z., Barat, S. et al. The Efficacy of Therapist-Guided Internet-Based Psychotherapy for Treating Mild to Moderate Depression and Anxiety Among Women Hospitalized with High-Risk Pregnancies. J Obstet Gynecol India (2024). https://doi.org/10.1007/s13224-024-01946-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13224-024-01946-0