Abstract
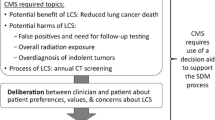
Shared decision-making (SDM) helps patients weigh risks and benefits of screening approaches. Little is known about SDM visits between patients and healthcare providers in the context of lung cancer screening. This study explored the extent that patients were informed by their provider of the benefits and harms of lung cancer screening and expressed certainty about their screening choice. We conducted a survey with 75 patients from an academic medical center in the Southeastern U.S. Survey items included knowledge of benefits and harms of screening, patients’ value elicitation during SDM visits, and decisional certainty. Patient and provider characteristics were collected through electronic medical records or self-report. Descriptive statistics, Kruskal–Wallis tests, and Pearson correlations between screening knowledge, value elicitation, and decisional conflict were calculated. The sample was predominately non-Hispanic White (73.3%) with no more than high school education (53.4%) and referred by their primary care provider for screening (78.7%). Patients reported that providers almost always discussed benefits of screening (81.3%), but infrequently discussed potential harms (44.0%). On average, patients had low knowledge about screening (score = 3.71 out of 8) and benefits/harms. Decisional conflict was low (score = − 3.12) and weakly related to knowledge (R= − 0.25) or value elicitation (R= − 0.27). Black patients experienced higher decisional conflict than White patients (score = − 2.21 vs − 3.44). Despite knowledge scores being generally low, study patients experienced low decisional conflict regarding their decision to undergo lung cancer screening. Additional work is needed to optimize the quality and consistency of information presented to patients considering screening.
Similar content being viewed by others
Data Availability
All data and materials as well as software application or custom code support published claims and comply with field standards.
Code Availability
Available upon request to the corresponding author.
Abbreviations
- EHR:
-
Electronic health record
- CMS:
-
Centers for Medicare and Medicaid Services
- KW:
-
Kruskal–Wallis
- LDCT:
-
Low-dose computed tomography
- REDCap:
-
Research Electronic Data Capture system
- SD:
-
Standard deviation
- SDM:
-
Shared decision-making
- USPSTF:
-
US Preventive Services Task Force
References
Aberle D, Adams A, Berg C et al (2015) Reduced lung-cancer mortality with low-dose computed tomographic screening. N Engl J Med 365(5):2155–2165. https://doi.org/10.1056/NEJMoa0707943
de Koning HJ, van der Aalst CM, de Jong PA et al (2020) Reduced lung-cancer mortality with volume CT screening in a randomized trial. N Engl J Med 382(6):503–513. https://doi.org/10.1056/nejmoa1911793
Krist AH, Davidson KW, Mangione CM et al (2021) Screening for lung cancer: US Preventive Services Task Force recommendation statement. JAMA 325(10):962–970. https://doi.org/10.1001/jama.2021.1117
Meza R, Jeon J, Toumazis I et al (2021) Evaluation of the benefits and harms of lung cancer screening with low-dose computed tomography: modeling study for the US Preventive Services Task Force. JAMA 325(10):988–997. https://doi.org/10.1001/jama.2021.1077
Centers for Medicare & Medicaid Services. Decision memo for screening for lung cancer with low dose computed tomography. Medicare Coverage Database. https://www.cms.gov/medicare-coverage-database/details/nca-decision-memo.aspx?NCAId=274. Published 2015
Nishi SPE, Lowenstein LM, Mendoza TR et al (2021) Shared decision making for lung cancer screening: how well are we “sharing”? Chest May:1–11. https://doi.org/10.1016/j.chest.2021.01.041
Dharod A, Bellinger C, Foley K, Case LD, Miller D (2019) The reach and feasibility of an interactive lung cancer screening decision aid delivered by patient portal. Appl Clin Inform 10(1):19–27. https://doi.org/10.1055/s-0038-1676807
Brenner AT, Malo TL, Margolis M et al (2018) Evaluating shared decision making for lung cancer screening. JAMA Intern Med 178(10):1311–1316. https://doi.org/10.1001/jamainternmed.2018.3054
Shen J, Crothers K, Kross EK, Petersen K, Melzer AC, Triplette M (2021) Provision of smoking cessation resources in the context of in-person shared decision making for lung cancer screening. Chest. Published online. https://doi.org/10.1016/j.chest.2021.03.016
Eberth JM, McDonnell KK, Sercy E et al (2018) A national survey of primary care physicians: perceptions and practices of low-dose CT lung cancer screening. Prev Med Rep 11(January):93–99. https://doi.org/10.1016/j.pmedr.2018.05.013
McDonnell KK, Estrada RD, Dievendorf AC et al (2019) Lung cancer screening: practice guidelines and insurance coverage are not enough. J Am Assoc Nurse Pract 31(1):33–45. https://doi.org/10.1097/JXX.0000000000000096
Melzer AC, Golden SE, Ono SS, Datta S, Crothers K, Slatore CG (2020) What exactly is shared decision-making? A qualitative study of shared decision-making in lung cancer screening. J Gen Intern Med 35(2):546–553. https://doi.org/10.1007/s11606-019-05516-3
Zeliadt SB, Hoffman RM, Birkby G et al (2018) Challenges implementing lung cancer screening in federally qualified health centers. Am J Prev Med 54(4):568–575. https://doi.org/10.1016/j.amepre.2018.01.001
Kanodra N, Pope C, Halbert C, Silvestri G, Rice L, Tanner N (2016) Primary care provider and patient perspectives on lung cancer screening. A qualitative study. Ann Am Thorac Soc 13(11):1977–1982
Wiener RS, Koppelman E, Bolton R et al (2018) Patient and clinician perspectives on shared decision-making in early adopting lung cancer screening programs: a qualitative study. J Gen Intern Med 33(7):1035–1042. https://doi.org/10.1007/s11606-018-4350-9
Slatore C (2019) COUNTERPOINT: can shared decision-making of physicians and patients improve outcomes in lung cancer screening? No. Chest 156(1):15–17
Hoffman RM, Reuland DS, Volk RJ (2021) The Centers for Medicare & Medicaid Services requirement for shared decision-making for lung cancer screening. JAMA 325(10):933–934. https://doi.org/10.1056/nejmoa1102873
Lowenstein LM, Richards VF, Leal VB et al (2016) A brief measure of smokers’ knowledge of lung cancer screening with low-dose computed tomography. Prev Med Rep 4:351–356. https://doi.org/10.1016/j.pmedr.2016.07.008
Elwyn G, Hutchings H, Edwards A et al (2005) The OPTION scale: measuring the extent that clinicians involve patients in decision-making tasks. Health Expect 8(1):34–42. https://doi.org/10.1111/j.1369-7625.2004.00311.x
Carter-Harris L, Slaven JE, Monohan P, Rawl SM (2017) Development and psychometric evaluation of the lung cancer screening health belief scales. Cancer Nurs 40(3):237–244. https://doi.org/10.1097/NCC.0000000000000386
Fukunaga MI, Halligan K, Kodela J et al (2020) Tools to promote shared decision-making in lung cancer screening using low-dose CT scanning: a systematic review. Chest 158(6):2646–2657. https://doi.org/10.1016/j.chest.2020.05.610
Khairy M, Duong DK, Shariff-Marco S et al (2018) An analysis of lung cancer screening beliefs and practice patterns for community providers compared to academic providers. Cancer Control 25(1):1–8
Hoffman RM, Sussman AL, Getrich CM et al (2015) Attitudes and beliefs of primary care providers in New Mexico about lung cancer screening using low-dose computed tomography. Prev Chronic Dis 9(12):E108
Kanodra NM, Pope C, Halbert CH et al (2016) Primary care provider and patient perspectives on lung cancer screening. A qualitative study. Ann Am Thorac Soc 13(11):1977–1982
Melzer AC, Golden SE, Ono SS, et al (2020) "We just never have enough time": clinician views of lung cancer screening processes and implementation. Ann Am Thorac Soc 17(10):1264-1272. https://doi.org/10.1513/AnnalsATS.202003-262OC
Coughlin JM, Zang Y, Terranella S et al (2020) Understanding barriers to lung cancer screening in primary care. J Thorac Dis 12(5):2536–2544
Lewis JA, Petty WJ, Tooze JA et al (2015) Low-dose CT lung cancer screening practices and attitudes among primary care providers at an academic medical center. Cancer Epidemiol Biomarkers Prev 24(4):664–670
Ersek JL, Eberth JM, McDonnell KK et al (2016) Knowledge of, attitudes toward, and use of low-dose computed tomography for lung cancer screening among family physicians. Cancer 122(15):2324–2331. https://doi.org/10.1002/cncr.29944
Henderson LM, Benefield TS, Bearden SC et al (2019) Changes in physician knowledge, attitudes, beliefs, and practices regarding lung cancer screening. Ann Am Thorac Soc 16(8):1065–1069. https://doi.org/10.1513/AnnalsATS.201812-867RL
Triplette M, Kross EK, Mann BA et al (2018) An assessment of primary care and pulmonary provider perspectives on lung cancer screening. Ann Am Thorac Soc 15(1):69–75. https://doi.org/10.1513/AnnalsATS.201705-392OC
Rajupet S, Doshi D, Wisnivesky JP et al (2017) Attitudes about lung cancer screening: primary care providers versus specialists. Clin Lung Cancer 18(6):e417–e423. https://doi.org/10.1016/j.cllc.2017.05.003
Raju S, Khawaja A, Han X, Wang X, Mazzone PJ (2020) Lung cancer screening: characteristics of nonparticipants and potential screening barriers. Clin Lung Cancer 21(5):e329–e336. https://doi.org/10.1016/j.cllc.2019.11.016
Roth JA, Carter-Harris L, Brandzel S et al (2018) A qualitative study exploring patient motivations for screening for lung cancer. PLoS ONE 13(7):e0196758. https://doi.org/10.1371/journal.pone.0196758
Bellinger C, Pinsky P, Foley K, Case D, Dharod A, Miller D (2019) Lung cancer screening benefits and harms stratified by patient risk: information to improve patient decision aids. Ann Am Thorac Soc 16(4):512–514. https://doi.org/10.1513/AnnalsATS.201810-690RL
Pinsky PF, Bellinger CR, Miller DP Jr (2018) False-positive screens and lung cancer risk in the National Lung Screening Trial: implications for shared decision-making. J Med Screen 25(2):110–112. https://doi.org/10.1177/0969141317727771
Lowenstein LM, Godoy MCB, Erasmus JJ et al (2020) Implementing decision coaching for lung cancer screening in the low-dose computed tomography setting. JCO Oncol Pract 16(8):e703–e725. https://doi.org/10.1200/JOP.19.00453
Studts JL, Thurer RJ, Brinker K, Lillie SE, Byrne MM (2020) Brief education and a conjoint valuation survey may reduce decisional conflict regarding lung cancer screening. MDM Policy Pract 5(1):1–10. https://doi.org/10.1177/2381468319891452
Tammemägi MC, Katki HA, Hocking WG et al (2013) Selection criteria for lung-cancer screening. N Engl J Med 368(8):728–736. https://doi.org/10.1056/nejmoa1211776
Lau YK, Bhattarai H, Caverly TJ et al (2021) Lung cancer screening knowledge, perceptions, and decision making among African Americans in Detroit, Michigan. Am J Prev Med 60(1):e1–e8. https://doi.org/10.1016/j.amepre.2020.07.004
Caverly TJ, Hayward RA (2020) Dealing with the lack of time for detailed shared decision-making in primary care: everyday shared decision-making. J Gen Intern Med 35(10):3045–3049. https://doi.org/10.1007/s11606-020-06043-2
Caverly TJ, Cao P, Hayward RA, Meza R (2019) Identifying patients for whom lung cancer screening is preference-sensitive: a microsimulation study. Physiol Behav 176(3):139–148. https://doi.org/10.7326/M17-2561
Acknowledgements
The authors wish to thank Ms. Erica Sercy for her editorial guidance and edits.
Funding
This study was funded through an institutional grant from the University of South Carolina Office of the Vice President for Research.
Author information
Authors and Affiliations
Contributions
All members of the research team contributed to the review and editing of the manuscript. In addition, authors contributed to study conceptualization (AZ, JME, DM), data curation (SP, SW, AZ), formal analysis (AZ), methodology (AZ, JME, DM), funding acquisition (JME), project administration (JME, DM), supervision (JME, DM), visualization (AZ), and original draft writing (JME, AZ, DM).
Corresponding author
Ethics declarations
Ethics Approval
The study was approved under expedited review (45 CFR 46 — categories #5 and #7) by the Institutional Review Boards of the University of South Carolina and of Wake Forest University.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Previous Abstract Presentation
Selected components of this research were presented at the North Carolina Chapter of the American College of Physician Annual Meeting (February 2021).
Supplementary Information
ESM 1
(DOCX 33.4 KB)
Appendix
Appendix







Rights and permissions
About this article
Cite this article
Eberth, J.M., Zgodic, A., Pelland, S.C. et al. Outcomes of Shared Decision-Making for Low-Dose Screening for Lung Cancer in an Academic Medical Center. J Canc Educ 38, 522–537 (2023). https://doi.org/10.1007/s13187-022-02148-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13187-022-02148-w