Abstract
Purpose
Antenatal depression is a common mental health problem among pregnant women that negatively affects maternal and neonatal outcomes. Women with obstetric complications, defined as high-risk pregnancies, seem to be at particularly increased risk for developing depressive symptomatology. The purpose of this study was to review the prevalence of antenatal depression among pregnant women with obstetric complications and to identify possible associated factors.
Methods
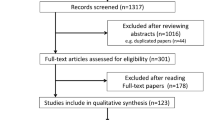
A literature search was performed in the PubMed database and a scoping review was conducted to identify studies with data on the prevalence of antenatal depression and associated factors among high-risk pregnancies due to obstetric complications. The included studies were written in English and published up to 31/12/2018.
Results
The prevalence of antenatal depression among pregnant women with high-risk pregnancies ranges from 12.5 to 44.2% among the reviewed studies. The associated factors significantly associated with antenatal depression include maternal age, maternal education, dwelling place, relationship with the partner, previous psychiatric diagnosis, perceived stress, antenatal attachment, abortion thoughts, smoking, diabetes, parity, number of pregnancies, gestational age, threatened preterm labour, preeclampsia and oligohydramnios.
Conclusions
Our findings indicate a high prevalence of depressive disorders in women with obstetric complications, suggesting the need for more rigorous screening among this population. The identification of associated factors also merits clinical attention. Further research is warranted to develop evidence-based effective screening strategies and relevant interventions.

Similar content being viewed by others
References
WHO (2008) World Health Organisation. Improving Maternal Mental Health: Millennium Developmental Goal, p 5
Brandon AR, Trivedi MH, Hynan LS, Miltenberger PD, Labat DB, Rifkin JB, Stringer CA (2008) Prenatal depression in women hospitalized for obstetric risk. J Clin Psychiatry 69(4):635–643
Logsdon MC, Wisner KL, Pinto-Foltz MD (2006) The impact of postpartum depression on mothering. J Obstet Gynecol Neonatal Nurs 35(5):652–658. https://doi.org/10.1111/j.1552-6909.2006.00087.x
Gotlib IH, Whiffen VE, Mount JH, Milne K, Cordy NI (1989) Prevalence rates and demographic characteristics associated with depression in pregnancy and the postpartum. J Consult Clin Psychol 57(2):269–274
Austin MP (2004) Antenatal screening and early intervention for "perinatal" distress, depression and anxiety: where to from here? Arch Womens Ment Health 7(1):1–6. https://doi.org/10.1007/s00737-003-0034-4
Koutra K, Vassilaki M, Georgiou V, Koutis A, Bitsios P, Chatzi L, Kogevinas M (2014) Antenatal maternal mental health as determinant of postpartum depression in a population based mother-child cohort (Rhea Study) in Crete. Greece Soc Psychiatry Psychiatr Epidemiol 49(5):711–721. https://doi.org/10.1007/s00127-013-0758-z
Dagklis T, Papazisis G, Tsakiridis I, Chouliara F, Mamopoulos A, Rousso D (2016) Prevalence of antenatal depression and associated factors among pregnant women hospitalized in a high-risk pregnancy unit in Greece. Soc Psychiatry Psychiatr Epidemiol 51(7):1025–1031. https://doi.org/10.1007/s00127-016-1230-7
Dibaba Y, Fantahun M, Hindin MJ (2013) The association of unwanted pregnancy and social support with depressive symptoms in pregnancy: evidence from rural Southwestern Ethiopia. BMC Pregnancy Childbirth 13:135. https://doi.org/10.1186/1471-2393-13-135
Melo EF Jr, Cecatti JG, Pacagnella RC, Leite DF, Vulcani DE, Makuch MY (2012) The prevalence of perinatal depression and its associated factors in two different settings in Brazil. J Affect Disord 136(3):1204–1208. https://doi.org/10.1016/j.jad.2011.11.023
Nasreen HE, Kabir ZN, Forsell Y, Edhborg M (2011) Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: a population based study in rural Bangladesh. BMC Womens Health 11:22. https://doi.org/10.1186/1472-6874-11-22
Mohammad KI, Gamble J, Creedy DK (2011) Prevalence and factors associated with the development of antenatal and postnatal depression among Jordanian women. Midwifery 27(6):e238–245. https://doi.org/10.1016/j.midw.2010.10.008
Ritter C, Hobfoll SE, Lavin J, Cameron RP, Hulsizer MR (2000) Stress, psychosocial resources, and depressive symptomatology during pregnancy in low-income, inner-city women. Health Psychol 19(6):576–585
Alder J, Fink N, Bitzer J, Hosli I, Holzgreve W (2007) Depression and anxiety during pregnancy: a risk factor for obstetric, fetal and neonatal outcome? A critical review of the literature. J Matern Fetal Neonatal Med 20(3):189–209. https://doi.org/10.1080/14767050701209560
Grote NK, Bridge JA, Gavin AR, Melville JL, Iyengar S, Katon WJ (2010) A meta-analysis of depression during pregnancy and the risk of preterm birth, low birth weight, and intrauterine growth restriction. Arch Gen Psychiatry 67(10):1012–1024. https://doi.org/10.1001/archgenpsychiatry.2010.111
Hermon N, Wainstock T, Sheiner E, Golan A, Walfisch A (2019) Impact of maternal depression on perinatal outcomes in hospitalized women-a prospective study. Arch Womens Ment Health 22(1):85–91. https://doi.org/10.1007/s00737-018-0883-5
Yedid Sion M, Harlev A, Weintraub AY, Sergienko R, Sheiner E (2016) Is antenatal depression associated with adverse obstetric and perinatal outcomes? J Matern Fetal Neonatal Med 29(6):863–867. https://doi.org/10.3109/14767058.2015.1023708
Field T (2011) Prenatal depression effects on early development: a review. Infant Behav Dev 34(1):1–14. https://doi.org/10.1016/j.infbeh.2010.09.008
ACOG Committee Opinion No. 757 (2018) Screening for perinatal depression. American College of Obstetricians and Gynecologists. Obstet Gynecol 132:e208–12
NICE (2014) National Institute for Health and Care Excellence. Antenatal and postnatal mental health: clinical management and service guidance. https://www.nice.org.uk/guidance/cg192
RANZCOG (2015) The Royal Australian and New Zealand College of Obstetricians and Gynaecologists. Perinatal Anxiety and Depression (C-Obs 48)
Siu AL, Force USPST, Bibbins-Domingo K, Grossman DC, Baumann LC, Davidson KW, Ebell M, Garcia FA, Gillman M, Herzstein J, Kemper AR, Krist AH, Kurth AE, Owens DK, Phillips WR, Phipps MG, Pignone MP (2016) Screening for depression in adults: US preventive services task force recommendation statement. JAMA 315(4):380–387. https://doi.org/10.1001/jama.2015.18392
Hidalgo Landa A, Szabo I, Le Brun L, Owen I, Fletcher G (2011) Evidence based scoping reviews. Electr J Inf Syst Eval 14:46–52
Arskey H, O’Malley L (2005) Scoping studies: towards a methodological framework. I J Soc Res Methodol 8(1):9–32
Daudt HM, van Mossel C, Scott SJ (2013) Enhancing the scoping study methodology: a large, inter-professional team’s experience with Arksey and O'Malley's framework. BMC Med Res Methodol 13:48. https://doi.org/10.1186/1471-2288-13-48
Dagklis T, Tsakiridis I, Chouliara F, Mamopoulos A, Rousso D, Athanasiadis A, Papazisis G (2018) Antenatal depression among women hospitalized due to threatened preterm labor in a high-risk pregnancy unit in Greece. J Matern Fetal Neonatal Med 31(7):919–925. https://doi.org/10.1080/14767058.2017.1301926
Dame P, Cherubini K, Goveia P, Pena G, Galliano L, Facanha C, Nunes MA (2017) Depressive symptoms in women with gestational diabetes mellitus: the LINDA-Brazil study. J Diabetes Res 2017:7341893. https://doi.org/10.1155/2017/7341893
Kharaghani R, Geranmaye M, Janani L, Hantooshzade S, Arbabi M, Rahmani Bilandi R, Bagheri F (2012) Preeclampsia and depression: a case–control study in Tehran. Arch Gynecol Obstet 286(1):249–253. https://doi.org/10.1007/s00404-012-2260-3
Qiu C, Sanchez SE, Lam N, Garcia P, Williams MA (2007) Associations of depression and depressive symptoms with preeclampsia: results from a Peruvian case-control study. BMC Womens Health 7:15. https://doi.org/10.1186/1472-6874-7-15
Uguz F, Gezginc K, Yazici F (2011) Are major depression and generalized anxiety disorder associated with intrauterine growth restriction in pregnant women? A case–control study. Gen Hosp Psychiatry 33(6):640e647–649. https://doi.org/10.1016/j.genhosppsych.2011.05.007
Tsakiridis I, Dagklis T, Zerva C, Mamopoulos A, Athanasiadis A, Papazisis G (2019) Depression in pregnant women hospitalized due to intrauterine growth restriction: prevalence and associated factors. Midwifery 70:71–75. https://doi.org/10.1016/j.midw.2018.12.008
Uguz F, Gezginc K, Korucu DG, Sayal B, Turgut K (2017) Are Major depression and generalized anxiety disorder associated with oligohydramnios in pregnant women? A case–control study. Perspect Psychiatr Care 53(4):275–279. https://doi.org/10.1111/ppc.12174
Bisson M, Series F, Giguere Y, Pamidi S, Kimoff J, Weisnagel SJ, Marc I (2014) Gestational diabetes mellitus and sleep-disordered breathing. Obstet Gynecol 123(3):634–641. https://doi.org/10.1097/AOG.0000000000000143
Ertel KA, Silveira M, Pekow P, Braun B, Manson JE, Solomon CG, Markenson G, Chasan-Taber L (2014) Prenatal depressive symptoms and abnormalities of glucose tolerance during pregnancy among Hispanic women. Arch Womens Ment Health 17(1):65–72. https://doi.org/10.1007/s00737-013-0379-2
Katon JG, Russo J, Gavin AR, Melville JL, Katon WJ (2011) Diabetes and depression in pregnancy: is there an association? J Womens Health (Larchmt) 20(7):983–989. https://doi.org/10.1089/jwh.2010.2662
Ragland D, Payakachat N, Hays EB, Banken J, Dajani NK (2003) Ott RE (2010) Depression and diabetes: establishing the pharmacist’s role in detecting comorbidity in pregnant women. J Am Pharm Assoc 50(2):195–199. https://doi.org/10.1331/JAPhA.2010.09191
Varela P, Spyropoulou AC, Kalogerakis Z, Vousoura E, Moraitou M, Zervas IM (2017) Association between gestational diabetes and perinatal depressive symptoms: evidence from a Greek cohort study. Prim Health Care Res Dev 18(5):441–447. https://doi.org/10.1017/S1463423617000317
Byrn M, Penckofer S (2015) The relationship between gestational diabetes and antenatal depression. J Obstet Gynecol Neonatal Nurs 44(2):246–255. https://doi.org/10.1111/1552-6909.12554
Huang T, Rifas-Shiman SL, Ertel KA, Rich-Edwards J, Kleinman K, Gillman MW, Oken E, James-Todd T (2015) Pregnancy hyperglycaemia and risk of prenatal and postpartum depressive symptoms. Paediatr Perinat Epidemiol 29(4):281–289. https://doi.org/10.1111/ppe.12199
Keskin FE, Ozyazar M, Pala AS, Elmali AD, Yilmaz B, Uygunoglu U, Bozluolcay M, Tuten A, Bingol A, Hatipoglu E (2015) Evaluation of cognitive functions in gestational diabetes mellitus. Exp Clin Endocrinol Diabetes 123(4):246–251. https://doi.org/10.1055/s-0034-1395634
Natasha K, Hussain A, Khan AK (2015) Prevalence of depression among subjects with and without gestational diabetes mellitus in Bangladesh: a hospital based study. J Diabetes Metab Disord 14:64. https://doi.org/10.1186/s40200-015-0189-3
Byatt N, Hicks-Courant K, Davidson A, Levesque R, Mick E, Allison J, Moore Simas TA (2014) Depression and anxiety among high-risk obstetric inpatients. Gen Hosp Psychiatry 36(6):644–649. https://doi.org/10.1016/j.genhosppsych.2014.07.011
Murray L, Carothers AD (1990) The validation of the Edinburgh post-natal depression scale on a community sample. Br J Psychiatry 157:288–290
Brouwers EP, van Baar AL, Pop VJ (2001) Does the Edinburgh postnatal depression scale measure anxiety? J Psychosom Res 51(5):659–663
Gibson J, McKenzie-McHarg K, Shakespeare J, Price J, Gray R (2009) A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand 119(5):350–364. https://doi.org/10.1111/j.1600-0447.2009.01363.x
Kroenke K, Spitzer RL, Williams JB (2001) The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med 16(9):606–613
Adouard F, Glangeaud-Freudenthal NM, Golse B (2005) Validation of the Edinburgh postnatal depression scale (EPDS) in a sample of women with high-risk pregnancies in France. Arch Womens Ment Health 8(2):89–95. https://doi.org/10.1007/s00737-005-0077-9
Thiagayson P, Krishnaswamy G, Lim ML, Sung SC, Haley CL, Fung DS, Allen JC Jr, Chen H (2013) Depression and anxiety in Singaporean high-risk pregnancies—prevalence and screening. Gen Hosp Psychiatry 35(2):112–116. https://doi.org/10.1016/j.genhosppsych.2012.11.006
Biaggi A, Conroy S, Pawlby S, Pariante CM (2016) Identifying the women at risk of antenatal anxiety and depression: a systematic review. J Affect Disord 191:62–77. https://doi.org/10.1016/j.jad.2015.11.014
Melville JL, Gavin A, Guo Y, Fan MY, Katon WJ (2010) Depressive disorders during pregnancy: prevalence and risk factors in a large urban sample. Obstet Gynecol 116(5):1064–1070. https://doi.org/10.1097/AOG.0b013e3181f60b0a
Vitale SG, La Rosa VL, Rapisarda AM, Lagana AS (2017) Psychology of infertility and assisted reproductive treatment: the Italian situation. J Psychosom Obstet Gynaecol 38(1):1–3. https://doi.org/10.1080/0167482X.2016.1244184
Gdanska P, Drozdowicz-Jastrzebska E, Grzechocinska B, Radziwon-Zaleska M, Wegrzyn P, Wielgos M (2017) Anxiety and depression in women undergoing infertility treatment. Ginekol Pol 88(2):109–112. https://doi.org/10.5603/GP.a2017.0019
Pope CJ, Sharma V, Sharma S, Mazmanian D (2015) A Systematic review of the association between psychiatric disturbances and endometriosis. J Obstet Gynaecol Can 37(11):1006–1015. https://doi.org/10.1016/S1701-2163(16)30050-0
Lagana AS, La Rosa VL, Rapisarda AMC, Valenti G, Sapia F, Chiofalo B, Rossetti D, Ban Frangez H, Vrtacnik Bokal E, Vitale SG (2017) Anxiety and depression in patients with endometriosis: impact and management challenges. Int J Womens Health 9:323–330. https://doi.org/10.2147/IJWH.S119729
Zullo F, Spagnolo E, Saccone G, Acunzo M, Xodo S, Ceccaroni M, Berghella V (2017) Endometriosis and obstetrics complications: a systematic review and meta-analysis. Fertil Steril 108(4):667–672 e665. https://doi.org/10.1016/j.fertnstert.2017.07.019
Dennis CL, Falah-Hassani K, Shiri R (2017) Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br J Psychiatry 210(5):315–323. https://doi.org/10.1192/bjp.bp.116.187179
Funding
None.
Author information
Authors and Affiliations
Contributions
IT: project development, title and abstracts screening, data analysis, manuscript writing. VB: title and abstracts screening, data collection, data analysis, manuscript writing. TD: data analysis, manuscript drafting, CS: data collection, manuscript editing, VN: data collection, manuscript drafting, GP: project development, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Informed consent
This is a review study; informed consent is not required.
Ethical approval
This is a review study; ethical approval is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsakiridis, I., Bousi, V., Dagklis, T. et al. Epidemiology of antenatal depression among women with high-risk pregnancies due to obstetric complications: a scoping review. Arch Gynecol Obstet 300, 849–859 (2019). https://doi.org/10.1007/s00404-019-05270-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-019-05270-1