Abstract
Introduction
Perforation peritonitis is one of the most common surgical emergencies encountered by general surgeons in India. The spectrum of aetiology of perforation differs from its western counterpart. This prospective study conducted at a tertiary healthcare centre was designed to highlight the spectrum of perforation in terms of aetiology, presentation site of perforation, surgical treatment and postoperative complications so as to improve its outcome in our region.
Methods
This was a single-centre prospective cohort study conducted by the department of surgery from January 2001 to December 2014. In total, 1908 consecutive cases of perforation peritonitis admitted to surgical unit 6 were recruited in the study. Continuous variables are presented as mean ± SD, and categorical variables are presented as absolute numbers and percentages.
Results
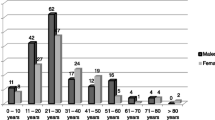
The mean age of the patients was 34.42 years (range 18 to 60 years) and the standard deviation was ± 11.10. The majority of patients were male (77.6%). Perforated duodenal ulcer due to acid-peptic disease and small bowel perforation due to typhoid were the most common causes of perforation peritonitis, followed by small bowel tubercular perforations. Postoperative complications included wound infection 18.4%, wound dehiscence 3.9%, respiratory complications 10.5%, septicaemia 5.2%, and abdominal collection 3.9%.
Conclusion
Perforation peritonitis is still a dreadful disease. Malignancy is a rare cause in our region. Resuscitation before surgery improves outcome. The formation of only a stoma in bowel perforations and omentopexy in the stomach and duodenum perforations rather than extensive emergency surgery contribute to low mortality.
Similar content being viewed by others
References
Ramakrishnan K, Salinas RC. Peptic ulcer disease. Am Fam Physician 2007; 76:1005–12
Sharma L, Gupta S, Soin AS, et al. Generalized peritonitis in India. The tropical spectrum. Jpn J Surg 1991; 21:272–7
Ersumo T, W/Meskel Y, Kotisso B. Perforated peptic ulcer in Tikur Anbessa Hospital; a review of 74 cases. Ethiop Med J 2005; 43:9–13
Adesunkanmi AK, Badmus TA, Fadiora FO, et al. Generalized peritonitis secondary to typhoid ileal perforation: Assessment of severity using modified APACHE II score. Indian J Surg 2005; 67:29–33
Adesunkanmi ARK, Badmus TA, Ogundoyin OO. Causes and determinants of outcome of intestinal perforations in a semiurban African community. Surg Pract 2003; 7:116–23
Agarwall N, Saha S, Srivastava A, et al. Peritonitis: 10 years experience in a single surgical unit. Trop Gastroenterol 2007; 28:117
Malangoni MA, Inui T. Peritonitis the western experience. World J Emerg Surg 2006; 1:2
Gupta S, Kaushik R. Peritonitis—the Eastern experience. World J Emerg Surg 2006; 1:13
Siu WT, Leong HT, Law BK, et al. Laproscopic repair for perforated peptic ulcer. A randomized controlled trial. Ann Surg 2002; 235:313–9
Jhobta RS, Attri AK, Kaushik R, et al. Spectrum of perforation peritonitis in India—review of 504 consecutivecases. World J Emerg Surg 2006; 1:26
Veliyev NA, Merrell RC. Differentiated approach to surgical treatment of patients with perforatred duodenal ulcer. Chirurgia (Bucur) 2004; 99:119–23
Koninger J, Bottinger P, Redeeke J, et al. Laparoscopic repair of perforated gastroduodenal ulcer by running suture. Langenbecks Arch Surg 2004; 389:11–6
Ohene-Yeboah M, Togbe B. Perforated gastric and duodenalulcers in an urban African population. West Afr J Med 2006; 25:205–11
Franco R, Simone R, Daniele M, et al. Perforated gastric carcinoma; a report of 10 cases and review of the literature. World J Surg Oncol 2006; 4:19
Sefr R, Rotterova P, Konecny J. Perforation peritonitis in primary intestinal tuberculosis. Case report. Dig Surg 2001; 18:475–9
Collado C, Stirnemann J, Ganne N, et al. Gastrointestinal tuberculosis: 17 cases collected in 4 hospitals in the northeastern suburb of Paris. Gastroenterol Clin Boil 2005; 9:419–24
Muquit S, Shah M, Abayajeewa K. A case of miliary tuberculosis presenting with bowel perforation: Newham University Hospital, London, UK. Emerg Med J 2006; 23:e62
Sharma MP, Vikram B. Abdominal tuberculosis. Indian J Med Res 2004; 120:305–15
Seward E. Hyperplastic tuberculosis of the intestine. Ann Surg 1920; 71:637–44
Kasahara K, Fukuoka K, Okamura H, et al. Tuberculous peritonitis developing during chemotherapy for pulmonary and intestinal tuberculosis. Respirology 2005; 10:257–60
Ara C, Sogutlu G, Yildiz R, et al. Spontaneous small bowel perforation due to intestinal tuberculosis should not be repaired by simple closure. J Gastrointest Surg 2005; 9:514–7
Ramesh J, Banait GS, Ormerod LP. Abdominal tuberculosis in a district general hospital. A retrospective review of 86 cases. QJM 2008; 10:189–95
Saxe JM, Cropsey R. Is operative management effective in treatment of perforated typhoid? Am J Surg 2005; 189:342–4
Ramachandran CS, Agarwal S, Dip DG, et al. Laproscopic surgical management of perforative peritonitis in enteric fever: a preliminary study. Surg Laprosc Endosc Percutan Tech 2004; 14:122–4
Di Venere B, Testini M, Miniello S, et al. Rectal perforations. Personal experience and literature review. Minerva Chir 2002; 57:357–62
Breitenstein S, Kraus A, Hahnloser D, et al. Emergency left colon resection for acute perforation: Primary anastomosis or Hartmann’s procedure? A case matched control study. World J Surg 2007; 31:2117–24
Oheneh-Yeboah M. Postoperative complications after surgery for typhoid illeal perforation in adults in Kumasi. West Afr J Med 2007; 26:32–6
Ozman MM, Zulfikaroglu B, Kece C, et al. Factors influencing mortality in spontaneous gastric tumor perforations. J Inter Med Res 2002; 30:180–4
Capoor MR, Nair D, Chintamani MS, et al. Role of Enteric fever in ileal perforation. Indian J Med Microbiol 2008; 26:54–7
Shinkawa H, Yasuhara H, Naka S, et al. Factors afecting the early mortality of patients with non-traumatic colorectal perforation. Surg Today 2003; 33:13–7
Uccheddu A, Floris G, Altana ML, et al. Surgery for perforated peptic ulcer in the elderly. Evaluation of factors influencing prognosis. Hepatogastroenterology 2003; 50:1956–8
Subramanyam SG, Sunder N, Saleem KM. Peritonitis in patients over the age of 50 years: 98 cases managed surgically. Trop Doct 2005; 35:247–50
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nabi, I., Munjewar, C., Ranjan, G. et al. Spectrum of perforation peritonitis at a tertiary healthcare centre: A prospective cohort study of 1908 cases. Hellenic J Surg 88, 181–185 (2016). https://doi.org/10.1007/s13126-016-0312-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13126-016-0312-z