ABSTRACT
Native Hawaiians/Pacific Islanders experience a high prevalence of overweight/obesity. The Diabetes Prevention Program Lifestyle Intervention (DPP-LI) was translated into a 3-month community-based intervention to benefit these populations. The weight loss and other clinical and behavioral outcomes of the translated DPP-LI and the socio-demographic, behavioral, and biological factors associated with the weight loss were examined. A total of 239 Native Hawaiian/Pacific Islander adults completed the translated DPP-LI through four community-based organizations (CBOs). Changes from pre- to post-intervention assessments in weight, blood pressure, physical functioning, exercise frequency, and fat in diet were measured. Significant improvements on all variables were found, with differences observed across the four CBOs. CBOs with predominately Native Hawaiian and ethnically homogenous intervention groups had greater weight loss. General linear modeling indicated that larger baseline weight and CBO predicted weight loss. The translated DPP-LI can be effective for Native Hawaiians/Pacific Islanders, especially when socio-cultural, socio-economic, and CBO-related contextual factors are taken into account.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
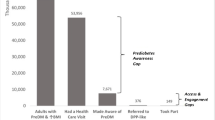
Overweight (body mass index [BMI] ≥25) and obesity (BMI ≥30) have reached epidemic proportions in the Unites States affecting 68 % of the adult population [1–3]. The combined prevalence of overweight and obesity is between 76 % and 90 % for Native Hawaiians and Pacific Islanders (e.g., Samoans and Chuukese) [4–6]. They have a higher prevalence of obesity-related diseases, such as diabetes at 19 %, hypertension at 41 %, and heart disease at 20 % compared to the general population at 8 %, 25 %, and 12 %, respectively [5, 7, 8]. Translating evidence-based lifestyle interventions for at-risk populations, such as Native Hawaiians and Pacific Islanders, to curb obesity-related diseases is a public health priority [9].
The Diabetes Prevention Program (DPP) showed that lifestyle interventions are efficacious in achieving moderate weight loss and significant health improvements in people at risk for diabetes [3, 10]. Participants of the DPP Lifestyle Intervention (DPP-LI) had a 34 % lower incidence of diabetes over 10 years [10]. Since this landmark clinical trial, there has been a profusion of translational research to establish the DPP-LI's effectiveness in real world settings [11–13]. The DPP-LI has been successfully translated into various settings to include rural and urban communities [14–16], health centers [17–20], community centers, churches, and senior care facilities [21–24]. The DPP-LI has also been translated into many ethnic/racial populations, such as Latinos [25, 26], Native Americans [27], and African-Americans [21, 22, 24].
A meta-analysis of 28 translational DPP-LI studies indicated its effectiveness in achieving moderate weight loss, averaging 4 %, across diverse settings and modes of delivery (using medical and allied health professionals, lay educators, and electronic media) [28]. It was found that lay educators achieved comparable, and in some instances better, weight-loss outcomes as clinically trained professionals (e.g., nurses, nutritionists, and social workers). Although no difference in weight change was found by treatment length, there was a trend of increased weight change associated with the number of treatment sessions attended, which corresponded to the number of treatment sessions offered by the programs.
The PILI 'Ohana Project (POP), a community-based participatory research project (CBPR), conducted a pilot study (2005 to 2008) to determine the feasibility and weight-loss effects of a translated DPP-LI in Native Hawaiians and Pacific Islanders [29]. The translated DPP-LI was modified to be community-based and delivered by community health advocates (CHAs) who ranged from lay peer educators to master-level social workers, nurses, and nutritionists. It was built into a two-phase weight loss and weight loss maintenance program, called the PILI Lifestyle Program (PLP). Phase 1 was the translated DPP-LI, delivered in eight sessions over 3 months to initiate weight loss [29], and Phase 2 was a family and community focused weight-loss maintenance intervention, delivered in six sessions over 6 additional months [30]. Mau et al. [29] found that the translated DPP-LI (Phase 1) for Native Hawaiians and Pacific Islanders (n = 169) with excess body weight led to significant, albeit modest, weight loss (−1.5 kg) and improvements in systolic (−6.0 mmHg) and diastolic (−2.8 mmHg) blood pressure (BP), distance walked in 6 min, and self-reported physical activity levels and fat intake.
To more definitively evaluate the DPP-LI translated into Native Hawaiian and Pacific Islander communities, the POP further examined its effects on initial weight loss, systolic and diastolic BP, physical functioning, physical activity levels, and fat intake in a larger and different sample. It was done between 2009 and 2012 across four distinct community-based organizations (CBOs). The POP also sought to examine the baseline socio-demographic (i.e., age, sex, education, and marital status), behavioral (e.g., physical activity level and fat intake), and clinical (e.g., BP, weight, and physical functioning) correlates of initial weight loss, and the effects of attendance on weight loss. Previous studies have indicated that greater weight loss early in an intervention program and better attendance leads to greater weight loss and its maintenance [30–33]. The long term goal of improving the effectiveness of translating proven interventions into diverse communities is facilitated by a deeper understanding of the social and cultural context of these communities. The purpose of this paper is to elucidate the socio-demographic, behavioral, and biological factors associated with early weight-loss efforts among four ethnically and organizationally diverse groups with members at high risk for diabetes.
METHODS AND PROCEDURES
Participants
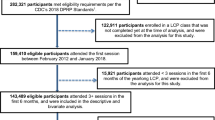
Data for this study come from 239 Native Hawaiian and Pacific Islander adults (18 years of age and older) who completed the 3-month DPP-LI translated weight-loss intervention [30]. The inclusion criteria for participation in the intervention study were: (a) Native Hawaiian, Filipino or other Pacific Islander ancestry (i.e., Chuukese, Samoan), (b) ≥18 years of age, (c) overweight/obese — defined as BMI ≥25 for Native Hawaiians and Pacific Islanders and ≥23 for Filipinos [34], (d) willing and able to perform 150 min of moderate physical activity (equivalent to brisk walking) per week and to follow a healthy diet to induce weight loss of up to 1 kg per week, and (e) identifying at least one family member or friend to provide support throughout the program. A detailed description of the methods can be found in the work of Mau et al. [29] and Kaholokula et al. [30].
Study design and procedures
The study design (pre- to post-intervention evaluation) was developed collaboratively between the community and academic partners of the POP using a fully engaged CBPR approach [29, 35]. Four CBOs participated in the POP: Hawai'i Maoli of the Association for Hawaiian Civic Clubs (HM), Ke Ola Mamo (KOM; a Native Hawaiian Health Care System), Kōkua Kalihi Valley Comprehensive Family Services (KKV; a community health center), and Kula no nā Po'e Hawai'i (KULA; a non-profit organization serving three Hawaiian Homestead communities). HM, KOM, and KULA are predominately Native Hawaiian-serving CBOs and KKV is a predominately immigrant Pacific Islander-serving CBO by nature of their location in urban O'ahu. For more details about these CBOs, refer to Nacapoy et al. [35]. Recruitment of participants and the implementation and evaluation of the intervention were conducted in the respective participating CBOs by trained CHAs. Recruitment strategies were developed and implemented by the CBOs, which included physician referrals, recruitment booths at health fairs, newsletters, and word-of-mouth.
Consistent with our CBPR approach, assessments were performed by trained community researchers using standardized protocols for data collection on demographics, clinical measures, physical functioning, and self-reported dietary and physical activity behaviors. The institutional review boards of the Native Hawaiian Health Care Systems and the University of Hawai'i at Mānoa approved this study. This study is also registered on ClinicalTrials.gov (NCT01093924). Informed consent was obtained from all participants prior to their involvement. Data presented here were collected at pre- and post-intervention.
Translated DPP lifestyle intervention
The original DPP-LI was developed using the social cognitive theory (SCT) [36] by nutritionists, behavioral psychologists, exercise physiologists, nurses, and physicians from the University of Pittsburgh Medical Center and the DPP Interventions Committee [37, 38]. Nine of the 16 behavior change technique clusters as defined by Michie et al. [39] were used repeatedly in the DPP-LI curriculum, including: reward (e.g., self-reward), antecedents (e.g., avoidance and changing exposure to cues for the behavior), associations (e.g., prompts/cues), natural consequences (e.g., social consequences), feedback and monitoring (e.g., self-monitoring of behavior), goals and planning (e.g., goal setting — outcome), social support (e.g., social support — general), self-belief (e.g., self-talk), and shaping knowledge (e.g., instructions on how to perform a behavior). All of these techniques were applied to both dietary and physical activity behaviors.
The adaptation of the DPP-LI was based on community assessments to identify salient issues of obesity affecting Native Hawaiians and other Pacific Islanders. Mau et al. [29] described in detail the methods and results of the community assessments and how the DPP-LI was adapted. Briefly, key-informant interviews, focus groups, and surveys with 333 Native Hawaiian and other Pacific Islander stakeholders and community "windshield tours" (i.e., walking/driving through a defined community to visually survey its infrastructure, condition, and available resources) were conducted and the information obtained from them informed the DPP-LI adaptation.
Salient socio-economic and socio-cultural factors identified from the community assessments were incorporated into the intervention: lessons on economical healthy eating and communicating effectively with the doctor were added to the curriculum based on POP analysis of community and provider group interviews and discussions. To capitalize on the cultural value of 'ohana (i.e., the preference for working together and group decision making) and for feasibility purposes, the lessons were delivered in group settings of 10–20 people (M = 12) and participants were encouraged to have a support person, a family member or friend, attend with them. In order for the intervention to be feasible and accessible for delivery in community settings by CHAs, it was shortened from 16 lessons delivered over 24 weeks to eight lessons delivered over 12 weeks but with all original foci and strategies retained. The first four lessons were delivered weekly and the second four lessons were delivered every other week for the remaining 8 weeks. Each lesson was 1–1½ h in length with group interaction. As with the original DPP-LI, the intervention focused on evidence-based behavioral weight loss strategies for healthy eating, physical activity and stress/negative emotions management utilizing individual action planning [29, 40].
Although the consolidation and condensing of the original DPP-LI lessons may have weakened the intervention effects, it was necessary to make it practical for the socioeconomic realities of many Native Hawaiians and Pacific Islanders. The community partners believed it was necessary to ensure its feasibility and sustainability across different types of Native Hawaiian and Pacific Islander communities. A summary of the translated lessons in comparison to the original DPP-LI lessons is presented in Table 1 and can also be found in Mau et al. [29].
The adaption of the DPP-LI was also informed by the SCT, which emphasizes the importance of social and interpersonal influences in behavior change and cognitive processes as important mediators of behavior change [36]. Constructs used in curriculum adaptation from the SCT included: self-efficacy, self-regulation, social support, and social modeling. These constructs have been successfully used to improve healthy eating and physical activity [41–44]. The behavior change techniques used in the original DPP-LI were all maintained in the adapted DPP-LI. Because the adapted DPP-LI was delivered in group settings (vs. one-on-one delivery in the original DPP-LI), covert learning (e.g., vicarious reinforcement) was also a behavioral strategy used.
All participants were encouraged to achieve a weight loss of ≥5 % of their initial body weight, to engage in at least 30 min of physical activity for most days of the week, and to eat <30 % fat in their daily diet over the course of the 3-month intervention. However, the community partners believed that making the intervention goals too stringent and inflexible would lead to higher attrition and an inability for the participants to maintain the amount of effort needed to obtain large weight loss in a 3-month period. It was preferred to allow the participants to make slow and gradual changes if they so desired and to set realistic goals based on their individual life situation, resources, and level of support.
Assessment measures
Clinical measures
Systolic and diastolic BP was obtained using an automatic BP device (HEM-907XL IntelliSense). Body weight in kilograms (kg) and height in centimeters (cm) were measured using an electronic scale (Tanita BWB800AS) and a stadiometer (Seca 222), respectively. Height was measured at baseline only. All clinical measures were obtained in duplicate, recorded, and computed as the average of the two values. BMI was computed as body weight in kg divided by height in meters squared.
Socio-demographics
Date of birth, sex, marital status, education level, and self-reported Native Hawaiian, Filipino and other Pacific Islander ancestry were collected. The ethnic/racial category of Native Hawaiians and other Pacific Islanders in the United States includes people with origins in the original inhabitants of Polynesia (e.g., Native Hawaiians, Samoans, and Tahitian), Micronesia (e.g., Chuukese), or Melanesia (e.g., Fijian) [6]. Due to their similar risk profile as Pacific Islanders for obesity and related diseases in Hawai'i, Filipinos (often federally classified as "Asian") were included in this study [7].
Physical functioning
Physical functioning was assessed using a 6-min walk test (6MWT) that measures the distance (in feet) a person is able to walk in 6 min [45]. Participants were asked to walk as far as possible (without running) back and forth using a fixed-lap distance. Participants were allowed to stop and to rest, if needed, but asked to resume walking as soon as they were able. Immediately following the walk test, the number of laps completed and the distance walked in final lap were recorded. The 6MWT has been found to be highly associated with functional capacity [46].
Exercise frequency
The brief Physical Activity Questionnaire (PAQ) was used to assess exercise frequency and change during the past month [47]. It consists of three items: one item to assess moderate activity level (e.g., bowling, golf, and walking), one item to assess vigorous activity level (e.g., running, swimming, aerobics), and one item to assess change in activity level. The first two items were used to calculate exercise frequency for this study. Frequency for moderate and vigorous activities were both rated on a scale from 1 (>4 times per week) to 5 (rarely or never). Exercise frequency scores were computed by summing participants' responses to each item and dividing by two. Scores ranged from 1 to 5, with lower scores indicating greater exercise frequency.
Fat in diet
A 39-item modified version of the Eating Habits Questionnaire (EHQ) was used to estimate the amount of fat in participants' diet over the last month [29, 48]. The questionnaire assesses frequency in four fat consumption categories: (1) modify meat, (2) avoid fat, (3) modification/substitution, and (4) replace with vegetables, using a 4-point scale ranging from 1 (always) to 4 (never). The summary score for fat consumption was obtained by adding the mean of each of the fat categories and dividing that by 4. A dietary fat score of ≥2.5 indicates greater than 30 % of calories from fat in diet.
Statistical analysis
Demographic, clinical, and behavioral variables at pre- and post-intervention were summarized by descriptive statistics: mean and standard deviation for continuous variables (e.g., age) and frequency and percentage for categorical variables (e.g., ethnicity). Differences in baseline characteristics were compared by one-way analysis of variance (ANOVA) for continuous variables, followed by Tukey–Kramer procedure for pairwise comparison if significant differences were observed. For categorical variables, Chi-square tests or Fisher's exact tests, if applicable, were used. For subsequent analyses, participants reporting "other Pacific Islander" and "Filipino" ancestry, and no Native Hawaiian ancestry, were aggregated into an "other" category. Changes in clinical and behavioral measures at post-intervention from pre-intervention (baseline) measures were evaluated using paired t-tests by CBO and for the combined sample. All changes in clinical and behavioral variables (including weight loss) were defined as post-intervention values minus baseline values. The differences in the changes across the CBOs were compared by one-way ANOVA, followed by Tukey–Kramer procedure, if significant differences were observed. The association of weight loss (from baseline to post-intervention) with the baseline socio-demographic, clinical, and behavioral measures was also examined using correlation analysis.
A general linear model (GLM) was developed to identify variables contributing to weight loss from baseline to post-intervention. Included were those baseline variables that were suggestive with p < 0.10 in their bivariate associations with weight change from baseline to post-intervention. Because the ethnic distribution overlapped to some degree with CBOs, ethnicity was also entered into the model to determine if it had any significant independent effect on weight loss after adjusting for the CBO variable. The ethnicity-by-CBO interaction term was also first examined to determine whether it was significant. F-tests were used to evaluate the significance of each variable in the GLM model. To better understand possible factors associated with the differences in weight loss between KKV and the other three CBOs, a post-hoc secondary and exploratory analysis was conducted to compare the impacts of education level, number of lessons, and Chuukese (an ethnic group mainly from KKV) on weight loss, either within KKV subset sample or between KKV and other CBOs, using Spearman correlation and one-way ANOVA. All statistical analyses were performed using SAS software version 9.3 (SAS Institute Inc., Cary, NC, USA). A two-sided p value < 0.05 was considered statistically significant.
RESULTS
Baseline characteristics
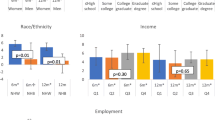
Baseline characteristics for each CBO and the combined sample are summarized in Table 2. Overall, participants had a mean age of 50.8 years (SD = 14.3) and BMI of 38.3 (SD = 8.7), and a majority were Native Hawaiian (71 %) and female (84 %). There were significant differences at baseline among CBOs on ethnic composition [χ 2(15, N = 238) = 156.39, p < 0.001], age [R 2 = 0.033, F(3,233) = 2.65, p = 0.0499], education level [χ 2(9, N = 238) = 41.56, p < 0.001], weight [R 2 = 0.050, F(3,235) = 4.11, p = 0.0072], systolic BP [R 2 = 0.045, F(3,235) = 3.68, p = 0.013], diastolic BP [R 2 = 0.098, F(3,235) = 8.51, p < 0.001], 6MWT [R 2 = 0.065, F(3,233) = 5.37, p = 0.0014], and Physical Activity Frequency [R 2 = 0.056, F(3,235) = 4.61, p = 0.0037]. At baseline, KKV participants tended to be younger (46.2 years), with a higher percentage at high school or less education level (65 %), higher weight (111 kg), lower physical activity frequency (3.8 with 4 = least active), but able to walk the furthest in a 6-min walk test (1,336 ft) compared to the other three CBOs. Notable ethnic differences were observed with KULA, HM, and KOM comprised primarily of Native Hawaiians (84–87 %), while at KKV 15 % were Native Hawaiian, with 39 % Chuukese, 29 % Samoan, and 14 % Filipino.
Change in clinical and behavioral measures
When examining combined data from the four CBOs, all variables had significant changes from pre- to post-intervention assessments as summarized in Table 3. There were significant improvements in weight loss of [M = −1.7 kg, SD = 3.5; t(238) = −7.59, p < 0.001] and systolic BP [M = −3.3 mmHg, SD = 18.6; t(238) = −2.80, p = 0.0056] and diastolic BP [M = −3.4 mmHg, SD = 12.5; t(238) = −4.23, p < 0.001] improvements. There were also significant improvements in feet walked during the 6MWT [M = 106.6 ft, SD = 238.4; t(235) = 6.87, p < 0.001], Physical Activity Frequency [M = −0.5, SD = 1.2, t(236) = −6.12, p < 0.001], and Fat in Diet [M = −0.3, SD = 0.4, t(237) = −12.37, p < 0.001].
Because of baseline differences in CBOs involved in delivering the intervention, the outcomes by CBO were also examined. Although all four CBOs showed similar changes in Physical Activity Frequency and Fat in Diet, outcomes on the following variables differed significantly: weight [R 2 = 0.051, F(3, 235) = 4.24, p = 0.0061], BMI [R 2 = 0.055, F(3, 232) = 4.51, p = 0.0043], systolic BP [R 2 = 0.036, F(3, 235) = 2.92, p = 0.035], diastolic BP [R 2 = 0.08, F(3, 235) = 6.81, p < 0.001], and 6MWT [R 2 = 0.087, F(3, 232) = 7.33, p < 0.001]. Statistically significant weight loss was found at KOM [−2.0 kg, SD = 3.8, t(69) = −4.39, p < 0.001], KULA [−2.2 kg, SD = 3.1, t(58) = −5.34, p < 0.001], and HM [−2.3 kg, SD = 3.6, t(57) = −4.91, p < 0.001]; whereas, KKV showed some weight loss (−0.2 kg, SD = 3.2), but this was not significant. Only KULA showed a statistically significant reduction in BP, with the average reduction of −9.3 mmHg, SD = 22.4 [t(58) = −3.17, p = 0.0024] for systolic BP and −9.5 mmHg, SD = 14.2 [t(58) = −5.13, p < 0.001] for diastolic BP. In the other three CBOs, there was a trend towards BP reduction at the end of study. All CBOs showed an improvement in 6MWT performance; however, only KULA and HM were statistically significant with average improvements of 183.7 ft, SD = 207.4 [t(57) = 6.75, p < 0.001] and 169.8 ft, SD = 237.6 [t(56) = 5.39, p < 0.001], corresponding to 15.1 % and 12.9 % average increases from baseline, respectively.
Bivariate analyses
The bivariate associations between baseline socio-demographic, clinical, and behavioral characteristics and weight loss at post-intervention were examined. There was a significant association between CBOs and post-intervention weight loss [R 2 = 0.051; F(3,235) = 4.24, p = 0.0061]. Higher baseline weight was also significantly associated with more weight loss [r(237) = −0.15, p = 0.021]. Because CBOs and ethnicity were significantly associated [χ 2(3, N = 238) = 97.80, p < 0.001] and the association between higher diastolic BP at baseline and more weight loss approached significance [r(237) = −0.12, p = 0.073], they along with baseline weight and CBO were considered in the following multivariable analysis.
The number of lessons received by participants across the CBOs and its association with weight loss was also examined. KKV participants received significantly [R 2 = 0.199, F(3, 219) = 18.18, p < 0.001] fewer lessons (M = 6.2, SD = 2.6) compared to KULA (M = 7.7, SD = 0.5), HM (M = 7.8, SD = 1.1), and KOM (M = 7.9, SD = 0.5). However, the number of lessons received was not significantly associated with weight loss [r(221) = −0.039, p = 0.57].
Multivariate analysis predicting weight loss
Table 4 shows the GLM results of baseline weight, diastolic BP, ethnicity, and CBOs, and predicting post-intervention weight loss from baseline. The two-way interaction of CBO and ethnicity (Hawaiian vs. other) was not statistically significant. Thus, only main effects of these two variables were included in the model, which explained a small amount of the variance in weight loss [R 2 = 0.092, F(6,231) = 3.88, p = 0.0010]. Only baseline weight [F(1,231) = 9.33, p = 0.0025] and CBO [F(3,231) 4.11, p = 0.0073] were significant predictors of weight loss.
Post-hoc analysis
Because there were notable difference between KKV and the other three CBOs, we conducted a post-hoc secondary analysis to better understand possible factors contributing to these differences. It was found that higher educational obtainment was associated with more weight loss [Spearman correlation, ρ (n = 52) = 0.273, p = 0.0499] only within the KKV sample, but not within the other three CBOs [ρ (n = 186) = 0.033, p = 0.66]. A positive correlation between education level and number of lessons attended was also only found within the KKV sample [ρ (n = 52) = 0.43, p = 0.0017], but not within the other three CBOs [ρ (n = 170) = 0.056, p = 0.46].
Conducting one-way ANOVA within the KKV sample, there was no significant difference in weight loss between Chuukese and participants from other Pacific Islander ethnicities [F(1, 50) = 1.29, p = 0.26]. However, Chuukese tended to gain weight (M =0.39 kg, SD = 3.43) compared to the other participants (M = −0.63 kg; SD = 2.98). The effects of education level was stronger for Chuukese [F(1, 50) = 4.27, p = 0.044]: those with a high school or less education tended to gain weight (n = 17; M = 1.02; SD = 1.90), whereas those with higher than a high school education tended to lose weight (n = 35; M = − 0.85; SD = 3.49). Chuukese also attended less lessons (M = 5.35; SD = 2.60) than other participants (M = 6.63; SD = 2.53) but the difference was not significant [F(1, 50) = 2.86, p = 0.097].
DISCUSSION
Translating evidence-based interventions into real-world settings to benefit health disparate populations is a national priority in the U.S. [49, 50]. To address obesity disparities experienced by Native Hawaiians and Pacific Islanders, the POP translated the DPP-LI for these populations to initiate weight-loss efforts as part of a larger community-based lifestyle intervention. Following completion of the adapted DPP-LI the participants continued on in a weight loss maintenance program (not reported here). Overall, the translated DPP-LI yielded significant, although modest, weight loss (average of −1.7 kg), which was comparable to its pilot testing results (−1.5 kg) in another sample of Native Hawaiians and Pacific Islanders [29]. Significant improvements in systolic and diastolic BP, physical functioning and activity level, and dietary fat intake were also achieved. However, these outcomes were not comparable across the different types of CBOs where the intervention was delivered.
Three of the four CBOs (KULA, HM, and KOM) achieved a greater average weight loss (−2.0 to −2.3 kg) than that of the combined sample. To place these findings in the context of their clinical significance, the DPP showed that for every kilogram (or 2.2 lbs) of weight loss in a person with excess weight reduces his or her risk for diabetes by 16 % [3]. It is important to note that the three CBOs (KULA, HM, and KOM) with greater weight loss had predominantly Native Hawaiian participants (84 % to 87 %), making their intervention groups more ethnically homogenous in contrast to the fourth CBO (KKV). KKV's intervention groups had a more diverse Pacific Islander representation (i.e., Native Hawaiian, Chuukese, Filipino, and Samoan). These differences are expected given that KULA, HM, and KOM are predominately Native Hawaiian serving CBOs and KKV is a community health center serving mainly immigrant Pacific Islanders. A significant ethnic effect in weight-loss outcomes was not observed in this study, which may be partially due to the smaller sample size of Pacific Islanders other than Native Hawaiians. Notwithstanding, the difference between the weight-loss outcomes of KULA, HM, and KOM compared to KKV may be related to differences in socio-cultural (e.g., native vs. immigrant status) and socio-economic (e.g., living conditions) characteristics across Pacific Islander groups.
In conducting a post-hoc analysis to better understand the factors related to the lower weight loss achieved by participants in the KKV sample, it appears that education level may play a role in weight loss for immigrant Pacific Islanders, especially for Chuukese, but not so much for Native Hawaiians. Chuukese were the largest ethnic group in the KKV sample and were the group least likely to lose weight. They were also the ethnic group most likely to have less than a high school education, and education level was associated with their weight loss. Chuukese who had less than a high school education tended to attend less lessons than those with a high school education or greater. It would appear that, for Chuukese, either having a lower education level itself and/or factors related to having a lower education level, such as less stable employment, is adversely affecting their ability to fully participate in, and benefit from, a behavioral weight loss intervention. Fully participating in such an intervention is important given that studies have found a significant positive correlation between the number of prescribed lessons received and weight loss [30, 33].
Of Native Hawaiians and other Pacific Islanders in Hawai'i, Chuukese are the most economically disadvantaged and marginalized ethnic group. In addition to their lower educational obtainment on average, other factors related to their acculturation status may have affected their ability to fully benefit from the lifestyle intervention, such as poorer English proficiency, experiences of discrimination, and other social stressors. It appears that the adapted DPP-LI can be effective for Chuukese and other Pacific Islander immigrant groups with higher educational obtainment but questionable for those with lower educational obtainment.
Another possible factor related to the lower weight loss at KKV might have something to do with the ethnic mixing in their intervention groups. It is important to note that KKV has effectively implemented other health interventions [51], and KKV participants actually yielded the largest weight loss compared to the other three CBOs in the pilot testing of the translated DPP-LI in which a majority were Chuukese [29, 30]. Whereas their education status was similar in both studies, a notable difference between the groups at KKV in this study compared to the previous study is that they were much more heterogeneous. In the pilot study, KKV segregated the intervention groups by Pacific Islander ethnicity (e.g., Chuukese-, Samoan-, and Filipino-only groups), which allowed them to deliver the intervention in the native language of the participants. In the current study, they delivered the intervention to mixed groups of Native Hawaiians and Pacific Islanders and only delivered it in the English language (with the exception of one Chuukese-only in language group). This mixing of distinct Pacific Islander groups into a single intervention group may partly explain the lower weight loss observed among KKV participants in this study. It is likely that the socio-cultural differences between these groups may have influenced how the intervention was delivered and received (e.g., favoring examples more relevant to one group) and/or impeded the ability of participants to solicit the necessary social support from other group members.
There are socio-political tensions (e.g., competition for limited resources and negative stereotyping and discrimination) between Pacific Islander groups in Hawai'i [52], which may have interfered in their ability to fully participate and engage with each other. The more ethnically homogenous groups may have been able to form and sustain the needed social support network to assist them in achieving their lifestyle goals because of similar sociocultural and socioeconomic characteristics. Social support is an important factor in a person's weight-loss efforts when undergoing a behavioral lifestyle intervention [53, 54].
KULA's outcomes further point to the importance of social networks in obesity intervention for Native Hawaiian and Pacific Islanders. Their CBO yielded one of the highest mean weight losses and they were the only CBO that yielded significant improvements on all clinical and behavioral measures, to include systolic and diastolic BP. They are also the only CBO that is defined as a neighborhood (i.e., homestead community) compared to the other three CBOs that are defined as a community health center (KKV), health service organization (KOM), and a civic club (HM). Being a homestead community, the participants at KULA were more familiar to each other and lived amongst each other in the same immediate neighborhood, and the CHA delivering the intervention was from the community and knew most of the participants intimately. It is likely that this kind of familiarity and living situation led to better social networking to support the lifestyle modifications promoted by the intervention. KULA's participants were more likely to form community walking groups and participate in Zumba (a Columbian-inspired dance fitness program) and Hula (the traditional Hawaiian dance) classes as a group. Their shared Hawaiian values and interests may have also spurred this process, something that may be missing in mixed ethno-cultural intervention groups.
Overall, there was significant weight loss (−1.7 kg) and significant improvements in systolic and diastolic BP, physical functioning and activity level, and dietary fat intake. When placed in the context of being delivered by CHAs with varying backgrounds and who are relatively inexpensive to employ compared to traditional health professionals, and delivered in and across various community settings, it appears that the DPP-LI can be successfully translated into Native Hawaiian and Pacific Islander communities. However, it does appear that the weight loss and other clinical and behavioral benefits of this translated DPP-LI may be influenced by the ethnic composition of the intervention group and the degree to which social support and networking amongst the participants are possible. It is less likely that differences in the CHAs' experience and background across the CBOs contributed to the differences observed. All the CHAs followed the same standardized protocols and materials, confirmed by intermittent fidelity checks and regular meetings, and a majority of them also participated in the pilot study. Also, previous studies find no difference between lay educators and clinically trained professionals in the amount of weight loss achieved by their participants given the same intervention [28].
There are some limitations of this study. A pre- and post-intervention design was used, which does not allow us to compare against a no-intervention control group to determine the intervention's efficacy. However, the intent of this study was to translate the DPP-LI, which was already found efficacious, into real-world settings. Also, it is highly unlikely that the participants would have lost the amount of average weight loss observed and obtained the other clinical and behavioral benefits over 3 months in the absence of the intervention. The intervention may have not been delivered in the same manner as intended across CBO settings, which could have led to the differences observed. However, this is a translational study and real-world circumstances that would alter the delivery of the intervention are entirely expected and cannot be practically eliminated. Although most of the measures used were objective (i.e., weight, BP, and 6MWT), subjective measures of physical activity levels and dietary changes were used. Short of direct behavioral observations or daily self-monitoring of these behaviors, it is challenging to obtain more objective data, feasibly, from participants across diverse CBOs. Finally, the condensing of the DPP-LI may have weakened the weight loss effects of the intervention. However, most behavioral lifestyle interventions that apply stringent weight loss, caloric intake, and exercise goals are extremely difficult to maintain over time, especially for economically challenged communities.
Implications
The findings of this study have several important practice, policy, and research implications. In regards to the practice implications, the effective translation of evidence-based lifestyle interventions into real-world settings can occur when properly adapted to the specific characteristics of a population, such as those shared by ethnic populations and CBOs. They can be feasibly implemented using the human resources (e.g., lay community health educators) already inherent in many types of CBOs. Regarding policy implications, this study highlights the importance and benefits of expeditiously translating evidence-based intervention strategies into real-world contexts. The average reported 17-year delay in getting only 14 % of original scientific discoveries applied in real-world settings is unacceptable, given that they could have immediate public health benefits [55]. The POP's translation of the DPP-LI into Native Hawaiian and Pacific Islander communities demonstrates how evidence-based interventions can be rapidly disseminated using CBPR approaches [56]. This study's findings also suggest that more research is needed to elucidate the role of social support and social networking in obesity interventions, especially for economically challenged and socially marginalized groups, such as immigrants and indigenous peoples of the U.S. Overall, the findings of this study point to the importance of disaggregating Native Hawaiians and other Pacific Islanders in practice, policy, and research decisions. Differences in their acculturation history and status and socio-cultural and socio-economic characteristics may necessitate different public health intervention foci and strategies. It appears that a "one-size-fits-all" assumption is erroneous; that is, context matters in the translation of evidence-based interventions, whether it is the ethno-cultural, socio-economic, and/or CBO context.
References
Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999–2008. JAMA. 2010; 303(3): 235-241. doi:10.1001/jama.2009.2014[published Online First: Epub Date].
Ogden C, Carroll M. Prevalence of overweight, obesity, and extreme obesity among adults: United States, trends 1960–1962 through 2007–2008. Division of Health and Nutrition Examination Surveys: Centers for Disease Control and Prevention, 2010.
Hamman RF, Wing RR, Edelstein SL, et al. Effect of weight loss with lifestyle intervention on risk of diabetes. Diabetes Care. 2006; 29(9): 2102-2107. doi:10.2337/dc06-0560[published Online First: Epub Date].
World Health Organization. American Samoa NCD Risk Factors STEPS Report. Western Pacific Region, 2007.
Salvail F, Nguyen D, Liang S. State of Hawaii by demographic characteristics: Behavioral Risk Factor Surveillance System. Honolulu, HI: Hawaii State Department of Health; 2008.
Mau MK, Sinclair K, Saito EP, Baumhofer KN, Kaholokula JK. Cardiometabolic health disparities in Native Hawaiians and other Pacific Islanders. Epidemiol Rev. 2009; 31(1): 113-129. doi:10.1093/ajerev/mxp004[published Online First: Epub Date].
Grandinetti A, Kaholokula JK, Theriault AG, Mor JM, Chang HK, Waslien C. Prevalence of diabetes and glucose intolerance in an ethnically diverse rural community of Hawaii. Ethn Dis. 2007; 17(17): 250-255.
Schiller JS, Lucas JW, Ward BW, Peregoy JA. Summary health statistics for U.S. adults: National Health Interview Survey, 2010. National Center for Health Statistics. Vital Health Stat 2012;10(252)
National Institutes of Health. Strategic plan for NIH obesity research: a report of the NIH Obesity Research Task Force, March 2011.
Knowler W, Fowler S, Hamman R, Diabetes Prevention Program Research Group, et al. 10-Year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program outcomes study. Lancet. 2009; 374(9702): 1677-1686. doi:10.1016/s0140-6736(09)61457-4[published Online First: Epub Date].
Colditz GA, Emmons KM, Vishwanath K, Kerner JF. Translating science to practice: community and academic perspectives. J Public Health Manag Pract. 2008; 14(2): 144-149.
Woolf SH. The meaning of translational research and why it matters. JAMA. 2008; 299(2): 211-213. doi:10.1001/jama.2007.26[published Online First: Epub Date].
Zerhouni EA. Translational and clinical science — time for a new vision. New Engl J Med. 2005; 353(15): 1621-1623. doi:10.1056/NEJMsb053723[published Online First: Epub Date].
Vadheim LM, Brewer KA, Kassner DR, et al. Effectiveness of a lifestyle intervention program among persons at high risk for cardiovascular disease and diabetes in a rural community. J Rural Health. 2010; 26(3): 266-272. doi:10.1111/j.1748-0361.2010.00288.x[published Online First: Epub Date].
Delgadillo AT, Grossman M, Santoyo-Olsson J, Gallegos-Jackson E, Kanaya AM, Stewart AL. Description of an academic community partnership lifestyle program for lower income minority adults at risk for diabetes. Diabetes Educ. 2010; 36(4): 640-650. doi:10.1177/0145721710374368[published Online First: Epub Date].
Seidel MC, Powell RO, Zgibor JC, Siminerio LM, Piatt GA. Translating the diabetes prevention program into an urban medically underserved community — a nonrandomized prospective intervention study. Diabetes Care. 2008; 31(4): 684-689. doi:10.2337/dc07-1869[published Online First: Epub Date].
Whittemore R, Melkus G, Wagner J, Dziura J, Northrup V, Grey M. Translating the Diabetes Prevention Program to primary care: a pilot study. Nurs Res. 2009; 58(1): 2-12.
Myers VH, Ryan DH, Kaiser M, Butler M, Brantley PJ. The Lifestyle Change (TLC) Program: a translation of the Diabetes Prevention Program to a primary care setting for at-risk and disadvantaged patients. Ann Behav Med. 2010; 39(suppl 1): S145.
Schneider KL, Pagoto S, Sullivan C. Barriers and facilitators to translation of the Diabetes Prevention Program into a community mental health organization. Ann Behav Med. 2012; 43(suppl 1): S161.
McTigue KM, Conroy MB, Bigi L, Murphy C, McNeil M. Weight loss through living well: translating an effective lifestyle intervention into clinical practice. Diabetes Educ. 2009; 35(2): 199-208. doi:10.1177/0145721709332815[published Online First: Epub Date].
Yeary KH-cK, Cornell CE, Turner J, et al. Feasibility of an evidence-based weight loss intervention for a faith-based, rural, African American population. Prev Chronic Dis 2011;8(6)
Boltri JM, Davis-Smith M, Okosun IS, Seale JP, Foster B. Translation of the National Institutes of Health Diabetes Prevention Program in African American churches. J Natl Med Assoc. 2011; 103(3): 194-202.
West DS, Bursac Z, Cornell CE, et al. Lay health educators translate a weight-loss intervention in senior centers: a randomized controlled trial. Am J Prev Med. 2011; 41(4): 385-391. doi:10.1016/j.amepre.2011.06.041[published Online First: Epub Date].
Davis-Smith M. Implementing a diabetes prevention program in a rural African-American church. J Natl Med Assoc. 2007; 99(4): 440-446.
Ruggiero L, Castillo A, Quinn L, Hochwert M. Translation of the Diabetes Prevention Program's lifestyle intervention: role of community health workers. Curr Diab Rep. 2012; 12(2): 127-137. doi:10.1007/s11892-012-0254-y[published Online First: Epub Date].
Ruggiero L, Oros S, Choi YK. Community-based translation of the Diabetes Prevention Program's lifestyle intervention in an underserved Latino population. Diabetes Educ. 2011; 37(4): 564-572. doi:10.1177/0145721711411107[published Online First: Epub Date].
Brown BD, Harris KJ, Harris JL, Parker M, Ricci C, Noonan C. Translating the Diabetes Prevention Program for Northern Plains Indian youth through community-based participatory research methods. Diabetes Educ. 2010; 36(6): 924-935. doi:10.1177/0145721710382582[published Online First: Epub Date].
Ali MK, Echouffo-Tcheugui JB, Williamson DF. How effective were lifestyle interventions in real-world settings that were modeled on the Diabetes Prevention Program? Health Aff. 2012; 31(1): 67-75. doi:10.1377/hlthaff.2011.1009[published Online First: Epub Date].
Mau MK, Kaholokula JK, West M, et al. Translating diabetes prevention into Native Hawaiian and Pacific Islander communities: the PILI 'Ohana Pilot project. Prog Community Health Partnersh. 2010; 4(1): 7-16.
Kaholokula JK, Mau MK, Efird JT, et al. A family and community focused lifestyle program prevents weight regain in pacific islanders: a pilot randomized controlled trial. Health Educ Behav 2012:386–95
Wing RR, Jeffery RW. Achieving weight and activity goals among diabetes prevention program lifestyle participants — the Diabetes Prevention Program Research Group. Obes Res. 2004; 12(9): 1426-1434.
Parikh P, Simon EP, Fei K, Looker H, Goytia C, Horowitz CR. Results of a pilot diabetes prevention intervention in East Harlem, New York City: Project HEED. Am J Public Health. 2010; 100(suppl 1): S232-S239. doi:10.2105/AJPH.2009.170910[published Online First: Epub Date].
Hollis JF, Gullion CM, Stevens VJ, et al. Weight loss during the intensive intervention phase of the weight-loss maintenance trial. Am J Prev Med. 2008; 35(2): 118-126. doi:10.1016/j.amepre.2008.04.013[published Online First: Epub Date].
World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications; 2000.
Nacapoy AH, Kaholokula JK, West MR, et al. Partnerships to address obesity disparities in Hawai'i: the PILI 'Ohana Project. Hawaii Med J. 2008; 67(9): 237-241.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall; 1986.
Diabetes Prevention Program Research G. The Diabetes Prevention Program (DPP): description of lifestyle intervention. Diabetes care. 2002; 25(12): 2165-2171.
Diabetes Prevention Program Outcomes Study Research G, Orchard TJ, Temprosa M, et al. Long-term effects of the Diabetes Prevention Program interventions on cardiovascular risk factors: a report from the DPP Outcomes Study. Diabetic Med. 2013; 30(1): 46-55. doi:10.1111/j.1464-5491.2012.03750.x[published Online First: Epub Date].
Michie S, Richardson M, Johnston M, et al. The Behavior Change Technique Taxonomy (v1) of 93 Hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Annals of behavioral medicine. 2013; 46(1): 81-95. doi:10.1007/s12160-013-9486-6[published Online First: Epub Date].
Knowler WC, Barrett-Connor E, Fowler SE, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New Engl J Med. 2002; 346(6): 393-403.
Ammerman AS, Lindquist CH, Lohr KN, Hersey J. The efficacy of behavioral interventions to modify dietary fat and fruit and vegetable intake: a review of the evidence. Preventive medicine. 2002; 35(1): 25-41.
Anderson ES, Wojcik JR, Winett RA, Williams DM. Social-cognitive determinants of physical activity: the influence of social support, self-efficacy, outcome expectations, and self-regulation among participants in a church-based health promotion study. Health Psychol. 2006; 25(4): 510-520. doi:10.1037/0278-6133.25.4.510[published Online First: Epub Date].
Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Annals of behavioral medicine. 2007; 34(3): 304-312. doi:10.1080/08836610701677659[published Online First: Epub Date].
Hermans RC, Larsen JK, Herman CP, Engels RC. Effects of social modeling on young women's nutrient-dense food intake. Appetite. 2009; 53(1): 135-138. doi:10.1016/j.appet.2009.05.004[published Online First: Epub Date].
American Thoracic Society. ATS statement: guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med. 2002; 166(1): 111-117.
Du H, Newton PJ, Salamonson Y, Carrieri-Kohlman VL, Davidson PM. A review of the six-minute walk test: its implication as a self-administered assessment tool. Eur J Cardiovasc Nurs. 2009; 8(1): 2-8. doi:10.1016/j.ejcnurse.2008.07.001[published Online First: Epub Date].
Marshall AL, Smith BJ, Bauman AE, Kaur S. Reliability and validity of a brief physical activity assessment for use by family doctors. Brit J Sport Med. 2005; 39(5): 294-297.
Kristal AR, Beresford SA, Lazovich D. Assessing change in diet-intervention research. Am J Clin Nutr. 1994; 59(suppl 1): S185-S189.
Glasgow RE, Green LW, Taylor MV, Stange KC. An evidence integration triangle for aligning science with policy and practice. Am J Prev Med. 2012; 42(6): 646-654. doi:10.1016/j.amepre.2012.02.016[published Online First: Epub Date].
Koh HK, Oppenheimer SC, Massin-Short SB, Emmons KM, Geller AC, Viswanath K. Translating research evidence into practice to reduce health disparities: a social determinants approach. Am J Public Health. 2010; 100(suppl 1): S72-S80. doi:10.2105/Ajph.2009.167353[published Online First: Epub Date].
Sinclair KA, Makahi EK, Solatorio CS, Yoshimura SR, Townsend CKM, Kaholokula JK. Outcomes from a diabetes self-management intervention for Native Hawaiians and Pacific Peoples: Partners in Care. Ann Behav Med. 2013; 45(1): 24-32.
McDermott JF, Andrade NN, eds. Peoples and culture of Hawaii: the evolution of culture and ethnicity. Honolulu, HI: University of Hawaii Press; 2011.
Wing RR, Jeffery RW. Benefits of recruiting participants with friends and increasing social support for weight loss and maintenance. J Consult Clin Psych. 1999; 67(1): 132-138.
Bishop J, Irby MB, Isom S, Blackwell CS, Vitolins MZ, Skelton JA. Diabetes prevention, weight loss, and social support: program participants' perceived influence on the health behaviors of their social support system. Family & Community Health. 2013; 36(2): 158-171.
Balas EA. From appropriate care to evidence-based medicine. Pediatric annals. 1998; 27(9): 581-584.
Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: the intersection of science and practice to improve health equity. Am J Public Health. 2010; 100(Suppl 1): S40-S46. doi:10.2105/ajph.2009.184036[published Online First: Epub Date].
Acknowledgements
The authors thank the PILI 'Ohana Project participants, community researchers, and staff of the participating community organizations: Hawai'i Maoli — the Association of Hawaiian Civic Clubs, Ke Ola Mamo, Kula no nā Po'e Hawai'i, and Kōkua Kalihi Valley Comprehensive Family Services, Honolulu, Hawai'i. This study was supported by the National Institute on Minority Health and Health Disparities (NIMHD) with awards to the PILI 'Ohana Program: Partnerships to Overcome Obesity Disparities in Hawaii (grant number R24MD001660). GXZ and JC were partially supported by two NIMHD institutional infrastructure grants (grant numbers U54MD007584 and G12MD007601). The content is solely the responsibility of the authors and does not necessarily represent the official views of National Institute on Minority Health and Health Disparities or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Additional information
Implications
Practice: Evidence-based lifestyle interventions can be effectively translated into real-world settings when adapted to a specific ethnic population and the characteristics of community-based organizations, and they can be feasibly implemented using in place human resources.
Policy: The expeditious translation of evidence-based intervention strategies into real-world contexts is needed to address serious shortfalls in the application of scientific discoveries.
Research: More research is needed to elucidate the role of social support and networking in obesity interventions, especially for economically challenged and socially marginalized groups, such as immigrants and indigenous peoples.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kaholokula, J.K., Wilson, R.E., Townsend, C.K.M. et al. Translating the Diabetes Prevention Program in Native Hawaiian and Pacific Islander communities: the PILI ‘Ohana Project. Behav. Med. Pract. Policy Res. 4, 149–159 (2014). https://doi.org/10.1007/s13142-013-0244-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13142-013-0244-x