Abstract
In this paper, we propose a new approach to address the problem of designing pharmaceutical copayments. The rationale for positive copayments in our setting lies in the presence of budgetary constraints and, hence, in the need to raise funds in order to finance the costs of the treatments. We use results from the literature on axiomatic bargaining with claims to incorporate criteria of distributive justice into the design of copayments. We find that if the government constrains patient rights to what is medically feasible, equity-based copayments vary from a percentage of the cost of the treatment, to a flat rate per prescription. If the government also takes into account the burden of disease experienced by patients, then copayments based on equity lead to a relation between copayments and clinical status that diverges from those proposals based on efficiency arguments. In particular, we show that equity-based copayments might be increasing in the health gains that the treatments provide to the patients. The reason is that these copayments try to avoid a “double jeopardy” problem, by ensuring that those patients with a large burden of disease do not face also an important monetary cost.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Pharmaceutical copayments are used in almost all health systems, although there is significant variation across countries in access to prescription drug insurance. In Spain, patients under the age of 65 have to pay 40% of their drug costs, while patients over 65 years of age (pensioners) or patients disabled by industrial accidents do have to pay a lower percentage (or do not pay anything). Belgium, Denmark, France, Greece, Luxembourg, and Portugal also charge patients a percentage of the cost of the drug. In other countries, like Austria and the UK flat-rate copayments per prescription exist. Moreover, in all countries protection mechanisms may apply to particular groups of people—for instance low-income individuals, or to particular types of product—for example, essential drugs or drugs for chronic or life-threatening illnesses.Footnote 1
In a public health system, copayments serve either of two objectives, or the two combined: (a) to control unnecessary demand and (b) to raise funds for the health system. Since the seminal paper by Pauly (1968), the literature has focused on the use of copayments as an efficiency-enhancing tool. Their main objective has been to avoid over-consumption, that is, the use of medical services whose costs are larger than their benefits. However, they also play a role as a cost-containment instrument and some governments introduce copayments with the objective of making the health system financially sustainable (Donaldson and Gerard 2005).Footnote 2
In this paper, we elaborate on this second objective of copayments. Our aim is to offer some guidance on the principles that should govern copayment mechanisms if their main objective is to contribute to the financing of the health system and its budgetary sustainability.
While there is a huge literature on the use of copayments to reduce moral hazard, there are hardly any papers that have dealt with this second role of copayments from a theoretical point of view. Chernikovsky (2000) suggests that if the objective is to raise funds copayments should be placed on those treatments where elasticity of demand is low. However, this is problematic since among treatments with low elasticity of demand are those that produce the largest benefit. Increasing copayments for those treatments could, therefore, raise important equity issues. This is precisely the aim of this paper, that is, to suggest how copayments should be established in order to raise funds while preserving, at the same time, some equity principles.
As far as we are aware there is only one paper (Smith 2005) that has dealt with the issue of how equity should influence copayments if the objective is to balance the health budget. The motivation of our paper is thus similar to Smith (2005). We focus on a health system with a given benefits package that it is budgetary unfeasible to fund only through taxes. At the same time, policy makers do not consider the option of restricting the package of care provided by the health system. That is, we live in a second-best world as is the case in Smith (2005). The choice of the policy maker is, hence, to provide free access for a limited amount of health services or to provide partial funding to a larger amount of services. The main conceptual difference between this paper and Smith (2005) is in the objective of the health system. Smith (2005) assumes that it is to maximize health. He incorporates equity introducing a societal weight on health based on income, that is, the health gains for poor people receive, ceteris paribus, a higher weight than the health gains of rich people. This changes the problem of the policy maker from health maximization to a problem of maximizing a weighted health-benefits function. His copayments are directly related to the cost/benefit ratio. This result is not purely utilitarian because “the benefit of treatment is scaled in proportion to the social weight attached to the marginal patient deterred” (Smith 2005, p. 1026).
Our approach departs, we believe, more radically from the traditional utilitarian (health maximization) approach, and it is more strongly linked with philosophical equity principles such as fair innings or severity (Nord 2005). We introduce equity in the objective of the health system itself. We assume that the objective of the health system is not to maximize health (weighted or not), but to ensure that copayments charged to population preserve some basic equity principles. Given this objective, we find that copayments should be influenced by both the severity of the illness of the patient and her possibilities of recovery. These elements are not present in Smith (2005). Moreover, copayments are no longer directly proportional to the cost/benefit ratio of the medical treatment.
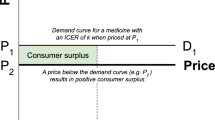
In order to avoid confusion between our approach and the more traditional perspective of copayments as an efficiency-enhancing device, we assume that health managers have enough information to determine the optimal consumption of health services for each kind of patient. Medical treatments can be provided only to those patients whose benefits outweigh costs. Under these circumstances, “optimal insurance should cover the cost of treatment in full for those with severities high enough to yield benefits greater than costs, and should not pay at all for treatment of people with lower levels of severity” (Pauly and Blavin 2008). In spite of that, we assume that the government cannot raise enough taxes to fully fund those services. The problem is how to distribute available resources in an equitable way.
In this framework, copayments are, so to speak, a residual. Since public resources are not enough to fully fund all medical services, subjects will have to provide the rest from their own pocket. Thus, depending on the amount of the budget that each patient is allocated, she will face a different copayment. Our objective is to establish some equity principles to allocate this budget and, in consequence, to determine how much each patient will have to pay to access medical treatments.
The theoretical framework that we will use is the so-called axiomatic bargaining literature.Footnote 3 This literature interprets the budget allocation problem as a bargaining process between agents and advocates for sharing solutions that fulfil a series of a priori desirable properties (axioms). Then, the model presented in this paper views the problem as a bargaining situation in which two patients (or groups of patients) have the opportunity to agree with each other on a division of the budget which satisfies them both. The game does not actually have to be played, rather we could imagine the health planner solving the resource allocation problem by treating the situation as if it were a bargaining game. The use of an axiomatic bargaining framework to solve a resource allocation problem in health care was first suggested by Clark (1995), who compared the healthcare budget allocation between two patients under four alternative rules. Later, Cuadras-Morató et al. (2001) enriched Clark’s original setting by allowing for the possibility that agents have claims about the resources they would like to receive.Footnote 4
A central element in our resource allocation problem is the aggregate need or claim. In our model, claims are measured in terms of the utility to which patients are entitled in an ideal situation with no budget constraints. This “ideal situation” depends on the reference point the health planner uses to evaluate equity. Equity is not a concept so well defined in the health literature as efficiency (see Culyer and Wagstaff 1993 for a discussion). Thus, in order to design equity-based copayments we first need to conceptualize equity, as different concepts of equity give rise to different copayments. In this respect, we use two reference points to evaluate equity that yield two scenarios for claims. In the first scenario—the constrained scenario in what follows—the health planner links the right of the patients to request a higher amount in the final sharing of resources to their health improvement given the treatment available. This interpretation of equity coincides with the definition of need “as capacity to benefit” suggested by Williams (1974). In this scenario, the claim is constrained to be the utility that patients would enjoy if they had access to the drug free of any charge. One may think, however, that if the health planner constrains patients’ rights to what is medically feasible, this limits the equity of the final sharing. Thus, we analyse a second scenario—named unconstrained scenario—where the health planner assumes that all patients have the right to enjoy a certain level of well-being based on an exogenously determined amount of health [the quality-adjusted life expectancy (QALE) at birth, for instance]. This second approach is more in line with the fair-innings theory (Williams 1997), that argues that individuals should be compensated for those circumstances beyond their control, like their type of illness or their possibilities of recovery. In this second scenario, the claim is exogenous and requires that all individuals enjoy the same level of utility irrespective of their personal circumstances or treatment possibilities. Notice that the two claim scenarios we consider may be suitable to deal with different types of diseases. In this sense, the health need approach would be appropriate to analyse situations where patients suffer from mild or common illnesses for which there exist effective treatments, while the “fair-innings” approach is more adequate for dealing with patients suffering from severe or rare illnesses with no effective treatment available.
In order to allocate resources, we consider two well-known solutions that emerge from the axiomatic bargaining literature. The first solution advocates for a sharing of resources that is proportional to what the agents would obtain in the absence of scarcity and is, therefore, labelled as the proportional solution.Footnote 5 The second alternative is to equally share the difference between what the agents would obtain if the resources were unlimited and the overall amount of available resources to share. This rule, that equally splits the overall loss among the agents, is named the equal-loss solution.Footnote 6
Our results show that copayments based on equity lead to a relation between copayments and clinical status that diverges from those proposals based on efficiency arguments. In the constrained case, only costs of treatment matter. Moreover, depending on the specific rule used to allocate resources (proportional vs equal-loss rule) copayments vary from a fixed percentage of the cost of the treatment (as copayments in Spain), to a flat rate per prescription (as it is in the UK). In the unconstrained case, we find that copayments should be increasing (rather than decreasing) in the health benefits of the treatment. Equity-based copayments, in this case, try to avoid a “double jeopardy” problem, and thus, they favour the patient who suffers a larger burden of disease through a larger subsidization.
The paper is organized as follows: Sect. 2 lays out the model and presents the rules we use in the resource allocation problem. Section 3 computes the copayments in the constrained and unconstrained scenarios. Section 4 studies the incentives that our equity-based copayments provide to patients. Section 5 introduces income considerations in the model. Finally, Sect. 6 concludes. All of the proofs are in “Appendix A”.
2 The model
2.1 The basic framework
There are two patients (or, alternatively, groups of patients), \(i=\left\{ 1,2\right\} ,\) who are in need of a pharmaceutical treatment to recover from a certain health loss.Footnote 7 Each patient i has an initial health status \(s_{i}.\) We measure health status in monetary terms. (\(s_{i}\) could be interpreted as a monetization of QALYs, for instance.)
Patients have access to drugs that can improve their health status. Each patient has been prescribed a particular drug, and hence, it is not at the patients’ discretion to choose their preferred pharmaceutical.Footnote 8 For patient i, the consumption of drug i can provide him with an extra \(h_{i}\) QALYs (measured in monetary terms). Hence, \(h_{i}\) is a measure of the effectiveness of the treatment for illness i.Footnote 9
The treatment needed by patient i has a total cost \(c_{i}\), and the patient faces a copayment rate of \(\alpha _{i}\in \left[ 0,1\right] .\)Footnote 10 Thus, we can define the utility of agent i (in monetary terms) as:
For simplicity, we abstract from any income effect, i.e. we do not include the income of the patients as a determinant of the copayment levels they will face.Footnote 11 Moreover, we assume that all treatments have a positive net benefit (i.e. \(\beta _{i}\equiv h_{i}-c_{i}>0,\) for every i), so that there is no need to analyse the decision of whether a drug should be eligible for subsidization or not.
In order to address different equity principles behind the objectives of the health planner, we consider two different situations regarding the rights or claims that the health planner assigns to patients. Notice that these rights are measured in terms of the utility that patients should enjoy in an ideal situation with no budget constraints. In the first scenario—the constrained scenario—the claim is constrained to be the utility the agents would enjoy if they had access to the drug free of any charge, i.e. \( s_{i}+h_{i}.\) This alternative links the right of the patients to request a higher amount in the final sharing of resources to their possibilities of recovery or health improvements. One may think that these claims are reasonable when patients suffer from mild or common illnesses for which there exist effective treatments. In the second scenario—the unconstrained—the health planner assumes that all patients should be entitled to a certain level of well-being based on an exogenously determined amount of health (the quality-adjusted life expectancy at birth, for instance). In this case, the claim is exogenously given by e. Given the claim e and the treatment possibilities, we define \(\lambda _{i}\equiv e-\left( s_{i}+h_{i}\right) \ge 0\), that can be conceptualized as the burden of disease after treatment (ex post burden of disease) or, simply, as burden of disease.Footnote 12 This scenario is more appropriate when patients experience severe diseases for which no effective treatment is available.
The health authority (HA) is responsible for paying all the costs of the treatments not levied through the copayments. The total budget to be allocated to drug financing is B. Thus, the budget constraint faced by the HA is given by:
To make the analysis non-trivial, we assume that it is impossible to simultaneously fully subsidize both patients. FormallyFootnote 13:
2.2 The resource allocation problem
The impossibility to fully subsidize both patients generates a resource allocation problem with claims.
The feasibility set is determined by the vectors of copayment rates that are simultaneously “affordable” for the health authority. As in any other allocation problem in the presence of scarcity, there are four key elements that need to be identified: (1) the budget constraint, (2) the disagreement point, (3) the claims point, and (4) the resource allocation rule to be used.
The budget constraint of the allocation problem relates the subsidies that can be awarded to each patient with the amount of resources available to distribute. From (1), we get:
Substituting the equation above into (2), rearranging terms and binding the budget constraint, we get
We also need to define the “disagreement” point of the problem. Formally, this is the vector of utility levels that the agents would obtain in case there is no distribution of the resources. In our setting, it corresponds to the value of the patients’ utility in the absence of any subsidization of the drugs, i.e. \(U_{i}\left( \alpha _{i}=1\right) =s_{i}+h_{i}-c_{i}\).
As already mentioned, we consider two reference points to evaluate equity which implies that the claims to adjudicate are different in both scenarios. In the constrained scenario, patients have the right to receive medical treatment free of any charge. Formally, their claims are \(U_{i}^{\varepsilon _{i}}=s_{i}+h_{i}\), where the index \(\varepsilon _{i}\) denotes the portion of the budget that each patient should receive to satisfy her claim. In the constrained scenario, this portion would correspond to the cost of her medical treatment, \(\varepsilon _{i}=c_{i}.\) In the second scenario, the health planner adopts a different reference point and requires that all individuals enjoy the same level of well-being irrespective of their personal circumstances or treatment possibilities. In this case, the patient’s claim would be \(U_{i}^{\varepsilon _{i}}=e.\) Notice that in this scenario the portion of the budget that each patient should receive does not only incorporate the cost of treatment but also a compensation for her experienced burden of disease. Formally, \(\varepsilon _{i}=c_{i}+\lambda _{i}.\)
Finally, regarding the resource allocation rule to be used, we focus on two solution concepts that have been widely used in claim problems (see Chun and Thomson 1992; Bossert 1993; Marco 1994 for a complete characterization). The first rule we use to allocate the budget is the proportional rule. Under this rule, the available budget is distributed in such a way that is proportional to what the agents would obtain in the absence of scarcity, i.e. the rule distributes awards proportionally to claims. Formally, this solution corresponds to the maximal point inside the feasible set in the segment connecting the disagreement point with the claim point. More precisely, the proportional solution is given by the utility levels \(\left( U_{1}^{P},U_{2}^{P}\right) \) that simultaneously satisfy:
We also consider the equal-loss rule that splits equally the difference between what the agents would obtain in the absence of scarcity, i.e. the aggregate claim, and the overall amount of resources available B. In other words, this solution implies an equal-sharing of the aggregate loss, subject to the condition that no one ends up with a negative award. Formally, it allocates resources in such a way that the agents end up at the same “distance” from their ideal utility point. The idea is that every patient should receive the same amount of the budget as long as this does not exceed the claim. If the claims of the patients are equal, then this solution equalizes the awards across patients. More precisely, the equal-loss solution is given by the utility levels \(\left( U_{1}^{E},U_{2}^{E}\right) \) that simultaneously satisfy:
Finally, for the two solutions, we also impose the restriction that the copayment has to be smaller than or equal to 1. Formally, for every \(i\in \left\{ 1,2\right\} ,\) and \(k\in \left\{ P,E\right\} \)
The two solutions proposed satisfy some basic properties (see Chun and Thomson 1992; Bossert 1993). Most of them are just slight reformulations of the corresponding properties for bargaining problems without claims. While the second property has a clear ethical content, the remaining five can be regarded as procedural requirements. These properties are: (1) Weak Pareto optimality: There is no feasible alternative solution that is strictly preferred by all agents to the solution outcome; (2) Symmetry: Agents with equal characteristics should be treated equally; (3) Boundedness: No agent is worse off at the solution outcome than at the disagreement point (a condition which is often considered in bargaining theory under the name of “individual rationality”), and no agent is better off at the solution outcome than at the claims point; (4) Continuity: A small change in the problem never cause a large change in the solution outcome; (5) Strong Monotonicity: If the feasible set (i.e. the budget to be shared) expands, other things being equal, all agents should be better off; and (6) Translation invariance: the solution proposed is not affected by a change in the units in which the variables of the problem are defined.
The two solutions, however, differ in the role they give to the disagreement point (the utility of the agents in the absence of any subsidization in our model).Footnote 14 In the proportional solution, this utility level is crucial, as the final allocation will be proportional to the difference between the claim of the agent and his disagreement point. The equal-loss solution, on the contrary, is independent on the disagreement point. As highlighted by Bossert (1993), this property might be plausible in situations where parties bargain in good faith and the arbitrator believes claims are reasonable and justified. Therefore, in such cases recommendation should be based entirely on the claims. Then, in the equal-loss solution the disagreement point only sets a minimum reservation utility that is secured for all agents but, other than that, it plays no role on the allocation of resources.
The following section computes the copayment under these two different rules to allocate the budget.Footnote 15 Notice that the bargaining problem with claims we face could also be formulated as a bankruptcy problem involving the allocation of a given amount of a single (perfectly divisible) good B among a group of agents, when this amount is insufficient to satisfy all their demands (\(\varepsilon _{1}+\varepsilon _{2}\)).Footnote 16
3 Equity-oriented pharmaceutical copayments
3.1 Proportional versus equal-loss rule
In this section, we compute copayments under the two rules to distribute the budget described above. First, the proportional rule that distributes resources proportionally to claims. In the proportional solution, the sharing of the budget has to satisfy the restrictions in Eq. (5). Second, the equal-losses rule that makes losses as equal as possible, subject to the condition that no patient ends up with a negative award. In the equal-loss solution, the sharing of the budget has to satisfy the restrictions in Eq. (5).
In any of the two rules, we also have to take into account the restriction given by (7) in order to ensure that the resulting copayment is well defined (i.e. are smaller than or equal to 1). In case (7) is violated for one patient, then the solution is obtained by binding the restriction for this patient and allocating the remaining budget to the other.
Assume, without loss of generality, that \(\varepsilon _{1}<\varepsilon _{2}.\) It is straightforward to obtain that:
Lemma 1
The utilities awarded to each patient \(i\in \left\{ 1,2\right\} \) are given by :
Under the proportional rule
$$\begin{aligned} U_{i}^{P}=s_{i}+h_{i}-c_{i}+\frac{\varepsilon _{1}}{\varepsilon _{1}+\varepsilon _{2}}B. \end{aligned}$$Under the equal-loss rule
- (i)
If \(\varepsilon _{1}\ge \varepsilon _{2}-B,\) then :
$$\begin{aligned} U_{i}^{E}=s_{i}+h_{i}-\frac{\left( \varepsilon _{1}+\varepsilon _{2}-B\right) }{2}. \end{aligned}$$ - (ii)
If \(\varepsilon _{1}<\varepsilon _{2}-B,\) then :
$$\begin{aligned} U_{1}^{E}= & {} s_{1}+h_{1}-c_{1} \\ U_{2}^{E}= & {} s_{2}+h_{2}-c_{2}+B. \end{aligned}$$
- (i)
Note that the equal-loss solution is divided into two different regions depending on whether when equalizing across patients the losses in utility relative to their claim point, patient 1 ends up being worse off than at her initial (unsubsidized) utility, or not. If this happens, the solution leaves this patient fully unsubsidized and allocates the whole budget to the other patient. This possibility that one patient remains totally unsubsidized does not appear under the proportional rule. Once the utilities are computed, and using the fact that from (1) we have that
it is straightforward to obtain that:
Proposition 1
The copayment charged to each patient \(i=\left\{ 1,2\right\} \) is given by :
Under the proportional rule
$$\begin{aligned} \alpha _{i}^{P}=1-\frac{\varepsilon _{i}}{\left( \varepsilon _{1}+\varepsilon _{2}\right) c_{i}}B. \end{aligned}$$Under the equal-loss rule
- (i)
If \(\varepsilon _{1}\ge \varepsilon _{2}-B,\) then :
$$\begin{aligned} \alpha _{i}^{E}=\frac{\left( \varepsilon _{1}+\varepsilon _{2}-B\right) }{ 2c_{i}}. \end{aligned}$$ - (ii)
If \(\varepsilon _{1}<\varepsilon _{2}-B,\) then :
$$\begin{aligned} \alpha _{1}^{E}= & {} 1 \\ \alpha _{2}^{E}= & {} 1-\frac{B}{c_{2}} \end{aligned}$$
- (i)
Note first that under the proportional rule, patients are never charged the whole price of the drug (i.e. \(\alpha _{i}^{P}<1\) for every i), and hence, both patients are always subsidized. Thus, even if the proportional criterion favours one patient over the other, this prioritization is never absolute. Under the equal-loss criterion, on the contrary, it can be the case that one patient has to bear the full cost of the drug. In other words, when the prioritization is based on an equal-loss argument, it may give an absolute priority to finance one illness and hence lead to the exclusion of the other. This occurs if one treatment is very cheap relative to the other one.
In order to provide further insights about the characteristics of the copayments, we need to analyse the two scenarios for claims separately.
3.2 Constrained claims
Remember that in the constrained scenario patients should receive \( \varepsilon _{i}=c_{i}\) from the budget in order to satisfy their claims. Thus, according to Proposition 1 the copayment under the proportional rule becomes \(\alpha _{i}^{P}=1-\frac{B}{\left( c_{1}+c_{2}\right) },\) while the equity-loss rule yields a copayment \(\alpha _{i}^{E}=\frac{\left( c_{1}+c_{2}-B\right) }{2c_{i}}\) when both patients are subsidized.
Several insights emerge comparing both rules. First, the proportional copayment depends only on the overall shortage of resources. The copayment rate does not differ across patients depending on the relative costs of their drugs or their health states. It is, therefore, an homogeneous system in which all patients pay the same percentage of the cost of the drug. Secondly, the equal-loss copayment is inversely related to the cost of the treatment: If drug i is more costly than drug j, the percentage of the cost paid by patient i is smaller than the one paid by patient j, in such a way that the total expenditures made on the drugs (\(\alpha _{i}c_{i}\)) are equal for the two patients. Formally,
This, in fact, can be seen as a copayment system where all drugs face a constant total copayment. Since the copayment is fixed in absolute terms, it can be reinterpreted as being a decreasing proportion of the total cost of the drug.
It is also interesting to highlight that under both prioritization rules the resulting copayments are independent from the health benefits that the treatments can provide. This illustrates the difference between our approach for the design of copayments and an utilitarian approach where the health authority aims at maximizing the overall health of the population. From an utilitarian perspective, priority should be given to those patients with the highest potential benefits from treatment as they are the ones that contribute most to the overall health (see Smith 2005). The equity-based approach we propose here takes a different view. Thus, despite the government takes into account health benefits in the sharing problem, both sharing rules recommend copayments not to discriminate against low-benefit patients. As a result, copayments are independent from the effectiveness of the treatment.
Finally, some comparative statics allow us to study how the two rules compare in terms of the way they handle the costs of the treatments. First of all, it is worth recalling that an increase in the cost of a drug implies that, given a fixed budget B, the overall subsidizing possibilities of the health planner are diminished, and therefore, a larger share of the costs has to be charged to the patients. We find that under the proportional rule both \(\frac{\partial \alpha _{i}^{P}}{\partial c_{i}}\) and \(\frac{\partial \alpha _{j}^{P}}{\partial c_{i}}\) are positive. As the objective is to keep the relative position of the patients unchanged, an increase in the cost of a drug increases the copayment charged to all patients, in such a way that the proportionality is preserved. The equal-loss criterion takes a different approach. What matters now is the fact that the higher the cost of one patient’s drug, the less utility she will have relative to her ideal point and therefore the larger subsidization she should receive in order to compensate. This increased egalitarianism of the equal-loss rule, relative to the proportional one, causes that, as a result of the increase in the price of drug i, the copayment charged to patient i decreases and it is patient j, whose drug’s price has not changed, who is charged with a larger copayment rate.Footnote 17
3.3 Unconstrained claims
In the unconstrained scenario, the health planner takes into account the burden of disease experienced by patients, and thus, patients should receive \(\varepsilon _{i}=c_{i}+\lambda _{i}\) from the budget in order to satisfy their claims.
It is straightforward from Proposition 1 that the copayment charged to each patient \(i,j\in \left\{ 1,2\right\} \) with \(i\ne j\) becomes \(\alpha _{i}^{P}=1-\frac{\lambda _{i}+c_{i}}{c_{i}\left( \lambda _{1}+c_{1}+\lambda _{2}+c_{2}\right) }B\) under the proportional criterion, while the equal-loss rule yields a copayment \(\alpha _{i}^{E}=\frac{\left( c_{1}+c_{2}-B\right) +\left( \lambda _{j}-\lambda _{i}\right) }{2c_{i}}\) when both patients are subsidized (i.e. when \(\lambda _{1}+c_{1}\ge \lambda _{2}+c_{2}-B).\)
Note first that, as in the constrained case, only the equal-loss rule may leave some patients unsubsidized. The only difference is that before, the prioritization was solely based on the treatment costs, while in this scenario the sum of both the monetary cost (c) and the health cost (\( \lambda \)) are the basis for the prioritization. As a result, if one patient has a very low value of \(\lambda +c\), then she may have to bear the full cost of the treatment.
Secondly, when both treatments are (at least partially) subsidized, the resulting copayments with unconstrained claims also depart from those that would be recommended under an utilitarian approach. This time, the burden of disease plays a prominent role. The higher the burden of disease, the lower the copayment.Footnote 18\(^{,}\)Footnote 19 Given the definition of burden of disease, the lower the health without treatment (i.e. the higher the severity) the lower the copayment, and the lower the health gain, the lower the copayment. This can be interpreted, in fact, as a fair-innings effect: If the patient is “unlucky”, that is, if she is severely ill and the treatment is not very effective she should not be penalized paying a high proportion of the treatment costs. Copayments with unconstrained claims try to avoid, thus, a double jeopardy situation by favouring the patient who has a worse health-recovery possibility through a larger subsidization.Footnote 20 What equity requires (of course, as we defined it) is that those patients who face larger losses (monetary and health) should receive a larger share of the budget.
3.4 Discussion
In this section, we provide a brief discussion of how the constrained and the unconstrained scenarios compare. Associating these two claim scenarios with different types of diseases also allows us to offer some policy recommendations. Moreover, we also contrast our results with those offered by the more traditional perspective of copayments as an efficiency-enhancing device.
As we have seen, the main difference between the two scenarios is the role that severity and patients’ health gains play in the design of the copayments. When patients’ rights are based on what is medically feasible, equity-based copayments do not depend neither on the severity of the patient nor on his possibilities of recovery. The only thing that matters is the cost of the treatment. On the contrary, if the government assigns an exogenous level of well-being to all patients the burden of disease plays a prominent role. Notice that although the two operationalizations of equity will lead to different relationships between costs and copayments, all solutions imply more resources should be allocated to those patients facing higher costs. This could imply that cheap treatments might charge the full cost. In addition to this, since equity-based copayments in the unconstrained scenario are increasing in the health benefits that treatments provide to patients, the agent who has a worse health-recovery possibility is favoured through a larger subsidization.
One may also wonder how medical innovation could affect the design of our copayments. Assume that governments decide to devote more resources to pursue research on the developing of new drugs. According to our results, in the constrained case, medical innovations that yield better health gains do not have any effect on the copayments, unless the innovation involves a variation in costs. In the unconstrained scenario, on the contrary, medical innovations that improve the possibilities of recovery do have an effect. In particular, those patients that profit from the innovation and enjoy better health-recovery possibilities should contribute more to the financing of their drug.
If we agree that claims in the constrained scenario are reasonable when patients experience mild or common illnesses for which there exist effective available treatments, and claims in the unconstrained scenario are reasonable for rare or severe diseases for which no effective treatment is available, then different policy recommendations could be extracted from our analysis. First, for common illnesses it seems appropriate to use copayments similar to those existing in Europe (which vary from a percentage of the cost of the treatment to a flat rate per prescription). For this kind of illnesses, neither the sanitary characteristics of the patients nor the effectiveness of the treatments is relevant in determining the copayment. On the contrary, for rare diseases our results advocate introducing copayments increasing in the health gains that the treatments provide to the patients. Thus, governments should grant preferential treatment to those patients suffering from severe or rare diseases. In Spain, for example, the Spanish Federation of Rare Diseases (FEDER) has been fighting since 16/2012 Act was published for the exemption of the copayment for all those affected by some type of rare pathology (Diario Médico 2013).
Finally, it might seem that equity arguments lead to a relation between copayments and clinical status that diverges from those proposals based on efficiency arguments. The efficiency approach suggests that more cost-effective medications should have lower associated copayments to induce patients to consume these and not others existing to treat the same pathology but with a lower level of cost-effectiveness. However, we believe that the conclusions of the equity and efficiency approaches could be considered, in fact, complementary. There are certain illnesses with a wide variety of treatments available, with different degrees of cost-effectiveness, and with some discretion by the patient (or the doctor) in their choice. In these cases, criteria based on efficiency that prioritize the most cost-effective medications by associating them with lower copayments may be appropriate to discipline consumption. For other types of situations in which patients do not enjoy discretion in the choice of treatment, the efficiency arguments would lose weight in favour of others aimed at guaranteeing fairness in the distribution of public budget. In these cases, reasonable copayments would arise in line with those found in this work that try to avoid, above all, that patients with a significant unrecoverable loss of health also suffer a substantial monetary penalty.
4 Efficiency considerations
As we have said in Introduction, in this paper we explicitly depart from the usual efficiency-enhancing role assigned to pharmaceutical copayments as we have not aimed at designing copayments that rationalize consumption or influence patients’ choice among different treatment possibilities. However, at this point, we can easily assess how the copayments under both the proportional and the equal-loss rules provide incentives to patients to choose among drugs.
Consider that, instead of having two patients, each one with her prescribed medicine and with no possibility to substitute among drugs, we face a single patient who has the capacity to choose among drugs 1 and 2, both of them being alternative treatments. In such a setting, the incentive role of copayments becomes relevant. We would like copayment schemes that induce the patient to make the “right” choice, i.e. that make patients decide to buy the drug with the highest cost-effectiveness ratio or net benefit. Note that, as the copayments with constrained claims do not depend on the health benefits of the patient—but only on costs—we restrict the efficiency analysis to the unconstrained scenario.
If we compare the net utility of a patient when purchasing either of the two drugs, we can conclude thatFootnote 21:
Proposition 2
With unconstrained claims, the proportional criterion generates a copayment scheme that provides the patient with incentives to purchase the drug with the highest net benefit, while the equal-loss criterion does not.
Proof
See “Appendix A.1”. \(\square \)
We find that only proportional copayments are compatible with providing the patient with the right incentives. The main reason for this result lies in the higher egalitarianism of the equal-loss rule. As the rule downgrades the impact of the price of the drug on the value of the copayment, the agent does not fully internalize the cost dimension in her decision. This is detrimental to the provision of incentives as, other things been equal, the agent is not induced to purchase the less costly drug.
5 Income effects
In this section, we illustrate how the introduction of income considerations does not alter the main insights that can be extracted from our analysis. For this purpose, assume that agents are endowed with a simple utility function that is not additively separable in health (\(\eta _{i}\)) and income (\(I_{i}\)) of the form \(U_{i}\left( \eta _{i},I_{i}\right) =\eta _{i}I_{i}.\)Footnote 22 Since the utility function is not quasilinear in money, income effects will be present. For this exercise, let us focus again on the case with unconstrained claims and, therefore, assume the claim assigned to patient i is given by e (which implies that the portion of the budget that should be assigned to patient i is \(c_{i}+\lambda _{i}).\) For the constrained case, the analysis would be analogous and so would be the conclusions.
Taking into account that the net income of an agent is the difference between her initial wealth (measured by \(m_{i}\)) and the cost of the treatment (\(\alpha _{i}c_{i}\)), we have that:
This allows us to write the budget constraint faced by the health authority as:
with \(\eta _{i}=s_{i}+h_{i}\) being the health of agent i after treatment.
This restatement of the budget constraint allows us to recompute the copayments under the two rules under consideration:
Proposition 3
When the utility of the agents is of the form \( U_{i}\left( \eta _{i},I_{i}\right) =\eta _{i}I_{i},\) the copayments charged to each patient \((i=1,2)\) with unconstrained claims are given by :
Under the proportional criterion,
$$\begin{aligned} \tilde{\alpha }_{i}^{P}=1-\frac{\left( \lambda _{i}+c_{i}\eta _{i}\right) \eta _{j}}{c_{i}\left( \eta _{2}\left( \lambda _{1}+c_{1}\eta _{1}\right) +\eta _{1}\left( \lambda _{2}+c_{2}\eta _{2}\right) \right) }B. \end{aligned}$$Under the equal-loss criterion,
- (i)
If for every \(i=1,2,\) with \(j\ne i,\) it holds that \(c_{i}\eta _{i}+\lambda _{i}\ge c_{j}\eta _{j}+\lambda _{j}-B\eta _{j},\) then
$$\begin{aligned} \tilde{\alpha }_{i}^{E}=\frac{\left( c_{1}+c_{2}-B\right) \eta _{1}+\left( \lambda _{j}-\lambda _{i}\right) }{c_{i}\left( \eta _{1}+\eta _{2}\right) }. \end{aligned}$$ - (ii)
If there exists \(i=1,2,\) with \(j\ne i,\) such that \(c_{i}\eta _{i}+\lambda _{i}<c_{j}\eta _{j}+\lambda _{j}-B\eta _{j},\) then
$$\begin{aligned} \tilde{\alpha }_{i}^{E}= & {} 1 \\ \tilde{\alpha }_{j}^{E}= & {} 1-\frac{B}{c_{j}}. \end{aligned}$$
- (i)
Proof
See “Appendix A.2”. \(\square \)
We can see how despite the introduction of income effects altering the shape of the copayment rates, they preserve the main insight of the analysis: the larger the value of the unrecoverable utility loss the agent will face, the smaller the copayment. Note that, in this case, the value of \(\lambda =e-\eta _{i}m_{i}\) captures two effects. First, there is the fair-innings effect by which an agent with a larger burden of disease should be prioritized in order to avoid a double jeopardy. Second, with income effects, the initial wealth of the agent also plays a role. The poorer the patient (i.e. the lower \(m_{i}\)), the smaller should also be the value of the copayment she is charged.
6 Conclusions
In this paper, we have proposed a new way to address the problem of designing pharmaceutical copayments. We have departed from the traditional “efficiency-enhancing” argument assuming an environment where moral hazard problems are absent. The rationale for positive copayments in our setting lies in the presence of budgetary constraints and, hence, in the need to raise funds in order to finance the costs of the treatments.
This new perspective brings about new insights in the design of copayments. When the objective of copayments is to preserve equity, we have shown that:
- 1.
The structure of copayments depends on the way we operationalize equity. Different concepts of equity give rise to different copayment systems. This is important since equity is not a concept so well defined as efficiency, and it is not enough to talk about “equity-adjusted” copayments without specifying how equity is conceptualized. In that respect, we have shown that equity-based copayments depend on the reference point that it is used to evaluate equity (constrained or unconstrained) and on the rule used to allocate resources (proportional rule vs equal-loss rule).
- 2.
Equity arguments lead to a relation between copayments and clinical status that diverges from those proposals based on efficiency arguments. In the constrained case, patients’ health gains play no role. In the unconstrained case, equity-based copayments should be increasing rather than decreasing in the health benefits that the treatments provide to the patients. The main reason is that a low health benefit implies that the patient has an important permanent health loss that cannot be avoided with the medication. The allocation rules try to avoid a double jeopardy problem where on top of the health loss, the patient also faces a substantial monetary cost. As a result, the agent who has a worse health-recovery possibility is favoured through a larger subsidization.
- 3.
Severity is also important. The higher the severity, the lower the copayment. Again, the objective of this is to avoid a double penalty for the patient. Severity does not play any role if the only objective of copayments is to reduce moral hazard.
- 4.
In relation to costs of treatments, different operationalizations of equity will lead to different relationships between costs and copayments. However, all solutions imply more resources should be allocated to those patients facing higher costs. This could imply that cheap treatments might charge the full cost (100% copayment).
In summary, when we use a framework based on equity principles in order to establish copayments, we observe that: (1) new elements (like severity) have to be taken into consideration, and (2) other elements (e.g. health gains) play a different role than they play when the objective is to reduce moral hazard.
Governments have tried to preserve equity elements when they have introduced/increased copayments. But they have mainly focused on income. For example, they have established different copayments for different income groups, or they had set limits to the total financial burden derived from cost-sharing. Our paper shows that equity may require more than that. In particular, it might require incorporation of the effect of severity and compensation (or, at least, not penalization) of those with a limited capacity to benefit either because their medical condition limits the effect of a medical treatment or because the medical treatment itself is not very effective. A patient in a severe condition with a limited capacity to benefit should not be penalized with a higher copayment.
Finally, although our paper shows that there might be a conflict between efficiency and equity in the design of copayments, it does not imply that there has to be always a conflict. For example, our paper suggests that copayments should be higher for low-cost treatments and treatments for mild conditions. One could think in cases where these two features can be correlated with a high elasticity of demand and/or high cost/benefit ratio. In these cases, efficiency and equity may both justify the same structure of copayments. However, as we move towards higher severity and higher costs, both perspectives may conflict. In this case, it is clearly a matter for health authorities to decide.
The spirit of this work is eminently positive. We have identified equity-based copayments using the axiomatic bargaining framework to solve a resource allocation problem in health care. The structure of copayments depends on the reference point that it is used to evaluate equity and the allocation rule we use. There is no consensus in the literature on how governments should conceptualized equity (health need or fair-innings approaches). However, if we accept that the health need approach is suitable for analysing common and mild diseases, and the fair-innings approach is valid for severe or rare illnesses, we can extract some policy recommendations from our results. While for common illnesses, standard copayments in Europe (which vary from a percentage of the cost of the treatment to a flat rate per prescription) seem to be appropriate to guarantee equity, governments should grant preferential treatment to those patient suffering from rare diseases. Regarding the allocation rules, there is no compelling theoretical argument that has been found to select a unique optimal solution to adjudicate conflicting claims, and theory (and practice) appeals to one or another depending on the economic context at stake.Footnote 23 Thus, regulation of access to prescription drug insurance is obviously a political decision. Still we hope this study can inform the debates on health policy and contribute to the development of a better policy making process.
Notes
There is in fact a debate about the effectiveness of copayments in order to facilitate the sustainability of the health system (see, for instance, Baicker and Goldman 2011). There is some evidence that copayments may generate an increase in the total costs of the system (see, for instance, Chandra et al. 2010), since savings in some areas (e.g. pharmaceutical products) could be offset by an increase in expenditures in some other areas (e.g. hospital care).
This analysis is based on the literature on axiomatic bargaining with claims pioneered by Chun and Thomson (1992).
Historically, this has been advocated as a reasonable criterion of distributive justice since Aristotle’s Maxim (“Equals should be treated equally, and unequal, unequally in proportion to relevant similarities and differences”). For a formal analysis of this solution, see Chun and Thomson (1992).
We restrict ourselves to the case with only two groups of patients to simplify the exposition. The analysis of the general case is available in “Appendix B”. The main features of our equity-based copayments are preserved in this more general set-up.
We are implicitly assuming that the insurer has enough information to implement this policy.
Note that \(s_{i}\) can also be interpreted as an inverse measure of the severity of the patient. The larger the patient’s initial health status, the lower her severity.
Note that \(c_{i}\) does not measure the cost of a single dose of the drug, but that of the whole duration of the treatment. Therefore, copayments are defined over the total expenditures that the patient makes during the treatment.
The abstraction from income effects is inessential for our main insights but eases the exposition. See Sect. 5 for a version of the model that incorporates this feature.
The traditional concept of burden of disease, defined by the World Health Organization, would correspond in our model to \(e-s_{i}.\)
As we will see later, this assumption directly implies that the portion of the budget that patients should receive to satisfy their claims is larger than the available resources B.
Note that the proportional solution does not satisfy the axiom of independence of unclaimed alternatives (see Chun and Thomson 1992) while the equal-loss solution does satisfy it.
To ease the exposition, we consider a simplified environment where the budget constraint is so tight that it prevents from fully subsidizing any patient. Formally, this amounts to assuming that \(B<\min \{c_{1},c_{2}\}.\) This assumption clarifies the presentation of the results without eliminating any valuable insight.
See Herrero and Villar (2001) for a comparative analysis of some classical solutions to bankruptcy problems from an axiomatic viewpoint.
It is straightforward to check that \(\frac{\partial \alpha ^{E}}{\partial c_{i}}<0,\) while \(\frac{\partial \alpha _{j}^{E}}{\partial c_{i}}>0.\)
It is straightforward to see that \(\frac{\partial \alpha _{i}^{P}}{\partial \lambda _{i}}\) and \(\frac{\partial \alpha _{i}^{E}}{\partial \lambda _{i}}\) are negative.
Note that in the limit case where the burden of disease is extremely high it could be the case that patients do not have to copay but have the right to receive some monetary compensation.
Notice that this does not imply that the government should prioritize ineffective treatments for all severely ill patients. We stated in Introduction that we assume that all treatments passed the cost/benefit ratio.
We are implicitly assuming that patients are fully informed, or have been fully informed by their physicians, about benefits and costs of drugs.
Note that if both \(\eta _{i}>0\) and \(I_{i}>0\) this utility function represents separable preferences (Le Breton and Sen 1999).
Cuadras-Morató et al. (2001) study the appeal of several solutions in an empirical study of healthcare expenses. Although the equal-loss solution is, on average, the most preferred solution, the authors cannot conclude that is the most preferred solution.
We focus on the unconstrained claims case, as it is the one involving the higher complexity in the resulting copayments.
Note that this feature did not appear in Sect. 3, as there we assumed that the budget was not enough to fully subsidize any of the two groups of patients.
References
Baicker K, Goldman D (2011) Patient cost-sharing and healthcare spending growth. J Econ Perspect 25(2):47–68
Bossert W (1993) An alternative solution to bargaining problems with claims. Math Soc Sci 25:205–220
Chandra A, Gruber J, McKnight R (2010) Patient cost-sharing and hospitalization offsets in the elderly. Am Econ Rev 100(1):193–213
Chun Y, Thomson W (1992) Bargaining problems with claims. Math Soc Sci 24:19–33
Chernikovsky D (2000) The public-private mix in the modern health care system–concepts, issues and policy options revisited. NBER Working Paper, 7881
Clark D (1995) Priority setting in health care: an axiomatic bargaining approach. J Health Econ 14:345–360
Cuadras-Morató X, Pinto-Prades JL, Abellán-Perpiñan JM (2001) Equity considerations in health care: the relevance of claims. Health Econ 10:187–205
Culyer AJ, Wagstaff A (1993) Equity and equality in health and health care. J Health Econ 12:431–457
Diario Médico (2013) Feder pide que las enfermedades raras queden exentas de copagos. https://www.diariomedico.com/profesion/feder-pide-enfermedades-raras-queden-exentas-copagos.html. Accessed 1 Sept 2019
Donaldson C, Gerard K (2005) Economics of health care financing: the visible hand. Palgrave MacMillan, New York
Espin J, Rovira J (2007) Analysis of differences and commonalities in pricing and reimbursement systems in Europe. European Commission, DG Enterprise and Industry, Brussels
Herrero C, Villar A (2001) The three musketeers: four classical solutions to bankruptcy problems. Math Soc Sci 42:307–328
Marco MC (1994) An alternative characterization of the extended claim-egalitarian solution. Econ Lett 45:41–46
Le Breton M, Sen A (1999) Separable preferences, strategyproofness, and decomposability. Econometrica 67(3):605–628
Nash JF (1950) The bargaining problem. Econometrica 18:155–162
Nord E (2005) Concerns for the worse off: fair innings versus severity. Soc Sci Med 60(2):257–263
Pauly MV (1968) The economics of moral hazard: comment. Am Econ Rev 58(3):531–537
Pauly MV, Blavin FE (2008) Moral hazard in insurance, value-based cost sharing, and the benefits of blissful ignorance. J Health Econ 27(6):1407–1417
Roth AE (1979) Axiomatic models of bargaining. Springer, Berlin
Smith PC (2005) User charges and priority setting in health care: balancing equity and efficiency. J Health Econ 24:1018–1029
Williams A (1974) Need as a demand concept (with special reference to health). In: Culyer AJ (ed) Economic policies and social goals. Martin Robertson, London, pp 11–38
Williams A (1997) Intergenerational equity: an exploration of the ‘fair innings’ argument. Health Econ 6:117–132
World Health Organization (2018) Medicines reimbursement policies in Europe. http://www.euro.who.int/en/publications/abstracts/medicines-reimbursement-policies-in-europe. Accessed 1 Sept 2019
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she has no conflict of interest.
Ethical approval
This article does not contain any studies with human or animal participants performed by any of the authors.
Informed consent
This article does not contain any information that requires informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
I am especially indebted to Jose Luis Pinto-Prades and Nicolás Porteiro for their contribution on earlier versions of the paper. I am also very grateful to Carmen Herrero, Juan D. Moreno-Ternero and David Pé rez-Castrillo for their careful reading of the paper. The comments by the Associate Editor and two anonymous referees substantially improved the paper. This work has been partially funded by Projects: ECO2012-36480 and ECO2015-65408-R (Spanish Ministry of Science and Innovation and FEDER), and PAI-SEJ 479 (Junta de Andalucía). All remaining errors are my sole responsibility.
Appendices
Appendix A
1.1 Proof of Proposition 2
Consider, without loss of generality, that drug 1 has a larger net benefit than drug 2, and recall that \(\beta _{i}=h_{i}-c_{i}\) denotes the net benefit of drug i.
First of all, since it is a single patient who chooses among the two drugs, we have that \(s_{1}=s_{2}=s\).
With this simplification, we can write the net utility of the patient, under the proportional rule, when purchasing drug i as:
Since we have assumed that \(\beta _{1}>\beta _{2},\) the copayment will provide the right incentives if \(U_{1}^{P}>U_{2}^{P}.\) Rearranging the terms, we have that
Since \(\beta _{1}>\beta _{2},\) we have that \(U_{1}^{P}>U_{2}^{P}\) if and only if
Using the fact that \(\beta _{i}=h_{i}-c_{i},\) and \(\lambda _{i}=e-\left( s_{i}+h_{i}\right) \ge 0,\) the above condition is equivalent to
And this always holds since, by construction, \(B<c_{1}+c_{2}\).
We proceed analogously for the equal-loss rule. We can write the net utility of the patient when purchasing drug i as:
From here, it follows directly that \(U_{1}^{E}=U_{2}^{E}\). This completes the proof.
1.2 Proof of Proposition 3
First, the proportional solution \(\left( U_{1}^{P},U_{2}^{P}\right) \) is given by the utility levels \(\left( \tilde{U}_{1}^{P},\tilde{U} _{2}^{P}\right) \) that simultaneously satisfy:
provided they fulfil the restriction that copayments have to be smaller than or equal to 1. Formally, for every \(i\in \left\{ 1,2\right\} \)
From the first equation of the system, we get
Plugging this expression into the second equation and after some tedious but straightforward algebraic manipulations, we get:
Now, using the fact that \(\alpha _{i}=\frac{1}{c_{i}}\left( m_{i}-\frac{U_{i} }{\eta _{i}}\right) ,\) we can simplify and obtain:
It is straightforward to see that \(\tilde{\alpha }_{i}^{P}<1\) and, hence, that \(\tilde{U}_{i}^{P}\ge \eta _{i}\left( m_{i}-c_{i}\right) .\) This completes the proof.
Secondly, the equal-loss solution \(\left( U_{1}^{E},U_{2}^{E}\right) \) is given by the utility levels \(\left( \tilde{U}_{1}^{E},\tilde{U} _{2}^{E}\right) \) that simultaneously satisfy:
provided they fulfil the restriction that copayments have to be smaller than or equal to 1. Formally, for every \(i\in \left\{ 1,2\right\} \)
From the second equation of the system, we get
Plugging this expression into the first equation and after some algebraic manipulations, we get:
Now, using the fact that \(\alpha _{i}=\frac{1}{c_{i}}\left( m_{i}-\frac{U_{i} }{\eta _{i}}\right) ,\) we can simplify and obtain:
This is the solution, provided \(\tilde{\alpha }_{i}^{E}<1\) (i.e. \(\tilde{U} _{i}^{E}\ge \eta _{i}\left( m_{i}-c_{i}\right) \)). It is direct to check that
Otherwise, we have that \(\tilde{\alpha }_{i}^{E}=1\) and \(\tilde{\alpha } _{j}^{E}=1-\frac{B}{c_{j}}.\) This completes the proof.
Appendix B: Design of copayments with n patients
In this “Appendix”, we compute the complete vector of copayments in a more general environment where there are n different types of illnesses and where it may be possible to fully subsidize some (but not all) types of patients.Footnote 24 As it will become clear in what follows, the possibility that for some patients the cost of the drugs is fully subsidized makes the complete characterization of the solutions be more complex. In particular, to compute the copayment vector we need to resort to an iterative process.
Let us start, first, with the proportional criterion. First of all, order the set of patients according to \(\frac{\lambda _{i}}{c_{i}},\) in such a way that \(\frac{\lambda _{1}}{c_{1}}\le \frac{\lambda _{2}}{c_{2}}\le \cdots \le \frac{\lambda _{n}}{c_{n}}.\)
The algorithm is defined iteratively. At any iteration t, there is a set of patients \(N_{t}=\left\{ 1,2,\ldots n_{t}\right\} \) whose subsidization remains undecided, with \(n_{t}\) identifying the patient with the highest order in \( N_{t}\). The remaining budget to share is \(B_{t}.\) For the first iteration, let us define \(N_{1}=\left\{ 1,2,\ldots n\right\} ,\) i.e. the whole set of patients according to the ordering above and also let \(B_{1}=B\) (the whole budget is available to share).
The algorithm would be as follows:
At any iteration \(t\ge 1,\)
- (a)
If \(N_{t}=\left\{ n_{t}\right\} ,\) then \(\alpha _{n_{t}}^{P}=1- \frac{B_{t}}{c_{n_{t}}}\) and the algorithm stops. Otherwise, move to b)
- (b)
Split the budget \(B_{t}\) between the set of agents in \(N_{t}\) according to the Proportional criterion. This is done by finding the vector \( \tilde{\mathbf {U}}=\{ \tilde{U}_{1},\ldots \tilde{U}_{n_{t}}\}\) that solves the following system of equations:
$$\begin{aligned}&\sum _{j\in N_{t}}\tilde{U}_{j}=B_{t}+\sum _{j\in N_{t}}\left( s_{j}+h_{j}-c_{j}\right) . \\&\quad \forall i,j\in N_{t}, \frac{\tilde{U}_{i}-\left( s_{i}+h_{i}-c_{i}\right) }{\lambda _{i}+c_{i}}=\frac{\tilde{U}_{j}-\left( s_{j}+h_{j}-c_{j}\right) }{\lambda _{j}+c_{j}} \end{aligned}$$Compute the vector \(\tilde{\alpha }=\left\{ \tilde{\alpha }_{1},\tilde{\alpha } _{2},\ldots \tilde{\alpha }_{n_{t}}\right\} \) using:
$$\begin{aligned} \tilde{\alpha }_{i}=\frac{s_{i}+h_{i}-\tilde{U}_{i}}{c_{i}} \end{aligned}$$If \(\tilde{\alpha }_{n_{t}}\ge 0,\) then for every \(i\in N_{t}\)
$$\begin{aligned} \alpha _{i}^{P}=\tilde{\alpha }_{i} \end{aligned}$$and the algorithm stops. Otherwise, move to c).
- (c)
\(\alpha _{n_{t}}^{P}=0,\) and move to iteration \(t+1\) with \( B_{t+1}=B_{t}-c_{n_{t}}\) and \(N_{t+1}=N_{t}{\backslash } \left\{ n_{t}\right\} .\)
This iterative process computes the whole vector of copayments. These can have two configurations. It can be the case that all copayments are strictly positive (i.e. there is no type of agent that is fully subsidized). This occurs if no patient has a very large \(\frac{\lambda _{i}}{c_{i}},\) relative to the others. In this case, copayments for all types of patients are given by:
that is simply the n-type generalization of the copayments obtained in Sect. 3. In the other configuration, some types of patients, those with a large \(\frac{\lambda _{i}}{c_{i}},\) face a zero copayment, while for the remaining ones, the budget that is left after fully subsidizing this set of patients is split according to the rule above.
Two issues are key under the proportional rule. First, what determines whether the patient will face a positive or a zero copayment is how large is the burden of disease, relative to the cost of the treatment. The larger this health loss is, the more likely it is that the patient’s treatment is fully subsidized.Footnote 25 Secondly, analogously as in the case with two types, no patient has to face the whole cost of the treatment. The prioritization always subsidizes a fraction of the cost of the treatment.
The principles that lie behind the proportional prioritization can be better illustrated if we focus on the case where the copayment is positive and smaller than 1 for all types of patients. In this case, i.e. if \(\alpha _{j}\in \left( 0,1\right) \) for every j, if we compute the total amount of subsidy that each type of patient receives (denote it by \(\mathrm{Sub}_{j}\equiv c_{j}-\alpha _{j}c_{j}\)), we get that:
Hence, the fraction of the budget that is allocated to each type is determined by the total cost faced by these patients, i.e. not only the monetary cost (\(c_{i}\)) but also the health loss (\(\lambda _{i}\)) they incur.
Let us move now to the equal-loss criterion and order the set of patients according to \(\lambda _{i},\) in such a way that \(\lambda _{1}\le \lambda _{2}\le \cdots \le \lambda _{n}.\)
The algorithm is again defined iteratively. At any iteration t, there is a set of patients \(N_{t}\) whose subsidization remains undecided, with \(n_{t}\) identifying the patient with the highest order in \(N_{t}\). The remaining budget to share is \(B_{t}.\) Also, at each iteration define \(\alpha _{t}\) as the element in \(N_{t}\) that minimizes \(\lambda _{i}+c_{i}.\) Formally, \( \alpha _{t}=\arg \min \nolimits _{i\in N_{t}}\lambda _{i}+c_{i}.\)
For the first iteration, let us define \(N_{1}=\left\{ 1,2,\ldots n\right\} ,\) i.e. the whole set of patients according to the ordering above and also let \(B_{1}=B\). (The whole budget is available to share.)
The algorithm would be as follows:
At any iteration \(t\ge 1,\)
- (a)
If \(N_{t},\) consists of more than one type of patients, move to b). Otherwise, denote by h this remaining type of patient. We compute \( \alpha _{h}^{E}=\min \left\{ 1-\frac{B_{t}}{c_{h}},0\right\} .\) If \(\alpha _{h}^{E}>0\), the algorithm stops. Otherwise, move to the first iteration of subroutine \(a^{\prime })\).
- (b)
Split the budget \(B_{t}\) between the set of agents in \(N_{t}\) according to the equal-loss criterion. This is done by finding the vector \( \tilde{\mathbf {U}}=\{ \tilde{U}_{1},\ldots \tilde{U}_{n_{t}}\}\) that solves the following system of equations:
$$\begin{aligned} \sum _{j\in N_{t}}\tilde{U}_{j}&=B_{t}+\sum _{j\in N_{t}}\left( s_{j}+h_{j}-c_{j}\right) . \\ \forall i,j&\in N_{t}, e-\tilde{U}_{i}=e-\tilde{U}_{j}. \end{aligned}$$Compute the vector \(\tilde{\alpha }=\left\{ \tilde{\alpha }_{1},\tilde{\alpha } _{2},\ldots \tilde{\alpha }_{n_{t}}\right\} \) using:
$$\begin{aligned} \tilde{\alpha }_{i}=\frac{s_{i}+h_{i}-\tilde{U}_{i}}{c_{i}} \end{aligned}$$If \(\tilde{\alpha }_{\alpha _{t}}\le 1,\) move to c). Otherwise, \(\tilde{ \alpha }_{\alpha _{t}}^{E}=1,\) and move to iteration \(t+1\) with \( B_{t+1}=B_{t} \) and \(N_{t+1}=N_{t}{\backslash } \left\{ \alpha _{t}\right\} \).
- (c)
If \(\tilde{\alpha }_{n_{t}}\ge 0,\) then for every \(i\in N_{t},\)
$$\begin{aligned} \alpha _{i}^{E}=\tilde{\alpha }_{i}, \end{aligned}$$and the algorithm stops. Otherwise, \(\alpha _{n_{t}}^{E}=0,\) and move to iteration \(t+1\) with \(B_{t+1}=B_{t}-c_{n_{t}}\) and \(N_{t+1}=N_{t}{\backslash }\left\{ n_{t}\right\} .\)
Subroutine \(a^{\prime })\) At any iteration \(\tau \) there is a set of patients \(N_{\tau }^{\prime }\) whose subsidization can be altered with respect to what the main routine of the algorithm proposed. The remaining budget to share is \(B_{\tau }^{\prime }.\) Also, at each iteration define \( \omega _{\tau }\) as the element in \(N_{\tau }^{\prime }\) that maximizes \( \lambda _{i}+c_{i}.\) Formally, \(\omega _{\tau }=\arg \max \nolimits _{i\in N_{\tau }^{\prime }}\lambda _{i}+c_{i}.\) In the first iteration of the subroutine, we let \(N_{1}^{\prime }\) be the set of patients who, in the main routine of the algorithm, received no subsidization. Formally, \( N_{1}^{\prime }\) is such that for every \(j\in N_{1}^{\prime },\)\(\alpha _{j}^{E}=1.\) Also, we let \(B_{1}^{\prime }=B_{t}-c_{h}\).
At any iteration of the subroutine \(\tau \ge 1\):
- (i)
Take agent \(\omega _{\tau }\) and recompute its copayment according to \(\alpha _{\omega _{\tau }}^{E}=\min \left\{ 1-\frac{B_{\tau }^{\prime }}{ c_{\omega _{t}}},0\right\} .\)
- (ii)
If \(\alpha _{\omega _{\tau }}^{E}>0\), the algorithm stops. Otherwise, move to iteration \(\tau +1\) with \(N_{\tau +1}^{\prime }=N_{\tau }^{\prime }{\backslash } \left\{ \omega _{\tau }\right\} \) and \(B_{\tau +1}^{\prime }=B_{\tau }^{\prime }-c_{\omega _{\tau }}.\)
The fact that when the prioritization is based on an equal-loss argument, it may lead to the exclusion of some of the patients, complicates the computation of the optimal copayments. Now, the resulting vector of copayments might feature: (i) some patients facing a zero copayment (those with a large unrecoverable health loss, relative to the others), (ii) some patients facing a full copayment (those with a small value of \(\lambda +c\)), and (iii) the remaining ones being only partially subsidized. Copayments for these latter types of patients are given by:
Analogously as in the proportional scenario, the principles that lie behind the equal-loss prioritization can be better illustrated if we focus on the case where the copayment is positive and smaller than 1 for all types of patients. In this case, i.e. if \(\alpha _{j}\in \left( 0,1\right) \) for every j, if we compute the total amount of expenditures that each type of patient bears (denote it by \(\mathrm{Exp}_{j}\equiv \alpha _{j}c_{j}\)), we get that:
Hence, under the equal-loss criterion, the expenditures that all types of patients have to incur are the sum of: (i) an equal division of the shortage of resources relative to the total expenditure in prescriptions and (ii) a correction term that depends on the value of the unrecoverable health of each type of patient, relative to the average of the whole population. If one patient faces a larger than average permanent health loss, she pays less.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
González, P. On the design of equity-oriented pharmaceutical copayments. SERIEs 11, 179–202 (2020). https://doi.org/10.1007/s13209-019-00207-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13209-019-00207-y
Keywords
- Pharmaceutical copayments
- Budget
- Health
- Equity
- Proportional solution
- Equal-loss solution
- Axiomatic bargaining
- Claims