Abstract
Background
Perforation is a rare complication of gastric carcinoma, accounting for less than 1% of all gastric cancer cases. The aim of the present study is to evaluate the prognostic value of perforation and to point out the surgical treatment options.
Methods
A total of 10 patients with perforated gastric carcinoma were retrospectively reviewed among 2564 consecutive cases of gastric cancer operated in three Centers belonging to the Italian Research Group for Gastric Cancer. The clinicopathological features including tumor stage and survival were analyzed and compared to literature data.
Results
Incidence rate was 0.39%. All patients underwent emergency surgery, being performed gastrectomy in 6 patients (mortality 17%) and repair surgery in 4 patients (mortality 75%). The survival of patients was related to the stage of the disease, with 2 long-survival cases.
Conclusion
Perforation usually occurs in advanced stages of gastric cancer; nevertheless surgeons should not be always discouraged from a radical treatment of perforated gastric cancer, since perforation even occurs in early stages and seems not to be a negative prognostic factor itself. When possible, emergency gastrectomy should be performed, leaving repair surgery for unresectable tumors. A two-stage treatment is a good treatment option for frail patients with resectable tumors.
Similar content being viewed by others
Background
Perforation of gastric carcinoma results in an acute abdominal syndrome due to the spilled gastric contents and the consequent peritonitis. It is a rare condition representing less than 1% of gastric cancer cases in the reports of the last years[1, 2] and up to 6% in reports dated before 1980 [3–5]; it has been reported that about 10–16% of all gastric perforations are caused by gastric carcinoma [6–9]. In most instances gastric carcinoma is not suspected as the cause of perforation prior to emergency laparotomy and the diagnosis of malignancy is often made only on postoperative pathologic examination. It is often difficult to recognize the kind of lesion that caused gastric perforation at the time of emergency surgery, particularly when pathologic evaluation of frozen sections is not available. The treatment should aim to manage both the emergency condition of peritonitis and the oncologic technical aspects of surgery: it may be hazardous to embark on a major procedure observing the principles of radical oncological surgery; on the other hand a limited procedure only may jeopardize long-term survival in a patient with potentially curable gastric malignancy. In order to further understand the optimal management of patients with perforated gastric cancer, we reviewed the clinicopathological features and surgical results in our experience, comparing data with the International literature.
Methods
We reviewed the medical records of 2564 patients with gastric cancer who had undergone surgical treatment in three Centers belonging to the Italian Research Group for Gastric Cancer (IRGGC): Dipartimento di Chirurgia Generale ed Oncologica, University of Siena, Istituto di Semeiotica Chirurgica, University of Verona and Divisione di Chirurgia 1, G.B. Morgagni Hospital, Forlì. Ten patients (0.39%) were treated for perforated gastric carcinoma. The clinicopathological features of all patients were analyzed on the basis of their medical records. Age and sex, preoperative diagnosis, location of perforation, depth of gastric wall invasion, absence or presence of lymph node metastasis, type of surgery, degree of lymph node dissection, UICC stage and outcome of the patients were examined. Overall survival from the time of primary operation was calculated using Kaplan-Meier estimates. A search of the literature was conducted in the Medline database; the terms "perforated", "perforation", "gastric cancer", "gastric ulcer" were associated for the search and English language journals only were selected.
Results
Clinicopathological features of patients are given in Table 1. The incidence rate of perforation among gastric carcinoma was 0.39%. Most cases were tumors invading serosa (4/6) and with metastatic lymph nodes (4/6). The disease was more frequently in stages III/IV (7/10), but one case (1/10) of stage I gastric cancer was also observed. All patients underwent emergency surgery. In only 3 patients on 10 a preoperative diagnosis of gastric carcinoma was made. Table 2 shows surgical and postsurgical survival data. Operations performed were gastrectomy in 6 patients and simple closure in 4 patients. Surgery-related deaths were observed in 4 patients: 3 of them underwent simple closure and 1 subtotal gastrectomy. All tumors treated with simple closure were at clinical stage IV of the disease and emergency gastrectomy was not performed because of the advanced stage with adjacent organs invasion. Five subtotal gastrectomies (4 D1 and 1 D2) and one D3 total gastrectomy were performed. Three surgical and two non-surgical complications were observed. The only patient who survived surgery after simple repair died at 5.2 months from operation for the primary disease. The only patient who underwent gastrectomy whose death was surgery-related was 80 and presented cardiologic comorbidity. Two patients underwent adjuvant chemotherapy and they both are still alive after 47.7 and 41.6 months after surgery, one with no evidence of disease and the other with bone recurrence.
Discussion
Perforation is a rare complication of gastric cancer. In our series an incidence of less than 1% (0.39%) was observed comparable to the most recent studies[1, 2]. Preoperative diagnosis of malignancy is unusual, accounting for about 30% of cases[1, 2, 10]; the other patients are usually accepted for acute abdomen at the Emergency Units where generic preoperative diagnosis of gastroduodenal perforation is made. The only preoperative feature that may guide the surgeon is the age of the patient: perforated gastric carcinoma usually occurs in patients with a mean age of 65 years (68 years in our series) in contrast with the mean age of 51 years of the patients with perforated peptic ulcers [9–13]. Even during surgery the gastric ulcer is often diffucult to be characterized as benign or malignant by the surgeon. Therefore a biopsy and frozen section should be performed in all gastric perforations when a pathologist is available. Histologic determination is fundamental for the surgeon to choose the type of operation and to perform it with oncological criteria, for example considering adequate distance from the lesion and the resection margin. Malignant gastric perforation is more often a manifestation of advanced cancer with serosal invasion (55–82%) and lymph node metastasis (57–67%). Nevertheless, as confirmed by different observations[14, 15], gastric cancer can perforate at an early stage. Indeed at the pathologic examination of specimens, the process of gastric wall perforation is sustained by infectious and ischaemic factors due to the tumoral neovascularization which result in the shedding of the neoplastic tissue[3, 16].
It is still debated whether positive peritoneal cytology has an independent prognostic impact in gastric cancer. Several studies have noted free gastric cancer cells in the peritoneum to be associated with poor prognosis[17, 18]. However, viable free cancer cells have not been demonstrated in the peritoneal cavity of patients with perforated gastric cancer and the metastatic efficiency of gastric cancer cells possibly shed during perforation is uncertain in the presence of the peritonitis; different studies, included the present one, report of long-term survivors[19]. When a curative operation can be performed, survival rates after gastric cancer perforation[1, 20] appear similar to survival rates observed in elective patients[21, 22]. Moreover, Gertsch et al. demonstrated how the only factor predicting long term survival is the TNM stage, while age or the size, the location, the depth of infiltration and the histologic grading of the tumor or a delay in treatment after perforation showed no correlation with long-term survival[10]. Earlier, in 1997, Adachi et al. reviewed 155 cases of perforated gastric cancer collected from the Japanese literature finding that infiltrative gross type of the tumor, presence of serosal invasion, presence of lymph node metastasis, stage III-IV and curability of the tumor were the only negative prognostic factors influencing the 5-years survival rate, while age, sex, location, histologic type and type of lymph node dissection were not found to be significantly related to the long term survival[1]. In another study of Gertsch et al., the Authors compared three groups of patients with perforated, bleeding and non-complicated gastric cancer, finding that perforation, as well as bleeding, does not significantly affect long term survival after gastrectomy[23].
Treatment of choice is still debated. Table 3 shows the results of our research in the International English literature. From the first study of Aird[24] in 1935 until the early 1980's we found how the most frequent type of operation performed for perforated gastric cancer was the simple closure or the omental patch, sometimes associated with gastroenteroanastomosis. In these papers is also shown the high surgery-related mortality of this type of surgery, nevertheless surgeons seemed to prefer simple repair, probably because malignant gastric perforation, with consequent peritoneal dissemination of tumor cells, was generally thought to be always a manifestation of terminal disease. Of course, the high mortality of simple closure is also due to the different kind of patients who undergo this type of minimal surgery: this approach is usually preferred for minimal therapy in frail patients or in advanced unresectable tumors. Therefore over the years the resection rate has been increasing and the overall mortality rate has been decreasing. In 2002 Lehnert et al.[9] proposed the two-stage radical gastrectomy as the treatment of choice in the majority of patients with perforated gastric cancer: this approach aims to avoid major surgical procedures in emergency performing a first-step simple closure or a gastric resection and later, a secondary elective gastrectomy with oncological radicality intent. This kind of approach has been approved by Ozmen et al.[25] who found that preoperative shock is a negative prognostic factor influencing surgery-related mortality.
Conclusion
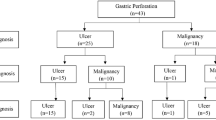
From the the personal experience of the IRGGC and from the studies reported in the literature we tried to make the point for the treatment of choice of perforated gastric carcinoma. Perforated gastric carcinoma is not to be considered as a unique disease, but the surgeon should consider the single elements that compose every peculiar clinical case. The treatment of the peritonitis would require a minimal surgery in order to avoid major procedures in an emergency situation; on the other hand the treatment of gastric cancer would require an oncological-oriented surgery in order to satisfy oncological radicality criteria. These two aims are not always compatible in a single emergency surgical treatment. The most important factors to be recalled in the management of a patient with histological diagnosis of perforated gastric carcinoma are: 1) the presence of preoperative shock[26]; 2) the gravity of peritonitis; 3) the curability of the neoplasm; 4) eventual comorbidities of the patient. If we add together points 1, 2 and 4 considering them as the general condition of the patient, we may identify four classes of patients with different options for surgical treatment (Figure 1). If a patient has a curable tumor and acceptable general condition, for example no signs of shock, localized peritonitis and no comorbidities, the treatment of choice seems to be radical total or subtotal gastrectomy with associated D2 or D3 lymphadenectomy or, for a less aggressive approach, two-stage radical gastrectomy. When general condition is good but the tumor is at an advanced stage with no possibility of R0 resection, a palliative gastrectomy, if technically possible, is recommended considering the minor surgery-related mortality[27]. Two-stage radical gastrectomy seems to find its peculiar indication when general condition is poor but a curative resection is possible, even though this approach was never chosen in our experience. Simple repair or omental patch are reserved only for those patients with advanced stage disease and whose general condition is poor. If a pathologist is not available and histologic examination is not possible during surgery, we suggest to perform a gastric resection, since for perforated peptic ulcer too the treatment of choice is resection both for the better morbility and the lower rate of recurrence [28–30]; only intraoperative hemodynamic instability should limit operative selection to a faster procedure. In both cases when the postoperative histologic examination would assess the malignancy of the ulcer a secondary radical gastrectomy is mandatory.
References
Adachi Y, Mori M, Maehara Y, Matsumata T, Okudaira Y, Sugimachi K: Surgical results of perforated gastric carcinoma: an analysis of 155 Japanese patients. Am J Gastroenterol. 1997, 92 (3): 516-8.
Kasakura Y, Ajani JA, Fujii M, Mochizuki F, Takayama T: Management of perforated gastric carcinoma: a report of 16 cases and review of world literature. Am Surg. 2002, 68: 434-40.
Stechenberg L, Bunch RH, Anderson MC: The surgical therapy for perforated gastric cancer. Am Surg. 1981, 47: 208-210.
McNealy RW, Hedin RF: Perforation in gastric carcinoma. J Am Coll Surg. 1938, 67: 818-823.
Bisgard JD: Gastric resection for certain acute perforated lesions of stomach and duodenum with diffuse soiling of the peritoneal cavity. Surgery. 1945, 17: 498-509.
Sage M, Ghoutti A, Delalande JP, Alexandre JH, Champault G, Patel JC: Notre expérience clinique de dix cas de péritonite par perforation de cancer gastrique au cours de la dernière décenne. Ann Chir. 1983, 37: 355-359.
Kennedy TL: Gastric carcinoma and acute perforation. Brit Med J. 1951, 2: 1489-
Mouchet A, Marquand J: A propos de 2 cas de perforations en péritoine libre des néoplasmes gastriques. Arch Mal Appar Dig. 1953, 42: 634-645.
Lehnert T, Buhl K, Dueck M, Hinz U, Herfarth C: Two-stage radical gastrectomy for perforated gastric cancer. Eur J Surg Oncol. 2000, 26: 780-784. 10.1053/ejso.2000.1003.
Gertsch P, Yip SKH, Chow LWC, Lauder IJ: Free perforation of gastric carcinoma. Results of surgical treatment. Arch Surg. 1995, 130: 177-181.
Cortese AF, Zahn D, Cornell GN: Perforation in gastric malignancy. J Surg Oncol. 1972, 4: 190-206.
Wilson TS: Free perforation in malignancies of the stomach. Can J Surg. 1966, 9: 357-364.
Larmi TKI: Perforation of gastric carcinoma. Acta Chir Scand. 1962, 123: 222-227.
Andreoni B, Salvini P, Gridelli B, Balestri M, Strada L, Tognini L, Grezzi C, Bevilacqua G: Diagnostic précoce du cancer de l'estomac: 23 cas dont 15 avec complication aigue d'hémorragie ou de perforation. J Chir (Paris). 1981, 118: 253-259.
Kitakado Y, Tanigawa N, Muraoka R: A case report of perforated early gastric cancer. Nippon Geka Hokan. 1997, 66: 86-90.
Sarro Palau M, Sans Segarra M: Cirugia de urgencia en el cancer gastrico. Rev Esp Enf Ap Digest. 1974, 42: 529-536.
Bonenkamp JJ, Songun I, Hermans J, van de Velde CJ: Prognostic value of positive cytology findings from abdominal washing in patients with gastric cancer. Br J Surg. 1996, 83: 672-674.
Wu CC, Chen JT, Chang MC, Ho WL, Chen CY, Yeh DC, Liu TJ, P'eng FK: Optimal surgical strategy for potentially curable serosa-involved gastric carcinoma with intraperitoneal cancer cells. J Am Coll Surg. 1997, 184: 611-617.
Adachi Y, Aramaki M, Shiraishi N, Shimoda K, Yasuda K, Kitano S: Long-term survival after perforation of advanced gastric cancer: case report and review of the literature. Gastric Cancer. 1998, 1: 80-83. 10.1007/s101200050059.
Miura T, Ishii T, Shimoyama T, Hirano T, Tomita M: Surgical treatment of perforated gastric cancer. Dig Surg. 1985, 2: 200-204.
Cuschieri A, Weeden S, Fielding J, Bancewicz J, Craven J, Joypaul V, Sydes M, Fayers P: Patient survival after D1 and D2 resections for gastric cancer: long term results of the UK MRC randomised surgical trial. Br J Cancer. 1999, 79: 1522-1530. 10.1038/sj.bjc.6690243.
Bonenkamp JJ, Hermans J, Sasako M, van de Velde CJ: Extended lymph-node dissection for gastric cancer. N Engl J Med. 1999, 340: 908-914. 10.1056/NEJM199903253401202.
Gertsch P, Choe LWC, Yuen ST, Chau KY, Lauder IJ: Long term survival after gastrectomy for advanced bleeding or perforated gastric carcinoma. Eur J Surg. 1996, 162: 723-727.
Aird I: Perforation of carcinoma of the stomach into the general peritoneal cavity. Br J Surg. 1935, 22: 545-554.
Ozmen MM, Zulfikaroglu B, Kece C, Aslar AK, Ozalp N, Koc M: Factors influencing mortality in spontaneous gastric tumour perforations. J Int Med Res. 2002, 30: 180-184.
So JBY, Yam A, Cheah WK, Kum CK, Goh PM: Risk factors related to operative mortality and morbidity in patients undergoing emergency gastrectomy. Br J Surg. 2000, 87: 1702-1707. 10.1046/j.1365-2168.2000.01572.x.
Kasakura Y, Ajani JA, Mochizuki F, Morishita Y, Fujii M, Takayama T: Outcomes after emergency surgery for gastric perforation or severe bleeding in patients with gastric cancer. J Surg Oncol. 2002, 80: 181-185. 10.1002/jso.10127.
McGee GS, Sawyers JL: Perforated gastric ulcers. A plea for management by primary gastric resection. Arch Surg. 1987, 122: 555-561.
Tsugawa K, Koyanagi N, Hashizume M, Tomikawa M, Akahoshi K, Ayukawa K, Wada H, Tanoue K, Sugimachi K: The therapeutic strategies in performing emergency surgery for gastroduodenal ulcer perforation in 130 patients over 70 years of age. Hepatogastroenterology. 2001, 48: 156-162.
Vibert E, Boufflerd C, Régimbeau JM, Menegaux F: Ulcère gastrique perforé: suture ou gastrectomie?. Ann Chir. 2005, 130: 92-95. 10.1016/j.anchir.2005.01.006.
Casberg MA: Perforation as complication of gastric carcinoma. Arch Surg. 1940, 41: 937-944.
Siegert TA, Donegan WL: Acute perforation of gastric carcinoma. Wis Med J. 1982, 81: 17-21.
Acknowledgements
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
FR: conceived of the study and participated in the design of the study
SR: participated in the design of the study and drafted the manuscript
DM: participated in the design of the study and performed the statistical analysis
GDM: participated in the design of the study
CP: participated in the design of the study
PM: participated in the design of the study
GC: participated in the design of the study and helped to draft the manuscript
EP: coordinated the study
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Roviello, F., Rossi, S., Marrelli, D. et al. Perforated gastric carcinoma: a report of 10 cases and review of the literature. World J Surg Onc 4, 19 (2006). https://doi.org/10.1186/1477-7819-4-19
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-7819-4-19