Abstract
Background
Population aging is a global public health issue involving increased prevalence of age-related diseases, and concomitant burden on medical resources and the economy. Ninety-two diseases have been identified as age-related, accounting for 51.3% of the global adult disease burden. The economic cost per capita for older people over 60 years is 10 times that of the younger population. From the aspects of predictive, preventive, and personalized medicine (PPPM), developing a risk-prediction model can help identify individuals at high risk for all-cause mortality and provide an opportunity for targeted prevention through personalized intervention at an early stage. However, there is still a lack of predictive models to help community-dwelling older adults do well in healthcare.
Objectives
This study aims to develop an accurate 1-, 3-, 5-, and 8-year all-cause mortality risk-prediction model by using clinical multidimensional variables, and investigate risk factors for 1-, 3-, 5-, and 8-year all-cause mortality in community-dwelling older adults to guide primary prevention.
Methods
This is a two-center cohort study. Inclusion criteria: (1) community-dwelling adult, (2) resided in the districts of Chaonan or Haojiang for more than 6 months in the past 12 months, and (3) completed a health examination. Exclusion criteria: (1) age less than 60 years, (2) more than 30 incomplete variables, (3) no signed informed consent. The primary outcome of the study was all-cause mortality obtained from face-to-face interviews, telephone interviews, and the medical death database from 2012 to 2021. Finally, we enrolled 5085 community-dwelling adults, 60 years and older, who underwent routine health screening in the Chaonan and Haojiang districts, southern China, from 2012 to 2021. Of them, 3091 participants from Chaonan were recruited as the primary training and internal validation study cohort, while 1994 participants from Haojiang were recruited as the external validation cohort. A total of 95 clinical multidimensional variables, including demographics, lifestyle behaviors, symptoms, medical history, family history, physical examination, laboratory tests, and electrocardiogram (ECG) data were collected to identify candidate risk factors and characteristics. Risk factors were identified using least absolute shrinkage and selection operator (LASSO) models and multivariable Cox proportional hazards regression analysis. A nomogram predictive model for 1-, 3-, 5- and 8-year all-cause mortality was constructed. The accuracy and calibration of the nomogram prediction model were assessed using the concordance index (C-index), integrated Brier score (IBS), receiver operating characteristic (ROC), and calibration curves. The clinical validity of the model was assessed using decision curve analysis (DCA).
Results
Nine independent risk factors for 1-, 3-, 5-, and 8-year all-cause mortality were identified, including increased age, male, alcohol status, higher daily liquor consumption, history of cancer, elevated fasting glucose, lower hemoglobin, higher heart rate, and the occurrence of heart block. The acquisition of risk factor criteria is low cost, easily obtained, convenient for clinical application, and provides new insights and targets for the development of personalized prevention and interventions for high-risk individuals. The areas under the curve (AUC) of the nomogram model were 0.767, 0.776, and 0.806, and the C-indexes were 0.765, 0.775, and 0.797, in the training, internal validation, and external validation sets, respectively. The IBS was less than 0.25, which indicates good calibration. Calibration and decision curves showed that the predicted probabilities were in good agreement with the actual probabilities and had good clinical predictive value for PPPM.
Conclusion
The personalized risk prediction model can identify individuals at high risk of all-cause mortality, help offer primary care to prevent all-cause mortality, and provide personalized medical treatment for these high-risk individuals from the PPPM perspective. Strict control of daily liquor consumption, lowering fasting glucose, raising hemoglobin, controlling heart rate, and treatment of heart block could be beneficial for improving survival in elderly populations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Population aging is an important public health issue
Population aging is a global phenomenon. The number of people over the age of 60 years was 600 million in 2000 and is expected to be 2 billion worldwide in 2050 [1]. Population aging increased the prevalence of age-related diseases and a concomitant burden on medical resources and the economy. Ninety-two diseases have been identified as age-related, accounting for 51.3% of the global adult disease burden [2]. Among individuals over 60 years old, 75.8% have at least one chronic disease, 58.3% have hypertension, 19.4% have diabetes, and 10.5% have hypercholesterolemia, which often reduces the quality of life and life expectancy [3]. The economic cost per capita for older people over 60 years was 10 times that of the younger population [4]. Early intervention may improve prognosis and extend life expectancy for older adults [5]. Current healthcare strategies mainly involve reactive medicine, which is a delayed intervention approach in response to already existing clinical signs and symptoms, and which leads to high cost of most medical services and high long-term mortality [6]. To improve this phenomenon, in the framework of predictive, preventive, personalized medicine, physicians and scientists are trying to transform the paradigm from delayed reactive medicine to proactive medicine by developing risk-prediction models and screening for risk factors in community-dwelling older adults by using clinical multidimensional variables.
Development of an all-cause mortality prediction model for the elderly in the framework of PPPM
Predictive preventive personalized medicine (PPPM) is an integrative approach that mainly contains three aspects: individual predisposition prediction, targeted preventive measures, and personalized treatment algorithms [7]. The European Association for Predictive, Preventive and Personalized Medicine (EPMA) has proposed the concept of anti-aging that pays much attention to preventive healthcare measures, rather than hospital-based medicine [5]. In view of the aging populations, a PPPM approach in health care systems is critical for keeping the quality of health care on a global scale [8]. Following the concept of PPPM, developing an effective risk-prediction model to recognize high-risk individuals early, providing targeted prevention, and carrying out personalized treatment are important for community-dwelling older adults. However, prior studies mainly focus on hospitalized patients with pronounced symptoms [9,10,11]. Many community-dwelling older adults suffer from at least one chronic disease, but without obvious symptoms, which leads to delayed diagnosis and personalized treatment. Community-dwelling older adults also often fail to recognize risk factors of long-term mortality and easily ignore proactive prevention management. Demographic variables, comorbid conditions, lifestyle behaviors, laboratory-based molecular patterns, and electrocardiogram indices have been reported to be independently associated with long-term mortality [12,13,14,15,16]. Multidimensional clinical data integrating all these factors may improve the accuracy of predictive models. However, this has not been fully considered. Therefore, we integrated multidimensional clinical data, developed a risk prediction model, and identified risk factors for 1-, 3-, 5-, and 8-year all-cause mortality, providing targeted prevention and individual treatment for community-dwelling older adults, based on the identified risk factors, in the framework of PPPM.
Working hypothesis
It is hypothesized that an early application PPPM approach would contribute to the healthcare of older adults. Compared to a separate questionnaire, the clinical multidimensional variables add an electrocardiogram (ECG) and clinical laboratory examination, which reflect the characteristics of the participants more comprehensively and objectively. In this study, we predict that an accurate all-cause mortality risk-prediction model can be developed using clinical multidimensional variables for community-dwelling older adults. Such a model would add value to personalized medicine for community-dwelling older adults by enabling PPPM. To test our hypothesis, we developed and externally validated a nomogram prediction model. AUC, C-index, IBS, and calibration curves were used to evaluate the discriminatory and calibration abilities of the nomogram. Decision curve analysis was used to assess the clinical utility of the nomogram.
Methods
Participants and sampling methods
A two-center cohort study was established in 2012 by the First Affiliated Hospital of Shantou University Medical College in Shantou, Guangdong Province, southern, China. We used a multi-stage, stratified cluster sampling method, and selected two out of seven districts (counties) in the Shantou City, namely, the Haojiang and Chaonan districts. Forty-five communities in the Chaonan district and thirty-two communities in the Haojiang district were selected. A health census was carried out in these communities for the whole population over 18 years of age. Populations meeting inclusion and exclusion criteria were included in the final analysis. Inclusion criteria: (1) community-dwelling adult, (2) resided in the districts of Chaonan or Haojiang for more than 6 months in the past 12 months, and (3) completed a health examination. Exclusion criteria: (1) age less than 60 years, (2) more than 30 incomplete variables, (3) no signed informed consent. This study was in accordance with the principles of the Declaration of Helsinki and approved by the Ethics Committee of the First Affiliated Hospital of Shantou University Medical College (NO: SDFY-EC-SOP-004–3.0-A06).
Data collection
The demographic characteristics, lifestyle behaviors, symptoms, medical history, and family history were collected via a standardized questionnaire by trained medical personnel. The information included age, gender, alcohol status, smoking status, daily liquor consumption, and history of cancer. Physical examinations were performed by trained physicians, who provided patient information including height, weight, waist circumference (WC), hip circumference (HC), waist-to-hip ratio (WHR), and systolic and diastolic blood pressures (SBP; DBP). WC was measured immediately above the iliac crest and HC at the maximal circumference of the buttocks, both in centimeters (cm). WHR was calculated by dividing WC by HC. SBP and DBP were presented as the average of three measurements on the right arm using a sphygmomanometer after resting for at least 10 min. BMI was calculated as weight (kg) divided by the square of the height (cm2).
Blood samples were collected from participants who had fasted for at least 10 h overnight and were analyzed within 2 h of collection for multiple indicators, including white blood cell counts (WBC), red blood cell counts (RBC), hemoglobin, percentage of monocytes, percentage of lymphocytes, fasting glucose, high-density lipoprotein (HDL), low-density cholesterol (LDL), and creatinine in the clinical laboratory of the First Affiliated Hospital of Shantou University Medical College. The study strictly followed standard laboratory protocols and procedures.
An electrocardiogram (ECG) examination was conducted using a standard 12-lead ECG (NIHON KOHDEN ECG-1350p), by technical staff. A standard 12-lead ECG, whose frequency response characteristics were in accordance with American Heart Association recommendations, was recorded at 25 mm/s and 0.1 mv/mm standardization during quiet respiration [17]. All ECG parameters, including heart rate, P-wave duration (PWD), R wave in V5 voltage (RV5), and S wave in V1 voltage (SV1) were acquired from the ECG database. Overall, a total of 95 variables were collected for the analysis (Supplementary Material Table s1).
Outcome evaluation
Follow-up visits for outcomes were conducted annually over 8 years from 2012 to 2021, including face-to-face interviews and telephone interviews, and death was verified from the medical death database. The primary outcome of the study was all-cause death.
Feature selection
We interpolated the data of Chaonan and Haojiang districts by using R multivariate imputation, respectively. There was no information leakage between these two districts. Variables with more than 30% missing were deleted without interpolation. The rates of missing data for the Chaonan district are shown in the supplementary material (Table s2). The 3091 individuals from Chaonan were randomly divided into two groups after data interpolation, where 75% (n = 2318) of participants were allocated to the training set, and the remaining 25% (n = 773) were allocated to the internal validation set. The rates of missing data for Haojiang district are shown in the supplementary material (Table s3). There were 1994 individuals from Haojiang who were recruited as the external validation set. The prediction model was developed using the training set. Feature selection was conducted by least absolute shrinkage and selection operator (LASSO) and multivariable Cox proportional-hazards regression analysis.
Model development and evaluation
Based on LASSO-Cox analyses, independent risk features were selected and incorporated into the nomogram prediction model for 1-, 3-, 5-, and 8-year all-cause mortality. The validity of the nomogram prediction model was then assessed through an internal validation set and an external validation set. The two sets shared similar characteristics with the training set, as shown in Table 1 and Supplementary Material Table s4. AUC, C-index, IBS, and the calibration curves were used to evaluate the discriminatory and calibration abilities of the nomogram. Decision curve analysis was performed to assess the clinical usefulness of the nomogram. We calculated the risk scores according to the formula (risk score = coefficient 1 * variable 1 + coefficient N * variable N). According to the optimum cut-off for risk score, participants were divided into low-risk and high-risk groups [18]. Kaplan–Meier survival curves were used to describe the risk stratification. Finally, to facilitate clinical work, a corresponding web calculator was established to present and help understand the nomogram prediction model.
Statistical analysis
All statistical analyses were conducted with R software (version 4.1.0; R Foundation for Statistical Computing, Vienna, Austria). The optimum cut-off value for the risk score was calculated by X-tile software version 3.6.1 [18]. The characteristics of all skewed distributed continuous variables are presented as the median and interquartile range (IQR) determined by Mann–Whitney U tests. Categorical variables are presented as numbers and percentages, and analyzed by the chi-square test or Fisher’s exact test. Differences with a two-sided p-value less than 0.05 were considered statistically significant. The chained equation (MICE) package was used to deal with continuous missing variables [19]. The “glmnet” package was used for the LASSO algorithms [20]. The “survminer” (https://rpkgs.datanovia.com/survminer/) and “survival” packages (https://github.com/therneau/survival) were used for Cox proportional hazard regression analysis and Kaplan–Meier curves [21]. The nomogram and calibrated curve were generated with the “rms” package (https://cran.r-project.org/web/packages/rms/). The web calculator was developed using the “DynNom” package [22].
Results
Baseline characteristics of participants
There were 15,057 participants in Chaonan who completed the health examination. Excluded subjects were 332 participants who refused to sign the informed consent form, 750 participants who dropped out of follow-up, 562 participants who had more than 30 data variables missing, and 10,322 participants who were younger than 60 years old. The 3091 participants from Chaonan were included in the training and internal validation sets. Another 1994 individuals from Haojiang were used for the external validation set. Ultimately, a total of 5085 participants were included in the final analysis and followed up for 16,432 person years (Fig. 1). The baseline characteristics of the participants in the training and internal validation sets are shown in Table 1. All-cause death occurred in 370 of the 3091 Chaonan participants during follow-up (11.97%, 192 males, and 178 females). All-cause death occurred in 138 of 1994 Haojiang residents in the external validation set (6.92%, 75 males and 63 females). The baseline characteristics of the external validation set are shown in Supplementary Material Table s2.
Feature selection
LASSO was performed on the training set (N = 2318, variables = 95). From the LASSO coefficient profiles of the 95 variables and tenfold cross-validation for tuning parameter selection in the LASSO model, twenty-five features were selected from the training set: age, gender, BMI, anhelation, sour regurgitation, smoking status, alcohol status, daily beer consumption, daily liquor consumption, stroke sequelae, WBC, hemoglobin, percentage of monocytes, percentage of lymphocytes, fasting glucose, LDL, creatinine, coronary heart disease, history of cancer, family history of cancer, heart rate, heart block, RV5, SV1, and PWD (Fig s1a and b). In the multivariable Cox proportional-hazards regression analysis, nine potential predictors were selected based on the hazard ratios (95% CI) and p-values. The nine predictive factors that were selected involved two demographic characteristics (age and gender), two lifestyle behavioral features (alcohol status and daily liquor consumption), one medical history feature (history of cancer), two laboratory-based measures (fasting glucose and hemoglobin), and two ECG parameters (heart rate and heart block) (Table 2). For the training set, The LASSO-Cox AUC and C-index were 0.793 (95% CI 0.765–0.822) and 0.792 (95% CI 0.763–0.821), respectively. For the internal validation set, the corresponding results were 0.800 (95% CI 0.751–0.849) and 0.828 (95% CI 0.785–0.871). We found good agreement between the AUC and C-index. The IBSs of these two sets were less than 0.25, which demonstrated their good calibration (Supplementary Material Table s5).
Nomogram prediction model
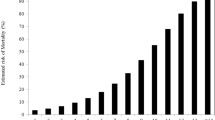
As shown in Fig. 2, a nomogram prediction model for predicting 1-, 3-, 5-, and 8-year all-cause mortality among community-dwelling older adults was developed based on the nine potential predictors. Each predictor was assigned a weighted value, and the total points were calculated from the sum of all potential predictors in the nomogram corresponding to a probability of survival at different times. For the training set, internal validation set, and external validation set, the nomogram AUC was 0.767 (95% CI 0.736–0.798), 0.776 (95% CI 0.722–0.831), and 0.806 (95% CI 0.768–0.845); the C index was 0.765 (95% CI 0.733–0.797), 0.775 (95% CI 0.719 –0.831), and 0.797 (95% CI 0.76–0.834); and the IBS was 0.079 (95% CI 0.037–0.123), 0.076 (95% CI 0.045–0.108), and 0.047 (95% CI 0.012–0.083), respectively (Table 3). The AUC and C-index were in good agreement, suggesting that the nomogram model has high predictive ability. The IBSs were less than 0.25, which demonstrated their good calibration. In the training cohort, the AUC values of the nomogram model for 1-, 3-, 5-, and 8-year all-cause mortality were 0.741, 0.769, 0.780, and 0.722, respectively. In both the internal and external validation sets, the AUC values at different time points were greater than 0.750, indicating that the model has good predictive capability (Fig. 3). The calibration curves showed different survival probabilities, predicted by the nomogram, and actual survival (Fig. 4). These results demonstrate that the nomogram prediction model had good predictive and good calibration capabilities. The decision curve analysis (DCA) of the nomogram is shown in Fig. 5. For a given probability threshold, the greater the net benefit of the model, the better. The DCA showed that the use of the nomogram could have a positive net benefit. To facilitate clinical work, a corresponding web calculator was established to present and help understand the prediction model (https://sdfysqjc2021.shinyapps.io/DynNomapp/).
Nomogram for predicting 1-, 3-, 5-, and 8-year mortality in community-dwelling older adults. The corresponding value is found on each variable axis of the nomogram, and then a red line and dots are drawn upward to determine the points received by each variable, the sum of these points is located on the total points axis, and a line is drawn downward to the survival axes to determine the probability of 1-, 3-, 5-, and 8-year mortality in community-dwelling older adults. For instance, if a patient was a 70-year-old male, with no history of cancer, who formerly drank alcohol, and had a current liquor consumption of 0 ml/day, hemoglobin 132 g/L, glucose 6.43 mmol/L, heart rate 86 beats/minute, and no heart block, he would have a total of 322 points. This participant would be predicted to have an approximately 96.5% probability of survival at 1 year, 85.8% probability of survival at 3 years, 72.6% probability of survival at 5 years, and 40% probability of survival at 8 years
ROC curves of the nomogram for 1-, 3-, 5-, and 8-year all-cause mortality in a community-dwelling older adult cohort in the training set (a), internal validation set (b), and external validation set (c). a In the training set, the AUCs of the nomogram for 1-, 3-, 5-, and 8-year all-cause mortality were 0.741, 0.769, 0.780, and 0.722, respectively. b In the internal validation set, the AUCs of the nomogram for 1-, 3-, 5-, and 8-year all-cause mortality were 0.794, 0.768, 0.778, and 0.806, respectively. c In the external validation set, the AUCs of the nomogram for 1-, 2-, 3-, and 4-year all-cause mortality were 0.803, 0.797, 0.809, and 0.751, respectively
Calibration curves showing how close the nomogram-predicted probability is to the actual probability regarding predicting all-cause mortality in the training set (a), internal validation set (b), and external validation set (c). a Calibration curves for 1-, 3-, 5-, and 8-year survival probability for community-based older residents in the training set. b Calibration curves for 1-, 3-, 5-, and 8-year survival probability for community-based older residents in the internal validation set. c Calibration curves for 1-, 2-, 3-, and 4-year survival probability for community-based older residents in the external validation set. The X-axis is the nomogram-predicted probability; the Y-axis is the observed probability. The dashed blue line represents perfect prediction. The solid red line represents the nomogram performance. The solid red lines above or below the blue dashed line represent an underestimation or overestimation, respectively. The closer the solid red line is to the dashed blue line, the better the prediction by the nomogram
Decision curve analysis of the nomogram for all-cause mortality in the training set (a), internal validation set (b), and external validation set (c). The black line represents the net benefit when no participant was considered to exhibit death, while the gray line represents the net benefit when all participants were considered to exhibit death. The area among the model curve, “non-treated line” (black line) and “treated line” (gray line), represents the clinical usefulness of the model. The further the nomogram model curve is from these two lines (the grey and black lines), the higher the clinical value
Risk stratification
Based on the LASSO-Cox model, we calculated the risk score as follows: Risk score = 0.084 * age − 0.431 * gender (female) + 0.477 * alcohol status (former) + 0.007 * daily liquor consumption − 0.018 * hemoglobin + 0.073 * fasting glucose + 1.342 * history of cancer + 0.462 * heart block + 0.009 * heart rate. The risk score of participants ranged from 2.1 to 7.3, and the optimal cut-off was 4.7. According to the optimum cut-off, people were divided into a low-risk group (risk score ≤ 4.7) and a high-risk group (risk score > 4.7) (Supplementary Material Fig s2). Kaplan–Meier curves showed that the low-risk group exhibited higher survival than the high-risk group both in the training, internal validation, and external validation sets (Supplementary Material Fig s3).
Discussion
Summary of the important findings
In this cohort study, we adopted an integrated PPPM approach using multidimensional data to develop and validate a personalized risk model predicting 1-, 3-, 5-, and 8-year all-cause mortality for community-dwelling older adults. Nine risk factors were identified, i.e., increased age, male, alcohol status, higher daily liquor consumption, history of cancer, elevated fasting glucose, lower hemoglobin, higher heart rate, and the occurrence of heart block. The AUC and C-index show high precision of the nomogram model. The lower IBS and calibration curves suggest that the nomogram prediction model exhibits good calibration. Moreover, DCA suggests that the nomogram has a positive net benefit. Our model provides accurate predictions within diverse community-based elderly populations, aiding in the identification of individuals at high risk of mortality and facilitating early interventions for mortality prevention. This model holds significant potential for influencing healthcare and policy formulation for the elderly, fostering the development of personalized preventive and interventional strategies. Our estimations serve as valuable tools in clinical discussions, assisting in informed decision-making, with an emphasis on considering life expectancy in treatment decisions [23]. Through this research, our aim is to propel the shift of healthcare models from traditional treatments towards a more proactive and preventive approach, ultimately enhancing the quality of life for the elderly and reducing all-cause mortality.
An all-cause mortality prediction model for the elderly
This model holds tremendous potential in the realms of prediction, prevention, and personalized medicine for the elderly, particularly as the global elderly population continues to grow, posing challenges to healthcare resources and economic burdens. Prior research mainly focuses on exploring the progress and prognosis of the disease to reduce mortality [24, 25]. However, few studies have predicted all-cause mortality in community-dwelling older adults. For these hospitalized elderly patients who have significant symptoms, the current healthcare outcomes are considered inadequate. Compared with previous reactive medicine, PPPM is a new integrative paradigm that focuses on predicting and preventing disease before the onset of symptoms, as well as providing personalized treatment and focuses on proactive preventative measures [7]. All-cause mortality prediction, targeted prevention, and intervention before the onset of symptoms are important and could improve the quality of life and extend life expectancy. Previous all-cause mortality prediction models for community populations have been developed in Europe, but their prediction indicators are limited in demographic variables, comorbid conditions, and lifestyle behaviors [26,27,28,29]. The participants of these studies were not limited to community-dwelling older adults, and also included young and middle-aged adults, and none of these models underwent external validation [26,27,28,29]. There is especially a lack of studies to predict all-cause mortality for community-dwelling older adults in China. To solve this problem, we developed an all-cause mortality risk prediction model in community-dwelling older adults to identify individuals on the basis of individual heterogeneity following the concept of PPPM. To the best of our knowledge, this is the first study using clinical multidimensional variables to develop and validate a nomogram prediction model, with external validation, for 1-, 3-, 5-, and 8-year all-cause mortality among community-dwelling older adults. Our study fills a gap, in the framework of PPPM, for all-cause mortality prediction with multidimensional data and external validation to provide targets for proactive prevention and individual management in personalized medicine of community-dwelling older adults. This easy-to-use prediction model can easily identify elderly people at high risk of all-cause mortality, guide-targeted prevention, provide personalized interventions for high-risk individuals, and promote a paradigm shift from delayed reactive medicine to proactive medicine. Our risk-prediction model can help generate a tailored, targeted PPPM approach that benefits both individuals and healthcare systems.
Risk factors and targets provide insights for prediction prevention and intervention
Our prediction model helps identify people at high mortality risk for all-cause mortality. However, early prediction may have little effect if effective interventions are not implemented. In this direction, we identified nine risk factors from clinical multidimensional data, including three nonmodifiable (increased age, male, and history of cancer) and six modifiable (alcohol status, daily liquor consumption, elevated fasting glucose, lower hemoglobin, higher heart rate, and the occurrence of heart block) risk factors. The identified risk factors are common and easily obtained in clinical work at low cost, which makes it convenient to use in early personal prevention and interventions for high-risk individuals.
Although the three nonmodifiable risk factors cannot be used for prevention and intervention, there is an important role in prediction for the identification of people at high risk of all-cause mortality. Our study found that increased age was an independent risk factor for all-cause mortality, which is consistent with the previous models [28, 29]. Advanced age may lead to multi-system functional decline, including the immune system, and cardiovascular, metabolic, autoimmune, and neurodegenerative diseases [30], thereby increasing the risk of all-cause mortality. Healthcare professionals should prioritize assessing all-cause mortality risk in elderly patients and implement interventions, such as health assessments, chronic disease management, and promotion of healthy lifestyles, to enhance longevity and quality of life. In our study, male gender had a higher risk of all-cause mortality, which is consistent with the previous models [28, 29]. This gender difference may be attributable in part to differences in lifestyle and behavioral risk factors (e.g. inadequate diet, physical inactivity, tobacco use, and excessive alcohol use), and psychosocial and environmental exposures [31]. Identifying male gender as a risk factor for all-cause mortality helps healthcare professionals to better identify high-risk individuals. It also provides a basis for developing gender-specific interventions to reduce all-cause mortality. We also found that a history of cancer is an independent risk factor for all-cause mortality, which is consistent with the previous studies [28]. Psychosocial stress of cancer survivors may lead to dysregulated immune function and induce chronic inflammation [32]. In addition, some cancer treatments may be cardiotoxic, resulting in cardiovascular disease being the second leading cause of morbidity and mortality in cancer survivors, after recurrent malignancies [33]. Healthcare professionals should pay more attention to all-cause mortality risks for the elderly with a history of cancer. The health and psychosocial stress of cancer survivors should be regularly assessed, and interventions should be made at an early stage to improve their quality of life and extend their life expectancy.
The six modifiable risk factors are beneficial for providing targets for prediction, prevention, and intervention at early stages in high-risk individuals. Heavy alcohol consumption is associated with the risk of fall [34] and cardiovascular disease [35], potentially increasing the cost of unnecessary hospitalization. In our study, we found that high, daily liquor consumption and alcohol status were predictors of all-cause mortality. However, the relationship between alcohol consumption and all-cause mortality may be complex. Continued heavy alcohol use can cause substantial morbidity and mortality from all causes, cancer, and accidents [36]. Light and moderate alcohol consumption have been inversely associated with mortality from all causes, cardiovascular disease, chronic lower respiratory tract diseases, Alzheimer’s disease, and influenza and pneumonia [37]. Clarifying the relationship between alcohol status and higher daily liquor consumption and all-cause mortality can help healthcare professionals better advise their patients. Strict control of daily liquor consumption is a good behavior that will avoid unnecessary hospitalizations and long-term care.
Elevated fasting glucose, whether incident, persistent, or due to diabetes, confers a higher risk of mortality [38]. For patients with diabetes mellitus, a good control of glucose facilitates the reduction of short- and long-term complications, reduces the burden of treatment, and improves quality of life [39]. Our findings emphasize the potential impact of high fasting glucose levels to increase all-cause mortality in older adults. Hyperglycemic states may trigger several physiological and metabolic changes, such as inflammation, oxidative stress, and vascular dysfunction, which may contribute to the onset and progression of multiple chronic diseases [40]. Healthcare professionals should closely monitor blood glucose levels in older patients and intervene as necessary to reduce long-term complications and mortality. This may include maintaining normal blood glucose levels through an improved diet, increased physical activity, medication, or other interventions.
Low hemoglobin, an indicator of anemia, is very common in the older population and is associated with reduced quality of life and increased mortality [41]. It is also strongly associated with more frequent hospitalization and longer hospital stays [42]. Even mild anemia may substantially affect physical and cognitive capacities and quality of life [42]. In our study, a low hemoglobin level was clearly identified as an independent factor associated with all-cause mortality, which is consistent with the previous studies [43]. Low hemoglobin levels may influence the risk of all-cause mortality through mechanisms that reduce oxygen supply, increase cardiovascular burden, and impair immune function. Clinicians should pay special attention to hemoglobin levels in elderly patients and take the necessary steps to correct the low hemoglobin state, including complementary therapies (iron, vitamin B12 or folic acid supplementation, use of erythropoietic drugs) [42] or elimination of the underlying cause to correct the anemia, thereby improving oxygen supply and reducing the risk of all-cause mortality.
Higher heart rates have been reported to be associated with an increased risk of dementia and accelerated rates of cognitive decline in the general elderly population, which can affect the quality of life in older adults [44]. Our findings found that high heart rate is an important risk factor in the increased risk of all-cause mortality in older adults. Previous studies also indicated that accelerated heart rate increases the risk of sudden cardiac death, heart failure, and all-cause mortality [45]. Higher heart rates in patients with stable coronary heart disease raise the risk of complications, even when other factors are under control [46]. Keeping the heart rate of the elderly in the normal range contributes to improved quality of life and survival rates. Clinicians should closely monitor heart rate levels in older patients and take the necessary measures to control high heart rates. This may include heart rhythm medication, physical activity, and measures to improve cardiovascular health.
Our findings show that heart block is associated with a risk of all-cause mortality in older adults. In this study, the heart block includes an atrioventricular block, right bundle branch block, and left bundle branch block. An atrioventricular block is associated with heart failure, atrial fibrillation, and all-cause mortality [47]. Patients with right bundle branch block are more likely to have congestive heart failure, cardiogenic shock, hypertension, and ventricular tachyarrhythmias [48]. The left bundle branch block reduces left ventricular ejection fraction, which is an unfavorable prognostic parameter in patients with congestive heart failure [49]. Heart block may decrease the heart’s perfusion, systolic and diastolic function, and hemodynamics [50]. These lead to an increased risk of cardiac events and thus an increased risk of all-cause mortality. Clinicians should closely monitor the function of the cardiac conduction system in older patients and take the necessary measures to treat heart blocks. This may include medication, pacemaker implantation, and other cardiac therapeutic interventions.
Therefore, the application of the nine risk factors in predicting all-cause mortality among community-dwelling older adults seems to be well-founded. From the perspective of PPPM, modifiable risk factors should be monitored when developing targeted prevention and intervention measures to decrease mortality for community-dwelling older adults. We recommend increased monitoring of alcohol status, daily alcohol consumption, fasting glucose, hemoglobin, and electrocardiograms among older people in the community. Conducting person-specific preventative and treatment measures (e.g. strict control of daily liquor consumption, lowering fasting glucose, raising hemoglobin, controlling heart rate, and treatment of heart block) for high-risk elderly may help improve the quality of life and survival rates [23]. Eliminating these risk factors may reduce the frequency of hospitalization and care, reducing the length of hospital stay and saving healthcare costs. This easy-to-use predictive model may also be able to improve adherence/willingness to health care for the elderly [23]. Moreover, our findings aid in guiding physicians’ decisions on treatment and management, avoiding over- and under-treatment.
Strengths and limitations
The strengths of the study need to be emphasized: Firstly, in this two-center study, we developed and externally validated a nomogram prediction model, and showed that the model has good discrimination and calibration capabilities. Secondly, this is a clinical multidimensional variable cohort study with a large sample size. The 8 years of follow-up comprised a total of 16,432 person years among 5085 participants. We screened predictors from 95 clinical multidimensional variables, including demographics, lifestyle behaviors, symptoms, medical history, family history, physical examination, laboratory examination, and ECG data. Finally, the prediction models help to predict all-cause mortality in older adults and to identify high-risk individuals. The identified risk factors help the high-risk individuals to take personalized preventive and intervention measures at an early stage. The results of this study have significant clinical value in improving the health status, quality of life, and survival of older people.
There are also several limitations in this study. Firstly, this study lacks certain social factors, for example, health domains, housing status, transportation, years of retirement, or even activities of daily living, as no relevant data was available in the questionnaire. Secondly, we also did not obtain molecular omics data, such as genomics, proteomics, and transcriptome data. Molecular omics testing is mostly used in scientific research and is rarely performed for health checkups. Increasing these social factors and molecular omics data has the potential to improve the accuracy of the model. Finally, the demographic variables of this study were self-reported, which may have resulted in subjective bias, and may cast doubt on model effectiveness. However, the questionnaire was collected by trained medical personnel, which may lower this bias. The final prediction model did not include subjective variables.
Conclusions and expert recommendations
In conclusion, based on clinical multidimensional variables, we developed and externally validated a personalized prediction model to evaluate 1-, 3-, 5-, and 8-year all-cause mortality for community-dwelling older adults, and offer primary prevention and personalized medical treatment strategies based on modifiable risk factors. Strict control of daily liquor consumption, lowering fasting glucose, raising hemoglobin, controlling heart rate, and treatment of heart blocks will be beneficial for improving survival in elderly populations.
Our study supports the application of PPPM, from different perspectives, in the medical services of all-cause mortality community-dwelling older adults. Firstly, from the perspective of all-cause mortality prediction, we constructed an all-cause mortality risk-prediction model applicable to community-dwelling older adults. The risk-prediction model could identify individuals at high risk of all-cause mortality and contribute to the paradigm shift from delayed reactive medicine to proactive medicine, which could help save public health resources and decrease the mortality of community-dwelling older adults. Secondly, from the perspective of all-cause mortality prevention, current prediction indicators of mortality prediction models are limited in demographic variables, comorbid conditions, and lifestyle behaviors. In this study, we identified risk factors by clinical multidimensional variables, and these risk factors are easy to obtain, thus helping us to monitor the progression of all-cause mortality. Community older adults can prevent all-cause mortality by targeting daily health care against modifiable risk factors. Finally, from the perspective of personalized interventions, clinical multidimensional variables are more comprehensive and objective. Our risk-prediction model can predict the risk of mortality for community-dwelling older adults at different times, and develop tailored interventions through modifiable risk factors to reduce mortality.
Data availability
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Code availability
Not applicable.
References
WHO. Ageing and health. 2022. https://www.who.int/news-room/fact-sheets/detail/ageing-and-health. Accessed 1 Oct 2022.
Chang AY, Skirbekk VF, Tyrovolas S, Kassebaum NJ, Dieleman JL. Measuring population ageing: an analysis of the Global Burden of Disease Study 2017. Lancet Public Health. 2019;4:e159–67. https://doi.org/10.1016/s2468-2667(19)30019-2.
Wang LM, Chen ZH, Zhang M, Zhao ZP, Huang ZJ, Zhang X, et al. Study of the prevalence and disease burden of chronic disease in the elderly in China. Zhonghua liu xing bing xue za zhi = Zhonghua liuxingbingxue zazhi. 2019;40:277–83. https://doi.org/10.3760/cma.j.issn.0254-6450.2019.03.005.
Yin H, Brauer M, Zhang JJ, Cai W, Navrud S, Burnett R, et al. Population ageing and deaths attributable to ambient PM(2·5) pollution: a global analysis of economic cost. Lancet Planet Health. 2021;5:e356–67. https://doi.org/10.1016/s2542-5196(21)00131-5.
Golubnitschaja O, Costigliola V. General report & recommendations in predictive, preventive and personalised medicine 2012: white paper of the European Association for Predictive, Preventive and Personalised Medicine. EPMA J. 2012;3(1):14. https://doi.org/10.1186/1878-5085-3-14.
Golubnitschaja O, Watson ID, Topic E, Sandberg S, Ferrari M, Costigliola V. Position paper of the EPMA and EFLM: a global vision of the consolidated promotion of an integrative medical approach to advance health care. EPMA J. 2013;4:12. https://doi.org/10.1186/1878-5085-4-12.
Golubnitschaja O, Kinkorova J, Costigliola V. Predictive, preventive and personalised medicine as the hardcore of ‘Horizon 2020’: EPMA position paper. EPMA J. 2014;5:6. https://doi.org/10.1186/1878-5085-5-6.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation - EPMA position paper 2016. EPMA J. 2016;7:23. https://doi.org/10.1186/s13167-016-0072-4.
Qiu MJ, Fang XF, Huang ZZ, Li QT, Wang MM, Jiang X, et al. Prognosis of primary hepatic lymphoma: a US population-based analysis. Transl Oncol. 2021;14:100931. https://doi.org/10.1016/j.tranon.2020.100931.
Szlachetka WA, Pana TA, Mamas MA, Bettencourt-Silva JH, Metcalf AK, Potter JF, et al. Predicting 10-year stroke mortality: development and validation of a nomogram. Acta Neurol Belg. 2021. https://doi.org/10.1007/s13760-021-01752-9.
Li F, Xin H, Zhang J, Fu M, Zhou J, Lian Z. Prediction model of in-hospital mortality in intensive care unit patients with heart failure: machine learning-based, retrospective analysis of the MIMIC-III database. BMJ Open. 2021;11:e044779. https://doi.org/10.1136/bmjopen-2020-044779.
Porthan K, Viitasalo M, Jula A, Reunanen A, Rapola J, Väänänen H, et al. Predictive value of electrocardiographic QT interval and T-wave morphology parameters for all-cause and cardiovascular mortality in a general population sample. Heart Rhythm. 2009;6:1202–8, 8.e1. https://doi.org/10.1016/j.hrthm.2009.05.006.
Porthan K, Viitasalo M, Toivonen L, Havulinna AS, Jula A, Tikkanen JT, et al. Predictive value of electrocardiographic T-wave morphology parameters and T-wave peak to T-wave end interval for sudden cardiac death in the general population. Circ Arrhythm Electrophysiol. 2013;6:690–6. https://doi.org/10.1161/circep.113.000356.
Liu L, Lo K, Huang C, Feng YQ, Zhou YL, Huang YQ. Derivation and validation of a simple nomogram prediction model for all-cause mortality among middle-aged and elderly general population. Ann palliat Med. 2021;10:1167–79. https://doi.org/10.21037/apm-20-580.
Schonberg MA, Davis RB, McCarthy EP, Marcantonio ER. Index to predict 5-year mortality of community-dwelling adults aged 65 and older using data from the National Health Interview Survey. J Gen Intern Med. 2009;24:1115–22. https://doi.org/10.1007/s11606-009-1073-y.
Deo R, Norby FL, Katz R, Sotoodehnia N, Adabag S, DeFilippi CR, et al. Development and validation of a sudden cardiac death prediction model for the general population. Circulation. 2016;134:806–16. https://doi.org/10.1161/circulationaha.116.023042.
Hancock EW, Deal BJ, Mirvis DM, Okin P, Kligfield P, Gettes LS, et al. AHA/ACCF/HRS recommendations for the standardization and interpretation of the electrocardiogram: part V: electrocardiogram changes associated with cardiac chamber hypertrophy: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation. 2009;119:e251–61. https://doi.org/10.1161/circulationaha.108.191097.
Camp RL, Dolled-Filhart M, Rimm DL. X-tile: a new bio-informatics tool for biomarker assessment and outcome-based cut-point optimization. Clin Cancer Res: Off J Am Assoc Cancer Res. 2004;10:7252–9. https://doi.org/10.1158/1078-0432.ccr-04-0713.
Zhang Z. Multiple imputation with multivariate imputation by chained equation (MICE) package. Ann Transl Med. 2016;4:30. https://doi.org/10.3978/j.issn.2305-5839.2015.12.63.
Simon N, Friedman J, Hastie T, Tibshirani R. Regularization paths for Cox’s proportional hazards model via coordinate descent. J Stat Softw. 2011;9:1–13. https://doi.org/10.18637/jss.v039.i05.
Fisher LD, Lin DY. Time-dependent covariates in the Cox proportional-hazards regression model. Annu Rev Public Health. 1999;20:145–57. https://doi.org/10.1146/annurev.publhealth.20.1.145.
Jalali A, Alvarez-Iglesias A, Roshan D, Newell J. Visualising statistical models using dynamic nomograms. PLoS one. 2019;14:e0225253. https://doi.org/10.1371/journal.pone.0225253.
Akhmetov I, Bubnov RV. Assessing value of innovative molecular diagnostic tests in the concept of predictive, preventive, and personalized medicine. Epma J. 2015;6:19. https://doi.org/10.1186/s13167-015-0041-3.
McLaughlin VV, Hoeper MM, Channick RN, Chin KM, Delcroix M, Gaine S, et al. Pulmonary arterial hypertension-related morbidity is prognostic for mortality. J Am Coll Cardiol. 2018;71:752–63. https://doi.org/10.1016/j.jacc.2017.12.010.
Zhou Y, Chen Y, Zhang X, Zhao B, Gao F, Yuan X, et al. Nutritional risk and a high NRS2002 score are closely related to disease progression and poor prognosis in patients with COVID-19. Front Nutr. 2023;10:1089972. https://doi.org/10.3389/fnut.2023.1089972.
Ding D, Rogers K, van der Ploeg H, Stamatakis E, Bauman AE. Traditional and emerging lifestyle risk behaviors and all-cause mortality in middle-aged and older adults: evidence from a large population-based Australian cohort. PLoS Med. 2015;12:e1001917. https://doi.org/10.1371/journal.pmed.1001917.
Fleischmann KE, Orav EJ, Lamas GA, Mangione CM, Schron E, Lee KL, et al. Pacemaker implantation and quality of life in the Mode Selection Trial (MOST). Heart Rhythm. 2006;3:653–9. https://doi.org/10.1016/j.hrthm.2006.02.1031.
Kobayashi LC, Jackson SE, Lee SJ, Wardle J, Steptoe A. The development and validation of an index to predict 10-year mortality risk in a longitudinal cohort of older English adults. Age Ageing. 2017;46:427–32. https://doi.org/10.1093/ageing/afw199.
Óh B, Gransar H, Callister T, Shaw LJ, Schulman-Marcus J, Stuijfzand WJ, et al. Development and validation of a simple-to-use nomogram for predicting 5-, 10-, and 15-year survival in asymptomatic adults undergoing coronary artery calcium scoring. JACC Cardiovasc Imaging. 2018;11:450–8. https://doi.org/10.1016/j.jcmg.2017.03.018.
Müller L, Di Benedetto S, Pawelec G. The immune system and its dysregulation with aging. Subcell Biochem. 2019;91:21–43. https://doi.org/10.1007/978-981-13-3681-2_2.
Varì R, Scazzocchio B, D’Amore A, Giovannini C, Gessani S, Masella R. Gender-related differences in lifestyle may affect health status. Ann Ist Super Sanita. 2016;52:158–66. https://doi.org/10.4415/ann_16_02_06.
Antoni MH, Dhabhar FS. The impact of psychosocial stress and stress management on immune responses in patients with cancer. Cancer. 2019;125:1417–31. https://doi.org/10.1002/cncr.31943.
Lenneman CG, Sawyer DB. Cardio-oncology: an update on cardiotoxicity of cancer-related treatment. Circ Res. 2016;118:1008–20. https://doi.org/10.1161/circresaha.115.303633.
Sun Y, Zhang B, Yao Q, Ma Y, Lin Y, Xu M, et al. Association between usual alcohol consumption and risk of falls in middle-aged and older Chinese adults. BMC Geriatr. 2022;22:750. https://doi.org/10.1186/s12877-022-03429-1.
Puddey IB, Mori TA, Barden AE, Beilin LJ. Alcohol and hypertension-new insights and lingering controversies. Curr Hypertens Rep. 2019;21:79. https://doi.org/10.1007/s11906-019-0984-1.
Schuckit MA. Alcohol-use disorders. Lancet. 2009;373:492–501. https://doi.org/10.1016/s0140-6736(09)60009-x.
Tian Y, Liu J, Zhao Y, Jiang N, Liu X, Zhao G, et al. Alcohol consumption and all-cause and cause-specific mortality among US adults: prospective cohort study. BMC Med. 2023;21:208. https://doi.org/10.1186/s12916-023-02907-6.
Kohansal K, Masrouri S, Khalili D, Ramezankhani A, Azizi F, Blaha MJ, et al. Changes in fasting plasma glucose status and risk of mortality events in individuals without diabetes over two decades of follow-up: a pooled cohort analysis. Cardiovasc Diabetol. 2022;21:267. https://doi.org/10.1186/s12933-022-01709-z.
Rodriguez-Gutierrez R, Gonzalez-Gonzalez JG, Zuñiga-Hernandez JA, McCoy RG. Benefits and harms of intensive glycemic control in patients with type 2 diabetes. BMJ (Clinical research ed). 2019;367:l5887. https://doi.org/10.1136/bmj.l5887.
Luc K, Schramm-Luc A, Guzik TJ, Mikolajczyk TP. Oxidative stress and inflammatory markers in prediabetes and diabetes. J Physiol Pharmacol. 2019;70:809–24. https://doi.org/10.26402/jpp.2019.6.01.
Halawi R, Moukhadder H, Taher A. Anemia in the elderly: a consequence of aging? Expert Rev Hematol. 2017;10:327–35. https://doi.org/10.1080/17474086.2017.1285695.
Stauder R, Valent P, Theurl I. Anemia at older age: etiologies, clinical implications, and management. Blood. 2018;131:505–14. https://doi.org/10.1182/blood-2017-07-746446.
Kalra PR, Greenlaw N, Ferrari R, Ford I, Tardif JC, Tendera M, et al. Hemoglobin and change in hemoglobin status predict mortality, cardiovascular events, and bleeding in stable coronary artery disease. Am J Med. 2017;130:720–30. https://doi.org/10.1016/j.amjmed.2017.01.002.
Imahori Y, Vetrano DL, Xia X, Grande G, Ljungman P, Fratiglioni L, et al. Association of resting heart rate with cognitive decline and dementia in older adults: a population-based cohort study. Alzheimer’s Dement : J Alzheimer’s Assoc. 2022;18:1779–87. https://doi.org/10.1002/alz.12495.
Aune D, Sen A, ó'Hartaigh B, Janszky I, Romundstad PR, Tonstad S, et al. Resting heart rate and the risk of cardiovascular disease, total cancer, and all-cause mortality - a systematic review and dose-response meta-analysis of prospective studies. Nutr Metab Cardiovasc Dis. 2017;27:504–17. https://doi.org/10.1016/j.numecd.2017.04.004.
Lorgis L, Zeller M, Jourdain P, Beaune J, Cambou JP, Vaisse B, et al. Heart rate distribution and predictors of increased heart rate among French hypertensive patients with stable coronary artery disease. Data from the LHYCORNE cohort. Arch Cardiovasc Dis. 2009;102:541–7. https://doi.org/10.1016/j.acvd.2009.05.003.
Crisel RK, Farzaneh-Far R, Na B, Whooley MA. First-degree atrioventricular block is associated with heart failure and death in persons with stable coronary artery disease: data from the Heart and Soul Study. Eur Heart J. 2011;32:1875–80. https://doi.org/10.1093/eurheartj/ehr139.
Gaba P, Pedrotty D, DeSimone CV, Bonikowske AR, Allison TG, Kapa S. Mortality in patients with right bundle-branch block in the absence of cardiovascular disease. J Am Heart Assoc. 2020;9:e017430. https://doi.org/10.1161/jaha.120.017430.
Baldasseroni S, Opasich C, Gorini M, Lucci D, Marchionni N, Marini M, et al. Left bundle-branch block is associated with increased 1-year sudden and total mortality rate in 5517 outpatients with congestive heart failure: a report from the Italian network on congestive heart failure. Am Heart J. 2002;143:398–405. https://doi.org/10.1067/mhj.2002.121264.
El-Menyar AA, Abdou SM. Impact of left bundle branch block and activation pattern on the heart. Expert Rev Cardiovasc Ther. 2008;6:843–57. https://doi.org/10.1586/14779072.6.6.843.
Acknowledgements
The authors thank all participants who allowed their data to be used for this study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant 82073659), the 2020 Li Ka Shing Foundation Cross-Disciplinary Research Grant (2020LKSFG19B), the 2021 Special Fund Project for Science and Technology Innovation Strategy of Guangdong Province (2021–88-53), and the 2022 Guangdong Province Science and Technology Special Fund (2022–124-6).
Author information
Authors and Affiliations
Contributions
YQC and XRT: concept/design, data analysis/interpretation, critical revision of the article, and approval. YQC, XLD, DL, PXY, and SW: statistics, data analysis, and drafting of the article. YQC, XLD, XDW, HZ, XMC, XCW, WCW, and KBK: data collection, data analysis, critical revision of the article, and approval. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This two-center cohort study was approved by the Ethics Committee of the First Affiliated Hospital of Shantou University Medical College. All participants provided written informed consent to participate in this study.
Consent for publication
Participants gave their written informed consent for publishing the data. All authors have approved the manuscript submission to EPMA J.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Y., Deng, X., Lin, D. et al. Predicting 1-, 3-, 5-, and 8-year all-cause mortality in a community-dwelling older adult cohort: relevance for predictive, preventive, and personalized medicine. EPMA Journal 14, 713–726 (2023). https://doi.org/10.1007/s13167-023-00342-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-023-00342-4