Abstract
Introduction
The present study represents the first systematic review summarizing existing publications on older sexual and gender minority (LGBT+) people's engagement with physical activity (PA) aged 65 and over.
Methods
Relevant articles were systematically searched in four scientific databases (i.e., PsychArticles, PsychInfo, Pubmed, and Web of Science) in March 2023. We included original articles published after 1968 with relevant keywords associated with “PA”, “older adults”, and “LGBT+ identity”. Of the 887 records identified, 53 articles were included in the systematic review.
Results
Studies were critically reviewed according to participants’ subjectivity considered in the publications: (a) sexual minority (LGB+) identities; (b) sexual and gender minority (LGBT+) identities; (c) transgender and gender-diverse identities; (d) gay and bisexual male identities; and (e) lesbian and bisexual female identities. The most frequent research areas, taking together all the five identity categories considered in the present review, were the differences between LGBT+ people and cis-heterosexual people, the discrimination and homophobia/transphobia in sport-related contexts, and the competent interventions and aging well in LGBT+ older adults.
Conclusions
Findings suggest a lack of information regarding PA in older LGBT+ aged 65 and over. Future research should investigate the barriers and enablers of PA in older LGBT+ people.
Policy Implications
It is mandatory to promote regular exercise to reduce health disparities between older LGBT+ individuals and their cis-heterosexual counterparts. The policy and environmental implications of the findings for older LGBT+ people are discussed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Existing research underlying that the older LGBT+ community is a vulnerable and marginalized population due to the stigma and discrimination they have experienced over the years (Devís-Devís et al., 2022; Kendrick et al., 2021), especially in socialization contexts such as sport-related contexts (Baiocco et al., 2018, 2020; Brennan-Ing et al., 2022; Pistella et al., 2020). The global population is aging significantly, and the number of older LGBT+ adults is likely increasing (Fredricksen-Goldsen & de Vries, 2019; Fredriksen-Goldsen & Muraco, 2010). In addition, the older LGBT+ people belonged to a generation with very few rights or protection in law for sexual and gender minority people: Non-heterosexual sexual orientation was criminalized and pathologized in many countries. In addition, the relationship between physical activity (PA), older age, and sexual and/or gender minority identities is not documented thoroughly in the literature. Therefore, to our knowledge, the present study represents the first systematic review summarizing existing literature concerning the relationship between PA, LGBT+ identity, and older age.
Previous studies (Fredriksen-Goldsen, 2014; Gorczynski & Brittain, 2016; Hasson et al., 2017) highlighted the need for an LGBT+-focused PA research strategy, implementing the recommendations for physical exercise in older age and reviewing LGBT+ PA research. Consideration needs to be given to some salient factors and historical issues to understand the vulnerabilities of the LGBT+ elderly population and to address their PA levels. General literature is only beginning to understand the experiences and needs of these populations, given that many LGBT+ older adults have spent most of their lives “in the closet”, masking their sexual orientation and/or gender identity (Chandavarkar & Khan, 2015; Rosati et al., 2021a, 2021b).
Overall, the literature suggests that regular PA plays a relevant role in ameliorating health status associated with aging (An et al., 2020; Jakicic et al., 2019), improving physical and mental well-being (Warburton & Bredin, 2017), and increasing resilience to mental health disorders (Richards et al., 2015). PA is described as any body movement caused by the contraction of skeletal muscle, increasing energy expenditure above resting levels (Hasson et al., 2017): Walking, dancing, yoga, and gardening are a few examples of PA. For older people (over 65 years old), the World Health Organization (WHO) recommends a minimum of 150 min of moderate PA and/or 75 min of vigorous PA per week (World Health Organization, 2010). On the contrary, a lack of participation in regular PA is a risk factor for chronic disease, disability (Hasson et al., 2017), cardiovascular and coronary heart disease, type 2 diabetes mellitus (Kesaniemi et al., 2001), cancers, anxiety, and depression (Cary et al., 2016).
Generally, empirical research (Dilley et al., 2010) and scoping review (Kendrick et al., 2021) prove that health disparities between LGBT+ people and cis-heterosexual people may improve by engaging in more regular PA. Indeed, although health disparities between LGBT+ people and cis-heterosexual people are well documented (Baiocco et al., 2018; Fredricksen-Goldsen & de Vries, 2019; Pistella et al., 2018; Scandurra et al., 2017), studies about adherence to PA are limited and present mixed results. Some studies indicated that sexual minority people are less likely to engage in PA than heterosexual counterparts (Abichahine & Veenstra, 2017), while other evidence suggests they perform greater amounts of PA than heterosexual people (Fricke et al., 2019): Puhl et al. (2019) reported that the prevalence of PA is similar among heterosexual and sexual minority individuals.
An interesting systematic review (Fredriksen-Goldsen & Muraco, 2010) represented the first step toward a better understanding of older sexual minority adults from a life-course perspective according to the social contexts in which the research has been conducted. The authors suggested that the initial research on LGB+ aging focused on contrasting negative stereotypes about the accelerated or maladjustment to aging of older lesbian women and gay men due to depression and social isolation. Several studies showed that coming out has left some older LGBT+ adults vulnerable to a potential lack of family, social, and institutional support (Fredriksen-Goldsen & Muraco, 2010; Richard & Brown, 2006; Rosati et al., 2021b).
Many older LGBT+ populations do not access services because of their experiences of discrimination, victimization, and historical and institutional marginalization (Brennan-Ing et al., 2022; Rosati et al., 2021a). Ageism and homo/transphobia further contribute to older LGBT+ adults’ experiences of marginalization and lack of access to supportive services: The ageism and homo/transphobia phenomena are defined as a set of stereotypes, prejudices, or discriminations against people because of their chronological age (Fredricksen-Goldsen & de Vries, 2019; Iversen et al., 2009) and their sexual identity (Baiocco et al., 2020), respectively, and they tend to reinforce social inequalities towards older LGBT+ adults (Rosati et al., 2021a, 2021b).
Regarding psychosocial adjustment to aging in sexual and gender minority people, most research indicated that older LGBT+ individuals had positive psychosocial functioning despite widespread structural inequalities and discrimination (An et al., 2020; Fredricksen-Goldsen & de Vries, 2019; Fredriksen-Goldsen & Muraco, 2010). The resources of the older LGBT+ population are associated with other psychosocial factors that may affect successful aging in older sexual and gender minority adult populations, such as positive identity, socioeconomic resources, access to health care and other formal services, and informal and community-based social support. Indeed, LGBT+ older adults may have had the opportunity to reflect on and process stressful life experiences. They may be more inclined to practice queer generative behaviors aimed at strengthening LGBT+ identities and supporting the sexual and gender minority community (Rosati et al., 2021b).
The Present Study
Decades of research have highlighted the importance of studying an active lifestyle (e.g., physical exercise) as a predictor of aging well, especially in sexual and gender minority people (Slevin, 2010). Successful aging or aging well is defined as the ability to maintain a low risk of disease-related disability, high mental and physical function, and a desire to stay active and healthy in later life (Rowe & Kahn, 1997). Again, aging well “is a dynamic, interactive process that creates long-term, positive change by involving individuals in the physical, social, economic, historical, and cultural contexts of their environments” (Hawkins, 2005; pg 1). To our knowledge, few studies have comprehensively examined PA directly in LGBT+ older adults aged 65 and over. The literature on PA in LGBT+ elderly predominantly focused on discrimination and homo/transphobia in sports-related contexts (Denison & Kitchen, 2015; Fredriksen-Goldsen et al., 2015, 2017; Holder et al., 2022; Mereish & Goldstein, 2020) and PA participation in LGBT+ people compared to their cis-heterosexual counterparts over the lifespan (Cunningham et al., 2018; Kendrick et al., 2021).
However, most studies had some limitations: (a) considering older age when participants are over 50 years old. In the present review, we reported only studies that included older LGBT+ people over 65 years old; (b) focusing on a single combined monolithic group of “LGBT+ older adults”; (c) obscuring the complexities and intersections of age, sexual orientation, and gender identities; (d) considering mainly PA limitations status, i.e., the difficulty encountered by an individual in executing a task or action due to old age symptoms (Jablonski et al., 2013). Based on the limitations mentioned above, the present study focuses on the experiences of PA in LGBT+ older adults (people over 65 years old), considering the different subjectivities regarding sexual orientation and gender identity and analyzing previous qualitative and quantitative studies. Specifically, this systematic review examines the research’s results on older LGBT+ people’s engagement with PA through three main objectives: First, it aims to identify qualitative and quantitative studies published since 1968 on PA in LGBT+ older people through a systemic literature search. Second, it aims to review the qualitative studies on PA in LGBT+ older people, presenting recurring findings by identifying the main research areas. Third, our review seeks to identify research gaps, providing direction for future studies.
Method
Search Strategy
The present systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2015). The articles were identified by searching the following databases: PsychArticles, PsychInfo, Pubmed, and Web of Science. Further studies were identified through hand searches of the reference lists of the included articles, and the grey literature and informational papers were searched on Google Scholar. The investigation was conducted in March 2023, and the search included all original research articles published post-1968. The authors used the Rayyan (2016) software (Ouzzani et al., 2016) to screen articles and conduct a knowledge synthesis study as a suitable checklist for evaluating and controlling the quality of studies.
The exact search term combinations were: (["lesbian*" OR gay* OR homosexual* OR bisex* OR LGB* OR GLB* OR "non heterosexual*" OR "non-heterosexual*" OR "nonheterosexual* OR "sexual minorit*" OR transgender* OR transsex* OR "female-to-male" OR "male-to-female" OR "trans female" OR "trans wom*" OR "trans male" OR "trans man" OR "trans men" OR "trans people" OR "trans person*" OR "trans individual*" OR "trans-sexuality" OR transvestite OR nonbinary OR non-binary OR "non binary" OR "gender non-conforming" OR "gender nonconforming" OR "gender non conforming" OR queer OR genderqueer OR gender-queer OR "genderfluid" OR gender-fluid OR "gender fluid" OR pangender OR agender OR demi-gender OR demigender OR bigender OR trigender OR "gender varian*" OR "gender divers*" OR gender-divers* OR "gender creativ*" OR "gender minorit*"] AND ["elder* OR aged OR older* OR geriatric* OR "65+" OR "over 65"] AND ["sport* OR "physical activit*" OR exercis*]). They were all placed within titles and abstracts to retrieve extensive data.
Study Screening Selection
Language filters were applied to the databases to limit the search to studies reported in only English, French, German, Italian, Spanish, and Portuguese. Since the review focused on older LGBT+ adults, studies involving participants over 65 years old were included. Original research articles published in scientific journals, pure qualitative studies, studies involving clinical samples, books, book chapters, and grey literature were included in the systematic review. To our knowledge, only a scoping review (Kendrick et al., 2021) explored the internal psychological obstacles that gay men in middle-older age encounter in participating in PA. No other studies directly examined the association between PA, older age, and LGBT+ identity.
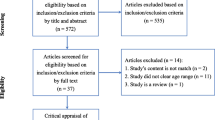
The present review included studies that met the following criteria: (a) consisted of a sample of LGBT+ older individuals over 65 years old, (b) the variable analyzed was PA and sport environment; (c) the research design was either cross-sectional/comparative, cohort/longitudinal, qualitative, or quantitative. When results appeared vague, the researchers contacted the authors (n = 19) to clarify their results, differentiating for participants’ age and sexual identity (n = 4 responded). Without a response, the relevant studies were inserted specifying “regardless of age,” or they were omitted. Figure 1 displays the PRISMA flowchart of the systematic review process.
Data Extraction and Qualitative Analysis of the Publications
The primary articles were screened, and the studies were extracted from databases via the Rayyan tool (Ouzzani et al., 2016) according to the inclusion criteria. The following information was independently extracted using a structured template: author(s), year of publication, country, study design, participant age, sexual orientation and/or gender identity, sample size, measures of PA, and measure of PA used. Coding disagreements were resolved through discussion between the first two reviewers. Cohen's kappa coefficient, calculated to assess inter-rater reliability, was 0.92, reflecting very high agreement. The other authors resolved any discrepancies (Table 1).
We used STROBE (Strengthening The Reporting of Observational studies in Epidemiology) to evaluate the quality of the selected studies (Vandenbroucke et al., 2007). Specifically, we obtained the STROBE results for each study, where the publications that included 0–7 items were considered low quality, 8–14 items were intermediate quality, and 15–22 items were high quality. To summarize the main findings of the different publications, we performed a qualitative analysis to find the prevalent research areas. In the process, we followed three steps: (a) the first and second authors independently open-coded the articles into one research area (i.e., discrimination and homo/transphobia in sport-related contexts); (b) the same authors compared the identified research areas and created a set of shared categories; (c) all authors discussed (over several meetings) the research areas emerged, and in some case, redefined the categories as presented in the manuscript’s final version. We presented details about the research (i.e., country), sample size, mean age, LGBT+ identity, and the STROBE results in Table 2, 3, 4, 5, and 6.
Results
In total, 887 articles pertaining to PA in older LGBT+ people were identified: 411 from PsychArticles and PsycInfo, 99 from Pubmed, 345 from Scopus, and 32 other records were added through other sources. After the 115 duplicates were removed, the titles and abstracts of selected articles were screened based on the inclusion criteria: 714 records were excluded due to failure to meet all necessary criteria. Accordingly, 58 papers met the inclusion criteria; only 53 articles were included in the review (see Fig. 1 for reasons to exclude the five articles). Although the search included works published between 1968–2023, the present review was restricted to 1986–2023 because no articles published before 1986 met the inclusion criteria. The final selection comprised qualitative (n = 6) and quantitative (n = 32) research, systematic or scoping review (n = 5), intervention sessions implementation (n = 3), commentary (n = 3), survey report (n = 2), book reviews (n = 1) and podium presentation (n = 1).
Regarding the study characteristics, LGBT+ sample sizes ranged from 10 (qualitative research) to 7,927 LGBT+ individuals. Participant ages were also heterogeneous, though predominantly falling within the youngest-old age range (65 and 74 years). The studies were conducted in different countries: 74% in the United States (n = 39), 7% in Canada (n = 4), 13% countries in Europe (i.e., 1 in Italy, 1 in New South Wales, 1 in Portugal, 1 in Spain, 1 in Sweden, and 2 in the UK), 4% in Australia (n = 2), and 2% in Brazil (n = 1). No studies were conducted in Asia. In addition, analyzing the 22 items proposed in STROBE, we found that the number of covered items varied from 6 to 20. Specifically, 28 studies were classified as intermediate quality, 18 as high quality, and only one publication was classified as low quality (see Table 2, 3, 4, 5, and 6 for more details). In comparison, the STROBE evaluation was not applicable for 6 studies (commentaries and article reviews) due to the lack of qualitative or quantitative design strategies.
The articles were categorized according to participants’ sex assigned at birth, gender identity, and sexual orientation and based on the studies’ numerosity. Sex assigned at birth (i.e., biological sex) means the male, female, or intersex designation that doctors ascribe to children based on genitalia and is marked on their birth records. Gender identity is a person’s internal sense of whether they are a man, a woman, or gender-diverse. Sexual orientation refers to an enduring pattern of emotional, romantic, and/or sexual attraction to men, women, both, or other genders, which encompasses identities such as heterosexual, lesbian, gay, bisexual, pansexual, asexual, or queer. Thus, our findings are presented separately for (1) sexual minority (LGB+) identities (n = 17); (2) sexual and gender minority (LGBT+) identities (n = 15); (3) transgender and gender-diverse identities (n = 8); (4) gay and bisexual male identities (n = 7); and (5) lesbian and bisexual female identities (n = 6).
Specifically, intersex identities were included in the LGBT+ identity category. Transgender and gender-diverse identities were comprised in (a) transgender and gender-diverse identity category and (b) LGBT+ identity category when the study considered a monolithic sexual and gender minority category. Sexual minority people were involved in all identity categories (LGB+, LGBT+, gay and bisexual male identities, and lesbian and bisexual female identities) except transgender and gender-diverse identity category. Table 1 presents the studies’ categorization according to participants’ identity categories and the research areas indagated (n = 53).
LGB+ Identities (n = 17)
Of the seventeen papers identified as relevant to PA in older sexual minority people (LGB+), thirteen were cross-sectional quantitative research designs (one dissertation, one longitudinal study, and one research project report), one systematic review, one article review, and two qualitative studies. Thirteen papers originated from the USA and Canada, one from Australia, one from Sweden, one from Italy, and one from Portugal. Only six papers reported exclusively on older LGB+ people, and the remaining papers reported the age range, including older participants.
Four papers focused on PA in the elderly LGB+ population and its associations with mental health. Six works identified the adverse effects of minority stressors on psychological and physical health, including discrimination, homophobia, and lack of PA in LGB+ people. Finally, seven empirical studies investigated differences in health outcomes and PA between sexual minority people and heterosexual counterparts. One relevant quantitative work was excluded because the authors did not provide data on PA, sexual orientation, and age (Adzrago et al., 2022). We found three mean research areas (Table 1 for the research areas and Table 2 for studies details): (a) discrimination and homophobia in sport-related contexts (n = 7); (b) differences between LGB+ and heterosexual people (n = 6); (c) physical activity and aging well (n = 4).
Discrimination and Homophobia in Sport-Related Contexts
Some studies (Caceres et al., 2017; Denison & Kitchen, 2015; Fredriksen-Goldsen et al., 2013; Grossman et al., 2001; Mereish & Goldstein, 2020) have identified the adverse effects of minority stressors on physical and mental health, including lack of PA and cardiovascular disease risk in LGB+ people. A systematic review (Caceres et al., 2017) that compared cardiovascular disease risk between sexual minority individuals and heterosexual adults highlighted that adverse social factors seem to exert a negative effect on chronic conditions and cardiovascular disease risk, especially among sexual minority people. Even if few sexual orientation differences were found for PA, results suggest that insufficient exercise and poor dietary habits significantly increase cardiovascular disease risk in older adults.
Similar to successive research results (Pharr et al., 2021), Mereish and Goldstein (2020) demonstrated that, regardless of age, gender, and sexual orientation, only 65% of 670 sexual minority participants (18–76 years old; M = 41.1, SD = 14.7) engaged in regular exercise. Minority stressors were not directly linked with the cardiovascular disease risk index. However, proximal stressors (e.g., internalized sexual stigma) are directly associated with lower odds of reporting regular exercise and indirectly related to more excess body fat and less reporting of regular exercise. Distal minority stress (e.g., discrimination) was directly associated with a lower likelihood of reporting regular exercise among sexual minority women. Thus, these findings indicated that both minority stressors were associated with less PA and proximal stress was associated with more significant excess body fat.
Rosati et al. (2021a), using semi-structured interviews with 23 older lesbian women and gay men over 60 years, confirmed the association between low levels of PA and expectations of discrimination in a homophobic environment such as sports-related contexts. Concerning participants’ actual experiences of discrimination, older lesbian women and gay refer to an explicit form of negative attitude and rejection exercised by some sports environments and linked to participants’ sexual identity, especially for the subgroup of seropositive persons. Indeed, participants who are HIV + experienced the first wave of the HIV/AIDS epidemic, representing the only sub-group in this study who reported explicit experiences of discrimination in sports environments and medical contexts.
Discrimination and homophobia were investigated in other international works. For example, Out on the Fields (Denison & Kitchen, 2015) is the largest (n = 9,494) and the first international study on homophobia in sports-related contexts. Research report findings suggest that homophobia is widely experienced around sports across the English-speaking world by people of all ages, sexual orientations, and gender identities: 80% of all participants have witnessed or experienced homophobia in sports. Younger participants were likelier to report personal experiences with victimization homophobia than older participants in sports-related contexts, potentially because they are more likely to be at least partially out of the closet. Indeed, younger participants were more likely to be out of the closet while playing in their youth than previous generations were. However, participants of all ages said they kept or continue to keep their sexuality secret while playing youth and adult team sports. Thus, older individuals, regardless of gender, reported less victimization and higher levels of internalized sexual stigma than their younger counterparts. The results align with Grossman and colleagues’ previous research (2001), showing that more than half (57%) of 416 older LGB adults exercised regularly, 27% sometimes, 12% seldom, and only 4% never.
Another research involving 2,439 older LGB adults over 50 years old (Fredriksen-Goldsen et al., 2013) revealed that lifetime victimization, obesity, and lack of PA among older LGB adults are significant predictors of health outcomes, such as poor general health, disability, and depression, even after adjusting for background characteristics and other covariates (e.g., socioeconomic status). Bisexual older women also reported lower rates of PA and less social support than older lesbian women, even if they showed a higher degree of lifetime victimization than bisexual older women. There was no significant difference between sexual minority women and men in PA levels.
Societal weight stigma is another relevant topic: Such stigma includes negative weight-based stereotypes, prejudice, discrimination, and unfair treatment in multiple life domains, including employment, health care, and sports-related contexts: Despite elevated rates of overweight and obesity among some groups of sexual minority people, quantitative research examining weight stigma in older LGB+ people scarce. Puhl et al. (2019) assessed weight stigma and weight-related health correlates in sexual minority people engaged in weight management compared with a matched heterosexual sample (M = 48.4, SD = 13.8). The final model examining PA yielded no significant difference in participants' sexual orientation: In line with successive research results (von Humboldt et al., 2021), only 35% of participants were physically active (considering the frequency with which individuals engage in mild, moderate, or strenuous exercise in a given week), and the prevalence is similar among heterosexual and sexual minority individuals.
Differences Between LGB+ and Heterosexual People
Literature on sexual orientation differences in PA found mixed results. Four studies involving LGB+ participants did not find differences between sexual minority people and their heterosexual counterparts (Dilley et al., 2010; Nelson, 2021, 2023). Nelson’s Ph.D. dissertation thesis (2021) and subsequent publication (2023) provided data on different ages and sexual orientations, indicating no significant differences among over 65 LGB people (n = 40) and their heterosexual older counterparts (n = 86) in PA, not even between participants younger than 60 (LGB: n = 115; heterosexual: n = 221). Data from the Washington State Behavioral Risk Factor Surveillance System to examine associations between sexual orientation and health risk behaviors (Dilley et al., 2010) found that lesbian (n = 589), bisexual (n = 561), and heterosexual women (n = 47,505) had similar odds for insufficient PA. Gay men (n = 498) were significantly less likely than heterosexual men (n = 30,112) to be overweight but had similar odds for insufficient PA. Compared with heterosexual men, bisexual men (n = 235) had twice the odds of inadequate exercise. Results were obtained adjusting for age.
Only two studies suggest that sexual minority people are less likely to engage in PA than heterosexual people (Abichahine & Veenstra, 2017; Lindström & Rosvall, 2020). Specifically, using an intersectional approach in a sample of 2,526 LGB people compared to 147,048 heterosexual individuals (Abichahine & Veenstra, 2017), it emerged that a sexual minority orientation is associated with a greater likelihood of regular PA among women, significantly less educated women of all ages but not among sexual minority men. Thus, less-educated lesbian or bisexual women are much more likely, and well-educated gay or bisexual men are much less likely to be physically active.
The percentages of exercise in heterosexual people and sexual minority people are also observed in another quantitative study (Lindström & Rosvall, 2020). The prevalence of regular PA in a sample of 23,585 respondents (3.8% and 3.9% sexual minority men and women, respectively) was higher among heterosexual men compared to sexual minority men: In particular, after adjusting for age (18–80 years old), 86.1%% of heterosexual men engaged in regular exercise versus 80.5% of gay men, 73.9% of bisexual men, and 73.4% of other sexual minority men. The prevalence of PA was 87.7% among heterosexual women, 81.5% among bisexual women, 84.4% among lesbian participants, and 81.5% among other women. In bivariate logistic regression analyses considering the age-adjusted model, low regular exercise was positively and significantly associated with bisexual identity and older age among men and women.
One longitudinal paper reported instances where some sexual minority people perform more significant amounts of PA than their heterosexual counterparts (Fricke et al., 2019). Data on 42,534 participants aged 20 – 80 compare PA patterns among sexual minority individuals and heterosexual people. Results showed that, regardless of age, sexual minority women engage in PA more frequently, for more minutes per week on average, and at higher levels of intensity than heterosexual women. Compared to heterosexual men, sexual minority men engage in PA more frequently, for fewer minutes per week on average, and at lower intensity levels. However, there was no difference by sexual orientation in the odds of meeting CDC (2011) PA recommendations.
Physical Activity and Aging Well
Overall, articles review (Cruikshank, 1991) and empirical studies (Pharr et al., 2021; Slevin, 2010; von Humboldt et al., 2021) involving LGB+ participants point out that an engaged lifestyle (e.g., physical exercise) represents a relevant predictor of aging well. In work comprising interviews with 57 sexual minority men and women aged 60 to 89 (Slevin, 2010), many interviewed engage in some form of physical exercise or activity – illustrating the increasingly ageless obligation to maintain fit and trim bodies. Sometimes, exercise takes the form of regular walks or running; for other participants, gym memberships provide a venue for regular exercise. Some interviewers are involved in more than 40 min of exercise every day: Almost half of them were regular exercisers in the form of running, walking, swimming, and workouts in the gym. For a few, golf and sailing are mentioned as forms of exercise – illustrating the importance of financial means to keeping active. Several respondents say gay men age better than heterosexual men because they focus more on keeping youthful bodies through exercise and discipline. Gay men are also more likely than heterosexual men to favor cosmetic intervention. Exercising, dieting, cosmetics, and cosmetic surgeries are cultural strategies of action to resist growing old. These strategies emphasize being fit, staying young, or not looking old.
Evidence concords to suggest that LGB adults who participated in any exercise reported almost less poor mental health than LGB adults who did not exercise. For instance, in a study involving 6,371 LGB participants (1,062 participants over 65; 8%), it emerged that older participants reported fewer days of poor mental health compared to younger individuals and that PA decremented with age (Pharr et al., 2021): 75% of LGB participants of all ages reported doing some exercise in the past month, while 40% of them did not meet either exercise guidelines. The work of von Humboldt et al. (2021) found a lower percentage of PA in the older LGB population using a sample of 287 community-dwelling older LGB adults aged 75 years and older from three different nationalities (Brazilian, English, and Portuguese): Only 34% of older sexual minority people were involved in regular PA.
LGBT+ Identities (n = 15)
Of the fifteen papers focused on LGBT+ people and PA, nine utilized quantitative surveys (three longitudinal, six cross-sectional), three reported commentary, two qualitative studies (including an intervention session), and one systematic review. Eleven papers originated from the USA and Canada, and one each from Brazil, England, Spain, and New South Wales. Six papers reported exclusively on older LGBT+ people; the remaining works included the age range comprising older sexual and gender minority people. However, the limitation of some studies on the LGBT+ population regards the age range considered. Indeed, in many studies, participants are considered older if over 50 years old. Most research on the elderly population evaluated older participants over 65 years old. However, given the lack of studies on older LGBT+ people, we included these empirical articles.
Seven papers reported discrimination and homo/transphobia associated with PA levels, and two articles analyzed the lifestyles during the Covid-19 pandemic. Only one research compared LGBT+ people and cis-heterosexual counterparts in PA. At the same time, other works included an interventions section in the older LGBT+ population, and commentary highlighted the relevance of PA in older age. One relevant quantitative work was excluded because the authors provided data on age, and the number of participants over 65 years old was just (Úbeda-Colomer et al., 2020).
We found four mean research areas (Table 1 for the research areas and Table 3 for studies details): (a) discrimination and homo/transphobia in sport-related contexts (n = 7); (b) the needs and competent interventions for an LGBT+-focused physical activity research strategy (n = 5); (c) physical activity during the Covid-19 pandemic (n = 2); (d) differences between LGBT+ and cis-heterosexual people (n = 1).
Discrimination and Homo/Transphobia in Sport-Related Contexts
Regarding discrimination and homo/transphobia in sports-related contexts, cross-sectional research (Devís-Devís et al., 2022) analyzed harassment disparities within 1,051 LGBT+ Spanish adults (aged 18 to 74), considering different contexts of perpetuation. Significant harassment disparities were found by age: Younger participants suffered more harassment (61%) than the older group (44%). In addition, regardless of age, the non-binary group had the highest probability of suffering harassment in the sports context, followed by transgender women and gay men: Thus, more non-binary and transgender people experienced harassment than cisgender people in the LGBT+ community.
Higher levels of negative attitudes towards sexual and gender minority people and older age in sports-related contexts may be explained by a conspicuous absence of explicit images of LGBT+ people, aging bodies, overall representation of non-normative bodies, and a lack of diversity in types of PA modalities. Griffin et al. (2022) used an intersectionality framework to explore 141 online posts using reflexive thematic analysis. Results showed that fitness and sports magazines are dominated by cisgender, heterosexual, young, white, tall, thin, seemingly affluent, happy, and able-bodied representations. Meanwhile, LGBT+ identities, aging, black, fat, and disabled bodies are nearly absent. A similar focus on appearance-related benefits and objectification of body parts can potentially have (unintended) negative consequences on the well-being of older sexual and gender minority people in sports-related contexts.
The role of discrimination in PA was also examined in other studies (Fredriksen-Goldsen et al., 2015, 2017, 2023b). After controlling for background characteristics (Fredriksen-Goldsen et al., 2023b) and using a sample of 754 LGBT+ caregivers (aged 50–98), results found that: (a) PA was positively associated with psychological health; (b) discrimination, identity stigma, and insufficient food intake were negatively related to the quality of life. PA slowed down the decline of physical and psychological health-related quality of life over time. These results were previously obtained by Fredriksen-Goldsen and colleagues using a cross-sectional research design (n = 2,463; age range: 50–80 and older; Fredriksen-Goldsen et al., 2015) and longitudinal data from 2014 (n = 2,415; age range: 50–98 years; Fredriksen-Goldsen et al., 2017).
Regarding health-promoting behaviors, the rates of PA for the young–and middle–old groups are higher than that for the old–old-age group. The middle–and old–old age groups are more likely to be engaged in leisure activities than the young–old age group (Fredriksen-Goldsen et al., 2015, 2017). Similar results were obtained in a previous research report on 312 LGBT+ people aged 50 and over (Hughes & Kentlyn, 2014): Health concerns included lack of exercise, memory loss and dementia, dental health, heart disease, loneliness, and anxiety and depression. PA was more problematic for the older group in the sample (those aged 65 +) than for the younger group, whereas the reverse was the case for anxiety and depression.
Thus, physical health is negatively associated with lifetime victimization and discrimination and positively related to PA, leisure activity, and being male (Fredriksen-Goldsen et al., 2015, 2017). One interesting work focused on homo/transphobic discrimination and cognitive impairment in sexual and gender minority older adults highlighted the relevance of exercise and PA in this at-risk population. In a podium presentation, Kim et al. (2022) presented data on 855 older sexual and gender minority people who self-reported having cognitive impairment. Results found that homo/transphobic discrimination, victimization, and identity stigma were associated with lower physical and psychological health-related quality of life. In contrast, PA, outdoor leisure activity, and social network size were positively related to physical and psychological health-related quality of life.
The Needs and Competent Interventions for an LGBT-focused Physical Activity Research Strategy
Thus, three commentaries introduce the need for an LGBT-focused PA research strategy, highlighting the recommendations for PA in older age and reviewing LGBT+ PA research. Indeed, the USA Department of Health and Human Services recommends that adults and older adults perform moderate- or high-intensity muscle-strengthening activities that involve all significant muscles two days/per week (Gorczynski & Brittain, 2016). Despite the known benefits of PA participation, many people in the United States remain inactive (Hasson et al., 2017).
More specifically, PA behavior is socially patterned with lower participation rates among women; racial/ethnic minorities; sexual minority youth; individuals with older age, sexual and gender minority people, persons with physical, mental, and cognitive disabilities, and those living in the southeast region of the United States. Another article commentary (Fredriksen-Goldsen, 2014) incorporates historical and changing social context to address the unique health and aging needs of LGBT+ mid-life and older adults through services, policy, socialization contexts, and research innovations. This commentary analyzed the health disparities of LGBT+ mid-life and older adults through a health-equity perspective.
Culturally competent interventions to improve the quality of life of older LGBT+ people have been an explored topic in the last year. A recent systematic review (Freedman & Nicolle, 2020) compared interventions to address social isolation, loneliness, and social vulnerability in older adults and the associated risks, recommending effective interventions and improving PA and exercise. The research’s conclusions suggested that the needs of underserviced and marginalized populations, including older adults identifying as LGBT+, as well as the needs of long-term care residents and older caregivers, require further evaluation. Fredriksen-Goldsen et al. (2023a) designed and developed the first randomized controlled trial of a culturally enhanced intervention (IDEA) for sexual and gender minority older adults living with dementia and care partners. The primary goal was to increase the physical functioning of LGBT+ older adults, improving PA, i.e., the number of days of aerobic exercise at least 30 min per week, and promoting intervention adherence.
Physical Activity During the Covid-19 Pandemic
Again, considering the quantitative research design, two papers analyzed the factors associated with deteriorating lifestyles during the Covid-19 pandemic, including PA in sexual and gender minority people (LGBT+). Of the 975 LGBT+ participants of all ages (18–50 and older; Braga et al., 2022), 49% decreased PA, 6% increased cigarette smoking, and 17% increased alcohol intake during the Covid-19 pandemic. A higher frequency of deterioration in practicing regular PA was found in sexual minority cisgender women (53%) and individuals 50 and over age groups (54%), while the other sexual (e.g., gay men, cisgender sexual minority men) and gender minority identities (e.g., transgender, non-binary or other gender minorities) percentages were below 50% of physical inactivity.
Another exploratory study (Marmo et al., 2021) utilized a cross-sectional survey design to examine participation in Senior Center programming of 113 LGBT+ over 60 adults. Specifically, during the Covid-19 pandemic, 52% of LGBT+ Senior Center participants engaged in virtual fitness programs and physical exercise (e.g., yoga, movement, general fitness, and diverse dance classes). Participants who reported they engaged in exercise and fitness programming had higher scores on well-being scales and lower mean scores for depression and anxiety when compared to those who did not engage in these activities.
Differences Between LGBT+ and Cis-Heterosexual People
To our knowledge, only one research directly compared LGBT+ people and cis-heterosexual counterparts. Results reported instances where some sexual minority people (15,824 LGB+ individuals aged 21- 65 and older) perform more significant amounts of PA than their heterosexual counterparts, regardless of age (Cunningham et al., 2018). Compared with heterosexual men, gay men were more likely to perform any leisure time exercise (82% versus 78%).
A similar pattern emerged in lesbian women (81%) compared to heterosexual women (74%). Regarding gender identity (3,415 gender minority people, aged 21- 65 and older), the prevalence of performing any leisure-time exercise was higher among cisgender adults (76%), transgender men (69%), and gender nonconforming (72%) than among transgender women adults (56%). In addition, transgender women adults had a lower prevalence of engaging in health-related behaviors (12%) than cisgender adults (19%), showing that they may be considered an at-risk population.
Transgender and Gender-Diverse Identities (n = 8)
Of the eight papers identified as relevant to PA in older transgender and gender-diverse populations, seven utilized surveys and one qualitative study through interviews. Seven papers originated from the USA and Canada, and one from Australia. Only one paper reported exclusively on older gender minority people (even if participants were over 50 years old), and the remaining papers reported on gender minority people generally, but the age range included older transgender, gender non-conforming, or non-binary participants.
Four articles reported less engagement with PA than age-matched cisgender people, two investigated exercise as an indicator of disordered eating behaviors, and one stated no average difference between transgender people and cisgender counterparts. Finally, one qualitative research investigated the role of the feminine/masculine voice in transgender women engaged in different sports activities. Two relevant quantitative works were excluded because the authors did not provide data on PA, gender identity, and old age (Bolijn et al., 2020; Newby et al., 2020).
We found four mean research areas (Table 1 for the research areas and Table 4 for studies details): (a) differences between transgender and cisgender people: eating behaviors/obesity (n = 3); (b) differences between transgender and cisgender people: cardiovascular diseases and cancer (n = 3); (c) physical activity during the Covid-19 pandemic (n = 1); (d) narratives of transgender women in sports related contexts (n = 1).
Differences Between Transgender and Cisgender People: Eating Behaviors/Obesity
Thus, previous research demonstrated that transgender older adults, regardless of gender, were less likely to be engaged in regular PA than the nontransgender older adult participants (Fredriksen-Goldsen et al., 2014). In addition, the study’s results (Fredriksen-Goldsen et al., 2014) showed that lowered PA levels were associated with higher rates of obesity and poor physical and mental health among 174 transgender older adults (Mage = 66.0; SD = 9.1). Generally, obesity is associated with low levels of PA and increases the risk of other adverse health outcomes, such as diabetes and coronary heart disease.
Eating disorder attitudes and disordered eating behaviors represent a significant area investigated among transgender and gender-diverse people using longitudinal research design (Nagata et al., 2020a; Uniacke et al., 2021). Specifically, in a sample of 287 transgender and gender nonbinary people (Uniacke et al., 2021), 7% of the participants reported compulsively exercising during the prior month, and 3.5% endorsed ≥ 4 episodes. This pattern is consistent with previous findings by Nagata et al. (2020a) that documented rates of objective binge episodes of 11% and 13% in transgender men and women, respectively. In addition, 8% of participants endorsed compulsively exercising at least 20 days during the past month. These results were obtained using a large-scale national longitudinal cohort study comprising 312 transgender men and 172 transgender women (age range 18–74). The evaluation of disordered eating behaviors remained relatively high among transgender participants of all ages.
Differences Between Transgender and Cisgender People: Cardiovascular Diseases and Cancer
Cardiovascular disease is another topic explored in transgender and gender-diverse populations. A study (Downing & Przedworski, 2018) used the most comprehensive sample of 1,772 transgender people, 449 gender non-conforming individuals, and 523,080 cisgender respondents (age 18-over 65; 17% over 65 participants) in the USA from 31 states and one territory (Guam). Interestingly, after controlling for age, transgender men had higher odds of no exercise and cardiovascular disease than cisgender males and cisgender females.
Again, gender non-conforming people had higher odds of no PA than cisgender men. Malhotra et al. (2022) found that the prevalence of cardiovascular disease (13.5%) was noted to be similar among 378 transgender women, 394 transgender men, and 247 gender non-conforming (aged 18–65). In addition, participants with cardiovascular disease were older, with lower rates of regular exercise and higher rates of smoking and chronic medical comorbidities. These findings identified that older age and low PA predict cardiovascular disease in transgender and gender-diverse people.
Only one paper reported no PA difference between transgender men/women and cisgender people using a sample of 950,811 participants who self-reported a cancer diagnosis (Boehmer et al., 2020). Results showed that gender non-conforming survivors (n = 876), but not transgender men (n = 1344) and transgender women (n = 1,877), have a greater likelihood of physical inactivity compared with cisgender men (n = 410,422) and cisgender women (n = 540,389). Consistently, research has suggested that gender-nonconforming survivors are an at-risk group in urgent need of complex interventions to reduce alcohol use, physical inactivity, and depression.
Physical Activity During the Covid-19 Pandemic
One research investigated mental health outcomes and PA in the general population during the Covid-19 pandemic. Tessier et al. (2023) found that body image dissatisfaction was also more frequent in gender minority people and cisgender women compared to cisgender men, which is typically observed in Western societies (Barnes et al., 2020). Evidence supports that individuals dissatisfied with their body image may engage in less healthy lifestyle behaviors, such as decreased PA. In addition, results showed that self-identifying as a gender minority was associated with adopting less healthy lifestyle habits. However, this group’s sample size was small: of 1,609 participants aged 18–89 (M = 40.2; SD = 15.5), only 24 (1.2%) self-identified as a gender minority, although the proportion was comparable to that reported in the previous research (Boehmer et al., 2020; Downing & Przedworski, 2018).
Narrative of Transgender Women in Sports Related Contexts
Finally, a qualitative study on twenty transgender women (aged 16–65) provided narratives of older people on PA (Stewart et al., 2020). Transgender women predominately engaged in female-only sporting environments and experienced anxiety because they had to ensure that they maintained their “female” communication: The participants shared that this was because they perceived that if their voice sounded masculine, they would be rejected by fellow females. They were concerned that those with whom they identified would not accept them. Specifically, Katie, a 65-year-old transgender woman, reported: "My voice is pretty much one of the main reasons I am accepted or isolated […] I did not really think of my voice really being that big of importance that it is in sport, you know? But sport is very clearly either male or female, and if your voice does not match that, it is pretty obvious” (Stewart et al., 2020, pg. 83).
Gay and Bisexual Male Identities (n = 7)
Of the papers identified that were relevant to PA in older gay men (n = 4) and older gay and bisexual men (n = 3), two utilized quantitative cross-sectional surveys, one a quantitative longitudinal study, two qualitative research, one scoping review, and one applied interventions sessions including PA. Six articles originated from the USA and one from England. Two papers reported exclusively on older gay men, and the remaining papers focused on gay and bisexual men generally, including over 65 participants.
Two articles reported less engagement with PA than age-matched heterosexual men, three suggested that sexual minority men perform greater exercise than their heterosexual counterparts, and one stated no average difference between gay/bisexual men and heterosexual men. Finally, one quantitative study highlighted the relevance of fitness engagement to ameliorating negative self-appraisals concerning body image and aging. One book chapter was not included because the authors did not provide specific data (Mitchell et al., 2019). We found two mean research areas (Table 1 for the research areas and Table 5 for studies details): (a) differences between gay men/bisexual men and heterosexual men (n = 5); (b) body image and aging (n = 2).
Differences Between Gay Men/Bisexual Men and Heterosexual Men
In a scoping review, Kendrick et al. (2021) found 23 papers that underlined the internal psychological obstacles that middle-older gay men encounter in participating in PA: Older gay men faced considerable challenges, having lived through times when homosexuality was less accepted than it currently is, regardless of geographical location (Fredricksen-Goldsen & de Vries, 2019). In addition, this scoping review provides mixed evidence for lower participation in PA in gay men compared to their heterosexual counterparts over the lifespan. However, there is a lack of information regarding PA in older gay men, especially those aged 65 and over. Compared with this previous scoping review (Kendrick et al., 2021), we did not include papers regarding general homophobia in sports-related contexts, PA limitation attributable to a physical, mental, or emotional disability, and studies with participants under 65 years old.
Evidence of adherence to PA by older gay men appeared to be mixed. Some studies (Bourne et al., 2017; Kendrick et al., 2021) suggested that gay and bisexual men of all ages perform less PA than the average population. Specifically, Bourne et al. (2017) reported that only 62% of gay and bisexual men were physically active (for 30 min or more on fewer than five days per week) and that the proportion of overweight increased successively with age. Only one paper reported no PA difference between older gay and heterosexual men (Slevin, 2008), using interviews with fifty-two gay and heterosexual men.
Some papers reported instances where gay men perform more PA than their heterosexual counterparts (Lightner et al., 2020; Zhang et al., 2017). In 2017, Zhang and colleagues developed a physical-activity intervention concerning the number of days people did vigorous-intensity aerobic activities for at least 20 min moderate-intensity aerobic activities. The participants were 503 African American men 18 to 69 (M = 41.6; SD = 10.7), of whom 41% self-identified as gay men and 41% as bisexual men. Results showed that the physical-activity intervention increased the weighted average number of days of overall PA and the average number of days of aerobic physical exercise, vigorous-intensity activity, and moderate-intensity activity, especially in sexual minority men. In addition, older men were more likely to return than younger men. Sexual minority participants were closer to meeting the muscle-strengthening guideline at baseline than heterosexual ones.
Similar results were obtained in the study of Lightner et al. (2020). Specifically, in a sample of 29,926 heterosexual men, 623 gay men, and 162 bisexual men (aged 18–85 years old), it emerged that gay men who were coupled were more likely to be active and to meet muscle-strengthening recommendations than heterosexual-coupled men. Adjusted odds ratios showed no significant differences in PA between coupled bisexual and heterosexual men. The results of these studies (Lightner et al., 2020; Slevin & Linneman, 2010; Zhang et al., 2017) may reflect gay and bisexual men’s desire to appear physically attractive and masculine.
Body Image and Aging
Substantial data in older sexual minority men demonstrates that PA could play an essential role in facilitating many aging-related health conditions. For instance, in a sample of 1,026 men who have sex with men (average age was 60 years), Brennan-Ing et al. (2022) found that, regardless of HIV serostatus and age, fitness engagement is positively associated with community connections and helps to ameliorate negative self-appraisals concerning body image and aging. This study supports the relevance of gay men community connections among aging sexual minority men through intervention programs and services that have the potential to support psychological well-being in this population, reducing loneliness and social isolation and thereby promoting healthy aging.
A desire to be physically attractive was listed as a motivating factor in performing PA in older age through intensive interviews with ten gay men ages 60–85 (Slevin & Linneman, 2010). Gay culture reinforces hegemonic masculinity, and old gay men interviewed talk about how gay men age better than heterosexual men because they pay more attention to keeping youthful bodies through exercise and disciplining them. Ageism and the emphasis on attractiveness are pervasive and culturally relevant factors shaping sexual minority men’s social experiences in the gay community.
Lesbian and Bisexual Female Identities (n = 6)
Of the six papers relevant to PA in older lesbian and bisexual women, two utilized quantitative surveys, two systematic or article reviews, and one focused on a funded program to promote healthy weight. The only study on bisexual participants used a cross-sectional survey design. All articles originated from the USA, and no studies reported specific age differences, distinguishing younger, middle, and older age. Quantitative studies did not report average discrepancies between sexual minority females compared to other sexual orientation participants. We found two mean research areas (Table 1 for the research areas and Table 6 for studies details): (a) differences between lesbian women/bisexual people and heterosexual counterparts (n = 4); (b) healthy-weight interventions (n = 2).
Differences Between Lesbian Women/Bisexual People and Heterosexual Counterparts
Kehoe (1986), in a not recent qualitative paper collecting narratives of old lesbian women, suggested that PA may be just as important: Old lesbian women may be more physically active than heterosexual women, from lifelong habit, partly because some held non-traditional jobs requiring physical labor. One article (Nagata et al., 2020b) dealt with only lesbian participants, assessing eating disorder attitudes and disordered eating behaviors among 563 self-identified cisgender lesbian women ages 18–77 (Mage = 38.0, SD = 14.3). Findings highlighted that age negatively correlated with episodes of excessive exercise (r = –0.11), even if, regardless of participants’ age, 5% percent of lesbian women reported excessive activity at least once a week in the previous 28 days. The same percentage of excessive exercise was reported in another study (Nagata et al., 2021) involving bisexual women (n = 462: ages 18–71, Mage = 32.0, SD = 9.4) and bisexual men (n = 93: ages 20–76, Mage = 38.0, SD = 12.8) compared to heterosexual women (n = 723) and heterosexual men (n = 404). Interestingly, a higher percentage of heterosexual women reported any occurrence of excessive exercise than bisexual women, while no significant differences were observed between bisexual and heterosexual men.
Regarding the studies involving lesbian and bisexual women (Fogel et al., 2016; Hutchcraft et al., 2021; Rizer et al., 2015), only once was quantitative in nature. Hutchcraft et al. (2021) reported detailed differences in health behaviors (including tobacco and alcohol use, PA, and preventive health care) in a sample of heterosexual (n = 10,830), lesbian (n = 141), and bisexual (n = 95) women cancer survivors ages 18–85. After controlling for age, a multivariable logistic regression showed that lesbian and bisexual women cancer survivors did not report lower odds of PA compared to heterosexual women.
Healthy-Weight Interventions
The other studies involving lesbian and bisexual women focused on the design of healthy-weight interventions in lesbian and bisexual women in middle-older age, given that evidence showed the highest obesity prevalence occurred among lesbian and bisexual women aged 60 and older. Rizer et al. (2015) systematically reviewed health interventions to reduce overweight and obesity in older lesbian and bisexual women through increased PA and improved nutrition. Five interventions were identified; only one involved PA in a sexual minority female population (Brittain & Dinger, 2014): Such program focused on education as the basis of the intervention, developing and practicing self-regulatory skills necessary to perform moderate PA in lesbian and bisexual adults (aged 29 to 55 years). Generally, other interventions were characterized by increased social support, friendly (LGBT+) intervention environments, and decreased alcohol and smoking consumption. Thus, results highlighted that the lack of published evidence for programs targeting improved health in sexual minority women is challenging and alarming, particularly given the high and disparate rates of overweight and obesity in lesbian and bisexual women.
Successively, given that lesbian and bisexual women are more likely to be obese than their heterosexual counterparts, Fogel et al. (2016) described five other culturally appropriate interventions implemented to address weight- and fitness-related health disparities among older lesbian and bisexual women, promoting their healthy weight. The five funded programs were conducted using 376 lesbian and bisexual women aged 40 to 85 (enrollment is defined as providing informed consent, completing a baseline questionnaire, and signing up for a group). The interventions incorporate evidence-based PA and nutrition recommendations and a series of pre-and post-program assessments that may guide model programs and future research on the older lesbian and bisexual women population.
Discussion
This systematic review represents a first step toward a better understanding of older LGBT+ adults and their engagement in PA, differentiating for their subjectivity in terms of sexual and/or gender minority identity. As discussed in the introduction, some researchers have argued that differences in PA may be observed in older adults based on their sexual orientation and/or gender identity (Cunningham et al., 2018; Fredriksen-Goldsen et al., 2014). Most studies investigated prejudice, discrimination (Denison & Kitchen, 2015), and differences in sexual orientation and/or gender identity (Kendrick et al., 2021). Most of these studies included participants of all ages (18- 60 and over) or considered “older people” when individuals aged 50 and over. Despite these considerations and the substantial amount of relevant research on the topic regardless of participants’ age, to our knowledge, no systematic literature review has explored PA engagement in LGBT+ adults over 65. Thus, the current systematic review aimed to identify the dominant dimensions related to the intersection of PA, sexual identity, and age.
Fifty-three studies were systematically reviewed, comprising six qualitative and thirty-two quantitative (cross-sectional and longitudinal) research, five systematic or scoping reviews, three intervention sessions implementation, three commentaries, two survey reports, one book review, and one podium presentation. Only seven studies were conducted in Europe, two in Australia, one in Brazil, and forty-three in the USA and Canada. No Asian research limited to older LGBT+ people’s engagement with PA was observed. The low number of countries may symbolize a low level of interest in the well-being of older LGBT+ individuals. The STROBE classification provided methodology reproducibility, interpretation, and application of study results. In the present systematic review, 28 publications presented intermediate quality, 18 were high quality, and one paper presented low quality. It is important to emphasize that most selected studies obtained a low possibility of reporting bias.
Five identity categories and different research areas emerged from a review of these studies according to participants’ subjectivity and based on the studies’ numerosity: (1) sexual minority (LGB+) identities; (2) sexual and gender minority (LGBT+) identities; (3) transgender and gender-diverse identities; (4) gay and bisexual male identities; and (5) lesbian and bisexual female identities. The most frequent research areas (see Table 1), taking together all the five identity categories considered in the present review, were focused on differences between sexual and/or gender minority people and cis-heterosexual people (n = 22 studies), discrimination and homophobia/transphobia in sport-related contexts (n = 14 studies), and competent interventions for aging well in LGBT+ older adults (n = 13 studies).
Regarding the relevance of discrimination in sports environments, studies have identified the adverse effects of minority stressors (distal and proximal stressors) on PA in LGB+ people (Caceres et al., 2017; Denison & Kitchen, 2015; Fredriksen-Goldsen et al., 2013; Grossman et al., 2001; Mereish & Goldstein, 2020) and LGBT+ samples (Devís-Devís et al., 2022; Fredriksen-Goldsen et al., 2015, 2017, 2023b; Griffin et al., 2022). Physical health seems negatively associated with lifetime discrimination and positively related to physical and psychological health-related quality of life (Fredriksen-Goldsen et al., 2015, 2017; Kim et al., 2022). To our knowledge, no qualitative or quantitative studies addressed the relevance of ageism in PA engagement.
Homo/transphobia, discrimination (Baiocco et al., 2018; Denison & Kitchen, 2015; Pistella et al., 2020), and societal weight stigma (Puhl et al., 2019) are widely experienced around sports-related contexts by people of all ages, sexual orientations, and gender identities (Correro et al., 2022). In addition, ageism (Iversen et al., 2009) contributes to older adults’ experiences of social exclusion in sports environments, reinforcing social inequalities towards older adults, especially for sexual and gender minority people (Rosati et al., 2021a). Engagement in PA was more problematic for older participants (65 and over) than for the younger group (Bourne et al., 2017; Hughes & Kentlyn, 2014). A low prevalence of PA due to the expectation of being discriminated against (Kim et al., 2022; Rosati et al., 2021b) or internalized sexual stigma (Mereish & Goldstein, 2020) may be associated with more excess body fat, cardiovascular disease risk index, and other chronic conditions (Pharr et al., 2021).
Another relevant research area regards the differences in PA between sexual and/or gender minority individuals and cis-heterosexual people. Some research involving sexual minority participants did not find differences between sexual minority people and their heterosexual counterparts (Dilley et al., 2010; Nelson, 2021, 2023). Other research has argued the lower prevalence of PA and health-related behaviors in LGB+ individuals (Abichahine & Veenstra, 2017; Lindström & Rosvall, 2020) and transgender people (Fredriksen-Goldsen et al., 2014) of all ages, especially transgender women (Cunningham et al., 2018) compared to cis-heterosexual counterparts, showing that they may be considered an at-risk population. Only two papers found that sexual minority people perform more significant amounts of PA than their heterosexual counterparts, regardless of age (Cunningham et al., 2018; Fricke et al., 2019).
Research involving only transgender individuals (Fredriksen-Goldsen et al., 2014) demonstrated that transgender older adults, regardless of gender, were less likely to be engaged in regular PA than the nontransgender older adult participants, while two works (Boehmer et al., 2020; Downing & Przedworski, 2018) found lower PA levels in a sample of gender non-conforming people than transgender and cisgender counterparts. Other studies investigated eating disorders behaviors reported that about 7% (Uniacke et al., 2021) and 8% (Nagata et al., 2020a) of two samples of transgender individuals and 5% of a group of lesbian women (Nagata et al., 2021) reported compulsively exercising during the prior month.
Similarly, mixed results were obtained in studies on sexual minority men, with a higher prevalence of lower PA levels than heterosexual men. Some research (Bourne et al., 2017; Kendrick et al., 2021) suggested that sexual minority men of all ages perform less PA than heterosexual men; one paper reported no PA differences, while others indicated that sexual minority men engaged in more PA than heterosexual men (Lightner et al., 2020; Zhang et al., 2017). No differences in PA were found in lesbian and bisexual women vs. heterosexual counterparts (Hutchcraft et al., 2021).
Again, much research focused on implementing and developing culturally competent interventions for healthy aging in sexual and/or gender older adults. This research area changes according to the subjectivity considered in this review: (a) available research involving samples of LGB+ people or (b) LGBT+ individuals focused on PA and aging well (Pharr et al., 2021; Slevin, 2010; von Humboldt et al., 2021), and the needs of competent interventions for an LGBT+-focused PA research strategy (Fredriksen-Goldsen, 2014; Gorczynski & Brittain, 2016; Hasson et al., 2017); (c) no research on intervention or aging well on transgender population was found; (d) studies on sexual minority men investigated the role of body image in aging (Brennan-Ing et al., 2022; Slevin & Linneman, 2010), with a specific focus on the desire to be physically attractive given that gay culture reinforces hegemonic masculinity; (e) healthy-weight interventions are considered relevant for sexual minority women (Fogel et al., 2016; Rizer et al., 2015), given the highest rates of obesity in this population sub-group.
Interestingly, no research on the transgender population indicates the relevance of intervention programs to increasing PA for a positive aging process. Indeed, most research on this gender minority sub-group regards differences between transgender older adults and cisgender counterparts on (a) physical and mental disorders, such as eating behaviors and obesity (Fredriksen-Goldsen et al., 2014; Nagata et al., 2020a; Uniacke et al., 2021); (b) high-mortality diseases, such as cardiovascular diseases/cancer (Downing & Przedworski, 2018; Malhotra et al., 2022) or (c) the negative impact of Covid-19 pandemic in reducing healthy lifestyle behaviors, such as decreased PA in the general population (Tessier et al., 2023).
Finally, few qualitative studies were found on sexual and/or gender minority older adults. Existing research analyzed (a) experiences of transgender women in sports-related contexts of all ages, and only one participant was 65 years old (Stewart et al., 2020); (b) episodes and expectations of discrimination in sports-related contexts of LGB+ individuals (Rosati et al., 2021a; Slevin, 2010); and (c) sexual minority men and their body image (Slevin, 2008; Slevin & Linneman, 2010). There is only one qualitative study involving (d) sexual minority females (Kehoe, 1986), indicating that older lesbian women may be more physically active than heterosexual older women partly because some held non-traditional jobs requiring physical labor.
Limitations and Future Research Directions
This systematic review provides mixed evidence for the participation of sexual and/or gender minority people in PA. Despite increasing research interest in PA of LGBT+ older adults (as evidenced by the growing number of publications in the last decade), there is a lack of information regarding PA in older sexual and gender minority individuals (Kendrick et al., 2021), and little was found regarding participation rates of older LGBT+ aged 65 and over (Gorczynski & Brittain, 2016). Future studies should implement longitudinal procedures to understand better the factors that improve PA in LGBT+ older adults. These studies should examine sexual identity variations between sporting disciplines (i.e., golf, basket, baseball) or competitive level groups (i.e., amateur, sub-elite, and elite) and analyze whether LGBT+ older adults avoid some types of sporting contexts due to homo/transphobia and ageism.
The systematic review demonstrated that no research on the transgender population highlights intervention programs' relevance to increasing PA to promote well-being. These results suggest that future research should focus on specific interventions to improve resilience and positive dimensions in transgender people to promote a healthy aging process. Again, to our knowledge, only one study explicitly refers to ageism and homophobia as factors influencing participation in PA during older age (Slevin & Linneman, 2010). Indeed, the interviewees point out the relevance of ageism and attractiveness as pervasive and culturally relevant factors shaping sexual minority people’s social experiences in sports-related contexts. Narratives and life experiences on engagement in PA of sexual and/or gender minority older adults could be explored in future studies.
Another partially unexplored theme is how appearance-related benefits and objectification of body parts can potentially have (unintended) negative consequences on the well-being of older sexual and gender minority people in sports-related contexts. Few studies demonstrated that, in Western societies, body image dissatisfaction was also more frequent in gender minority people and cisgender women than cisgender men (Barnes et al., 2020; Tessier et al., 2023). Specifically, sexual minority men reported greater body image dissatisfaction and negative attitudes toward aging than heterosexual men. Future studies should explore the relevance of body image dissatisfaction and understand more precisely how ageism and the emphasis on attractiveness are culturally relevant dimensions that shape social experiences in the LGBTQ + community for the different identity categories (i.e., transgender and non-binary people).
The lack of a unique measurement to investigate PA levels represents a significant gap in the literature: Some studies did not clearly define PA evaluation or the percentages of participants 65 and over. In addition, the heterogeneity of the samples (i.e., country and age range) limits the generalizability of the results. Indeed, 74% of the studies were conducted in the USA, only 7% in European contexts, and no research in Asia. Regarding age-ranged, most studies included participants of all ages (16–80 and over) or considered participants aged 50 and over as “older adults”.
Further investigations should assess the PA levels in sexual and/or gender minority people with a method to cross-classify sex assigned at birth, gender identity, sexual orientation, and age, comparing young–middle–old groups (age 65–79) vs. the old–old-age (age 80 +) group. Indeed, an intersectionality perspective considering variables that can marginalize people (i.e., gender, race, class, sexual identity, physical ability) is timely and necessary to understand the resilience and vulnerability of LGBT+ older adults. A future meta-analysis might examine overall effect sizes, which were not evaluated in the present systematic review. Moreover, using a meta-analytic approach (Passos et al., 2020), it could be helpful to perform other statistical examinations, such as sensitivity analysis (to assess how the results might change under different assumptions), report bias assessment (to ensure that all “a priori” results have been analyzed and reported), and evaluation of certainty of evidence (to interpret the strength of conclusions using a tool such as GRADE).
However, the present work has significant strengths, comprising a rigorous systematic review protocol with clearly defined inclusion and exclusion criteria and high reviewer reliability, reflecting a transparent selection methodology. This systematic review represents the first study to synthesize the literature on PA in LGBT+ older adults, filling a significant gap in the literature about the relationship between PA and successful aging. The World Health Organization has identified regular PA as an effective strategy by which people can reduce the risk of developing chronic diseases and adverse conditions and promote positive aging. To conclude, considering the mixed results obtained by previous qualitative and quantitative works, the next step should include investigating the enablers of PA in older LGBT+ people and promoting regular exercise as a modality for reducing health disparities between LGBT+ individuals and their cis-heterosexual counterparts aged 65 and over.
Policy Implications
The findings of this systematic literature review have relevant policy and environmental implications for increasing inclusion and LGBT+-affirming PA and sports experiences. It is now well known that disparities exist between sexual and/or gender minority older adults and cis-heterosexual counterparts in PA (Abichahine & Veenstra, 2017; Lindström & Rosvall, 2020). However, as far as we know, no previous literature review has investigated LGBT+ engagement in PA during aging. Overall, our results show that interventions are still needed to reduce health behavior disparities between older LGBT+ people and cis-heterosexual people (Baiocco & Pistella, 2019), especially concerning PA and healthy and unhealthy habits (Fredriksen-Goldsen, 2014; Gorczynski & Brittain, 2016; Pistella et al., 2019).
Indeed, efforts to assess the extent of reduced PA in older LGBT+ people should consider the challenges that minority stress has presented to them across their lifespan and whether those barriers still exist (Correro et al., 2022). Assessment of how minority stress, homo/transphobic experiences, and ageism may be linked to the impact on health conditions is pivotal to reducing the gap in health disparities (Bränström et al., 2016; Fredricksen-Goldsen & de Vries, 2019). Interventions on improving PA levels in the older LGBT+ population should include strategies that affirm and support the complexity of sexual orientation and gender identities and expressions. For instance, creating gender-inclusive restrooms, individual showers, or private changing rooms could make a safe place for sexual and/or gender minority people (Baiocco et al., 2020). Such safe zones could facilitate LGBT+ older adults to maintain healthy behaviors and regular exercise, especially in non-binary and gender non-conforming people, which will be a relevant part of the older LGBT+ community in the next few years (Rosati et al., 2021b).
Finally, implementing policies and practices focused on sexual and/or gender identity issues in sports-related contexts, such as training and enumerated policies, may improve the perception of safety for LGBT+ older adults and all people regardless of their age (Baiocco et al., 2018; Pistella et al., 2020). It is mandatory to support the relevance of LGBT+ community connections among sexual and gender minority people through services and intervention programs to reduce loneliness and social isolation and promote healthy aging.
The present review seems to confirm that building an inclusive and non-judgmental context is fundamental for the well-being of LGBT+ individuals engaged in PA and regular exercise. We promote a social change in sexual and gender stereotypes and prejudice to build a more inclusive sports environment where all sexual and gender minority identities can be free of rigid gender norms. Moreover, we hope this article review will help future researchers promote studies evaluating healthy behaviors in LGBT+ older adults, especially in countries with high levels of social-sexual stigma and negative beliefs regarding sexual and/or gender minority people.
Data Availability
Data are available under request to the first author.
Code Availability
Not applicable.
References
*References marked with an asterisk indicate studies included in the systematic review
*Abichahine, H., & Veenstra, G. (2017). Inter-categorical intersectionality and leisure-based physical activity in Canada. Health Promotion International, 32(4), 691–701. https://doi.org/10.1093/heapro/daw009
Adzrago, D., Sulley, S., Tagoe, I., Odame, E., Mamudu, L., & Williams, F. (2022). Association between COVID-19 pandemic declaration and depression/anxiety among US adults. PLoS ONE, 17(12), e0279963. https://doi.org/10.1371/journal.pone.0279963
An, H. Y., Chen, W., Wang, C. W., Yang, H. F., Huang, W. T., & Fan, S. Y. (2020). The relationships between physical activity and life satisfaction and happiness among young, middle-aged, and older adults. International Journal of Environmental Research and Public Health, 17, 4817. https://doi.org/10.3390/ijerph17134817
Baiocco, R., & Pistella, J. (2019). “Be as you are” clinical research center at the Sapienza University of Rome. Journal of Gay & Lesbian Mental Health, 23(4), 376–379. https://doi.org/10.1080/19359705.2019.1644572
Baiocco, R., Pistella, J., Salvati, M., Ioverno, S., & Lucidi, F. (2018). Sports as a risk environment: Homophobia and bullying in a sample of gay and heterosexual men. Journal of Gay & Lesbian Mental Health, 22(4), 385–411. https://doi.org/10.1080/19359705.2018.1489325
Baiocco, R., Pistella, J., Salvati, M., Ioverno, S., & Lucidi, F. (2020). Sexual prejudice in sport scale: A new measure. Journal of Homosexuality, 67(4), 489–512. https://doi.org/10.1080/00918369.2018.1547560
Barnes, M., Abhyankar, P., Dimova, E., & Best, C. (2020). Associations between body dissatisfaction and self-reported anxiety and depression in otherwise healthy men: A systematic review and meta-analysis. PLoS ONE, 15(2), e0229268. https://doi.org/10.1371/journal.pone.0229268
*Boehmer, U., Gereige, J., Winter, M., Ozonoff, A., & Scout, N. (2020). Transgender individuals’ cancer survivorship: Results of a cross-sectional study. Cancer, 126(12), 2829–2836. https://doi.org/10.1002/cncr.32784
Bolijn, R., Schalkers, I., Tan, H. L., Kunst, A. E., & Van Valkengoed, I. G. M. (2020). Patient perspectives on priorities for research on conventional and sex-and gender-related cardiovascular risk factors. Netherlands Heart Journal, 28, 656–661. https://doi.org/10.1007/s12471-020-01497-9
*Bourne, A., Davey, C., Hickson, F., Reid, D., & Weatherburn, P. (2017). Physical health inequalities among gay and bisexual men in England: A large community-based cross-sectional survey. Journal of Public Health, 39(2), 290–296. https://doi.org/10.1093/pubmed/fdw029
*Braga, L. H. R., Menezes, C. S., Martins, I. V., Silva, J. D. P. D., & Torres, J. L. (2022). Factors associated with lifestyle deterioration during the COVID-19 pandemic among Brazilian lesbians, gays, bisexuals, transsexuals, transvestites, and related identities: A cross-sectional study. Epidemiologia e Serviços De Saúde, 31(1), 1–13. https://doi.org/10.1590/S1679-49742022000100005
Bränström, R., Hatzenbuehler, M. L., & Pachankis, J. E. (2016). Sexual orientation disparities in physical health: Age and gender effects in a population-based study. Social Psychiatry and Psychiatric Epidemiology, 51, 289–301. https://doi.org/10.1007/s00127-015-1116-0
*Brennan-Ing, M., Haberlen, S., Ware, D., Egan, J. E., Brown, A. L., Meanley, S., ... & Plankey, M. W. (2022). Psychological connection to the gay community and negative self-appraisals in middle-aged and older men who have sex with men: The mediating effects of fitness engagement. The Journals of Gerontology: Series B, 77(1), 39–49. https://doi.org/10.1093/geronb/gbab076
Brittain, D. R., & Dinger, M. K. (2014). BE-PALS: An innovative theory-based intervention to promote moderate physical activity among adult lesbians. Women in Sport and Physical Activity Journal, 22(2), 71–75. https://doi.org/10.1123/wspaj.2014-0017
*Caceres, B. A., Brody, A., Luscombe, R. E., Primiano, J. E., Marusca, P., Sitts, E. M., & Chyun, D. (2017). A systematic review of cardiovascular disease in sexual minorities. American Journal of Public Health, 107(4), e13–e21. https://doi.org/10.2105/AJPH.2016.303630
Cary, M. A., Brittain, D. R., Dinger, M. K., Ford, M. L., Cain, M., & Sharp, T. A. (2016). Barriers to physical activity among gay men. American Journal of Men’s Health, 10(5), 408–417. https://doi.org/10.1177/1557988315569297
Centers for Disease Control and Prevention. (2011). Physical activity for everyone: Older adults. Retrieved from: http://www.cdc.gov/physicalactivity/everyone/guidelines/olderadults.html
Chandavarkar, R. V., & Khan, M. S. (2015). Older lesbian, gay, bisexual and transgender persons in UK: Reviewing issues and concerns. Journal of Geriatric Care and Research, 2(1), 9–11.
Correro, A. N., Hinrichs, K. L., Krishnan, M. C., Cottingham, M. E., Trittschuh, E. H., Parmenter, B. A., ... & Stelmokas, J. (2022). Neuropsychological assessment with lesbian, gay, bisexual, transgender, and queer/questioning (LGBTQ+) individuals: Practice, education, and training survey. The Clinical Neuropsychologist. Advance online publication. https://doi.org/10.1080/13854046.2022.2148379
Courneya, K. S., Katzmarzyk, P. T., & Bacon, E. (2008). Physical activity and obesity in Canadian cancer survivors: Population‐based estimates from the 2005 Canadian Community Health Survey. Cancer: Interdisciplinary International Journal of the American Cancer Society, 112(11), 2475–2482. https://doi.org/10.1002/cncr.23455
*Cruikshank, M. (1991). Lavender and gray: A brief survey of lesbian and gay aging studies. Journal of Homosexuality, 20(3–4), 77–88. https://doi.org/10.1300/J082v20n03_05
*Cunningham, T. J., Xu, F., & Town, M. (2018). Prevalence of five health-related behaviors for chronic disease prevention among sexual and gender minority adults—25 US States and Guam, 2016. Morbidity and Mortality Weekly Report, 67(32), 888–893. https://doi.org/10.15585/mmwr.mm6732a4
*Denison, E., & Kitchen, A. (2015). Out on the Fields: The first international study on homophobia in sport. Nielsen, Bingham Cup Sydney 2014, Australian Sports Commission, Federation of Gay Games. Retrieved from: www.outonthefields.com
*Devís-Devís, J., Pereira-García, S., Valencia-Peris, A., Vilanova, A., & Gil-Quintana, J. (2022). Harassment disparities and risk profile within lesbian, gay, bisexual and transgender Spanish adult population: Comparisons by age, gender identity, sexual orientation, and perpetration context. Frontiers in Public Health, 10, 4862. https://doi.org/10.3389/fpubh.2022.1045714
*Dilley, J. A., Simmons, K. W., Boysun, M. J., Pizacani, B. A., & Stark, M. J. (2010). Demonstrating the importance and feasibility of including sexual orientation in public health surveys: Health disparities in the Pacific Northwest. American Journal of Public Health, 100(3), 460–467. https://doi.org/10.2105/AJPH.2007.130336
*Downing, J. M., & Przedworski, J. M. (2018). Health of transgender adults in the US, 2014–2016. American Journal of Preventive Medicine, 55(3), 336–344. https://doi.org/10.1016/j.amepre.2018.04.045
*Fogel, S. C., McElroy, J. A., Garbers, S., McDonnell, C., Brooks, J., Eliason, M. J., ... & Haynes, S. G. (2016). Program design for healthy weight in lesbian and bisexual women: A ten-city prevention initiative. Women’s Health Issues, 26, S7–S17. https://doi.org/10.1016/j.whi.2015.10.005
*Fredriksen-Goldsen, K. I. (2014). Promoting health equity among LGBT mid-life and older adults: Revealing how LGBT mid-life and older adults can attain their full health potential. Generations, 38(4), 86–92.
*Fredriksen-Goldsen, K. I., Cook-Daniels, L., Kim, H. J., Erosheva, E. A., Emlet, C. A., Hoy-Ellis, C. P., ... & Muraco, A. (2014). Physical and mental health of transgender older adults: An at-risk and underserved population. The Gerontologist, 54(3), 488–500. https://doi.org/10.1093/geront/gnt021
Fredricksen-Goldsen, K. I., & de Vries, B. (2019). Global aging with pride: International perspectives on LGBT aging. The International Journal of Aging and Human Development, 88(4), 315–324. https://doi.org/10.1177/0091415019837648
*Fredriksen-Goldsen, K. I., Emlet, C. A., Kim, H. J., Muraco, A., Erosheva, E. A., Goldsen, J., & Hoy-Ellis, C. P. (2013). The physical and mental health of lesbian, gay male, and bisexual (LGB) older adults: The role of key health indicators and risk and protective factors. The Gerontologist, 53(4), 664–675. https://doi.org/10.1093/geront/gns123
*Fredriksen-Goldsen, K. I., Kim, H. J., Bryan, A. E., Shiu, C., & Emlet, C. A. (2017). The cascading effects of marginalization and pathways of resilience in attaining good health among LGBT older adults. The Gerontologist, 57(suppl_1), S72–S83. https://doi.org/10.1093/geront/gnw170
*Fredriksen-Goldsen, K. I., Kim, H. J., Shiu, C., Goldsen, J., & Emlet, C. A. (2015). Successful aging among LGBT older adults: Physical and mental health-related quality of life by age group. The Gerontologist, 55(1), 154–168. https://doi.org/10.1093/geront/gnu081
*Fredriksen-Goldsen, K., Jen, S., Emlet, C. A., Kim, H. J., & Jung, H. H. (2023b). Key determinants of physical and psychological health-related quality of life over time among midlife and older LGBTQ and sexual and gender-diverse caregivers. The Gerontologist, 63(4), 751–761. https://doi.org/10.1093/geront/gnac112
Fredriksen-Goldsen, K. I., & Muraco, A. (2010). Aging and sexual orientation: A 25-year review of the literature. Research on Aging, 32(3), 372–413. https://doi.org/10.1177/0164027509360355
*Fredriksen-Goldsen, K., Teri, L., Kim, H. J., La Fazia, D., McKenzie, G., Petros, R., ... & Emlet, C. A. (2023a). Design and development of the first randomized controlled trial of an intervention (IDEA) for sexual and gender minority older adults living with dementia and care partners. Contemporary Clinical Trials, 128, 107143. https://doi.org/10.1016/j.cct.2023.107143
*Freedman, A., & Nicolle, J. (2020). Social isolation and loneliness: The new geriatric giants: Approach for primary care. Canadian Family Physician, 66(3), 176–182.
*Fricke, J., Gordon, N., & Downing, J. (2019). Sexual orientation disparities in physical activity. Medical Care, 57(2), 138–144. https://doi.org/10.1097/MLR.0000000000001017
Godin, G., & Shephard, R. J. (1997). Godin Leisure-Time Exercise Questionnaire. Medicine & Science in Sports & Exercise, 29, 36–38. https://doi.org/10.1097/00005768-199706001-00009
*Gorczynski, P. F., & Brittain, D. R. (2016). Call to action: The need for an LGBT-focused physical activity research strategy. American Journal of Preventive Medicine, 51(4), 527–530. https://doi.org/10.1016/j.amepre.2016.03.022
*Griffin, M., Bailey, K. A., & Lopez, K. J. (2022). #BodyPositive? A critical exploration of the body positive movement within physical cultures taking an intersectionality approach. Frontiers in Sports and Active Living, 4, 908580. https://doi.org/10.3389/2Ffspor.2022.908580
*Grossman, A. H., D’augelli, A. R., & O’connell, T. S. (2001). Being lesbian, gay, bisexual, and 60 or older in North America. Journal of Gay & Lesbian Social Services, 13(4), 23–40. https://doi.org/10.1300/J041v13n04_05
*Hasson, R. E., Brown, D. R., Dorn, J., Barkley, L., Torgan, C., Whitt-Glover, M., ... & Keith, N. (2017). Achieving equity in physical activity participation: ACSM experience and next steps. Medicine and Science in Sports and Exercise, 49(4), 848–858. https://doi.org/10.1249/mss.0000000000001161
Hawkins, B. A. (2005). Aging well: Toward a way of life for all people. Preventing Chronic Disease, 2(3), 1–3. Retrieved from: http://www.cdc.gov/pcd/issues/2005/jul/05_0018.htm
Holder, J., Morris, J., & Spreckley, M. (2022). Barriers and facilitators for participation in physical activity in the transgender population: A systematic review. Physical Activity and Health, 6(1), 136–152. https://doi.org/10.5334/paah.190
*Hughes, M., & Kentlyn, S. (2014). Report of the survey of the health and wellbeing of lesbian, gay, bisexual, transgender and intersex (LGBTI) older people in NSW, 2013–2014. Retrieved from: https://grai.org.au/wp-content/uploads/2020/05/Outrageous-Ageing-Survey-Report-1.pdf
*Hutchcraft, M. L., Teferra, A. A., Montemorano, L., & Patterson, J. G. (2021). Differences in health-related quality of life and health behaviors among lesbian, bisexual, and heterosexual women surviving cancer from the 2013 to 2018 National Health Interview Survey. LGBT Health, 8(1), 68–78. https://doi.org/10.1089/lgbt.2020.0185
Iversen, T. N., Larsen, L., & Solem, P. E. (2009). A conceptual analysis of ageism. Nordic Psychology, 61(3), 4–22. https://doi.org/10.1027/1901-2276.61.3.4
Jablonski, R. A., Vance, D. E., & Beattie, E. (2013). The invisible elderly: Lesbian, gay, bisexual, and transgender older adults. Journal of Gerontological Nursing, 39(11), 46–52. https://doi.org/10.3928/00989134-20130916-02
Jakicic, J. M., Kraus, W. E., Powell, K. E., Campbell, W. W., Janz, K. F., Troiano, R. P., Torres, S. A., & Piercy, K. L. (2019). Association between about duration of physical activity and health: A systematic review. Medicine and Science in Sports and Exercise, 51(6), 1231–1219. https://doi.org/10.1249/MSS.0000000000001933
Jenkinson, C., Layte, R., Jenkinson, D., Lawrence, K., Petersen, S., Paice, C., & Stradling, J. (1997). A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? Journal of Public Health, 19(2), 179–186. https://doi.org/10.1093/oxfordjournals.pubmed.a024606
*Kehoe, M. (1986). A portrait for the older lesbian. Journal of Homosexuality, 12(3–4), 157–161. https://doi.org/10.1300/J082v12n03_14
*Kendrick, D., Hughes, M., Coutts, R., & Ardzejewska, K. (2021). Older gay men’s engagement with physical activity: A scoping review. Health & Social Care in the Community, 29(6), e457–e466. https://doi.org/10.1111/hsc.13480
Kesaniemi, Y. A., Danforth, E., Jensen, M. D., Kopelman, P. G., Lefèbvre, P. I. E. R. R. E., & Reeder, B. A. (2001). Dose-response issues concerning physical activity and health: An evidence-based symposium. Medicine & Science in Sports & Exercise, 33(6), S351–S358.
*Kim, H. J., Fredriksen-Goldsen, K., & Jung, H. H. (2022). Health-related quality of life among sexual and gender minority older adults living with cognitive impairment. Alzheimer’s & Dementia, 18, e063193. https://doi.org/10.1002/alz.063193
*Lightner, J. S., Heinrich, K. M., & Sanderson, M. R. (2020). A population-based study of coupling and physical activity by sexual orientation for men. Journal of Homosexuality, 67(11), 1533–1541. https://doi.org/10.1080/00918369.2019.1601435
*Lindström, M., & Rosvall, M. (2020). Sexual identity and low leisure-time physical activity: A population-based study. Public Health, 182, 77–79. https://doi.org/10.1016/j.puhe.2020.02.003
*Malhotra, A., Kort, S., Lauther, T., Mann, N., Skopicki, H. A., & Parikh, P. B. (2022). Prevalence and predictors of cardiovascular disease and risk factors in transgender persons in the United States. Critical Pathways in Cardiology, 21(1), 42–46. https://doi.org/10.1097/HPC.0000000000000271
*Marmo, S., Pardasani, M., & Vincent, D. (2021). Senior Centers and LGBTQ Participants: Engaging older adults virtually in a pandemic. Journal of Gerontological Social Work, 64(8), 864–884. https://doi.org/10.1080/01634372.2021.1937431
*Mereish, E. H., & Goldstein, C. M. (2020). Minority stress and cardiovascular disease risk among sexual minorities: Mediating effects of sense of mastery. International Journal of Behavioral Medicine, 27, 726–736. https://doi.org/10.1007/s12529-020-09919-z
Mitchell, J., Allen, J. O., & Perry, R. (2019). Men’s health in later life: Diverse and intersecting contexts. In D. M. Griffith, M. A. Bruce, & R. J. Thorpe (Eds.), Men’s Health Equity (pp. 86–100). Routledge.
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., ... & Stewart, L. A. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Systematic Reviews, 4(1), 1–9. https://doi.org/10.1186/2046-4053-4-1
*Nagata, J. M., Compte, E. J., Murray, S. B., Schauer, R., Pak, E., Flentje, A., ... & Obedin-Maliver, J. (2021). Community norms for the eating disorder examination questionnaire (EDE-Q) among cisgender bisexual plus women and men. Eating and Weight Disorders-Studies on Anorexia, Bulimia and Obesity, 26, 2227–2239. https://doi.org/10.1007/s40519-020-01070-8
*Nagata, J. M., Murray, S. B., Compte, E. J., Pak, E. H., Schauer, R., Flentje, A., ... & Obedin-Maliver, J. (2020a). Community norms for the Eating Disorder Examination Questionnaire (EDE-Q) among transgender men and women. Eating Behaviors, 37, 101381. https://doi.org/10.1016/j.eatbeh.2020.101381
*Nagata, J. M., Murray, S. B., Flentje, A., Compte, E. J., Schauer, R., Pak, E., ... & Obedin-Maliver, J. (2020b). Eating disorder attitudes and disordered eating behaviors as measured by the Eating Disorder Examination Questionnaire (EDE-Q) among cisgender lesbian women. Body Image, 34, 215–220. https://doi.org/10.1016/j.bodyim.2020.06.005
*Nelson, C. L. (2021). Resilience and health outcomes of Sexual minority middle-aged and older adults. Doctoral dissertation, University of South Florida. Retrieved from: https://digitalcommons.usf.edu/cgi/viewcontent.cgi?article=10395&context=etd
*Nelson, C. L. (2023). Personality profiles and health behaviors among sexual minority middle-aged and older adults: Identifying resilience through latent profile analysis. Personality and Individual Differences, 206, 112140. https://doi.org/10.1016/j.paid.2023.112140
Newby, J. M., O’Moore, K., Tang, S., Christensen, H., & Faasse, K. (2020). Acute mental health responses during the COVID-19 pandemic in Australia. PLoS ONE, 15(7), e0236562. https://doi.org/10.1371/journal.pone.0236562
Ouzzani, M., Hammady, H., Fedorowicz, Z., & Elmagarmid, A. (2016). Systematic Reviews, 5, 210. https://doi.org/10.1186/s13643-016-0384-4
Passos, T. S., Teixeira, M. S., & Almeida-Santos, M. A. (2020). Quality of life after gender affirmation surgery: A systematic review and network meta-analysis. Sexuality Research and Social Policy, 17(2), 252–262. https://doi.org/10.1007/s13178-019-00394-0
*Pharr, J. R., Flatt, J. D., Chien, L. C., Kachen, A., & Olakunde, B. O. (2021). Exercise as a mitigator of poor mental health among lesbian, gay, and bisexual adults. Journal of Physical Activity and Health, 18(5), 548–556. https://doi.org/10.1123/jpah.2020-0703
Pistella, J., Ioverno, S., & Russell, S. T. (2019). The role of peer victimization, sexual identity, and gender on unhealthy weight control behaviors in a representative sample of Texas youth. International Journal of Eating Disorders, 52(5), 597–601. https://doi.org/10.1002/eat.23055
Pistella, J., Rosati, F., Ioverno, S., Girelli, L., Laghi, F., Lucidi, F., & Baiocco, R. (2020). Coming out in family and sports-related contexts among young Italian gay and lesbian athletes: The mediation effect of the “don’t ask, don’t tell” attitude. Journal of Child and Family Studies, 29, 208–216. https://doi.org/10.1007/s10826-019-01551-0
Pistella, J., Tanzilli, A., Ioverno, S., Lingiardi, V., & Baiocco, R. (2018). Sexism and attitudes toward same-sex parenting in a sample of heterosexuals and sexual minorities: The mediation effect of sexual stigma. Sexuality Research and Social Policy, 15, 139–150. https://doi.org/10.1007/s13178-017-0284-y
*Puhl, R. M., Himmelstein, M. S., Pearl, R. L., Wojtanowski, A. C., & Foster, G. D. (2019). Weight stigma among sexual minority adults: Findings from a matched sample of adults engaged in weight management. Obesity, 27(11), 1906–1915. https://doi.org/10.1002/oby.22633
Richard, C. A., & Brown, A. H. (2006). Configurations of informal social support among older lesbians. Journal of Women & Aging, 18(4), 49–65. https://doi.org/10.1300/J074v18n04_05
Richards, J., Jiang, X., Kelly, P., Chau, J., Bauman, A., & Ding, D. (2015). Don’t worry, be happy: Cross-sectional associations between physical activity and happiness in 15 European countries. BMC Public Health, 15(1), 1–8. https://doi.org/10.1186/s12889-015-1391-4
*Rizer, A. M., Mauery, D. R., Haynes, S. G., Couser, B., & Gruman, C. (2015). Challenges in intervention research for lesbian and bisexual women. LGBT Health, 2(2), 105–112. https://doi.org/10.1089/lgbt.2014.0122
*Rosati, F., Pistella, J., & Baiocco, R. (2021a). Italian sexual minority older adults in healthcare services: Identities, discriminations, and competencies. Sexuality Research and Social Policy, 18, 64–74. https://doi.org/10.1007/s13178-020-00443-z
Rosati, F., Pistella, J., Giovanardi, G., & Baiocco, R. (2021b). Queer generativity in lesbian, gay, and bisexual older adults: Personal, relational, and political/social behaviours. Journal of Community & Applied Social Psychology, 31(6), 673–689. https://doi.org/10.1002/casp.2529
Rowe, J. W., & Kahn, R. L. (1997). Successful aging. The Gerontologist, 37(4), 433–440. https://doi.org/10.1093/geront/37.4.433
Scandurra, C., Mezza, F., Bochicchio, V., Valerio, P., & Amodeo, A. L. (2017). LGBT elders health from the minority stress perspective. Literature review & research recommendations. Psicologia Della Salute, 2, 70–96. https://doi.org/10.3280/PDS2017-002004
*Slevin, K. (2008). Disciplining bodies: The aging experiences of older heterosexual and gay men. Generations, 32(1), 36–42.
*Slevin, K. F. (2010). If I had lots of money… I’d have a body makeover: Managing the aging body. Social Forces, 88(3), 1003–1020. https://doi.org/10.1353/sof.0.0302
*Slevin, K. F., & Linneman, T. J. (2010). Old gay men’s bodies and masculinities. Men and Masculinities, 12(4), 483–507. https://doi.org/10.1177/1097184X08325225
*Stewart, L., Oates, J., & O’Halloran, P. (2020). “My voice is my identity”: The role of voice for trans women’s participation in sport. Journal of Voice, 34(1), 78–87. https://doi.org/10.1016/j.jvoice.2018.05.015
*Tessier, A. J., Moyen, A., Lawson, C., Rappaport, A. I., Yousif, H., Fleurent-Grégoire, C., ... & Chevalier, S. (2023). Lifestyle behavior changes and associated risk factors during the COVID-19 pandemic: Results from the Canadian COVIDiet online cohort study. JMIR Public Health and Surveillance, 9(1), e43786. https://doi.org/10.2196/43786
Úbeda-Colomer, J., Gil-Quintana, J., Pereira-García, S., López-Cañada, E., Pérez-Samaniego, V., & Devís-Devís, J. (2020). Development and validation of the barriers to physical activity and sport questionnaire for lesbian, gay, bisexual, transgender and queer/questioning persons. Public Health, 185, 202–208. https://doi.org/10.1016/j.puhe.2020.05.020
*Uniacke, B., Glasofer, D., Devlin, M., Bockting, W., & Attia, E. (2021). Predictors of eating-related psychopathology in transgender and gender nonbinary individuals. Eating Behaviors, 42, 101527. https://doi.org/10.1016/j.eatbeh.2021.101527
Vandenbroucke, J. P., Elm, E. V., Altman, D. G., Gøtzsche, P. C., Mulrow, C. D., Pocock, S. J., ... & Strobe Initiative. (2007). Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): Explanation and elaboration. Annals of Internal Medicine, 147(8), 163–194. https://doi.org/10.7326/0003-4819-147-8-200710160-00010-w1
*von Humboldt, S., Carneiro, F., & Leal, I. (2021). Older lesbian, gay, and bisexual adults: What predicts adjustment to aging? Sexuality Research and Social Policy, 18, 1042–1048. https://doi.org/10.1007/s13178-020-00507-0
Warburton, D. E. R., & Bredin, S. S. D. (2017). Health benefits of physical activity: A systematic review of current systematic reviews. Current Opinion in Cardiology, 32(5), 541–556. 498 https://doi.org/10.1097/HCO.0000000000000437
World Health Organization. (2010). Global recommendations on physical activity for health. World Health Organization. Retrieved from: https://apps.who.int/iris/handle/10665/44399
*Zhang, J., Jemmott, J. B., III., O’Leary, A., Stevens, R., Jemmott, L. S., Icard, L. D., & Rutledge, S. E. (2017). Efficacy and mediation of a theory-based physical activity intervention for African American men who have sex with men: A randomized controlled trial. Annals of Behavioral Medicine, 51(1), 106–116. https://doi.org/10.1007/s12160-016-9832-6
Acknowledgements
We acknowledge co-funding from Next Generation EU, in the context of the National Recovery and Resilience Plan, Investment PE8 – Project Age-It: “Ageing Well in an Ageing Society”. This resource was co-financed by the Next Generation EU [DM 1557 11.10.2022]. The views and opinions expressed are only those of the authors and do not necessarily reflect those of the European Union or the European Commission. Neither the European Union nor the European Commission can be held responsible for them.
Funding
Open access funding provided by Università degli Studi di Roma La Sapienza within the CRUI-CARE Agreement. This project was supported with funding from Next Generation EU, in the context of the National Recovery and Resilience Plan, Investment PE8 – Project Age-It: “Ageing Well in an Ageing Society”. This resource was co-financed by the Next Generation EU [DM 1557 11.10.2022].
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study’s conception and design. All the authors participated in the material preparation and data collection. Methodology, formal analyses, and investigation: Roberto Baiocco, Jessica Pistella, and Fabio Lucidi; Writing—original draft preparation: Jessica Pistella, Roberto Baiocco, Chiara Antoniucci, Guido Alessandri, Anna M. Borghi, Fabio Alivernini, Simone Tavolucci, Chiara Fini, Lorenzo Filosa, Tommaso Palombi, and Fabio Lucidi; Writing—review and editing: All the authors reviewed the manuscript. Supervision: Roberto Baiocco and Fabio Lucidi. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. Approval was granted by the Ethic Committee of the Developmental and Social Psychology, Faculty of Medicine and Psychology, Sapienza University of Rome.
Conflicts of Interest
The authors have no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pistella, J., Baiocco, R., Antoniucci, C. et al. Older LGBT+ Adults and Physical Activity: A Systematic Review of Qualitative and Quantitative Data. Sex Res Soc Policy (2024). https://doi.org/10.1007/s13178-023-00925-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s13178-023-00925-w