Abstract
The diagnosis of novel coronavirus (COVID-19) has gained the spotlight of the world’s scientific community since December 2019 and it remains an important issue due to the emergence of novel variants around the globe. Early diagnosis of coronavirus is captious to prevent and hard to control. This pandemic can be eradicated by implementing suppressing strategies which can lead to better outcomes and more lives being saved. Therefore, the analysis showed that COVID-19 can only be managed by adopting public health measures, such as testing, isolation and social distancing. Much work has been done to diagnose coronavirus. Various testing technologies have been developed, opted and modified for rapid and accurate detection. The advanced molecular diagnosis relies on the detection of SARS-CoV-2 as it has been considered the main causative agent of this pandemic. Studies have shown that several molecular tests are considered essential for the confirmation of coronavirus infection. Various serology-based tests are also used in the detection and diagnosis of coronavirus including point-of-care assays and high-throughput enzyme immunoassays that aid in the diagnosis of COVID-19. Both these assays are time-consuming and have less diagnostic accuracy. Nanotechnology has the potential to develop new strategies to combat COVID-19 by developing diagnostics and therapeutics. In this review, we have focused on the nanotechnology-based detection techniques including nanoparticles and biosensors to obstruct the spread of SARS-CoV-2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The viral pneumonia of exotic etiology, commonly recognized as a coronavirus (COVID-19), was found in Wuhan, Hubei Province, China and was broadcast to health professionals on 29 December 2019. This hallmark was affiliated with China’s largest seafood and animal market (García Reyes 2013; Yan et al. 2020). Coronavirus is the member of subfamily “Coronavirinae” (Family: coronaviridae, Order: nidovirales) that contains four genera α-coronavirus (α-CoV), β-coronavirus (β-CoV), γ-coronavirus (γ-CoV) and Δ-coronavirus (Δ-CoV). However, beta-CoV is the most important group, as this group mainly has humans as a host for pathogenic viruses including SARS-CoV-2 (2019), SARS-CoV (2002–2004) and MERS-CoV (2012–2013) (Kim et al. 2008). Several reports have found that the main origin of COVID-19 is the Chinese chrysanthemum bat because this virus has the highest sequence similarity with bat coronavirus RatG13 that was formerly recognized in horseshoe bats (belonged to the family Rhinolophidae) in Yunnan, China (Yan et al. 2020). Pangolin is considered as the intermediate host for SARS-CoV-2. Data derived from less than 1 k meta-genomic samples from the pangolin species suggest that pangolin coronavirus shows 99% sequence similarity with the current etiological agent (coronavirus) (Cortegiani et al. 2020; Zhang et al. 2020a, b).
Genetic sequence analysis possesses 79% sequence resemblance between SARS coronavirus and novel SARS-CoV-2, it also recognized two specific antigenic determinants on the SARS coronavirus S (spike) protein i.e., amino acids residues 447–458 and 789–799. Basic Local Alignment Search Tool (BLAST) analysis of SARS-CoV-2 spike protein showed approximately 75% homology with SARS-CoV (Yan et al. 2020). Hoffman et al., (Hofmann and Pöhlmann 2004) reported that both SARS-CoV and novel SARS-CoV-2 adhere to the surface of angiotensin-converting enzyme 2 (ACE2) receptor to gain entry into the host cell (Wang et al. 2020; Zhang et al. 2020a, b), it is also dependent on cellular protease TMPRSS2 for priming (Qi et al. 2020). Studies have found similarities between SARS-CoV-2 and previously reported coronavirus. Xu et al. reported that the 3-dimensional structure of S protein of both viruses has 76.5% sequence resemblance in their amino acid sequence (Zhang et al. 2020a, b). Wan et al., also reported that the glutamine residue in the SARS-CoV-2 receptor-binding domain can be identified by the critical lysine amino acid residue on the human angiotensin-converting enzyme 2 receptor. The further analysis reported that the efficiency of SARS-CoV-2 conjugated onto the surface of ACE2 receptor is higher as compared to the original SARS-CoV and it also has a greater ability for human-to-human transmission (Cortegiani et al. 2020). This novel virus can also enhance its infection rate by relying on the co-receptor and other accessory membrane proteins (Tetro 2020). Phylogenetic tree analysis of complete genome sequence confirmed that SARS-CoV-2 is dissimilar from the previous two species of coronavirus (SARS-CoV and MERS-CoV) (Qi et al. 2020). Both viruses showed an almost similar mechanism of transmission in human hosts. Similarly, a newly emerged virus is transferred to humans from the live animal market of Wuhan (Lu et al. 2020).
The genomic sequence of coronavirus (CoVs) is a positive-sense single-stranded RNA (+ ssRNA) having cap structure at 5’ and poly-A tail at 3’. A set of sub-genomic RNAs (sgRNAs) are formed from ssRNA by reverse transcription complex in a way of discontinues transcription (Chen et al. 2020). All these sub-genomic RNAs have a general leader sequence at 5’ and terminal sequence at 3’. The transcription termination and subsequent acquisition of a leader RNA occur at transcription regularity sequences (TRS), and present between the open reading frames. These sub-genomic RNAs are translated into SARS-CoV-2 proteins (V’kovski et al. 2021; Zhang et al. 2021). The genome and sub-genome of COVs have at least six (6) open reading frames (ORFs). The first ORF (ORFs1a/1b) is almost 2/3rd of the whole genomic sequence length and has the ability to encode 16 non-structural proteins (nsp-16). The first frameshift between ORF1a and ORF1b results in the formation of 2 polypeptides pp1a/b, they both help to encode the chymotrypsin like protease (3CLpro) or main protease (PLPs) into 16 non-structural proteins. Other than ORFs, one-third (1/3rd) genome of 3’ terminal encodes four structural proteins including envelope (E), nucleocapsid (N), membrane (M) and spike (S) protein (Yan and Wu 2021). Homo-trimetric S protein plays an important role in the adhesion of virus to the human surface receptor. M protein has three transmembrane domains. Many cellular proteases like furin and TMPRSS2 are helpful for the proteolytic cleavage of the spike protein at the S1/S2 site. First, the S1 subunit will ligate to the ACE2 receptor and second, the S2 subunit will show interaction with the membrane. Moreover, the spike glycoprotein will interact with another cleavage site (S2) which is present within the S2 domain, and its proteolysis will enclose the hydrophobic side chains ultimately facilitating the fusion of viral and host membranes where the viral genome will start the infection cycle. The entry of the deadly known virus SARS-CoV-2 and its infection cycle include the following diagrammatical cascade (Fig. 1). The E protein is required for the assembly, release and pathogenesis of the virus. The nucleocapsid protein has two domains and these domains are able to bind to the viral RNA genomic sequence via various mechanisms. Nucleocapsid protein can also attach to the nsp-3, it can package the genome and virons and help the interferon and viral encoded receptor of RNA interference (RNAi), which are helpful for the replication of viral activity. Besides these four main structural proteins, other coronaviruses can also encode the specialized structural and auxiliary proteins (Schoeman et al. 2020). The overall genomic size of CoV is approximately 30 kb and is considered to be the largest among all other RNA viruses, and is two times larger than the second largest RNA virus. The 3’–5’ exoribonuclease activity is exceptional only for coronaviruses and it is considered to be useful as a proofreading part of the reverse transcription complex (Romano et al. 2020).
Mechanism of SARS-CoV-2 entry in human hosts: initiation of viral entry and infection require the binding of a viral protein onto the surface of the target cell. The entry of coronavirus into the host cell is mediated by the spike glycoprotein which is composed of two units (S1 and S2). S1 is responsible for the binding of angiotensin-converting enzyme 2 (ACE2) on the host cell, whereas S2 will mediate the membrane fusion
Conventional diagnosis techniques for COVID-19
Diagnosis of viral antigens has always been challenging for the entire world. RNA viruses accumulate variations in their genomes, their rate of mutation is much higher as compared to DNA viruses which result in the formulation of false-negative results. SARS-CoV-2 is hard to detect, as their symptoms are similar to many other pathogenic agents like para-influenza viruses, respiratory syncytial viruses. Testing has become the most important factor to ensure the healthcare demand. A lot of research work has been done to devise the diagnostics for coronavirus. Several detection strategies are available to detect different strains of coronavirus. The most accurate technique for the detection of this etiological agent is RT-PCR as it is cost-effective and completely reliable but it has notable limitations (1) the sample collection may not be tolerated by the patients, commonly by children and elderly patients, (2) some of the RT-PCR tests showed larger sensitivity issues (3) high operational cost of RT-PCR. Several serological-based techniques are being introduced for the detection of COVID-19. Some point-of-care (POC) tests are also being opted for monitoring the SARS-CoV-2 infection. But these assays are less preferable over the newly developed nano-based detection methods because of certain limitations including greater procedural work, cost-ineffectiveness and larger sensitivity issues.
Detection of COVID-19 by nanoparticles
Gold nanoparticles
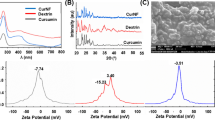
Nanoparticles (NPs) have the potential to diagnose coronavirus in the human genome with good accuracy. Serological detections are preferable over the molecular-based detection because of its cost-effectiveness and less procedural time. Gold nanoparticle-based point-of-care (POC) devices are highly efficient to recognize IgG, IgM and IgA antibody responses in human hosts against coronavirus structural proteins named spike 1 and 2 along with nucleocapsid N protein (Huang et al. 2020; Shaw et al. 2020). To diagnose the coronavirus genome, gold nanoparticles showed special characteristics like less sample consumption, more stability and biocompatibility, low cost of test, no use of expensive instruments and fast reaction rate (Ranjan et al. 2021). In this novel technology, antibody arrays coupled with gold nanoparticles (AuNP) were used which have the tendency to find out antigenic proteins in nasal swab samples (Fig. 2) (Huang et al. 2020; Shaw et al. 2020; Wen et al. 2020). For this, a highly sensitive (Fig. 4) gold NPs-based lateral-flow chromatographic (AuNP-LF) assay was developed (Fig. 3). Gold nanoparticles were characterized under transmission electron microscopy for the determination of their size and morphology (Huang et al. 2020; Shaw et al. 2020). The IgG anti-mouse antibody and recombinant nucleocapsid (N) protein of coronavirus were developed (Fig. 3) and decontaminated using sodium dodecyl sulfate polyacrylamide gel electrophoresis (SDS–PAGE) (Lopandić et al. 2021). The next step was the conjugation of gold nanoparticles with anti-human IgM antibodies under optimized reaction conditions. AuNP-based LF strips were then formed having one nitrocellulose membrane and three rectangular pads that are (1) sample (2) conjugate and (3) absorbent, each pad varies in size and diameter. The recombinant N protein and IgG anti-mouse antibody were then clogged with the nitrocellulose membrane of the lateral-flow strip. Bioconjugate (AuNP + IgM antibody) was bound to the conjugate pad. The sample pad was restricted for a serum sample. All these pads were blocked using BSA (bovine serum albumin) buffer after the immobilization of compounds on respective pads and dried at 37 °C for at least 1–2 h (Huang et al. 2020; Wen et al. 2020). For detection, the sample was first applied onto the sample pad. IgM antibody in blood serum is captured by the bio-conjugate, then it forms a bioconjugate (AuNP + IgM antibody)–IgM complex on the conjugate pad and moved toward the nitrocellulose membrane. If the resulting compound binds with SARS-CoV-2 N protein, then positive results will form, while negative results will appear when the resulting compound binds with an anti-mouse IgG antibody on the analytical membrane of the assay strip (Huang et al. 2020).
Silver nanoparticles
Silver (Ag) has a comprehensive antimicrobial activity against different bacterial, fungal and viral species. According to researchers, it is believed that, unlike other antibiotics, microorganisms have less tendency to generate resistance against silver nanoparticles (AgNPs) which is the ubiquitous fear of nowadays (Du et al. 2020; McKaya 2020) and in this context, AgNPs assumed to be more effective against SARS-CoV-2 for its inhibition (Jeremiah et al. 2020). Ag+ ions inhibit the growth of viruses by suppressing the electron transport mechanisms and by restricting the respiratory enzymes hence hinder the process of DNA function (McKaya 2020). In an overt manner, the potential antiviral activity of AgNPs on novel coronavirus was checked using different sizes and concentrations of AgNPs. The veroE6 cell line was cultured and virus propagation was made by taking the nasophyrengl swab sample from COVID-19-infected patient (Fig. 2). 96-well plates were fertilized with 5 × 10^4 cells, then dissolved in 10% FBS/DMEM and allowed to mature overnight. After that, supernatants were extracted and then added in corresponding virus-diluted wells. Incubation was done at 37 ℃ for 96 h. Median tissue culture-infecting dose and multiplicity of infection (MOI) were determined by quadruplicated test and desired concentration of silver nanoparticles was made. Cell Titer-Glo cell viability assay was done and luminescence intensities were detected by GIoMax. RT-qPCR was used to quantify viral copies from the culture supernatant. Results show that AgNPs exhibit cytotoxicity by the formation of reactive oxygen species (ROS) at the best level from 20 ppm veroE6 cells. Diameter around 10 nm was efficient for the inhibition of newly emerged virus at a concentration ranging from 1 to 10 ppm, while cytotoxicity can be seen at the concentration of 20 ppm. Luciferase-based pseudo-virus entry assay spills the beans on AgNps potential for inhibiting the viral entry process by disrupting viral integrity (Jeremiah et al. 2020). Filtering medium also plays a pivotal role in suppressing the spread of COVID-19 by limiting their circulation, but it cannot inactivate and suppress the proliferation of these viruses. Ag nanoparticles can be used to inactivate the SARS-CoV-2 virus on filtering media. In a study, the virucidal effects of Ag nanoparticles were conducted by depositing two disposable facial FFP3 masks with a thin sputtered antimicrobial silver nanocluster in pure Argon. Scanning electron microscopy was used to find out the structure and content of viral coating on masks. RNA taken from COVID-19 patients was added on coated and non-coated mask pieces. After adding strains, pieces were incubated in Petri dishes. Both samples were autoclaved and sterilized. The second experiment was done without sterilization under a laminar flow hood to check the maximum working capacity of Ag nanoparticles. After 1 h and 30 min, 100 µl from the first experiment and 200 µl from the second experiment were conjugated on all mask pieces, to obtain the inoculum. 50 µl inoculum with two-fold serial dilution was added to six wells of bottom tissue culture micro-titer plate. For the observation of structural changes, staining can be done using a crystal violet solution. In the end, the blue color indicates the absence of viable virus which is surely a sign of virucidal effects of AgNPs in mask resulting in the reduction of titer of SARS-CoV-2 to zero. It will increase the shelf life of filtering media with less waste production related to disposal (Balagna et al., 2020).
Magnetic nanoparticles
Nanoparticles in the treatment of viral infections showed very effective and promising results. The antimicrobial activity of metallic oxide nanoparticles having a good limit of detection (Fig. 4) was recently reported (Abo-zeid and Williams 2020). The production of reactive oxygen species (ROS) has antimicrobial properties, they oxidize multiple sites of microorganisms, resulting in cell death due to non-resistive activity (Abo-zeid et al. 2020). The antimicrobial activity of iron oxide nanoparticles against various viruses have also been reported (Abo-zeid and Williams 2020; Paunovic et al. 2020) and investigated against H1N1 (Kumar et al. 2019), dengue virus (Murugan et al. 2017) and rotavirus (Gutierrez et al. 2009). The potential antiviral activity of iron oxide nanoparticles on HCV and SARS-CoV-2 has been declared by molecular docking studies. This reveals the effective interaction of Fe2O3 and Fe3O4 with the receptor-binding domain of novel coronavirus and HCV glycoproteins, E1 and E2. Fe2O3 binds with HCV E1 and E2 and makes a stabilized complex, while Fe3O4 coupled with S1-RBD antigen. These interactions may cause conformational changes in virus structure and also influence the antiviral activity (Abo-zeid and Williams 2020).
Graphene nanoparticles
Graphite, an sp2 hybridized allotropic form of carbon is arranged in a honeycomb lattice-like specialized structure to form graphene-based nano-sheets (Raval et al. 2020). These nano-sheets possess characteristic features including lightweight, unique physical, chemical, optical, thermal and electrical properties along with specialized surface functionality, surface-enhanced Raman scattering, high surface-to-mass ratio and large surface area, which is useful for the biosensing and imaging of viral antigens in human hosts (Alphandéry 2020; Vermisoglou et al. 2020). Graphene-based nanoparticle (GBNs) acts as a diagnostic tool for the diagnosis of human coronavirus (SARS-CoV-2). Scientists can modify the surface of graphene nanoparticles by adding functional groups to enhance their sensitivity and specificity. Graphene is linked with other compounds to form graphene-based complexes like reduced graphene, functionalized graphene and graphene oxide which are useful for biomedical procedures, drug delivery and several therapeutic purposes (Alphandéry 2020; Cordaro et al. 2020). Physicochemical and mechanical exfoliation-based top–down approaches are used for the synthesis of GBNs (Cordaro et al. 2020; Seo et al. 2020). For the mechanical shear exfoliation method, graphite flakes were added in 25 ml acetone solution for almost 45 min. After this, the whole soaked mixture was centrifuged for 10 min at 1000 rpm. The supernatant was separated and washed with demineralized water and then dried under 80 °C for 12 h (Cordaro et al. 2020). For the detection of SARS-CoV-2, a blood serum/saliva sample was placed on the chip of the wireless device. A linker probe named 1-pyrenebutyric acid N-hydroxysuccinimide was used for the conjugation of anti SARS-CoV-2 spike antibody (S) onto the surface of graphene nanoparticles. To visualize the presence of a virus, electrochemical calculations were used and its detection is based on the voltage meter that is the part of the sensing device. The voltage of the device was checked before and after the immobilization of the S antibody. If the needle of the voltage meter moves downward, it means the virus is present in the sample. The lower limit of detection of SARS-CoV-2 from this method was 200 copies/ml (Fig. 4) (Seo et al. 2020).
Lipid nanoparticles
Nanotechnology-based challenges and the therapeutic development against SARS-CoV-2 are not different from other diseases (Kostarelos 2020). There are some similar vaccine developmental strategies against the previously known coronaviruses, i.e. SARS and MERS (Nicogossian 2012). Scientists can target-specific cellular and intracellular activities which are involved in the physiopathology of SARS-CoV-2. The controlled nanocarrier drug release is the best solution to mitigate viral rebounds during the treatment of viral infections (Sago et al. 2018). Thus, nanomedicine-based strategies can improve the therapeutic development against the SARS-CoV-2. In nanomedicine research, many challenges may occur in the nanomedicine developmental purposes (Szebeni et al. 2018), and for this, more efficient payload lump repression is required (Qi et al. 2017). Nanoparticles with some lipids, polylactide and aurora B kinase inhibitor develop very enthusiastic results that minimize the toxicity of the infection (Ashton et al. 2016). There are also some limitations in their systematic circulation with nano- and nucleic acid-based drug delivery (Draz et al. 2014; Ku et al. 2016). In nanobiotechnology, lipid nanoparticles containing siRNA help to prevent the disease (Adams et al. 2018). There are also many examples of lipid-based nanoparticles that assist in antiviral activities like mesoporous silica lipid nanoparticles help in the inhibition of some viral activities and increase the circulating time and biocompatibility by in vivo process (LaBauve et al. 2018). Nanocarriers can also prevent the systemic immunotoxicity of protein-based drugs and promote immuno-oncology therapeutics (Zhang et al. 2020a, b).
Quantum dots
Quantum dots (QDs) are useful for the diagnosis of different therapeutic diseases. QDs are not only helpful in the targeted delivery of drugs to treat infectious agents but are also used for the imaging of various microorganisms (Manivannan and Ponnuchamy 2020). They have the potential to combat the novel deadly coronavirus. They act as semiconductor nanomaterials and imaging probes for the biosensing of numerous microbes, as they generate fluorescence due to the pathogenic response (Boles et al. 2016). QDs having photostability, good specificity (Fig. 4), thermal stability, low toxicity and higher biocompatibility are useful for biological activities (Ahmed et al. 2018). Quantum dots interact with the structural protein of a novel coronavirus named "S" and interfere with the replication machinery of the viral genome (Huang 2008; Ting et al. 2018). Conjugation of specific functional groups with quantum dots exerts appropriate properties which affect the viral genome replication when binding to the SARS-CoV-2 receptor (Huang 2008). Carbon-based quantum dots (CDs) were previously used for the detection of viral species. CDs formed by the hydrothermal method were immobilized with boric acid and formed a bioconjugate which entered into the viral genome and activated the production of interferon-alpha genes to silence the spike protein of coronavirus and obstruct the accumulation of reactive oxygen species in the cell. (Łoczechin et al. 2019; Chen and Liang 2020). A combination of QDs with ultrasensitive lateral-flow chromatographic assay and transcription activators could significantly enhance the specificity and live cell imaging functionality of the assay (Iannazzo et al. 2018).
Newly developed chiral zirconium quantum dots (Zr QDs) from the IV B group of the periodic table have gained the spotlight because of their high chirality and low toxicity (Liu et al. 2016). Zr QDs were previously synthesized by the conjugation of Zr Nps with ascorbic acid and the resulting compound was kept in the autoclave at 150 °C for 1 h. Cytotoxicity of Zr QDs was checked by methylthiazolyldiphenyl-tetrazolium (MTT) assay on the C6 glioma cells of the rat. Zr QDs coupled with anti-infectious bronchitis virus (IBV) to form a bioconjugate (Ahmed et al. 2018). Magnetic nanoparticles immobilized with gold (Au) plasmonic element that were then attached with bioconjugate (Zr QDs + (IBV) coronavirus antibodies), these nanoparticles would typically increase the fluorescence up to 25% when attach with Zr QDs (Liu et al. 2016; Ahmed et al. 2018). An additional magnet was used to separate the magneto-plasmonic fluorescent and analyte concentration can easily be measured by photoluminescence intensity. IBV showed higher fluorescence and absorbance peak with bioconjugate (Zr QDs + (IBV) coronavirus antibodies), all this would confirm the presence of an analyte in the reaction mixture. This test was more sensitive as compared to the conventional immunological ELIZA-based assay (Ahmed et al. 2018).
Detection of COVID-19 through biosensors
Carbon nanotube-based nanosensors
Most chronically ill, immunosuppressed, diabetic, dementia, and aged patients are more susceptible to infection with SARS-CoV-2. Another great discovery has shown the fact that the dopamine-release mechanism in the central nervous system helps in the entry and propagation of the SARS-CoV-2. The patient having COVID-19 can also feel the acquaintance of cytokine storm syndrome, which is the symptom of blood–brain barrier breakage. Such cases are exceptional, but in the case of COVID-19, it is still unclear. Dopamine may cause up-regulation of viral entry and downregulation of the immune system response during the disease period and ultimately increase the shelf life of this etiological agent. As a result of this, the virus starts attacking the macrophages during early infection stages; however, dopamine agonists can suppress this activity. SARS-CoV-2 can increase its survival by taking the advantage of dopaminergic receptors (Khalefah and Khalifah 2020). For the detection, neurotransmitters including dopamine, fibrinogen (f), and serotonin type of nanoparticles are being engineered because of their prominent role in biological sensing, imaging, and delivery applications. Carbon single-walled nanotube-based nanosensors (SWCNT) can potentially detect such neurotransmitters rapidly because rapid protein binding events occur on the nanoparticle surface resulting in the detection of neurotransmitters (Pinals et al. 2020). In a study conducted with a bioinformatics MEM web tool (multi experiment matrix), the correlation links between messenger RNA (mRNA) levels along with large numerals of human microarray datasets were allowed to combine and integrate which surprisingly resulted in the statistically important co-expression link between ACE2 and Dopa Decarboxylate (DDC), while serotonin and dopamine provided significant proof that dopamine and serotonin levels are involved in the pathophysiology of COVID-19 (Nataf 2020). The screening process of single-walled carbon nanotubes was prepared in recent research to use against a panel of human blood proteins to detect fibrinogen along with high selectivity with fluorescence. A unique multi-walled carbon nanotube (MWCNT) has been made as a stable and most precise electrochemical sensor consisting of Zn–Ni (Zinc–Nickel) bimetallic nanoalloys. The characterization of this sensor has been performed by various physical techniques, such as XRD, XPS, TEM and Raman. They indicated that the sensor is capable of outstanding properties, such as structural durability, rich pore channels, and large surface area, which facilitated the mass transfer and conduction of electrons for the detection of neurotransmitters (dopamine and uric acid). In this study, the efficiency of MWCNT was enhanced by the help of f-MWCNT which was used as a supporting agent to determine dopamine, uric acid and ascorbic acid levels in the host body (Savk et al. 2019a).
Studies suggested that novel SARS-CoV-2 antibody functionalized with SWCNT-based FET biosensor has been developed to identify the antibodies of SARS-CoV-2 in less than 5 min with a high level of specificity and ultrasensitivity (Shao et al. 2021). For the sake of improved target sensing and optical imaging, covalent surface modifications could be done on single-walled carbon nanotubes SWCNT. As reported, covalent modifications can enhance the dispersion of hydrophobic SWCNTs in an aqueous solution to perform their delivery purposes and work as nanosensors. SWCNTs after covalent modifications maintain the intrinsic fluorescence response towards its analyte for particular nanosensors (Chio et al. 2020). An experimental analysis reported that non-photo bleaching fluorescent array-based SWCNT has been used to study the cellular dopamine efflux from PC12 neuroprogenitor cells. As it is believed cells communicate with each other using the waves of chemical concentrations. So this attribution of cells has been used to analyze the working of carbon-based sensors which not only indicate the chemical dopamine efflux but also give information about the cell morphology and its influence on the release sites (Kruss et al. 2017).
Wearable electronics with artificial intelligence
In this recent era, technology has been modified according to the needs of the twenty-first century. The newly developed technology has done manipulation in biosensors, all these electronic labs on a chip device can be inserted into wearable devices, so that coronavirus symptoms and other physiological factors like body’s internal temperature, oxygen saturation, palpitations and breathlessness can be easily monitored in a real time (Mujawar et al. 2020). Wearable devices have excellent adherence capability, positive and negative predictive values and show good sensitivity and specificity ratios (Hansora et al. 2015). Modifications in biosensors are always being made to enhance their sensitivity for clinical applications including the diagnosis of SARS-CoV-2. Artificial intelligence is a deep learning program that has the potential to copy human physical and chemical parameters by computers that then analyze and interpret data accordingly. An advanced technology, isothermal nucleic acid amplification used as an alternative to RT-PCR which helps to get rid of several cycles of temperature and a positive result could be easily obtained within 5 min and negative results might be obtained within 13 min. Wearable and non-wearable biosensors based on optical, thermal, electrochemical and piezoelectric properties have shown potential in diagnostic testing of cholesterol, infectious diseases, blood glucose, triglyceride and many others. Additionally, researchers are working to enhance their sensitivity and specificity ratios even at pico-molar stages using new and efficient technologies (Van Vliet et al. 2010). For the detection of infectious pathogens including alpha, beta and delta strains of COVID-19, sensitivity level up to femtomolar level is also emerging, this will ultimately be helpful in the early-stage detection of target-specific biomarkers at very low level.
Wearable electrical microsensors are referred to as the first generation of smart sensing devices. While second-generation sensing devices are considered as electrical and optical devices. Nanosensors are considered as the third-generation electrical devices; these devices are more flexible and biocompatible as compared to others (Li et al. 2020; Wu et al. 2020). These rechargeable wearable devices can be worn on the chest, upper and lower arm, legs and on other parts of the body for 22–23 h, resulting in the identification of severe COVID-19 symptoms (Hansora et al. 2015). Nanowires-based biosensors have also been discovered which utilize antibody mimic proteins to diagnose SARS-CoV-2. Patients who are positive or at high risk of COVID-19 are directed to attach the wearable biosensors to get remote monitoring at their homes. COVID-19 patients can use everion which is one of the arm-based wearable devices and is used to check heart rate, oxygen saturation, skin blood perfusion, body temperature, electrochemical activity, activities related to cough, and barometric pressure. Additionally, COVID-19 patients are instructed to note their cough sounds and report their developing physical factors through mobile phone devices. The obtained results will then be transferred to cloud storage and further processing will be done using artificial intelligence-based bio-vital platform for SARS-CoV-2 detection. The mobile phones of the recent era have the potential to easily record and manage data, while data analysis and data sharing can be performed by artificial intelligence-based internet of medical things (IoMT) through this E, (electronics) health would then be converted into I (Intelligent) health.
Paper-based electrochemical biosensor chip
The diagnosis of SARS-CoV-2 at a larger extent to down-regulate its spread is the exigency of the time. During the deadly COVID-19 pandemic, electrochemical platforms have shown the potential to recognize significant limitations of conventional diagnostic platforms including accuracy, affordability, sensitivity, and portability. Despite other limitations, electrochemical biosensors are proving their worth at the initial stages and responding in a good way. On the other hand, electrochemical techniques are good in use because of their properties like cost-effectiveness, simplicity of service, rapid response with high sensitivity, miniaturization, and easy to use in the molecular diagnostic field (Pashchenko et al. 2018).
An electrochemical biosensor has been prepared using antisense oligonucleotides for the ultrasensitive, quick, and quantitative discovery of SARS-CoV-2 in less than 5 min which ultimately overcome the disadvantages of the other two methods of detection being done in the market (Alafeef et al. 2020). This effective electrochemical biosensor chip has gold nanoparticles (AnNPs) which were capped to the extent with antisense oligonucleotides (ssDNA) directed to target the nucleocapsid phosphoprotein (N gene) of the virus. The sensing probe has been set in a conjugated form on a paper-based electrochemical device (Alafeef et al. 2020). In a study, samples were collected from Vero cells infected with SARS-CoV-2 having a sensitivity of 231 copies/µl –1 copy/µl. The electrochemical biosensor was successful in the detection of the target SARS-CoV-2 with 100% specificity, accuracy, and sensitivity in less than 5 minutes. The main performance of this sensor is its limit of detection (LOD). Due to this feature, the LOD of the target as substrate can distinguish from its absence with a pre-defined and pre-settled confidence level which is usually 99%. The LOD could easily be calculated based on the statistics obtained from the slop of the sensor and blank measurement points. This electrochemical biosensor could be the best source to quantify the viral RNA load, which is an important quantitative indicator and is pointing towards the progression of infection. These sensors could be effectively used at the hospitals or even at home for rapid testing with modifications like sensors attached with LED screens and microcontrollers or through a smartphone via WIFI or Bluetooth (Pashchenko et al. 2018).
Magnetic biosensor
Magnetic nanosensing represents different branches of biosensing and magnetic areas in the current time. Different platforms are using magnetic nanomaterials as subsidiaries to enhance virus detection. In magnetic biosensors, the magnetic nanoparticles as magnetic tags are functionalized with antibodies or DNA/RNA probes that can efficiently bind to the target analytes specifically. Magnetic tags convert these concentrations into signals. In comparison to electrochemical, optical, and plasmonic biosensing, magnetic biosensing makes low noise in the background due to this reason the greater part of the biological environment enables an accurate and effective detection process (Wu et al. 2020).
In research, rapid detection of the viral genome including + ssRNA and spike protein S of SARS- CoV-2 with a giant magnetoresistive (GMR) biosensor has been developed. Magnetic biosensors with magnetic tags usually magnetic nanoparticles (MNPs) are widely being used because of their small size, high coercivity, mono-dispersity, and super magnetic behavior, high magnetic susceptibility, and low temperature. MNPs are known for the detection of deadly respiratory pathogens. There are several methods to make magnetic nanoparticles like wet chemical, template-directed microemulsion, thermal decomposition, solid-state, deposition method, spray pyrolysis, self-assembly, and lithography. However, these methods have demerits due to their irregular shape and the possibility of contamination at the time of synthesis. Microemulsion, chemical vapor deposition and arc discharge are declared as suitable methods for biomedical applications by MNPs till today. Functionalization of MNPs is a major important step after synthesis to improve the defects from its surface with the help of grafting of inorganic coating. Without functionalization, MNPs can restrict bio-detection, bio-imaging, bio-sensing, and biomedicine mechanisms. For the enhancement of the stability of MNPs, some organic compounds are being used like glycine, carboxylate and acropolis. The basic principle of GMR biosensors is the changing of magnetization by altering the electrical resistance from high to low. Due to the spin collision at the interface between the pathogen to be detected and MNPs. With the increase in the spin collision, the electrical resistance decreases which ultimately increases the magnetization in the interface between MNPs and protein, by performing the proper calibration to the infected body. After getting signals, results can be obtained with low cost, low noise production, and less time consumption (Aminul Islam and Ziaul Ahsan 2020).
Nanoparticle-based biosensor combined with reverse transcription-loop mediated isothermal amplification (RT-LAMP)
A newly developed biosensor named lateral flow coupled with molecular-based amplification method shows remarkable advantages for the identification of SARS-CoV-2 in hospitalized patient samples (Zhu et al. 2020). This point-of-care device has unique physicochemical properties including excellent robustness, good sensitivity and specificity values, cost-effectiveness, good reliability and a lower limit of detection. For diagnosis, human coronavirus genes ORF1ab and N from oropharynx swab samples were amplified using two RT-LAMP primers. The five end of the ORF1ab gene was labeled with fluorescein, while digoxigenin was used to label the five end of N gene of coronavirus. Three ends of both genes were labeled with a bio-conjugate (biotin + streptavidin) (Zhu et al. 2020). The lateral-flow assay comprises four parts including an inlet pad, conjugating pad, middle nitrocellulose membrane and an absorbent pad (Fig. 5). A swab sample was inserted onto the inlet (sample pad) along with a running buffer, which was then absorbed by the lateral-flow biosensor (LFB). The nitrocellulose membrane has three sections represented by control, line 1 and line 2. Antibodies extracted from sheep (anti-digoxigenin) and rabbit (anti-fluorescein) were being attached to the nitrocellulose membrane along with labeled bovine serum albumin. To develop lateral-flow assay (LFA), streptavidin protein coupled with nanoparticles then loaded over the conjugated pad (Kaewphinit et al. 2013; Banerjee and Jaiswal 2018; Zhu et al. 2020). The developed LFA has the ability to identify SARS-CoV-2 genes.
Results were determined through lateral-flow biosensor using primers labeled with biotin, digoxin and fluorescein. ORF1ab gene was captured by anti-fluorescein antibody in the line 1 region of nitrocellulose membrane (NM) while N gene was captured by anti-digoxigenin antibody in test line 2 region of NM. Bovine serum albumin was immobilized on the control line of NM. Bio-conjugate coupled with nanoparticles was captured by the bovine serum (Kaewphinit et al. 2013; Zhu et al. 2020). All this explains the complete flow of the amplification products through the lateral-flow biosensor. For positive results, all three sections of the nitrocellulose membrane showed red lines simultaneously and if the red line appears only on the control line, then this would indicate the absence of the desired gene in the sample mixture. Both genes were detected due to the presence of nanoparticles (Banerjee and Jaiswal 2018; Zhu et al. 2020). This lab on a chip device is highly sensitive and specific and has a lower limit of detection approximately equal to 12 copies/reaction. The overall detection is completed within 1 h (Mukama et al. 2020; Zhu et al. 2020).
FET biosensor
Biosensors are point-of-care (POC) devices that play a significant role in the detection of biological analytes including viruses (Saylan et al. 2019). The diagnosis done by biosensors is fast, reliable and cost-effective as compared to other molecular-based detection methods (Pohanka and Skládal 2008). When COVID-19 occurred in late December 2019, detection of this etiological agent was very laborious at that time, although RT-PCR was the gold standard for the identification of SARS-CoV-2, detection through this method was time-consuming and costly (Arevalo-Rodriguez et al. 2020). Field effect transistor (FET) has significant importance in this regard. This immunological-based biosensing device has a greater limit of detection (1Fg/mL) instead of other molecular assays. The sensitivity and specificity of SARS-CoV-2 could enhance by the conjugation of nanoparticles (Seo et al. 2020). Specifically, graphene-based nanosheets are used in FET biosensor devices because of their unique characteristics like; greater surface area, good heat, electrical and optical conductivity (Torrente-Rodríguez et al. 2020). Graphene is light weighted material having a hexagonal monolayer lattice-type sp2 hybridized structure (Yin et al. 2020). This graphene-based biosensor was specifically designed to diagnose spike protein of SARS-CoV-2. Multiple sample types including nasopharyngeal swab, oropharyngeal swab, throat swabs and blood samples can be used for the detection of SARS-CoV-2 (Seo et al. 2020). For the fabrication of graphene sheets onto the biosensor, first, graphene was attached to the SiO2 surface by the wet transfer method. Polymethyl methacrylate (PMMA) was then centrifuged for 10 s at 500 rpm onto the graphene sheets. The copper foil was used to immobilize the polymethyl methacrylate over the graphene layer. When copper foil was fully implanted onto the graphene sheet, then PMMA layers were wiped off using microscope glass slides. Secondly, the PMMA scaffold was loaded over the SiO2 substrate and dried overnight and then it was removed using alcohol. Finally, isopropanol washing was done after the fabrication of graphene onto the substrate surface (Kuila et al. 2011; Seo et al. 2020). Through photolithography, the immobilized graphene was copied horizontally. The resulting biosensor was dipped into pyrene butanoic acid succidymidyl ester (PBASE) at 25 °C for 60 min and then washed with deionized water and phosphate buffer saline (Wu et al. 2017; Seo et al. 2020). After this, SARS-CoV-2 spike antibody was exposed to graphene-based biosensor device. The thermal evaporation method was used to generate copper electrodes onto the graphene layer. For the characterization of graphene sheets, Raman spectroscopy and high-resolution electron microscopy were selected. Electrical measurements were observed by a semiconductor detector that showed the presence or absence of the coronavirus spike protein through mapping images (Seo et al. 2020; Yin et al. 2020).
COVID-19 detection by surface enhanced raman spectroscopy
Advancement in the technological era has introduced a microfluidic chip-based biosensing device named Surface Enhanced Raman Spectroscopy (SERS). This device has the potential to detect and analyze the chemistry of various substances (Moore et al. 2018). SERS is considered as the most promising tool for the diagnosis of SARS-CoV-2 (Henry et al. 2016). This technology has become a viable alternative to the RT-PCR-based molecular diagnostic assay. Surface Enhanced Raman Spectroscopy is a surface tender approach that reinforce Raman scattering by absorbing different molecules on nanostructures including Au/Ag or carbon nanotubes (Maneeprakorn et al. 2016). This technology is widely used for the detection of various biomarkers (Wang et al. 2014). This lab on a chip device is preferable over the conventional techniques as it can provide highly selective, accurate, cost-effective, fast and ultrasensitive detection of viral antigens (Zhu et al. 2011). This point-of-care (POC) device does not need any special sample preparation protocols and has the ability to detect even a single molecule and traces of antigens under critical situations. For real-time detection of COVID-19 from bodily fluids including nasopharyngeal swabs, oral swabs and sputum samples, a specially designed microfluidic chip having microchannels coupled with either Ag functionalized-based Raman Spectroscopy strips or Au/Ag functionalized carbon nanotubes was used (Shanmukh et al. 2006; Sivashanmugan et al. 2017). Studies suggested that carbon nanotubes have the potential to capture pathogenic substances and keep the virus alive and its structure stable, all this can be achieved using Raman Spectroscopy (Zhu et al. 2011). 3D PDMS-based microfluidic assay having small filter membrane and detection chamber coupled with gold functionalized SERS strip was intended for rapid diagnosis of COVID-19 patients. Vertically arranged carbon nanotubes combined with a microfluidic disk can also be used for detection purpose. Raman signal would enhance the nanoparticles present in the detection chamber, all this can easily be analyzed by the artificial intelligence-based algorithm that was added before the start of the detection process. To predict the specificity of the captured antigen, this biosensing device at first captured the antigen by the vertically aligned nanotubes and then did the characterization of the trapped antigen using any molecular analyses (Lee and Choi 2019; Jadhav et al. 2021).
Conclusion
SARS-CoV-2 has been continuously spreading all over the globe since, December 2019. Scientists are ambitiously working to detect, kill and reduce its pathogenic effects using different amplification, serological and point-of-care devices. Nanotechnology has provided a platform for the scientific community to work together and to produce good strategies for the eradication of the SARS-CoV-2 pandemic. Nanoparticles and biosensors are considered as a hallmark in the detection of SARS-CoV-2 due to their high-throughput and robust mode of action. However, much knowledge is required to understand the nano-technological-based interactions between nano-bio-sensing and SARS-CoV-2 infection. In this review, we highlighted different nanoparticles and biosensor devices that have the potential to combat the current pandemic (COVID-19).
References
Abo-zeid Y, Williams GR (2020) The potential anti-infective applications of metal oxide nanoparticles: a systematic review. Wiley Interdiscip Rev: Nanomed Nanobiotechnology 12(2):1–36. https://doi.org/10.1002/wnan.1592
Abo-zeid Y et al (2020) A molecular docking study repurposes FDA approved iron oxide nanoparticles to treat and control COVID-19 infection. Eur J Pharm Sci 153(July):105465. https://doi.org/10.1016/j.ejps.2020.105465
Adams D et al (2018) Patisiran, an RNAi therapeutic, for hereditary transthyretin amyloidosis. N Engl J Med 379(1):11–21. https://doi.org/10.1056/nejmoa1716153
Ahmed SR et al (2018) Chiral zirconium quantum dots: a new class of nanocrystals for optical detection of coronavirus. Heliyon 4(8):e00766. https://doi.org/10.1016/j.heliyon.2018.e00766
Alafeef M et al (2020) Rapid, ultrasensitive, and quantitative detection of SARS-CoV-2 using antisense oligonucleotides directed electrochemical biosensor chip. ACS Nano 14(12):17028–17045
Alphandéry E (2020) The potential of various nanotechnologies for coronavirus diagnosis/treatment highlighted through a literature analysis. Bioconjug Chem 31(8):1873–1882. https://doi.org/10.1021/acs.bioconjchem.0c00287
Aminul Islam M, Ziaul Ahsan M (2020) Plausible approach for rapid detection of SARS-CoV-2 virus by magnetic nanoparticle based biosensors. Am J Nanosci 6(2):6. https://doi.org/10.11648/j.ajn.20200602.11
Arevalo-Rodriguez I et al (2020) False-negative results of initial RT-PCR assays for COVID-19: a systematic review. PLoS ONE. https://doi.org/10.1371/journal.pone.0242958
Ashton S et al (2016) Aurora kinase inhibitor nanoparticles target tumors with favorable therapeutic index in vivo. Sci Transl Med. https://doi.org/10.1126/scitranslmed.aad2355
Balagna C et al (2020) Virucidal effect against coronavirus SARS-CoV-2 of a silver nanocluster/silica composite sputtered coating. Open Ceram 1:100006. https://doi.org/10.1016/j.oceram.2020.100006
Banerjee R, Jaiswal A (2018) Recent advances in nanoparticle-based lateral flow immunoassay as a point-of-care diagnostic tool for infectious agents and diseases. Analyst 143(9):1970–1996. https://doi.org/10.1039/c8an00307f
Boles MA et al (2016) Erratum: the surface science of nanocrystals (Nature Materials (2016) 15 (141–153)). Nat Mater 15(3):364. https://doi.org/10.1038/nmat4578
Chen L, Liang J (2020) An overview of functional nanoparticles as novel emerging antiviral therapeutic agents. Mater Sci Eng, C 112:110924. https://doi.org/10.1016/j.msec.2020.110924
Chen Y, Liu Q, Guo D (2020) Emerging coronaviruses: Genome structure, replication, and pathogenesis. J Med Virol 92(4):418–423. https://doi.org/10.1002/jmv.25681
Chio L et al (2020) Covalent surface modification effects on single-walled carbon nanotubes for targeted sensing and optical imaging. Adv Func Mater 30(17):1–8. https://doi.org/10.1002/adfm.201910556
Cordaro A et al (2020) Graphene-based strategies in liquid biopsy and in viral diseases diagnosis. Nanomaterials 10(6):1–18. https://doi.org/10.3390/nano10061014
Cortegiani A et al (2020) A systematic review on the efficacy and safety of chloroquine for the treatment of COVID-19. J Crit Care 57:279–283. https://doi.org/10.1016/j.jcrc.2020.03.005
Draz MS et al (2014) Nanoparticle-mediated systemic delivery of siRNA for treatment of cancers and viral infections. Theranostics 4(9):872–892. https://doi.org/10.7150/thno.9404
Du T et al (2020) Gold/Silver hybrid nanoparticles with enduring inhibition of coronavirus multiplication through multisite mechanisms. Bioconjug Chem 31(11):2553–2563. https://doi.org/10.1021/acs.bioconjchem.0c00506
García Reyes LE (2013) 済無No title no title. J Chem Inf Model 53(9):1689–1699
Gutierrez L et al (2009) Adsorption of rotavirus and bacteriophage MS2 using glass fiber coated with hematite nanoparticles. Water Res 43(20):5198–5208. https://doi.org/10.1016/j.watres.2009.08.031
Hansora DP, Shimpi NG, Mishra S (2015) Graphite to graphene via graphene oxide: an overview on synthesis, properties, and applications. JOM 67(12):2855–2868. https://doi.org/10.1007/s11837-015-1522-5
Henry AI et al (2016) Surface-enhanced Raman spectroscopy biosensing: in vivo diagnostics and multimodal imaging. Anal Chem 88(13):6638–6647. https://doi.org/10.1021/acs.analchem.6b01597
Hofmann H, Pöhlmann S (2004) Cellular entry of the SARS coronavirus. Trends Microbiol 12(10):466–472. https://doi.org/10.1016/j.tim.2004.08.008
Huang SL (2008) Liposomes in ultrasonic drug and gene delivery. Adv Drug Deliv Rev 60(10):1167–1176. https://doi.org/10.1016/j.addr.2008.03.003
Huang C et al (2020) Rapid detection of IgM antibodies against the SARS-CoV-2 virus via colloidal gold nanoparticle-based lateral-flow assay. ACS Omega 5(21):12550–12556. https://doi.org/10.1021/acsomega.0c01554
Iannazzo D et al (2018) Graphene quantum dots based systems as HIV inhibitors. Bioconjug Chem 29(9):3084–3093. https://doi.org/10.1021/acs.bioconjchem.8b00448
Jadhav SA et al (2021) Development of integrated microfluidic platform coupled with surface-enhanced Raman spectroscopy for diagnosis of COVID-19. Med Hypotheses 146:110356. https://doi.org/10.1016/j.mehy.2020.110356
Jeremiah SS et al (2020) Potent antiviral effect of silver nanoparticles on SARS-CoV-2. Biochem Biophys Res Commun 533(1):195–200. https://doi.org/10.1016/j.bbrc.2020.09.018
Kaewphinit T et al (2013) Detection of mycobacterium tuberculosis by using loop-mediated isothermal amplification combined with a lateral flow dipstick in clinical samples. Biomed Res Int 2013:86–88. https://doi.org/10.1155/2013/926230
Khalefah MM, Khalifah AM (2020) Determining the relationship between SARS-CoV-2 infection, dopamine, and COVID-19 complications. J Taibah Univ Med Sci 15(6):550–553. https://doi.org/10.1016/j.jtumed.2020.10.006
Kim HY et al (2008) In vitro inhibition of coronavirus replications by the traditionally used medicinal herbal extracts, cimicifuga rhizoma, meliae cortex, coptidis rhizoma, and phellodendron cortex. J Clin Virol 41(2):122–128. https://doi.org/10.1016/j.jcv.2007.10.011
Kostarelos K (2020) Nanoscale nights of COVID-19. Nat Nanotechnol 15(5):343–344. https://doi.org/10.1038/s41565-020-0687-4
Kruss S et al (2017) High-resolution imaging of cellular dopamine efflux using a fluorescent nanosensor array. Proc Natl Acad Sci USA 114(8):1789–1794. https://doi.org/10.1073/pnas.1613541114
Ku SH et al (2016) Chemical and structural modifications of RNAi therapeutics. Adv Drug Deliv Rev 104:16–28. https://doi.org/10.1016/j.addr.2015.10.015
Kuila T et al (2011) Recent advances in graphene-based biosensors. Biosens Bioelectron 26(12):4637–4648. https://doi.org/10.1016/j.bios.2011.05.039
Kumar R et al (2019) Iron oxide nanoparticles based antiviral activity of H1N1 influenza A virus. J Infect Chemother 25(5):325–329. https://doi.org/10.1016/j.jiac.2018.12.006
LaBauve AE et al (2018) Lipid-coated mesoporous silica nanoparticles for the delivery of the ML336 antiviral to inhibit encephalitic alphavirus infection. Sci Rep 8(1):1–13. https://doi.org/10.1038/s41598-018-32033-w
Lee S, Choi I (2019) Fabrication strategies of 3D plasmonic structures for SERS. BioChip J 13(1):30–42. https://doi.org/10.1007/s13206-019-3105-y
Li G, Wu Y, Li Y, Hong Y, Zhao X, Reyes PI, Lu Y (2020) Early stage detection of Staphylococcus epidermidis biofilm formation using MgZnO dual-gate TFT biosensor. Biosensors Bioelectron 151:111993. https://doi.org/10.1016/j.bios.2019.111993
Liu C et al (2016) Efficient one-pot synthesis of colloidal zirconium oxide nanoparticles for high-refractive-index nanocomposites. ACS Appl Mater Interfaces 8(7):4795–4802. https://doi.org/10.1021/acsami.6b00743
Łoczechin A et al (2019) Functional carbon quantum dots as medical countermeasures to human coronavirus. ACS Appl Mater Interfaces 11(46):42964–42974. https://doi.org/10.1021/acsami.9b15032
Lopandić Z et al (2021) Igm and igg immunoreactivity of sars-cov-2 recombinant m protein. Int J Mol Sci. https://doi.org/10.3390/ijms22094951
Lu R et al (2020) Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. The Lancet 395(10224):565–574. https://doi.org/10.1016/S0140-6736(20)30251-8
Maneeprakorn W et al (2016) Surface-enhanced Raman scattering based lateral flow immunochromatographic assay for sensitive influenza detection. RSC Adv 6(113):112079–112085. https://doi.org/10.1039/C6RA24418A
Manivannan S, Ponnuchamy K (2020) Quantum dots as a promising agent to combat COVID-19. Appl Organomet Chem 34(10):17–22. https://doi.org/10.1002/aoc.5887
McKaya G (2020) Potential role of nitric oxide (NO) and silver/silver nanoparticles in the treatment of COVID-19 infections. Open Access J Biomed Sci. https://doi.org/10.38125/oajbs.000186
Moore TJ et al (2018) In vitro and in vivo sers biosensing for disease diagnosis. Biosensors. https://doi.org/10.3390/bios8020046
Mujawar MA, Gohel H, Bhardwaj SK, Srinivasan S, Hickman N, Kaushik A (2020) Nano-enabled biosensing systems for intelligent healthcare: towards COVID-19 management. Materials. today Chem 17:100306. https://doi.org/10.1016/j.mtchem.2020.100306
Mukama O et al (2020) Synergetic performance of isothermal amplification techniques and lateral flow approach for nucleic acid diagnostics. Anal Biochem 600(March):113762. https://doi.org/10.1016/j.ab.2020.113762
Murugan K et al (2017) Magnetic nanoparticles are highly toxic to chloroquine-resistant plasmodium falciparum, dengue virus (DEN-2), and their mosquito vectors. Parasitol Res 116(2):495–502. https://doi.org/10.1007/s00436-016-5310-0
Nataf S (2020) An alteration of the dopamine synthetic pathway is possibly involved in the pathophysiology of COVID-19. J Med Virol 92(10):1743–1744. https://doi.org/10.1002/jmv.25826
Nicogossian A (2012) In the news. World Med Health Policy 4(1):2020. https://doi.org/10.1515/1948-4682.1230
Pashchenko O et al (2018) A comparison of optical, electrochemical, magnetic, and colorimetric point-of-care biosensors for infectious disease diagnosis. ACS Infect Dis 4(8):1162–1178
Paunovic J et al (2020) Iron-based nanoparticles and their potential toxicity: focus on oxidative stress and apoptosis. Chemico-Biological Interact. https://doi.org/10.1016/j.cbi.2019.108935
Pinals RL et al (2020) Quantitative protein corona composition and dynamics on carbon nanotubes in biological environments. Angew Chem 132(52):23876–23885. https://doi.org/10.1002/ange.202008175
Pohanka M, Skládal P (2008) Electrochemical biosensors - principles and applications. J Appl Biomed 6(2):57–64. https://doi.org/10.32725/jab.2008.008
Qi R et al (2017) Nanoparticle conjugates of a highly potent toxin enhance safety and circumvent platinum resistance in ovarian cancer. Nature Commun. https://doi.org/10.1038/s41467-017-02390-7
Qi F et al (2020) Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem Biophys Res Commun 526(1):135–140. https://doi.org/10.1016/j.bbrc.2020.03.044
Ranjan P et al (2021) Rapid diagnosis of SARS-CoV-2 using potential point-of-care electrochemical immunosensor: toward the future prospects. Int Rev Immunol 40(1–2):126–142
Raval B et al (2020) Synthesis of exfoliated multilayer graphene and its putative interactions with SARS-CoV-2 virus investigated through computational studies. J Biomol Struct Dyn. https://doi.org/10.1080/07391102.2020.1817788
Romano M et al (2020) ‘A Structural view of SARS-CoV-2 RNA replication machinery: RNA synthesis proofreading a final capping.’ Cells. https://doi.org/10.3390/cells9051267
Sago CD et al (2018) Erratum: high-throughput in vivo screen of functional mRNA delivery identifies nanoparticles for endothelial cell gene editing (Proceedings of the National Academy of Sciences of the United States of America (2018) 115 (E9944–E9952) DOI: 10.1073/pnas.1811. Proc Natl Acad Sci USA 115(48):E11427. https://doi.org/10.1073/pnas.1818262115
Savk A et al (2019a) Multiwalled carbon nanotube-based nanosensor for ultrasensitive detection of uric acid, dopamine, and ascorbic acid. Mater Sci Eng C 99:248–254. https://doi.org/10.1016/j.msec.2019.01.113
Şavk A, Cellat K, Arıkan K et al (2019b) Highly monodisperse Pd-Ni nanoparticles supported on rGO as a rapid, sensitive, reusable and selective enzyme-free glucose sensor. Sci Rep 9:19228. https://doi.org/10.1038/s41598-019-55746-y
Saylan Y et al (2019) An alternative medical diagnosis method: biosensors for virus detection. Biosensors. https://doi.org/10.3390/bios9020065
Schoeman D et al (2020) Journal pre-proof does the pathogenesis of SAR-CoV-2 virus decrease at high-altitude? Does the pathogenesis of SAR-CoV-2 virus decrease at high-altitude? Corresponding authors. Cell Res 9(1):278–280. https://doi.org/10.3390/ijerph17082932
Seo G et al (2020) Rapid detection of COVID-19 causative virus (SARS-CoV-2) in human nasopharyngeal swab specimens using field-effect transistor-based biosensor. ACS Nano 14(4):5135–5142. https://doi.org/10.1021/acsnano.0c02823
Shanmukh S et al (2006) Rapid and sensitive detection of respiratory virus molecular signatures using a silver nanorod array SERS substrate. Nano Lett 6(11):2630–2636. https://doi.org/10.1021/nl061666f
Shao W et al (2021) Rapid detection of SARS-CoV-2 antigens using high-purity semiconducting single-walled carbon nanotube-based field-effect transistors. ACS Appl Mater Interfaces. https://doi.org/10.1021/acsami.0c22589
Shaw AM et al (2020) Real-world evaluation of a novel technology for quantitative simultaneous antibody detection against multiple SARS-CoV-2 antigens in a cohort of patients presenting with COVID-19 syndrome. Analyst 145(16):5638–5646. https://doi.org/10.1039/d0an01066a
Sivashanmugan K et al (2017) Nanoplasmonic Au/Ag/Au nanorod arrays as SERS-active substrate for the detection of pesticides residue. J Taiwan Inst Chem Eng 75:287–291. https://doi.org/10.1016/j.jtice.2017.03.022
Szebeni J et al (2018) Roadmap and strategy for overcoming infusion reactions to nanomedicines. Nat Nanotechnol 13(12):1100–1108. https://doi.org/10.1038/s41565-018-0273-1
Tetro JA (2020) Is COVID-19 receiving ADE from other coronaviruses? Microbes Infect 22(2):72–73. https://doi.org/10.1016/j.micinf.2020.02.006
Ting D et al (2018) Multisite inhibitors for enteric coronavirus: antiviral cationic carbon dots based on curcumin. ACS Appl Nano Mater 1(10):5451–5459. https://doi.org/10.1021/acsanm.8b00779
Torrente-Rodríguez RM et al (2020) SARS-CoV-2 rapidplex: a graphene-based multiplexed telemedicine platform for rapid and low-cost COVID-19 diagnosis and monitoring. Matter 3(6):1981–1998. https://doi.org/10.1016/j.matt.2020.09.027
Van Vliet D, de Vugt ME, Bakker C, Koopmans RTCM, Verhey FRJ (2010) Impact of early onset dementia on care givers: a review. Int J Geriat Psychia 25(11):1091–1100. https://doi.org/10.1002/gps.2439
V’kovski P et al (2021) Coronavirus biology and replication: implications for SARS-CoV-2. Nature Rev Microbiol 19(3):155–170. https://doi.org/10.1038/s41579-020-00468-6
Vermisoglou E et al (2020) Human virus detection with graphene-based materials. Biosens Bioelectron. https://doi.org/10.1016/j.bios.2020.112436
Wang Y, ‘Winston’, et al (2014) Rapid ratiometric biomarker detection with topically applied SERS nanoparticles. Technology 02(02):118–132. https://doi.org/10.1142/s2339547814500125
Wang Q et al (2020) Structural and functional basis of SARS-CoV-2 entry by using human ACE2. Cell 181(4):894-904.e9. https://doi.org/10.1016/j.cell.2020.03.045
Wen T et al (2020) Development of a lateral flow immunoassay strip for rapid detection of IgG antibody against SARS-CoV-2 virus. Analyst 145(15):5345–5352. https://doi.org/10.1039/d0an00629g
Wu G et al (2017) Doping effects of surface functionalization on graphene with aromatic molecule and organic solvents. Appl Surf Sci 425:713–721. https://doi.org/10.1016/j.apsusc.2017.07.048
Wu K et al (2020) Magnetic-nanosensor-based virus and pathogen detection strategies before and during covid-19. ACS Appl Nano Mater 3(10):9560–9580. https://doi.org/10.1021/acsanm.0c02048
Yan S, Wu G (2021) Potential 3-chymotrypsin-like cysteine protease cleavage sites in the coronavirus polyproteins pp1a and pp1ab and their possible relevance to COVID-19 vaccine and drug development. FASEB J 35(5):1–9. https://doi.org/10.1096/fj.202100280RR
Yan S et al (2020) An evolutionary RGD motif in the spike protein of SARS-CoV-2 may serve as a potential high risk factor for virus infection? Preprints. https://doi.org/10.2094/preprints202002.0447.v1
Yin X et al (2020) Lightweight and flexible 3D graphene microtubes membrane for high-efficiency electromagnetic-interference shielding. Chem Eng J 387:124025. https://doi.org/10.1016/j.cej.2020.124025
Zhang C, Shi L, Wang FS (2020a) Liver injury in COVID-19: management and challenges. The Lancet Gastroenterol Hepatol 5(5):428–430. https://doi.org/10.1016/S2468-1253(20)30057-1
Zhang H et al (2020b) Angiotensin-converting enzyme 2 (ACE2) as a SARS-CoV-2 receptor: molecular mechanisms and potential therapeutic target. Intensive Care Med 46(4):586–590. https://doi.org/10.1007/s00134-020-05985-9
Zhang Q et al (2021) Molecular mechanism of interaction between SARS-CoV-2 and host cells and interventional therapy. Signal Transduct Targeted Ther. https://doi.org/10.1038/s41392-021-00653-w
Zhu Z et al (2011) Superstructures and SERS properties of gold nanocrystals with different shapes. Angewandte Chemie-Int Edition 50(7):1593–1596. https://doi.org/10.1002/anie.201005493
Zhu X et al (2020) Multiplex reverse transcription loop-mediated isothermal amplification combined with nanoparticle-based lateral flow biosensor for the diagnosis of COVID-19. Biosens Bioelectron 166:112437. https://doi.org/10.1016/j.bios.2020.112437
Acknowledgements
Syed Babar Jamal acknowledges the contribution of all authors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethical approval
The review article is exempted for ethical approval.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Abid, R., Shahzad, M.K., Sulaman, S.M. et al. Therapeutic significance of nano- and biosensor technology in combating SARS-CoV-2: a review. Appl Nanosci 12, 3127–3140 (2022). https://doi.org/10.1007/s13204-022-02465-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13204-022-02465-y