Abstract
Non-communicable chronic diseases (NCDs) have become a major global health concern. They constitute the leading cause of disabilities, increased morbidity, mortality, and socio-economic disasters worldwide.
Medical condition-specific digital biomarker (DB) panels have emerged as valuable tools to manage NCDs. DBs refer to the measurable and quantifiable physiological, behavioral, and environmental parameters collected for an individual through innovative digital health technologies, including wearables, smart devices, and medical sensors. By leveraging digital technologies, healthcare providers can gather real-time data and insights, enabling them to deliver more proactive and tailored interventions to individuals at risk and patients diagnosed with NCDs.
Continuous monitoring of relevant health parameters through wearable devices or smartphone applications allows patients and clinicians to track the progression of NCDs in real time. With the introduction of digital biomarker monitoring (DBM), a new quality of primary and secondary healthcare is being offered with promising opportunities for health risk assessment and protection against health-to-disease transitions in vulnerable sub-populations. DBM enables healthcare providers to take the most cost-effective targeted preventive measures, to detect disease developments early, and to introduce personalized interventions. Consequently, they benefit the quality of life (QoL) of affected individuals, healthcare economy, and society at large.
DBM is instrumental for the paradigm shift from reactive medical services to 3PM approach promoted by the European Association for Predictive, Preventive, and Personalized Medicine (EPMA) involving 3PM experts from 55 countries worldwide. This position manuscript consolidates multi-professional expertise in the area, demonstrating clinically relevant examples and providing the roadmap for implementing 3PM concepts facilitated through DBs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Preamble
A limited access to diagnostic tests is recognized as one of the major barriers to provide healthcare services in remote and low- and middle-income countries (LMIC). In high-income countries (HIC), similar issues arise due to over-burdened and centralized healthcare systems that cannot provide diagnoses in a timely manner. The development of sensitive and accurate smart biosensors has been the focus of a major effort over the last decade to set up point-of-care tests supporting decentralization of healthcare services. Development of portable biosensors require a biorecognition element (BRE) that measures and quantifies the analyte of interest, a transducer that senses a change brought about by the binding of the analyte to the BRE and amplifies this signal so that it is detected by a smart device.
The evolution of wearable point-of-care devices for measuring disease-specific analytes has progressively utilized minimally invasive BREs to detect biomarkers in easily accessible biological fluids including the use of smart contact lenses for tear-based biosensors, epidermal biosensors, oral biosensors to detect salivary metabolites, urinary biosensors, breath-based biosensors, and smartphone-assisted colorimetric biosensors. Specifically in the area of cancer research, various BREs were developed to detect biological makers at physiological ranges, including carcinoembryonic antigen (CEA) detection in saliva showing promise for early oral cancer detection [1], measuring inflammation markers [2], detection of breast cancer marker Mucin1 in serum samples [3], and volatile organic compounds in breath-based biosensors [4] and biological fluids to detect cancers using odorant receptor-based biosensors [5]. Extensive work is being performed in the field utilizing biosensors for lung cancer detection, including the detection of analytes such as circulating tumor nucleic acids including Epidermal Growth Factor Receptor (EGFR) [6] and KRAS [7] mutations, microRNA [8], and specific proteins such as CEA [9].
Advances in microfluidics and nanotechnology provide the platforms towards real-time sensing of molecules and transduce the amplified signal to a digitalized readout, exemplified by personal glucose sensors that relay the measured levels to a smart watch. The enabling technology between the BREs that measure the analyte and readout involve microfluidics and highly sensitive detection systems such as smart devices. The microfluidic devices are low-volume chambers and channels, also known as lab-on-chip. The use of microfluidic point-of-care diagnostic devices coupled with paper-based biosensors and optical smartphone colorimetric readout is exemplified by detection of Alpha-fetoprotein (AFP) and Mucin-16 (MUC16) in serum considered potent biomarkers for liver and ovarian cancers [10], and Prostate-Specific Antigen (PSA) for prostate cancer [11]. Alternatively, the use of electrochemical biomedical sensors are exemplified by Human epididymis protein 4 (HE4) in serum as biomarker for ovarian cancer [12], and detection of tyrosinase (TYR) enzyme as a biomarker to monitor melanomas [13]. The electrochemical sensor measures a differential current following the conversion of the substrate immobilized on the transducer surface when it meets the analyte. The wearable sensors transmit data wirelessly to a smart device through an ultralight and flexible electronic board.
Integration of Artificial Intelligence (AI) with wearable sensors allows monitoring of an individual’s health in real time. The main objective is to transform sensor signals into clinically relevant parameters that improve the quality of care and disease management. The resulting parameters can further be utilized in dedicated AI models to predict disease risk, make diagnoses, and monitor disease progression [14,15,16,17,18].
The main challenge in developing point-of-care diagnostic biosensors is to lower the detection limit, enabling an enhanced sensitivity of corresponding analytes specific for health and medical conditions under consideration. Research in the development of modified nanobodies as the BRE and microfluidic devices enhances analyte sequestration and provides the tool to amplify the electron transfer rate towards the physical transducer to generate a sensitive, detectable readout. The use of AI has a pivotal role in the development of smart biosensing devices for advanced diagnostics and early detection of the health-to-disease transition [14, 19].
In this EPMA position manuscript, we focus on an emerging aspect in modern healthcare that originates from the technological advancements of our increasingly digitalized world: digital biomarkers. Progressively throughout this report, we will define digital biomarkers, elaborate how they are measured and validated, provide examples on how they transformed multiple indication areas, and explore their utility and potential in the context of predictive, preventive, and personalized medicine (3PM) [20].
Defining digital biomarkers
Digital biomarkers refer to the measurable and quantifiable physiological, behavioral, and environmental parameters collected for an individual through innovative digital health technologies, including wearables, smart devices, and medical sensors. In our modern, digitalized world, human beings constantly interact with digital devices and thereby produce measurable data as schematically presented in Fig. 1. Smartwatches and fitness trackers, for example, measure an individual’s heart rate, physical activity, and resting patterns. Smart devices track how their users interact with specific applications, how long and often they actively use their device throughout the day and are filled with sensors that can recognize subtle movements and record speech. All the measurements mentioned above are well-known modulators of personal health or correlate strongly with it and, thus, it seems obvious that they could support providing optimal healthcare to today’s patients. However, to make them applicable in a healthcare context, they need to be developed from patient-level data and validated to ensure their reliability [21].
Over the recent years, digital health applications have also been developed that specifically aim to monitor an individual’s disease symptoms and progression [22], monitor relevant health indicators in real time and provide notifications if they appear critical, or track dietary habits. Data is provided to these applications through direct transfer from a wearable sensor (e.g., a continuous glucose monitor in the context of diabetes) or can be self-reported by the patient (e.g., tracking mood swings in patients suffering from manic depressions).
Sleep disorders
Good quality sleep is considered an important aspect of protection against health-to-disease transition (primary care) and against disease progression (secondary care), which makes it instrumental in the context of 3PM. Further, there is evident reciprocity between compromised sleep quality/sleep disorders and a broad spectrum of generally preventable diseases including chronic inflammation; metabolic, immune, and mood disorders; malignancies; cardiovascular disease (CVD); and neurological and neurodegenerative disorders [14, 23,24,25,26]. Targeted prevention and individualized monitoring of sleep disorders is crucial to maintain health and life [27,28,29]. Table 1 highlights the DBs applied and proposed specifically in sleep medicine.
An increasing number of digital health platforms address the demand on multi-parametric analysis summarized above, and thereby enable professionals to perform digital screenings for sleep disorders, accurate diagnosis, personalized treatments and cost-effective prevention of sleep disorders, and associated pathologies in primary and secondary care.
Diabetes care
The prominent examples of DBs commonly used in diabetes care and monitoring are presented in Table 2.
These DBs enable individuals with diabetes to actively participate in self-management and empower healthcare providers with more comprehensive data for personalized care. Integration of DBs into digital health platforms allows for continuous monitoring, analysis, and early detection of deviations from optimal health. The CGM-related DBs have already become a standard of care in people with both type 1 and type 2 diabetes, resulting in improved outcomes as demonstrated in numerous studies [49,50,51].
Cardiovascular diseases
Cardiovascular diseases remain the leading cause of morbidity and mortality worldwide [52]. Traditional approaches to CVD management have primarily relied on subjective patient-reported symptoms and intermittent clinical assessments. Recent advances in digital health technologies have created new possibilities for monitoring and managing CVDs more effectively. Selected DBs related to CVDs are listed in Table 3.
The DBs in CVDs can capture subtle changes in physiological parameters, detect early warning signs, and enable personalized interventions.
Chronic obstructive pulmonary disease
Chronic obstructive pulmonary disease (COPD) is a progressive respiratory condition characterized by a persistent airflow limitation which leads to significant morbidity and mortality worldwide. The management of COPD traditionally involves subjective symptom reporting and periodic spirometry assessments. DBs offer numerous advantages for COPD management. They enable the detection of minor changes in disease progression, facilitate early intervention, and empower patients to actively participate in their own care. Examples of DBs used in COPD are presented in Table 4.
DBs used in the treatment of COPD have the potential to enhance remote monitoring, reduce hospitalizations, and optimize treatment strategies for COPD patients.
Cancers
To a large extent, cancer management relies on periodic imaging, laboratory tests, and subjective patient reporting. In contrast, DBs have the potential to revolutionize cancer management across the entire continuum, including real-time monitoring, cost-effective health risk assessment and individualized protection against health-to-disease transition, early detection of disease progression, treatment algorithms tailored to individualized patient profile, response assessment, and improved individual outcomes. Examples of DBs used in cancer management are listed in Table 5.
The role of digital biomarkers in predictive medicine
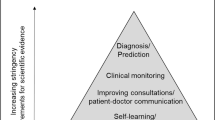
Digital biomarkers contribute to predictive medicine by providing insights into disease risk, progression, and treatment response. Continuous DBM through wearables, smart devices, or smartphone applications allows patients and healthcare providers to forecast the future progression of NCDs in real time as presented in Fig. 2.
Flow of DB data from wearable to the cloud processed through AI/ML, added to patients’ medical records, and provided to the healthcare practitioner. Previous medical records of the patients can support the AI in interpreting DB patterns. Please note that the patient becomes also aware of DB data increasing its engagement in the management process. Healthcare practitioners are using the DB processed data integrated with other data from the electronic health records (laboratory analyses, imaging, etc.) for adequate management decisions in the frame of 3PM
For example, studies have shown CGM to be cost effective, reduce hospitalizations, and improve QoL in patients with diabetes [65, 66], and home-based blood pressure monitoring was found to be more cost-effective compared to clinic-based care [67]. Telehealth could play a role in the care and management of people with COPD, and as part of multi‐component care packages may provide short‐term benefits for QoL and hospital re‐admissions [68]. Remote monitoring systems for COPD are expected to become integrated into the healthcare system, which could reduce costs and improve the quality of care by predicting an individual patient’s response and risk [69].
Considering the strong association between diabetes and CVDs, or diabetes and cancer, integrating several DBs related to different NCDs could enhance their predictive value.
Data-driven approaches from the field of AI and ML can analyze trends and patterns in DBs and predict potential exacerbations, complications, or a patient’s response to specific interventions. Providing healthcare practitioners with this information facilitates and focuses discussions about healthcare evaluation and implementing treatment regimens. The predictions provide decision support to clinicians and allow them to select personalized treatments that optimize therapeutic outcomes while minimizing adverse effects. This also opens the opportunity to take early, proactive measures, such as adjusting medications, recommending lifestyle modifications, or initiating early interventions to prevent adverse health outcomes. Predictions made with AI approaches leveraging DBs can also be utilized to inform screening processes in clinical trials and enrich trial cohorts with specific disease subtypes. This, subsequently, also enables employing novel clinical trial designs, such as umbrella or basket trials [70].
The role of digital biomarkers in preventive medicine
Prevention plays a crucial role in reducing the burden of NCDs. DBs offer novel opportunities to identify individuals at high risk of developing the condition and implement effective preventive strategies.
Wearable devices, such as smartwatches and fitness trackers, collect real-time data on vital signs, physical activity, sleep patterns, and other physiological parameters. To create an opportunity for early disease prevention, the means for early disease detection or risk prediction must be opened [71]. AI algorithms and ML models are poised to identify patterns and anomalies in an individual’s DB patterns that may signify the early onset of a disease or an increased risk (Fig. 2).
Considering the strong links between individual NCDs (diabetes and CVDs, diabetes and cancer, diabetes and COPD), it is obvious that the same DBs are associated with different NCDs, as demonstrated in the above presented Tables 1, 2, 3, 4, and 5. Hence, the prevention strategies towards individual NCD could benefit other NCDs, as well. Simultaneously, this bears challenges for differential diagnostics based on DBs alone, as subtle differences and interdependencies between them might be crucial to distinguish between related diseases. To this end, advanced AI models leveraging multi-modal datasets could demonstrate potential [72].
By analyzing the DBs used in diabetes care, for example, healthcare practitioners and patients can detect early signs of prediabetes, such as impaired fasting glucose or postprandial hyperglycemia. However, more specific guidelines are needed on the use of CGM metrics in defining people with prediabetes, as a target population for diabetes prevention. DB-related information enables targeted interventions, including lifestyle modifications, personalized nutrition plans, and exercise regimens, to prevent or delay the onset of diabetes. DBs could be of critical importance for the prevention of other NCDs, as well.
The role of digital biomarkers in personalized medicine
Personalized medicine aims to provide tailored interventions based on an individual’s unique characteristics, including genetics and environmental factors. DBs provide real-time, comprehensive data on an individual’s physiological, behavioral, and environmental parameters, enabling healthcare practitioners to gain a holistic view of a patient’s health and develop precise and personalized care plans (Fig. 2). Adequate management of NCDs is highly individualized, considering the diverse factors influencing the overall health of a patient. An individual with diabetes may benefit from a personalized nutrition plan, exercise regimen, and medication schedule based on its real-time glucose levels, activity patterns, and genetic markers. Likewise, it is important to evaluate the individual genetic markers of a cancer patient to administer the optimal treatment.
DBs and health applications offer additional benefits beyond the individualized planning and administration of treatment regimens by a healthcare practitioner. The patient benefits directly, as devices and apps provide direct, personalized feedback providing an opportunity to enhance patients’ understanding about the consequences of their behaviors, and suggest data-guided behavior change. Furthermore, they can help to monitor and incentivize treatment compliance and provide real-time reminders to patients to take medication. Diabetes patients, for example, can wear measurement patches that continuously monitor their glucose levels and send notifications to a patient’s smartphone should the levels reach critical ranges.
The personalized recommendations can be enabled and enhanced by AI methods. By analyzing the potentially complex patterns emitted through measuring an individual’s DBs, they allow them to make personalized predictions. Consequently, these predictions can be used to offer personalized behavior recommendations, optimize medication regimens, and provide ongoing guidance and support for individuals with NCDs.
Telemedicine and digital biomarkers
Another area of DB utilization in the light of the 3PM is telemedicine. The potential of telemedicine has been demonstrated during the recent COVID-19 pandemics, and in many areas remote healthcare practices have continued even after the end of the pandemics [73, 74].
In the ever-evolving landscape of healthcare, technology has emerged as a powerful tool to enhance patient care, improve access to services, and optimize resource utilization. Telemedicine, the remote delivery of healthcare services through telecommunications technology, has revolutionized the way patients interact with their healthcare practitioners, offering a convenient and accessible alternative to traditional in-person visits [75]. Coupled with the advent of DBs, telemedicine is poised to transform the future of healthcare delivery. For example, patients with NCDs can be remotely monitored through DBs, allowing their healthcare practitioners to adjust their treatment plan as needed, potentially preventing complications and hospitalizations.
Telemedicine and DBs also play a crucial role in addressing healthcare disparities and improving access to care, particularly in underserved and rural communities. In areas where in-person healthcare practitioners are scarce, telemedicine can bridge the gap, providing patients with essential medical services from the comfort of their homes. The use of telemedicine and remote monitoring also represents an opportunity for the healthcare industry to lower its carbon footprint by reducing carbon dioxide emissions associated with travel to and from clinic-based care.
Moreover, telemedicine and DBs can promote patient engagement and empowerment (Fig. 2). By providing patients with real-time access to their health data, these technologies can foster greater self-awareness and encourage active participation in their healthcare decisions. Patients can track their progress, identify potential concerns, and communicate more effectively with their healthcare practitioners, leading to a more personalized and patient-centered approach to care. As these technologies continue to evolve, their impact on healthcare is bound to grow, paving the way for a more efficient, accessible, and patient-centered healthcare system.
Challenges and future directions
While the potential of digital biomarkers in the context of 3PM is promising, several challenges need to be addressed. Data privacy and security concerns, regulatory oversight, and standardization of data collection and analysis methods are critical considerations. Additionally, the integration of DBs into routine clinical practice requires healthcare practitioners to be adequately trained in interpreting and utilizing digital health data effectively.
Building predictive AI models that utilize DBs to enable personalized, predictive, and potentially preventive interventions is non-trivial and requires interdisciplinary expertise by leveraging modern computer science concepts and aligning them to medical challenges and regulations. Gaining regulatory approval to apply such models in routine clinical care requires dedicated clinical trials for the technology in question [71, 76]. Looking ahead, advancements in AI and ML algorithms will enable more accurate analysis and interpretation of DB data. Additionally, the integration of multiple data sources, such as genomics, proteomics, and imaging, will further enhance the predictive power of DBs [72].
Despite these challenges, the future of DBs in the management of NCDs appears promising. Ongoing research, collaborations between technology and healthcare sectors, and advancements in AI and ML algorithms are likely to enhance the accuracy, reliability, and clinical utility of DBs.
Pediatric diseases in focus of future DB-based care
There are various pediatric diseases in which DBM could be helpful, for example, asthma, which is among the most common chronic diseases of childhood; perinatal asphyxia (PA); lack of oxygen at birth; and a more severe form of PA, hypoxic-ischemia encephalopathy. PA-affected newborns are potentially predisposed to cascading pathologies per evidence including metabolic, neurodegenerative, and malignant diseases [77] as summarized in Fig. 3. Whereas pathologies caused by severe PA are relatively abundantly described, individual health risks linked to mild forms of PA are less well investigated and may act as the trigger for severe pathologies developed later on in life. Corresponding DBM approaches are urgently needed to improve healthcare with significant benefits to the society at large.
Numerous maternal health risk factors are associated with PA, including but not restricted to diabetes, preeclampsia, and uterine (rupture), placental (acute abruption), and cord events (tight nuchal cord). Prepregnancy checkup of maternal vascular status and associated phenotype is crucial for the health of mother and offspring, predictive approach, and targeted prevention [80]. Application of telemedicine is crucial for primary prevention of birth asphyxia, particularly in areas with low density of healthcare units [77]. Application of AI is essential for multi-parametric analysis and effective data interpretation in predicting and preventing PA. The 3PM concepts are summarized in Fig. 3.
Concluding remarks and outlook in the framework of 3P medicine
In Fig. 1 it is clear that wearables are a key component to DBM. How can we define “wearables”?
“Wearables” are devices, in close contact with the individual, that provide personalized information to guide and optimize prediction, prevention, diagnosis and treatment of conditions affecting the individual’s healthcare and QoL”[81].
Wearables offer two critical advantages for predictive, preventive, and personalized diagnosis and treatment:
-
(1)
Wearables provide continuous monitoring, data collection, and treatment. Given that so many human functions and disorders exhibit circadian rhythms and other variations over time, continuous monitoring is essential for accurate personalized diagnosis and treatment.
-
(2)
Data from (and interventions by) wearables are transmitted directly to the “cloud.” The advantages of bypassing the need for a patient to visit a lab or clinic or hospital for data collection are several: (a) the logistics or expense for the patient to travel to a healthcare facility can be extremely burdensome if not prohibitive; (b) the time delay if data is collected at the healthcare facility can be fatal (e.g., hypoglycemia or hyperglycemia in diabetes, cardiac arrhythmias); and (c) the limited healthcare personnel in most LMICs (and many HICs as well) make personal visits for data collection impractical if not impossible.
The advantages of wearables plus AI can be linked to predictive, preventive, and personalized medicine [82]:
-
(1)
Predictive: gathering continuous data from thousands (or millions) of individuals allows the detection of early signals of future disorders (e.g., prediabetes, early cancer detection).
-
(2)
Preventive: once predictive data are available, one can determine the interventions that will be most effective to prevent (or ameliorate) the evolution of early signs into a full-blown disorder — whether activity alterations, dietary changes, and/or medications.
-
(3)
Personalized: the individual’s data can be compared with those data from other individuals with similar healthcare backgrounds as well as with “big data” from a population numbering in the thousands if not millions. The most efficacious predictive, preventive, and treatment strategies for that individual can thus be determined.
Participatory medicine and acceptance in the population
The evolution of digital technology and data science will positively impact healthcare, providing unprecedented opportunities for improving prediction, prevention, and personalization of disease management of individuals affected by NCDs, vulnerable sub-populations, and for society at large. However, citizens’ trust becomes essential for harnessing the full potential of the new digital possibilities and realities in which there would be integration of data of different types (e.g., real-world data and clinical research data) and the use of AI-based medical device software. Participation of citizens is thus the prerequisite for fostering a new collaborative and innovative ecosystem. Currently, there is no full trust on how all the retrieved data are kept, if they are accessed securely, used appropriately and responsibly, without jeopardizing their privacy. Only when this trust is obtained, citizens will be more likely to consent to the sharing and processing their data for secondary and tertiary use in healthcare, research, and innovation.
Developing and implementing transparent and accountable data governance frameworks play a vital role in creating citizens’ trust. To create this trust, it is essential to address any misconceptions, fears, or concerns that the citizens may have about data privacy, security, and the potential misuse of their data. Hence, engagement in open dialogue, providing accessible and transparent information, and promotion of public awareness campaigns are fundamental to contribute to a better understanding of the benefits and risks associated with data sharing and with digital tool development. Furthermore, citizens should be involved in decision-making processes (Participatory medicine). The demonstration of the tangible benefits of the new digital reality, such as improvements in personalized medicine and public health, fosters empowerment, and positively influences the citizen’s perceptions and behavior. By addressing these factors, healthcare practitioners, researchers, and policy makers can create an environment of trust, ultimately leading to increased participation and support for digital health.
Data availability
Not applicable.
Code availability
Not applicable.
Abbreviations
- AFP:
-
Alpha-fetoprotein
- AHI:
-
Apnea-hypopnea index
- AI:
-
Artificial intelligence
- BRE:
-
Biorecognition element
- CBT-I:
-
Cognitive behavioral therapy for insomnia
- CEA:
-
Carcinoembryonic antigen
- CGM:
-
Continuous glucose monitoring
- COPD:
-
Chronic obstructive pulmonary disease
- CVD:
-
Cardiovascular disease
- DB:
-
Digital biomarker
- DBM:
-
Digital biomarker monitoring
- ECG:
-
Electrocardiogram
- EEG:
-
Encephalogram
- EGFR:
-
Epidermal Growth Factor Receptor
- EPMA:
-
European Association for Predictive, Preventive, and Personalized Medicine
- HE4:
-
Human epididymis protein 4
- HIC:
-
High-income countries
- HRV:
-
Heart rate variability
- LMIC:
-
Low- and middle-income countries
- ML:
-
Machine learning
- MUC16:
-
Mucin-16
- NCD:
-
Non-communicable chronic disease
- OSA:
-
Obstructive sleep apnea
- PA:
-
Perinatal asphyxia
- PPPM/3PM:
-
Predictive, preventive, and personalized medicine
- PSA:
-
Prostate-Specific Antigen
- QoL:
-
Quality of Life
- TYR:
-
Tyrosinase
References
Li Y, Hu S, Chen C, Alifu N, Zhang X, Du J, Li C, Xu L, Wang L, Dong B. Opal photonic crystal-enhanced upconversion turn-off fluorescent immunoassay for salivary CEA with oral cancer. Talanta. 2023;258:124435. https://doi.org/10.1016/j.talanta.2023.124435.
Belizário JE, Faintuch J, Malpartida MG. Breath biopsy and discovery of exclusive volatile organic compounds for diagnosis of infectious diseases. Front Cell Infect Microbiol. 2020;10:564194. https://doi.org/10.3389/fcimb.2020.564194.
Wang H, Sun J, Lu L, Yang X, Xia J, Zhang F, Wang Z. Competitive electrochemical aptasensor based on a cDNA-ferrocene/MXene probe for detection of breast cancer marker Mucin1. Anal Chim Acta. 2020;1094:18–25. https://doi.org/10.1016/j.aca.2019.10.003.
Le T, Priefer R. Detection technologies of volatile organic compounds in the breath for cancer diagnoses. Talanta. 2024;265:124767. https://doi.org/10.1016/j.talanta.2023.124767.
Chung C, Cho HJ, Lee C, Koo J. Odorant receptors in cancer. BMB Rep. 2022;55(2):72–80. https://doi.org/10.5483/BMBRep.2022.55.2.010.
Weng X, Xu X, Wang C, Lin W, Liu A, Chen W, Lin X. Genotyping of common EGFR mutations in lung cancer patients by electrochemical biosensor. J Pharm Biomed Anal. 2018;150:176–82. https://doi.org/10.1016/j.jpba.2017.12.015.
Zhou X, Liu X, Xia X, Yang X, Xiang H. Sensitive, enzyme-free and label-free electrochemical sensor for K-ras G12D point mutation detection based on double cascade amplification reaction. JEAC. 2020;870:114270. https://doi.org/10.1016/j.jelechem.2020.114270.
Torul H, Yarali E, Eksin E, Ganguly A, Benson J, Tamer U, Erdem A. Paper-based electrochemical biosensors for voltammetric detection of miRNA biomarkers using reduced graphene oxide or MoS2 nanosheets decorated with gold nanoparticle electrodes. Biosensors. 2021;11(7):236. https://doi.org/10.3390/bios11070236.
Chakraborty B, Das A, Mandal N, Samanta N, Das N, Chaudhuri CR. Label free, electric field mediated ultrasensitive electrochemical point-of-care device for CEA detection. Sci Rep. 2021;11(1):2962. https://doi.org/10.1038/s41598-021-82580-y.
Celikbas E, Ceylan AE, Timur S. Paper-based colorimetric spot test utilizing smartphone sensing for detection of biomarkers. Talanta. 2020;208:120446. https://doi.org/10.1016/j.talanta.2019.120446.
Sharma S, Zapatero-Rodríguez J, Estrela P, O’Kennedy R. Point-of-care diagnostics in low resource settings: present status and future role of microfluidics. Biosensors (Basel). 2015;5(3):577–601. https://doi.org/10.3390/bios5030577.
Bianchi V, Mattarozzi M, Giannetto M, Boni A, De Munari I, Careri M. A Self-calibrating IoT portable electrochemical immunosensor for serum human epididymis protein 4 as a tumor biomarker for ovarian cancer. Sensors (Basel). 2020;20(7):2016. https://doi.org/10.3390/s20072016.
Ciui B, Martin A, Mishra RK, Brunetti B, Nakagawa T, Dawkins TJ, Lyu M, Cristea C, Sandulescu R, Wang J. Wearable wireless tyrosinase bandage and microneedle sensors: toward melanoma screening. Adv Healthc Mater. 2018;7(7):e1701264. https://doi.org/10.1002/adhm.201701264.
Golubnitschaja O, Polivka J Jr, Potuznik P, Pesta M, Stetkarova I, Mazurakova A, Lackova L, Kubatka P, Kropp M, Thumann G, Erb C, Fröhlich H, Wang W, Baban B, Kapalla M, Shapira N, Richter K, Karabatsiakis A, Smokovski I, Schmeel LC, Gkika E, Paul F, Parini P, Polivka J. The paradigm change from reactive medical services to 3PM in ischemic stroke: a holistic approach utilising tear fluid multi-omics, mitochondria as a vital biosensor and AI-based multi-professional data interpretation. EPMA J. 2024;15(1):1–23. https://doi.org/10.1007/s13167-024-00356-6.
Barrett M, Boyne J, Brandts J, Brunner-La Rocca HP, De Maesschalck L, De Wit K, Dixon L, Eurlings C, Fitzsimons D, Golubnitschaja O, Hageman A, Heemskerk F, Hintzen A, Helms TM, Hill L, Hoedemakers T, Marx N, McDonald K, Mertens M, Müller-Wieland D, Palant A, Piesk J, Pomazanskyi A, Ramaekers J, Ruff P, Schütt K, Shekhawat Y, Ski CF, Thompson DR, Tsirkin A, van der Mierden K, Watson C, Zippel-Schultz B. Artificial intelligence supported patient self-care in chronic heart failure: a paradigm shift from reactive to predictive, preventive and personalised care. EPMA J. 2019;10(4):445–64. https://doi.org/10.1007/s13167-019-00188-9.
Schalkamp AK, Peall KJ, Harrison NA, Sandor C. Wearable movement-tracking data identify Parkinson’s disease years before clinical diagnosis. Nat Med. 2023;29:2048–56. https://doi.org/10.1038/s41591-023-02440-2.
Kurysheva NI, Rodionova OY, Pomerantsev AL, Sharova GA, Golubnitschaja O. Machine learning-couched treatment algorithms tailored to individualized profile of patients with primary anterior chamber angle closure predisposed to the glaucomatous optic neuropathy. EPMA J. 2023;14(3):527–38. https://doi.org/10.1007/s13167-023-00337-1.
Harms RL, Ferrari A, Meier IB, Martinkova J, Santus E, Marino N, Cirillo D, Mellino S, Catuara Solarz S, Tarnanas I, Szoeke C, Hort J, Valencia A, Ferretti MT, Seixas A, Santuccione CA. Digital biomarkers and sex impacts in Alzheimer’s disease management — potential utility for innovative 3P medicine approach. EPMA J. 2022;13(2):299–313. https://doi.org/10.1007/s13167-022-00284-3.
Wang W, Yan Y, Guo Z, Hou H, Garcia M, Tan X, Anto EO, Mahara G, Zheng Y, Li B, Kang T, Zhong Z, Wang Y, Guo X, Golubnitschaja O, Suboptimal Health Study Consortium and European Association for Predictive, Preventive and Personalised Medicine. All around suboptimal health — a joint position paper of the Suboptimal Health Study Consortium and European Association for Predictive Preventive and Personalised Medicine. EPMA J. 2021;12(4):403–33. https://doi.org/10.1007/s13167-021-00253-2.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, Krapfenbauer K, Mozaffari MS, Costigliola V. Medicine in the early twenty-first century: paradigm and anticipation — EPMA position paper 2016. EPMA J. 2016;7(1):23. https://doi.org/10.1186/s13167-016-0072-4.
Meier IB, Buegler M, Harms R, Seixas A, Çöltekin A, Tarnanas I. Using a Digital Neuro Signature to measure longitudinal individual-level change in Alzheimer’s disease: the Altoida large cohort study. npj Digit Med. 2021;4:101. https://doi.org/10.1038/s41746-021-00470-z.
Larkin HD. Apple watch Parkinson disease symptom monitor is cleared. JAMA. 2022;328(5):416. https://doi.org/10.1001/jama.2022.12641.
Richter K, Kellner S, Hillemacher T, Golubnitschaja O. Sleep quality and COVID-19 outcomes: the evidence-based lessons in the framework of predictive, preventive and personalised (3P) medicine. EPMA J. 2021;12(2):221–41.
Liu H, Shu F, Ji C, Xu H, Zhou Z, Wang Y, Gao H, Luo P, Zheng Y, Lv K, Xiao S. Clarifying sleep characteristics and analyzing risk factors of sleep disorders to promote a predictive, preventive, and personalized medicine in patients with burn scars. EPMA J. 2023;14(1):131–42. https://doi.org/10.1007/s13167-022-00309-x.
Kucera R, Pecen L, Topolcan O, Dahal AR, Costigliola V, Giordano FA, Golubnitschaja O. Prostate cancer management: long-term beliefs, epidemic developments in the early twenty-first century and 3PM dimensional solutions. EPMA J. 2020;11(3):399–418. https://doi.org/10.1007/s13167-020-00214-1.
Golubnitschaja O, Liskova A, Koklesova L, Samec M, Biringer K, Büsselberg D, Podbielska H, Kunin AA, Evsevyeva ME, Shapira N, Paul F, Erb C, Dietrich DE, Felbel D, Karabatsiakis A, Bubnov R, Polivka J, Polivka J Jr, Birkenbihl C, Fröhlich H, Hofmann-Apitius M, Kubatka P. Caution, “normal” BMI: health risks associated with potentially masked individual underweight—EPMA position paper 2021. EPMA J. 2021;12(3):243–64. https://doi.org/10.1007/s13167-021-00251-4.
Richter KD, Acker J, Scholz F, Niklewski G. Health promotion and work: prevention of shift work disorders in companies. EPMA J. 2010;1(4):611–8.
Bajraktarov S, Novotni A, Manusheva N, Nikovska DG, Miceva-Velickovska E, Zdraveska N. Main effects of sleep disorders related to shift work—opportunities for preventive programs. EPMA J. 2011;2(4):365–70 (u. a).
Richter K, Acker J, Kamcev N, Bajraktarov S, Piehl A, Niklewski G. Recommendations for the prevention of breast cancer in shift workers. EPMA J. 2011;2(4):351–6. https://doi.org/10.1007/s13167-011-0126-6.
Richter K, Gjorgov N, Bajraktarov S. Predictive, preventive, and personalized approach in sleep medicine. In: Podbielska H, Kapalla M, editors. Predictive, preventive, and personalised medicine: from bench to bedside. Advances in predictive, preventive and personalised medicine, vol. 17. Cham: Springer; 2023. p. 243–60. https://doi.org/10.1007/978-3-031-34884-6_14.
Spiegelhalder K, Baumeister H, Al-Kamaly A, Bader M, Bauereiss N, Benz F, et al. Comparative effectiveness of three versions of a stepped care model for insomnia differing in the amount of therapist support in internet-delivered treatment: study protocol for a pragmatic cluster randomised controlled trial (GET Sleep). BMJ Open. 2022;12(8):e058212.
Retzer L, Feil M, Reindl R, et al. Anonymous online cognitive behavioral therapy for sleep disorders in shift workers—a study protocol for a randomized controlled trial. Trials. 2021;22:539. https://doi.org/10.1186/s13063-021-05437-9.
Peter L, Reindl R, Zauter S, Hillemacher T, Richter K. Effectiveness of an online CBT-I intervention and a face-to-face treatment for shift work sleep disorder: a comparison of sleep diary data. Int J Environ Res Public Health. 2019;16(17):3081.
Acker J, Golubnitschaja O, Büttner-Teleaga A, Richter K. Wrist actigraphic approach in primary, secondary and tertiary care based on the principles of predictive, preventive and personalised (3P) medicine. EPMA J. 2021;12(3):349–63.
Săndulescu VA, Richter K. Mögliche Non-24-Schlaf-Wach-Rhythmusstörung? Somnologie. 2021;25(3):221–5.
Richter K, Penzel T. Editorial: Circadian rhythms of mental health. Front Netw Physiol. 2023;3:1279911. https://doi.org/10.3389/fnetp.2023.1279911.
Penzel T, Schöbel C, Fietze I. New technology to assess sleep apnea: wearables, smartphones, and accessories. F1000Res. 2018;7:413. https://doi.org/10.12688/f1000research.13010.1.
Chocron A, Efraim R, Mandel F, Rueschman M, Palmius N, Penzel T, Elbaz M, Behar JA. Machine learning for nocturnal mass diagnosis of atrial fibrillation in a population at risk of sleep-disordered breathing. Physiol Meas. 2020;41(10):104001. https://doi.org/10.1088/1361.
Alugubelli N, Abuissa H, Roka A. Wearable devices for remote monitoring of heart rate and heart rate variability—what we know and what is coming. Sensors (Basel). 2022;22(22):8903. https://doi.org/10.3390/s22228903.
Battelino T, Danne T, Bergenstal MR, Amiel AS, Beck R, Biester T, Bosi E, Buckingham AB, Cefalu TW, Close LK, et al. Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care. 2019;42:1593–603.
Brickwood K-J, Watson G, O’Brien J, Williams AD. Consumer-based wearable activity trackers increase physical activity participation: systematic review and meta-analysis. JMIR Mhealth Uhealth. 2019;7:e11819. https://doi.org/10.2196/11819.
Miller JD, Sargent C, Roach DG. A validation of six wearable devices for estimating sleep, heart rate and heart rate variability in healthy adults. Sensors (Basel). 2022;22(16):6317. https://doi.org/10.3390/s22166317.
Galindo JR, Ramos C, Cardona S, Vellanki P, Davis MG, Oladejo O, Albury B, Dhruv N, Peng L, Umpierrez EG. Efficacy of a smart insulin pen cap for the management of patients with uncontrolled type 2 diabetes: a randomized cross-over trial. J Diabetes Sci Technol. 2023;17(1):201–7. https://doi.org/10.1177/19322968211033837.
Gioia S, Vlasac MI, Babazadeh D, Fryou LN, Do E, Love J, Robbins R, Dashti SH, Lane MJ. Mobile apps for dietary and food timing assessment: evaluation for use in clinical research. JMIR Form Res. 2023;7:e35858. https://doi.org/10.2196/35858.
Hickey AB, Chalmers T, Newton P, Lin CT, Sibbritt D, McLachlan SC, Clifton-Bligh R, Morley J, Lal S. Smart devices and wearable technologies to detect and monitor mental health conditions and stress: a systematic review. Sensors (Basel). 2021;21(10):3461. https://doi.org/10.3390/s21103461.
Smokovski I. Burden of diabetes prevalence. In: Managing diabetes in low income countries. Cham: Springer; 2021. https://doi.org/10.1007/978-3-030-51469-3_1.
Yap MJ, Tantono N, Wu XV, Klainin-Yoba P. Effectiveness of technology-based psychosocial interventions on diabetes distress and health-relevant outcomes among type 2 diabetes mellitus: a systematic review and meta-analysis. J Telemed Telecare. 2021:1357633X211058329. https://doi.org/10.1177/1357633X211058329.
Eberle C, Löhnert M, Stichling S. Effectiveness of disease-specific mHealth apps in patients with diabetes mellitus: scoping review. JMIR Mhealth Uhealth. 2021;9(2):e23477. https://doi.org/10.2196/23477.
Beck WR, Riddlesworth T, Ruedy K, Ahmann A, Bergenstal R, Haller S, Kollman C, Kruger D, McGill BJ, Polonsky W, Toschi E, Wolpert H, Price D, DIAMOND Study Group. Effect of continuous glucose monitoring on glycemic control in adults with type 1 diabetes using insulin injections. JAMA. 2017;317(4):371–8. https://doi.org/10.1001/jama.2016.19975.
Šoupal J, Petruželková L, Flekač M, Pelcl T, Matoulek M, Daňková M, Škrha J, Svačina S, Prázný M. Comparison of different treatment modalities for type 1 diabetes, including sensor-augmented insulin regimens, in 52 weeks of follow-up: a COMISAIR study. Diabetes Technol Ther. 2016;18(9):532–8. https://doi.org/10.7326/M16-2855.
Behnke AJ, Woodfield DJ. Intensive management of poorly controlled type 2 diabetes using a multidisciplinary approach and continuous glucose monitoring. J Endocrinol Metab. 2023;13(2):70–4.
Vaduganathan M, Mensah AG, Turco VJ, Fuster V, Roth AG. The global burden of cardiovascular diseases and risk: a compass for future health. J Am Coll Cardiol. 2022;80(25):2361–71. https://doi.org/10.1016/j.jacc.2022.11.005.
Randazzo V, Ferretti J, Pasero E. Anytime ECG monitoring through the use of a low-cost, user-friendly, wearable device. Sensors (Basel). 2021;21(18):6036. https://doi.org/10.3390/s21186036.
Islam SMS, Chow KC, Daryabeygikhotbehsara R, Subedi N, Rawstorn J, Tegegne T, Karmakar C, Siddiqui UM, Lambert G, Maddison R. Wearable cuffless blood pressure monitoring devices: a systematic review and meta-analysis. Eur Heart J Digit Health. 2022;3(2):323–37. https://doi.org/10.1093/ehjdh/ztac021.
Luo H, Yang D, Barszczyk A, Vempala N, Wei J, Wu JS, Zheng PP, Fu G, Lee K, Feng ZP. Smartphone-based blood pressure measurement using transdermal optical imaging technology. Circ Cardiovasc Imaging. 2019;12:e008857. https://doi.org/10.1161/CIRCIMAGING.119.008857.
Coutu FA, Iorio CO, Ross AB. Remote patient monitoring strategies and wearable technology in chronic obstructive pulmonary disease. Front Med (Lausanne). 2023;10:1236598. https://doi.org/10.3389/fmed.2023.1236598.
Majumder S, Deen JM. Smartphone sensors for health monitoring and diagnosis. Sensors (Basel). 2019;19(9):2164.
Chan PY, Ryan NP, Chen D, McNeil J, Hopper I. Novel wearable and contactless heart rate, respiratory rate, and oxygen saturation monitoring devices: a systematic review and meta-analysis. Anaesthesia. 2022;77(11):1268–80. https://doi.org/10.1111/anae.15834.
Xue B, Shi W, Chotirmall HS, Koh CAV, Ang YY, Tan XR, Ser W. Distance-based detection of cough, wheeze, and breath sounds on wearable devices. Sensors (Basel). 2022;22(6):2167. https://doi.org/10.3390/s22062167.
Keats RM, Yu X, Magee SM, Forbes CC, Grandy AS, Sweeney E, Dummer JBT. Use of wearable activity-monitoring technologies to promote physical activity in cancer survivors: challenges and opportunities for improved cancer care. Int J Environ Res Public Health. 2023;20(6):4784. https://doi.org/10.3390/ijerph20064784.
Beauchamp UL, Pappot H, Holländer-Mieritz C. The use of wearables in clinical trials during cancer treatment: systematic review. JMIR Mhealth Uhealth. 2020;8(11):e22006. https://doi.org/10.2196/22006.
Jacobsen M, Rottmann P, Dembek AT, Gerke LA, Gholamipoor R, Blum C, Hartmann NU, Verket M, Kaivers J, Jäger P, Baermann BN, Heinemann L, Marx N, Müller-Wieland D, Kollmann M, Seyfarth M, Kobbe G. Feasibility of wearable-based remote monitoring in patients during intensive treatment for aggressive hematologic malignancies. JCO Clin Cancer Inform. 2022:e2100126. https://doi.org/10.1200/CCI.21.00126.
Majumder A, Sen D. Artificial intelligence in cancer diagnostics and therapy: current perspectives. Indian J Cancer. 2021;58(4):481–92. https://doi.org/10.4103/ijc.IJC_399_20.
Gambalunga F, Iacorossi L, Notarnicola I, Serra V, Piredda M, Marinis DGM. Mobile health in adherence to oral anticancer drugs: a scoping review. Comput Inform Nurs. 2020;39(1):17–23. https://doi.org/10.1097/CIN.0000000000000643.
Jiao Y, Lin R, Hua X, Churilov L, Gaca JM, James S, Clarke MP, O’Neal D, Ekinci IE. A systematic review: cost-effectiveness of continuous glucose monitoring compared to self-monitoring of blood glucose in type 1 diabetes. Endocrinol Diabetes Metab. 2022;5(6):e369. https://doi.org/10.1002/edm2.369.
Jendle J, Eeg-Olofsson K, Svensson AM, Franzen S, Lamotte M, Levrat-Guillen F. Cost-effectiveness of the FreeStyle Libre® system versus blood glucose self-monitoring in individuals with type 2 diabetes on insulin treatment in Sweden. Diabetes Ther. 2021;12(12):3137–52. https://doi.org/10.1007/s13300-021-01172-1.
Hayek AM, Giannouchos T, Lawley M, Kum HC. Economic evaluation of blood pressure monitoring techniques in patients with hypertension: a systematic review. JAMA Netw Open. 2023;6(11):e2344372.
Cochrane Airways Group, Janjua S, Carter D, Threapleton JDC, Prigmore S, Disler TR. Telehealth interventions: remote monitoring and consultations for people with chronic obstructive pulmonary disease (COPD). Cochrane Database Syst Rev. 2021;2021(7):CD013196. https://doi.org/10.1002/14651858.CD013196.pub2.
Tomasic I, Tomasic N, Trobec R, Krpan M, Kelava T. Continuous remote monitoring of COPD patients—justification and explanation of the requirements and a survey of the available technologies. Med Biol Eng Comput. 2018;56(4):547–69. https://doi.org/10.1007/s11517-018-1798-z.
Fountzilas E, Tsimberidou AM, Vo HH, Kurzrock R. Clinical trial design in the era of precision medicine. Genome Med. 2022;14(1):101. https://doi.org/10.1186/s13073-022-01102-1.
Birkenbihl C, Emon MA, Vrooman H, Westwood S, Lovestone S, AddNeuroMed Consortium, Hofmann-Apitius M, Fröhlich H, Alzheimer’s Disease Neuroimaging Initiative. Differences in cohort study data affect external validation of artificial intelligence models for predictive diagnostics of dementia — lessons for translation into clinical practice. EPMA J. 2020;11(3):367–76. https://doi.org/10.1007/s13167-020-00216-z.
Powell D. Walk, talk, think, see and feel: harnessing the power of digital biomarkers in healthcare. npj Digit Med. 2024;7:45. https://doi.org/10.1038/s41746-024-01023-w.
Smokovski I, Srceva MJ, Petkovska L, Golubnitschaja O. Critical role of telemedicine as a platform for predictive, preventive, and personalized diabetes care during the COVID-19 pandemics. In: Podbielska H, Kapalla M, editors. Predictive, preventive, and personalised medicine: from bench to bedside. Advances in predictive, preventive and personalised medicine, 2013;17:129–39. Cham: Springer. https://doi.org/10.1007/978-3-031-34884-6_8.
Bhaskar S, Nurtazina A, Mittoo S, Banach M, Weissert R. Editorial: Telemedicine during and beyond COVID-19 Front. Public Health. 2021;9:662617. https://doi.org/10.3389/fpubh.2021.662617.
Dugas M, Crowley K, Gao GG, Xu T, Agarwal R, Kruglanski WA, Steinle N. Individual differences in regulatory mode moderate the effectiveness of a pilot mHealth trial for diabetes management among older veterans. PLoS ONE. 2018;13(3):e0192807. https://doi.org/10.1371/journal.pone.0192807.
Fröhlich H, Balling R, Beerenwinkel N, Kohlbacher O, Kumar S, Lengauer T, Maathuis MH, Moreau Y, Murphy SA, Przytycka TM, Rebhan M, Röst H, Schuppert A, Schwab M, Spang R, Stekhoven D, Sun J, Weber A, Ziemek D, Zupan B. From hype to reality: data science enabling personalized medicine. BMC Med. 2018;16(1):150. https://doi.org/10.1186/s12916-018-1122-7.
Golubnitschaja O, Yeghiazaryan K, Cebioglu M, Morelli M, Herrera-Marschitz M. Birth asphyxia as the major complication in newborns: moving towards improved individual outcomes by prediction, targeted prevention and tailored medical care. EPMA J. 2011;2(2):197–210. https://doi.org/10.1007/s13167-011-0087-9.
Peeva V, Yeghiazaryan K, Golubnitschaja O. Birth asphyxia as the most frequent perinatal complication. In: Golubnitschaja O, editor. Predictive diagnostics and personalized treatment: Dream or reality. New York: Nova Science Publishers; 2009;499–507.
Yeghiazaryan K, Peeva V, Morelli M, Herrera-Marschitz M, Golubnitschaja O. Potential targets for early diagnosis and neuroprotection in asphyxiated newborns. In: Golubnitschaja O, editor. Predictive diagnostics and personalized treatment: dream or reality. New York: Nova Science Publishers; 2009;509–25.
Evsevieva M, Sergeeva O, Mazurakova A, Koklesova L, Prokhorenko-Kolomoytseva I, Shchetinin E, Birkenbihl C, Costigliola V, Kubatka P, Golubnitschaja O. Pre-pregnancy check-up of maternal vascular status and associated phenotype is crucial for the health of mother and offspring. EPMA J. 2022;13(3):351–66. https://doi.org/10.1007/s13167-022-00294-1.
Andrews RJ. Wearable revolution: Predictive, preventive, personalized medicine (PPPM) par excellence. In: Podbielska H, Kapalla M, editors. Predictive, preventive, and personalised medicine: from bench to bedside. Advances in predictive, preventive and personalised medicine, 2023;17:339–48. Cham: Springer. https://doi.org/10.1007/978-3-031-34884-6_19.
Shajari S, Kuruvinashetti K, Komeili A, Sundararaj U. The emergence of AI-based wearable sensors for digital health technology: a review. Sensors. 2023;23:9498. https://doi.org/10.3390/s23239498.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
I.S. and O.G. were responsible for conception of the manuscript and project’s coordination. The manuscript was written by I.S., N.S., A.B., S.B., G.G., K.R., G.N., C.B., P.P., R.J.A., H.B., and O.G. Images were created by C.B. and O.G. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Disclaimer
O. G. is the Editor-in-Chief of the journal, but was not involved in, did not influence over, nor accessed to the details of the peer review process of this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Smokovski, I., Steinle, N., Behnke, A. et al. Digital biomarkers: 3PM approach revolutionizing chronic disease management — EPMA 2024 position. EPMA Journal 15, 149–162 (2024). https://doi.org/10.1007/s13167-024-00364-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-024-00364-6
Keywords
- Digital biomarkers
- Non-communicable chronic disease
- Health risk assessment
- Health-to-disease transition
- Health protection
- Health economy and policy
- Artificial intelligence
- Machine learning
- Wearable point-of-care devices
- Innovative ecosystem
- Sleep disorders
- Diabetes
- Cardiovascular diseases
- Chronic obstructive pulmonary disease
- Cancer
- Perinatal asphyxia
- Predictive Preventive Personalized Medicine
- PPPM / 3PM
- Primary and secondary care