Abstract
Background
The efficacy of a single bolus dose of epidural dexamethasone added to levobupivacaine–fentanyl combination for labor analgesia has not been studied. In this randomized double-blind controlled trial, we assessed the effect of epidural dexamethasone in reducing the hourly average consumption of epidural levobupivacaine–fentanyl combination in laboring parturients and to study its effect on pain score, maternal satisfaction, maternal and neonatal outcome.
Methods
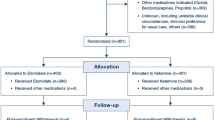
Sixty adult ASA I-II single-gestation full-term primigravid laboring parturients with cervical dilation ≤ 5 cm were randomly assigned to two equal-sized groups. Combined spinal–epidural block was performed in all the parturients. After placing the epidural catheter in epidural space, 8 mg of preservative-free dexamethasone was administered to the dexamethasone group, and 0.9% saline to the placebo group. All parturients received continuous background infusion of 5 ml of 0.1% levobupivacaine with 2 μg/ml of fentanyl with the provision of patient-controlled bolus of 5 ml of 0.1% levobupivacaine with 2 μg/ml of fentanyl (lockout interval 15 min). The primary outcome measure was the hourly total consumption of levobupivacaine–fentanyl mixture. The secondary outcome measures were maternal satisfaction, pain score, maternal hemodynamic parameters, fetal heart rate, duration of second stage of labor, mode of delivery, Apgar scores and adverse effects.
Results
Hourly drug consumption and hourly bolus requirement were significantly lower in the dexamethasone group than placebo group (6.97 ml ± 1.22 vs. 8.40 ml ± 2.59 and 0.41 ± 0.26 vs. 0.72 ± 0.55, respectively, P = 0.008 for both). There were no significant differences in other outcome measures.
Conclusion
Epidural dexamethasone significantly decreased average hourly drug consumption and the number of boluses in laboring parturients, thus providing epidural drug dose-sparing effect.

Similar content being viewed by others
References
Sng BL, Kwok SC, Sia AT. Modern neuraxial labor analgesia. Curr Opin Anaesthesiol. 2015;28:285–9.
Wong CA. Labor analgesia: is there an ideal technique? Anesth Analg. 2009;109:296–8.
Pandya ST. Labor analgesia: recent advances. Indian J Anaesth. 2010;54:400–8.
Albrecht E, Kern C, Kirkham KR. A systematic review and meta-analysis of perineural dexamethasone for peripheral nerve blocks. Anaesthesia. 2015;70:71–83.
Li X, Xu G, Xie W, et al. The efficacy and safety of dexamethasone for pain management after total knee arthroplasty: a systematic review and meta-analysis. Int J Surg. 2018;53:65–71.
Toner AJ, Ganeshanathan V, Chan MT, et al. Safety of perioperative glucocorticoids in elective noncardiac surgery: a systematic review and meta-analysis. Anesthesiology. 2017;126:234–48.
Curry PD, Pacsoo C, Heap DG. Patient-controlled epidural analgesia in obstetric anesthetic practice. Pain. 1994;57:125–7.
Ross VH, Pan PH, Owen MD, et al. Neostigmine decreases bupivacaine use by patient-controlled epidural analgesia during labor: a randomized controlled study. Anesth Analg. 2009;109:524–31.
Hefni AF, Mahmoud MS, Al Alim AA. Epidural dexamethasone for post-operative analgesia in patients undergoing abdominal hysterectomy: a dose ranging and safety evaluation study. Saudi J Anesth. 2014;8:323–7.
Naghipour B, Aghamohamadi D, Azarfarin R, et al. Dexamethasone added to bupivacaine prolongs duration of epidural analgesia. Middle East J Anesthesiol. 2013;22:53–7.
Jo YY, Yoo JH, Kim HJ, et al. The effect of epidural administration of dexamethasone on postoperative pain: a randomized controlled study in radical subtotal gastrectomy. Korean J Anesthesiol. 2011;61:233–7.
Waldron NH, Jones CA, Gan TJ, et al. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth. 2013;110:191–200.
Hussain N, Van den Langenbergh T, Sermer C, et al. Equivalent analgesic effectiveness between perineural and intravenous dexamethasone as adjuvants for peripheral nerve blockade: a systematic review and meta-analysis. Can J Anaesth. 2018;65(2):194–206.
Zorrilla-Vaca A, Li J. Dexamethasone injected perineurally is more effective than administered intravenously for peripheral nerve blocks: a meta-analysis of randomized controlled trials. Clin J Pain. 2018;34:276–84.
Min SH, Soh JS, Park JY, et al. Epidural dexamethasone decreased inflammatory hyperalgesia and spinal cPLA2 expression in a rat formalin test. Yonsei Med J. 2014;55:1631–9.
Wang LZ, Hu XX, Liu X, et al. Influence of epidural dexamethasone on maternal temperature and serum cytokine concentration after labor epidural analgesia. Int J Gynaec Obstet. 2011;113:40–3.
Wahdan AS, El-Sakka AI, Gaafar HM. The effect of addition of dexamethasone to levobupivacaine in parturients receiving combined spinal-epidural for analgesia for vaginal delivery. Indian J Anaesth. 2017;61:556–61.
Ali HM, Wahdan A. Using dexamethasone as an adjuvant to levobupivacaine in epidural anesthesia to change the pain intensity and duration in painless labor. Saudi J Anaesth. 2018;12:209–14.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare that they have no conflict of interest.
Human and Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Informed Consent
Informed consent was obtained from all patients for being included in the study.
Additional information
Ankur Dhal completed his postgraduation (M.D.) in anesthesiology from Government Medical College and Hospital, Chandigarh, India. Sukanya Mitra is a Professor in Department of Anesthesia and Intensive Care, Government Medical College and Hospital, Chandigarh, India. Richa Saroa is Associate Professor, Department of Anaesthesia and Intensive Care, Government Medical College and Hospital, Chandigarh, India. Jasveer Singh is Associate Professor, Department of Anaesthesia and Intensive Care, Government Medical College and Hospital, Chandigarh, India. Reeti Mehra is Associate Professor, Department of Obstetrics and Gynaecology, Government Medical College and Hospital, Chandigarh, India.
Rights and permissions
About this article
Cite this article
Dhal, A., Mitra, S., Saroa, R. et al. Can Epidural Dexamethasone Reduce Patient-Controlled Epidural Consumption of Fentanyl and Levobupivacaine in Laboring Women? A Double-Blind, Randomized, Placebo-Controlled Trial. J Obstet Gynecol India 69, 258–265 (2019). https://doi.org/10.1007/s13224-018-1189-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-018-1189-2