Abstract
Nonalcoholic fatty liver disease (NAFLD) is the most prevalent form of chronic liver disease in the world. New non-invasive diagnostic tools are needed to promptly treat this disease and avoid its complications. This study aimed to find key metabolites and related variables that could be used to predict and diagnose NAFLD. Ninety-eight subjects with NAFLD and 45 controls from the Fatty Liver in Obesity (FLiO) Study (NCT03183193) were analyzed. NAFLD was diagnosed and graded by ultrasound and classified into two groups: 0 (controls) and ≥ 1 (NAFLD). Hepatic status was additionally assessed through magnetic resonance imaging (MRI), elastography, and determination of transaminases. Anthropometry, body composition (DXA), biochemical parameters, and lifestyle factors were evaluated as well. Non-targeted metabolomics of serum was performed with high-performance liquid chromatography coupled to time-of-flight mass spectrometry (HPLC-TOF-MS). Isoliquiritigenin (ISO) had the strongest association with NAFLD out of the determinant metabolites. Individuals with higher concentrations of ISO had healthier metabolic and hepatic status and were less likely to have NAFLD (OR 0.13). Receiver operating characteristic (ROC) curves demonstrated the predictive power of ISO in panel combination with other NAFLD and IR-related variables, such as visceral adipose tissue (VAT) (AUROC 0.972), adiponectin (AUROC 0.917), plasmatic glucose (AUROC 0.817), and CK18-M30 (AUROC 0.810). Individuals with lower levels of ISO have from 71 to 82% more risk of presenting NAFLD compared to individuals with higher levels. Metabolites such as ISO, in combination with visceral adipose tissue, IR, and related markers, constitute a potential non-invasive tool to predict and diagnose NAFLD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is defined as the presence of steatosis in at least 5% of hepatocytes in the absence of excessive alcohol intake [8]. Currently, NAFLD represents the most common form of chronic liver disease in the world, with a continuously growing prevalence of approximately 30% of the overall population [35, 62].
NAFLD is greatly associated with obesity and its related comorbidities, such as type 2 diabetes mellitus, insulin resistance, dyslipidemias, and cardiovascular disease. Forsooth, NAFLD may be considered the hepatic manifestation of metabolic syndrome [79]. NAFLD encompasses simple steatosis and non-alcoholic steatohepatitis (NASH), its inflammatory phenotype. The progress of the disease to NASH is strongly related to an increased risk of fibrosis, cirrhosis, end-stage liver disease, and hepatocellular carcinoma [62].
NAFLD’s pathogenesis is complicated and multifactorial, involving individual elements such as lifestyle factors, genetics, and gut microbiota composition [13]. Nevertheless, increased inflammation and oxidative stress are among the main physio-pathological mechanisms involved in the development and progression of the disease [64, 76].
Liver biopsy is considered the gold-standard diagnostic methodology for NAFLD; however, this technique is invasive and expensive and cannot be applied as a routine checkup in the population [30]. Subrogate routine markers (transaminases), several scores and indexes (fatty liver index, FLI), and imaging techniques, such as magnetic resonance imaging (MRI) and ultrasonography, have also been proposed to diagnose this disease [7]. Nevertheless, NAFLD continues to be a silent epidemic that is manifested when there are advanced stages of fibrosis [59]. In this regard, there is increasing interest in finding non-invasive diagnostic markers that could help in the early diagnosis of this disease [35].
An early diagnosis of NAFLD with non-invasive methods may be a key factor in treating promptly this disease and avoiding its many complications [34]. In this sense, omics technologies represent an excellent tool, particularly helpful for the early diagnosis of several diseases [48, 63]. Recently, metabolomics has gained attention in the field of metabolic diseases, not only because of its ability to elucidate biomarkers but because, since metabolites directly influence metabolism, they could contribute to explain the pathophysiology of such diseases as well [27,28,29, 74].
With this background, this study aimed to identify and deepen the knowledge about metabolites and other non-invasive markers that could be used to predict NAFLD. This was achieved using omics technologies and more specifically non-targeted metabolomics.
Materials and methods
Study participants
The current research includes the assessment of baseline measurements of 98 participants with NAFLD, recruited for the FLiO (Fatty Liver in Obesity) study (NCT03183193), a randomized controlled trial that included adults between the ages of 40 and 80 years old, who were overweight or obese (BMI between 27.5 and 40 Kg/m2) and presented NAFLD diagnosed by ultrasonography. The control group consists of 45 individuals who were recruited as a part of the EHGNA study (a continuation of FLiO), presented similar age range and sex distribution as the NAFLD subjects but, contrarily to the NAFLD group, presented normal weight (BMI < 25 Kg/m2) and did not have fatty liver. Exclusion criteria included elevated alcohol consumption (> 21 units of alcohol per week for men and > 14 units for women), presence of known liver disease, endocrine disorders (hyperthyroidism or uncontrolled hypothyroidism), weight loss > 3 Kg in the past 3 months, the use of weight modifiers, severe psychiatric disorders, active autoimmune diseases, acute infections, pharmacological treatment with drugs that could cause hepatic steatosis or alteration in hepatic tests (immunosuppressants, cytotoxic agents, corticosteroids), the inability to follow the diet (food allergies/intolerances) and difficulty in following the scheduled visits. The study protocol was approved by the Research Ethics Committee of the University of Navarra (ref. 54/2015). All the procedures were done in accordance with the declaration of Helsinki. All the participants gave written informed consent prior to their inclusion in the study.
Anthropometric, body composition, and biochemical evaluation
Anthropometric measurements, body composition, and blood pressure were determined under fasting conditions in the Metabolic Unit of the University of Navarra, as previously described [11]. Body mass index (BMI) was calculated as the body weight of the subject measured in Kilograms divided by the squared height measured in meters (Kg/m2). Body composition, including visceral adipose tissue (VAT), was determined by dual-energy X-ray absorptiometry (DXA) following the instructions of the manufacturer (Lunar iDXA, enCORE 14.5, Madison, WI).
Blood samples were collected under 8–10 h fasting conditions. The samples were processed to obtain biochemical determinations in the biochemistry laboratory of the University of Navarra Clinic (CUN). Blood triglycerides (TG), total cholesterol, high-density lipoprotein cholesterol (HDL-c), glucose, and insulin were quantified on an autoanalyzer with specific commercial kits and following the instructions of the company (Cobas 8000, Roche Diagnostics, Switzerland). Low-density lipoprotein cholesterol (LDL-c) was calculated using the Friedewald formula [17].
The Homeostatic model assessment of insulin resistance (HOMA-IR) was calculated as \(\frac{\textrm{fasting}\ \textrm{insulin}\ \left(\frac{\upmu \textrm{U}}{\textrm{mL}}\right)\times \textrm{fasting}\ \textrm{glucose}\ \left(\textrm{mmol}/\textrm{L}\right)\ }{22.5}\) [58]. The Castelli’s risk index (CRI) was calculated as \(\frac{TC}{HDL-c}\), while the atherogenic index of plasma (AIP) was calculated as \(\log \frac{TG}{HDL-c}\) , as previously described [16, 39]
Retinol binding protein (RBP4), leptin, and adiponectin were analyzed and quantified using specific ELISA kits (Demeditec; Kiel-Wellsee, Germany) in a Triturus autoanalyzer (Grifols, Barcelona, Spain) at the biochemistry laboratory of the Center for the Nutrition Research at the University of Navarra (CIN, Pamplona, Spain). Leukocyte cell-derived chemotaxin-2 (LECT2) was analyzed and quantified using the same Triturus autoanalyzer with specific kits for this chemotaxin (Biovendor LLC, NC, USA).
Assessment of liver status
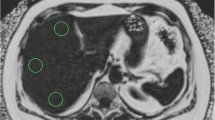
The entire hepatic assessment was performed by qualified professionals of the CUN under fasting conditions. The diagnosis of NAFLD was determined by ultrasonography (Siemens ACUSON S2000 and S3000), as described elsewhere [44]. The participants were classified into two groups: 0 (controls) and ≥ 1 (NAFLD). MRI (Siemens Aera 1.5T) determined liver fat content by the Dixon technique [6]. Aspartate aminotransferase (AST), alanine aminotransferase (ALT), and gamma-glutamyl transferase (GGT) were quantified on an autoanalyzer with specific commercial kits and following the instructions of the company (Cobas 8000, Roche Diagnostics, Switzerland). M30 and M65, which are considered hepatic fibrosis markers [36], were quantified with an enzyme-linked immunosorbent assay (ELISA) method using commercial kits (PEVIVA, Bromma, Sweden) according to the manufacturer’s instructions. The fatty liver index (FLI) was computed using a previously described formula [3], that considers serum triglycerides, BMI, waist circumference, and GGT concentrations to determine the probability of suffering NAFLD.
Metabolomics
Non-targeted serum metabolomics were carried out in the Metabolomics Unit of the University of Navarra. Sample pre-processing consisted in defrosting and homogenizing the samples that were stored at −80 °C. A total of 150 μL aliquots of serum were prepared, and 450 μL of methanol (MeOH, grade LC–MS, Scharlab, Sentemant, Spain) was added to each aliquot. Then, samples were vigorously vortexed for 2 min (VX-2500 multi-tube vortexer, VWR, PA, USA) and centrifuged for 10 min at 10000 rmp (Biofuge A, Heraeus Sepatech, Germany). The supernatant was collected, evaporated under nitrogen flux (Turvovap® LV, Caliper LifeSciences, Waltham, MA, USA), and recovered in 150 μL of H2O: MeOH (5:95 V:V). Then, the samples were analyzed under High performance liquid chromatography (HLPC; Agilent Technologies 1200) equipped with a Time of flight (TOF) mass detector (Agilent Mass Accuracy 6220) (LC–MS), operated in positive electrospray ionization mode (ESI+) and negative mode (ESI−). The stationary phase used was a Zorbax SB-C18 column (Agilent Technologies), and the mobile phase consisted of 0.1% formic acid in water (A) and 0.1% formic acid in MeOH (B). The gradient elution was 0% B, 0–5min; 0–100% B, 5–20 min; 100% B, 20–25 min; 100–0% B, 25–30 min. After the analyses, the column was re-equilibrated for 2 min at = % B. The injection volume was 20 μL and the flow rate was 0.5 mL min−1. Chromatography was performed at 40 °C. The ESI conditions were as follows: gas temperature, 350 °C; drying gas, 10 L min−1; nebulizer, 45 psig; capillary voltage, 3500 V; fragmentor, 17 V; and skimmer, 65 V. The instrument was set out to acquire over the m/z range 100–2000 with an acquisition rate of 1.03 spectra per s. To evaluate the quality in this analysis, three types of quality control samples (QCs) were used: (i) column test, (ii) pool plasma prepared by mixing equal volumes from each of the samples, (iii) pool spiked plasma prepared by mixing pool plasma with L-alanine, glycine, L-phenylalanine, citric acid, L-glutamic acid, caffeine, and leucine (Sigma-Aldrich, MA, USA). The analytical procedure has been previously described [2, 10].
Chromatograms were processed with MassHunter Qualitative Analysis B.06.00 software (Agilent Technologies, CA, USA) to ensure quality. Metabolite alignment was obtained with the XCMS Online software (The Scripps Research Institute, La Jolla, CA 92037, USA) attending to the mass-to-charge ratio and the retention time. The alignment used a 0.2 min-retention time and a 5 mDalton mass tolerance window. The peak intensity of the metabolites was controlled by a logarithmic transformation and monitored by Pareto scaling. Partial least squares discriminant analyses (PLSDA), Random forest, Volcano plots, and other multivariate tools were conducted in the MetaboAnalyst Software version 5.0 (Xia Lab of McGill University, Quebec, Canada) to obtain key metabolites differentiating the control and NAFLD groups. PLSDA determined the Variable of value of variable importance in projection (VIP). Metabolites with a VIP score value greater than 1.0 were chosen for proof of identity. Finally, the metabolite identification was carried out using the Metlin database (The Scripps Research Institute). The adducts used for the search criteria in the positive polarity were [M+H]+, [M+Na]+, and [M+H-H2O]+, while for the negative polarity were [M-H]− and [M-H-H2O]−, both considering a 5 mDalton mass tolerance window. Metabolites were expressed and analyzed according to their intensity measured in arbitrary units (AU), which carries a direct relation with its concentration. Identification of ISO (Sigma-Aldrich, MA, USA) was confirmed by analyzing commercial standards in identical conditions of samples.
Lifestyle assessment (dietary intake and physical activity)
Information about dietary intake and physical activity was extracted from validated questionnaires. Diet was assessed with a semiquantitative food frequency questionnaire (FFQ) of 137 items, previously validated in Spain for energy and nutrient intake [15]. The nutrient composition of the food items was derived from accepted Spanish food composition tables [18, 61]. Mediterranean diet adherence was evaluated using a 17-point screening questionnaire, whose final score ranged between 0 and 17, with a higher punctuation indicating better adherence [19, 46].
Statistical analyses
All statistical analyses were performed using Stata software version 12.0 (StataCorp, College Station, TX, USA). The normal distribution of each variable was evaluated using the Shapiro–Wilk tests. Parametrical tests were used for variables with a normal distribution, while non-parametrical tests were used for those which not. T-tests and Wilcoxon tests were used for numerical variables, and chi-squared tests were used for categorical variables to compare baseline characteristics of controls and subjects with NAFLD. Participants were then classified according to ISO intensity tertiles (T1: 8247.65-63573.35; T2: 63658.64-120638.35; and T3: 121582.47-1544021.9). Body composition, hepatic status, and insulin resistance markers among the tertiles were evaluated by Kruskal–Wallis tests for numerical variables and chi-squared tests for categorical variables. Spearman correlations were performed to evaluate the association between hepatic status, metabolites, insulin resistance, and cardiovascular risk markers. Bootstrap stepwise multivariable regressions were performed to select the metabolites that were further associated with the disease. Univariate and multivariate logistic regressions were performed with the presence of NAFLD as the dependent variable. Receiver operating characteristic curve analyses (ROC) and the areas under the ROC curve (AUROC) were calculated to evaluate the power of prediction and the diagnostic performance of several variables for liver fat. Validation of these results was performed by calculating the optimism-corrected value using Tibshirani’s enhanced bootstrap method described by Harrell [23]. All p-values presented are two-tailed. Statistical significance was considered at p < 0.05. Relative risk (RR) was calculated from OR using a previously described formula [47]
Results
General baseline characteristics
Body composition, hepatic status, insulin resistance, cardiovascular risk, and inflammatory markers of the study participants are presented in Table 1 (NAFLD group, n = 98; control group, n = 45). In the NAFLD group, 43 subjects were women and 55 were men. In the control group, 29 subjects were women and 16 were men (p = 0.022). The mean age of the control group was 50.34 (SD = 9.24) years, while in the NAFLD group was 48.77 (SD = 5.50); no significant differences were found regarding the age of the participants (p = 0.302).
Body composition measurements significantly differed between the groups, clearly suggesting that the NAFLD subjects present worst metabolic health and hepatic status. Glucose, insulin, HOMA-IR, triglycerides, LECT2, RBP4, and leptin were significantly increased in individuals with NAFLD. As expected, adiponectin was increased in controls. Total cholesterol and LDL cholesterol levels were significantly higher in the control group compared to the NALFD group (p < 0.001 and p = 0.004, respectively). However, both calculated atherogenic indexes, CRI and AIP, were significantly higher in the NAFLD group (p = 0.013 and p < 0.001). Moreover, several of these markers significantly correlated with hepatic fat percentage. Concretely, LECT2, RBP4, M30, and M65 were positively correlated with hepatic fat, while adiponectin was negatively correlated with hepatic fat (p < 0.001).
Metabolomics
HPLC-TOF-MS method allowed the detection of 6599 features in the ESI+ mode and 1036 features in the ESI- mode (data not shown). The discriminant analysis determined a total of 57 discriminant metabolites between the NAFLD and control groups (Fig. 1), 48 with positive polarity and 9 with negative polarity (Supplementary table 1). After their identification using the Metlin database, the metabolites were subjected to bootstrap stepwise regressions to select those with the most predictive capacity for NAFLD. A total of four metabolites were selected: vignatic acid A, perseitol, 4-(2-Nitroethyl) phenyl primeveroside, and ISO. After adjusting for other important variables and possible confounders, ISO was selected as the primary determinant metabolite, because of its predictive ability towards NAFLD.
Metabolomic fingerprint of controls and NAFLD subjects. A. Principal component analysis (PCA) in positive polarity of controls and NAFLD subjects. B. Volcano plot in positive polarity of controls and NAFLD subjects. C. Principal component analysis (PCA) in negative polarity of controls and NAFLD subjects. D. Volcano plot in negative polarity of controls and NAFLD subjects
ISO negatively correlated with key anthropometric measurements as well, such as waist circumference (p < 0.001), BMI (p < 0.001), VAT (p < 0.001), and body fat (p < 0.001). Moreover, ISO was significantly correlated with biochemical parameters involved in NAFLD. Concretely, the metabolite was positively correlated with HDL cholesterol (p = 0.015), while it was negatively correlated with triglycerides (p = 0.026), insulin (p < 0.001), and HOMA-IR (p < 0.001).
ISO was significantly correlated with cardiovascular risk and adiposity markers as well. Specifically, the metabolite was positively correlated with adiponectin (p < 0.001); while it was negatively correlated with LECT2 (p = 0.002), RBP4 (p = 0.011), leptin (p = 0.002), and fibrosis markers M30 and M65 (p = 0.005 and p = 0.044, respectively).
The study population was divided into tertiles according to their ISO intensity, which is a direct representation of their concentration. The first tertile consists of those individuals with the lowest levels of the metabolite, while the third tertile encompasses the individuals with the highest levels of ISO (T1: 8247.65-63573.35; T2: 63658.64-120638.35; and T3: 121582.47-1544021.9). The sex distribution in the tertiles (male/female) were 27/21, 20/28, and 24/23, respectively, with no significant differences between them (p = 0.350).
Body composition, hepatic status, insulin resistance, and cardiovascular risk markers were evaluated and compared among the tertiles as well (Table 2). BMI, waist circumference, VAT, body fat percentage, insulin, HOMA-IR, LECT2, RBP4, and leptin were significantly decreased in the third tertile of the studied group. Similarly, ALT, steatosis degree, hepatic fat, FLI index, M30, and M65 markers were reduced as well in individuals with higher ISO intensity. Contrarily, adiponectin was increased in the third tertile. Curiously, total cholesterol and LDL cholesterol were increased in the third tertile of the population as well; nevertheless, the AIP atherogenic index was significantly decreased in this tertile.
Logistic regressions
To further evaluate the predictive capacity and possible functionality of ISO as a predictor for NAFLD, logistic regressions with their respective odds ratios (OR) and ROC curves analyses were calculated. A univariate analysis between the presence of NAFLD and ISO tertiles demonstrated that the metabolite was significantly able to predict the disease (T2: OR = 0.60, 95% confidence interval = 0.22–1.63, p = 0.317; T3: OR = 0.17, 95% confidence interval = 0.06–0.45, p < 0.001) with a moderate capacity (AUROC 0.687, Table 3). Other contributing factors were evaluated and chosen based on bootstrap stepwise regressions as well, of which the ones with the most predictive capacity for the presence of NAFLD were VAT, adiponectin, plasmatic glucose, and M30. These results presented high statistical significance as well (p < 0.001).
After selecting these contributing variables, multivariable logistic regressions and ROC curve analyses were performed to evaluate ISO alongside a panel of other variables (Table 3). The regressions were then adjusted with sex, age, and physical activity. Age and physical activity did not seem to explain or predict NAFLD in any of the models. Sex did seem to have a significant effect, but only on the prediction of NAFLD in the VAT and ISO model. Model 1 combined ISO with VAT. Model 2 combined ISO with adiponectin. Model 3 combined ISO with plasmatic glucose, and Model 4 combined ISO with M30. ISO continued to have a significant predictive value even in combination with these potent contributing variables. The AUROC results were validated using the optimism-corrected value previously mentioned and are shown in Table 3 (Fig. 2). Additionally, RR was estimated from the OR obtained in each of the regression models. The RR from the univariate adjusted model was 0.22, which implies that the individuals with higher levels of the metabolite have 77% less risk of presenting NAFLD compared to those with lower levels. Similarly, for models 1, 2, 3, and 4, the calculated RR were 0.28, 0.17, 0.25, and 0.28, respectively, which denotes a risk reduction for NAFLD varying from 71 to 82% in individuals with higher levels of ISO compared to subjects with low levels.
Discussion
NAFLD is a metabolic pathology characterized by the accumulation of fat in the liver parenchyma with an alarmingly growing prevalence [78]. One of the main problems this disease presents is the increased risk of developing potentially deadly complications [35]. Liver biopsy, its diagnostic gold standard, is expensive and invasive, and therefore not suitable for routinary checkups [8]. In this regard, this study yearned to find functional markers that could work as diagnostic tools for NAFLD by using omics technologies. Among the main findings, ISO appeared as a metabolite with such marker characteristics.
To reach this objective, 143 human subjects, either controls or obese subjects with confirmed NAFLD, were enrolled. Metabolic and hepatic status was evaluated and as expected, almost all markers differed between the two groups. Concretely, the hepatic status was significantly worse in the NAFLD group compared to the controls, but these were expected results, since the NAFLD subjects presented hepatic steatosis, while the controls were specifically selected because of their lack of hepatic steatosis. Both diagnoses were confirmed by ultrasonography.
The NAFLD group had overall worst metabolic health compared to controls as well. Surprisingly, the control group showed higher LDL-c and total cholesterol levels despite showing overall better lifestyle and dietary habits; however, similar results were found in previously published literature [43]. Moreover, while the total cholesterol and LDL-c are higher in the control subjects, the LDL-c levels do not reach pathological levels according to both European and American guidelines [22, 42]. Furthermore, HDL-c levels are also higher in control individuals, which could be the reason why total cholesterol is also increased in this group. Low HDL-c levels are highly involved in the development of cardiometabolic diseases and have recently been associated with the development of NAFLD [12, 33, 65]. It is also important to highlight that triglycerides were increased in the NAFLD group. Plasmatic triglycerides are highly involved in the pathophysiology of NAFLD, being responsible for the fatty acid deposition in the hepatocytes which is one of the main causes of the development of the disease [57, 80]. Additionally, both calculated atherogenic indexes were significantly higher in the NAFLD group; suggesting that this group presented not only higher cardiovascular risk compared to the controls but also worst lipidic profiles [16, 39].
HOMA-IR, insulin, and glucose were significantly higher in NAFLD subjects, highlighting the link between the disease and IR, as previously described [70]. Additionally, LECT2 and RBP4 were also increased in these subjects. Similar results to these have been found, which is conceivable since both markers are involved in glucose metabolism, IR, obesity, and metabolic syndrome [31, 32, 54]. LECT2 is a hepatokine that induces the activation of inflammatory cytokines and prevents insulin signaling. Other studies have found that LECT2 is increased in individuals with NAFLD as well and could be considered as a fibrosis marker [24, 32]. RBP4 is associated to cardiovascular risk, inflammation, and insulin resistance, all of which are involved in NAFLD. Other studies have found similar results and suggest that RBP4 could be considered as a biomarker for obesity, metabolic syndrome, and type 2 diabetes [31, 54].
Similarly, leptin levels were also significantly higher in the NAFLD subjects, which has also been found in previous studies. Although leptin produces a satiety signal, it is known that obese individuals have higher concentrations of plasmatic leptin and may have a leptin resistance [26, 55]. In NAFLD concretely, higher leptin levels are associated with greater triglyceride content in the hepatocytes, inflammation, and insulin resistance [5, 45]. Contrarily, adiponectin’s concentration was higher in controls than NAFLD subjects, which was a probable result as well. Adiponectin has been found to be decreased in NAFLD in previous studies too, which has a plausible explanation, since this adipokine is involved in energy metabolism through the reduction of plasmatic triglycerides, increased β-oxidation, and amelioration of glucose metabolism [5, 45].
Dietary characteristics were also quite different among the NAFLD and control groups. Concretely, the NAFLD subjects significantly consumed more calories, carbohydrates, and sodium per day. The glycemic index of the diet was also increased in the NAFLD group compared to the controls. This is relevant since all these variables are associated with the development of insulin resistance and obesity [49, 50, 66]. It is also important to highlight that excessive sodium consumption also leads to other cardiovascular comorbidities, such as high blood pressure, and appears to be a risk factor for mortality, inflammation, and fibrosis in NAFLD patients [20, 56, 80].
Conversely, controls appeared to have higher protein and fat consumption. Slight hyper-proteic diets seem to have a protective effect against the development of obesity, mainly because of its satiating effects and its prevention of muscle loss [51, 71]. On the other hand, higher fat consumption is positively associated with increased body weight and cardiovascular disease [49, 50, 66]. However, the total fat intake in controls is significantly increased in monounsaturated fatty acids (MUFAs) and polyunsaturated fatty acids as well (PUFAs), which are mainly considered beneficial for overall cardiovascular health [14, 67]. Since metabolites are usually a product of diet-derived compounds, the fact that controls possess these significant differences in dietary characteristics compared to NAFLD gives an insight of how and why the serum metabolites differ among the two groups as well [9, 41, 53].
As described in the results, among the discriminant metabolites found between the NAFLD and control groups, four of them were found to be considerably better at predicting the disease through bootstrap stepwise regressions. However, after adjusting for other contributing factors, such as body composition, biochemical, and inflammatory parameters, ISO was considered the main predictive metabolite.
ISO is a bioactive compound found in foods from the Leguminosae/Fabaceae family. It has a polyphenolic structure and is classified as a flavonoid, and more specifically, a chalcone compound [60, 81]. Previous preclinical studies, performed mainly in cellular and animal models, have described its anti-inflammatory, antioxidative, cardiovascular, and liver-protective properties when orally administered [60, 81]. Taking into consideration these previous studies, this metabolite continued to be explored and further analyzed in this sample, since delving into the role of ISO as a biomarker for NAFLD could be of interest given the attributed properties mentioned above.
Furthermore, ISO, the main studied metabolite, correlated negatively not only with hepatic fat but also with key body composition measurements and biochemical parameters involved in NAFLD, specifically those associated with insulin resistance, such as insulin and HOMA-IR.
The observed differences in metabolic health between tertiles could be attributed to lifestyle differences. In fact, although it is not exactly clear why ISO appears to be increased in controls; when examining the lifestyle habits of this group compared to the NAFLD subjects, they do have significantly better dietary habits and increased adherence to the Mediterranean diet, which is characterized by a high consumption of vegetable-based foods, which are rich in these types of bioactive compounds, such as ISO.
Among the food items that contain isoliquiritigenin are garbanzo beans (otherwise known as chickpeas), soybeans, peanuts, and other legumes [52, 60, 81]. It is also found in licorice roots, which are used to make extracts in Chinese medicine [38, 82]. It is worth mentioning that the concentration of ISO may vary among species, and most importantly, there is a need for more research regarding the presence, concentration, and bioavailability of this compound in different food items. In this sense, ISO could also be considered as a biomarker, not only for the following of dietary strategies like the Mediterranean diet but also for the consumption of other produce/vegetables. Additionally, its inclusion could be used for patient feedback to reinforce or encourage healthy dietary behaviors.
Moreover, when divided into tertiles according to ISO intensity, individuals with higher levels presented significantly better body composition and biochemical profiles compared to those with lower levels. These results suggest that this metabolite might act as a protective factor for NAFLD and is overall associated with positive metabolic outcomes. Similar results have been found in previous studies as well [77].
Additionally, the tertile-divided population provided similar information regarding the lifestyle differences of the subjects, since the subjects with higher levels of the metabolite also show significantly better adherence to the Mediterranean diet as well. These results may suggest that a strategy for reaching higher levels of ISO could be sustained by implementing healthy dietary habits. These results are in accordance with previous studies as well, since ISO can be found in foods from the Leguminosae/Fabaceae family, and it seems that it is a diet-derived metabolite that could be considered as a marker for the intake of certain foods [60].
Finally, ISO’s predictive ability was proved with logistic regressions, where the metabolite was significantly evidenced as a predictive protector for NAFLD, even when adjusted and controlled by very potent variables involved in NAFLD as well, such as VAT, adiponectin, plasmatic glucose, and M30. When estimating RR from the OR obtained for easier comprehension [47], individuals with lower levels of the metabolite appeared to have from 71 to 82% of presenting NAFLD compared to those with higher levels.
As mentioned above, ISO is a previously described metabolite that has been studied in cancer, neurological, and liver diseases, including NAFLD, as an administered adjuvant treatment, but not as a biomarker [37, 75, 81]. This molecule is classified as a chalcone, and it is the precursor of several other flavonoids. Chalcones are polyphenols and ISO particularly has two phenyl groups in its structure [83]. Polyphenols are well-known antioxidant agents, capable of scavenging free radicals. Since one of the main mechanisms implied in the pathogenesis of NAFLD is oxidative stress and ISO is a compound with antioxidant properties, the association found in this study has a plausible explanation and has been previously described [40, 69].
Another mechanism in which ISO may exert its antioxidant capacity is by potentiating the nuclear factor, erythroid 2-like 2a (Nrf2) mitochondrial pathway. Nrf2 is a transcription factor critically implicated in the regulation of oxidative stress, inflammation, and autophagy. When attached to the nucleus DNA, Nrf2 seems to enhance the expression of antioxidative genes and their proteins, increasing the production of heme-oxygenase and superoxide dismutase [68, 69].
Recent studies have linked ISO as a protective factor against hepatic steatosis and NAFLD for its ability to increase β-oxidation and inhibit lipogenesis in the liver [72, 81], alleviate insulin resistance, and suppress inflammation [25], mostly through activating protein kinase (AMPK) and peroxisome proliferator-activated receptor alpha (PPAR-α) [75, 77]. PPAR-α is a transcription factor, considered as a major regulator of lipid metabolism in the liver and has a key role in metabolic diseases because of its triglyceride-lowering and insulin-sensitizing properties [4, 73]. AMPK is an enzymatic complex with numerous functions that mainly focus on the regulation of energy metabolism and energy expenditure; it has been proposed as a main mechanism in the pathogenesis of metabolic diseases, such as type 2 diabetes and NAFLD [1, 21].
It is worth noticing that most of the evidence on the effects of ISO are based on studies performed on cellular or animal models. More research, specifically from clinical trials in humans, is needed to further elucidate the role of ISO and its potential role as a biomarker or predictive tool in NAFLD.
It is important to consider that this study has some limitations, such as the lack of mechanistic information about the effect and metabolism of ISO in human physiology. The studies evaluating the role of ISO in humans are scarce, so more information is needed to establish a clear conclusion of the protective role found in this sample.
Nevertheless, this study presents many strengths as well, such as the metabolomic characterization of a sample of human subjects that was extensively characterized with information concerning body composition (measured by DXA), biochemical parameters, lifestyle and dietary habits, and different measures of hepatic variables. Noticeably, all these data were obtained for the controls as well, and in fact, controls were specifically selected because of their confirmed lack of hepatic steatosis. Additionally, the results were verified using a commercial standard of ISO and analyzed using the same conditions as the serum samples.
Furthermore, this study particularly evaluated obese subjects with NAFLD and lean controls, since NAFLD is intrinsically related with obesity and metabolic syndrome, and regressions were adjusted for weight-related confounding variables. However, it could be interesting to evaluate obese subjects without NAFLD as the control group as well and examine ISO in this type of sample. Lastly, it is worth mentioning that this study evaluated the baseline measurements of a particular population sample, but it could be interesting to study the longitudinal changes and behavior of ISO. Since the FLiO study also includes a 24-month dietary intervention of the NAFLD, evaluating the behavior of this metabolite (and possibly others) throughout time via targeted metabolomics could be of interest to continue to elucidate its role on NAFLD.
Conclusion
This study concludes that metabolites, such as ISO, in combination with visceral adipose tissue, insulin resistance, and other related markers, constitute a potential non-invasive tool to predict and diagnose NAFLD. Individuals with lower levels of ISO have from 71 to 82% more risk of presenting NAFLD compared to individuals with higher levels; therefore, ISO could be considered as a protective predictive factor for NAFLD.
References
Abdolahi A, Vahabzadeh Z, Izadpanah E, Moloudi MR (2022) Vaspin attenuates steatosis-induced fibrosis via GRP78 receptor by targeting AMPK signaling pathway. J Physiol Biochem 78:185–197. https://doi.org/10.1007/S13105-021-00852-7
Aranaz P, Romo-Hualde A, Zabala M, Navarro-Herrera D, Ruiz De Galarreta M, Gil AG, Martinez JA, Milagro FI, González-Navarro CJ (2017) Freeze-dried strawberry and blueberry attenuates diet-induced obesity and insulin resistance in rats by inhibiting adipogenesis and lipogenesis. Food Funct 8:3999–4013. https://doi.org/10.1039/C7FO00996H
Bedogni G, Bellentani S, Miglioli L, Masutti F, Passalacqua M, Castiglione A, Tiribelli C (2006) The fatty liver index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol 6:1–7. https://doi.org/10.1186/1471-230X-6-33
Botta M, Audano M, Sahebkar A, Sirtori CR, Mitro N, Ruscica M (2018) PPAR agonists and metabolic syndrome: an established role? Int J Mol Sci 19. https://doi.org/10.3390/IJMS19041197
Boutari C, Mantzoros CS (2020) Adiponectin and leptin in the diagnosis and therapy of NAFLD. Metabolism 103. https://doi.org/10.1016/J.METABOL.2019.154028
Cantero I, Elorz M, Abete I, Marin BA, Herrero JI, Monreal JI, Benito A, Quiroga J, Martínez A, Huarte MP, Uriz-Otano JI, Tur JA, Kearney J, Alfredo Martinez J, Angeles Zulet M (2019) Ultrasound/elastography techniques, lipidomic and blood markers compared to magnetic resonance imaging in non-alcoholic fatty liver disease adults. Int J Med Sci 16:75–83. https://doi.org/10.7150/ijms.28044
Castera L, Friedrich-Rust M, Loomba R (2019) Noninvasive assessment of liver disease in patients with nonalcoholic fatty liver disease HHS public access. Gastroenterology 156:1264–1281. https://doi.org/10.1053/j.gastro.2018.12.036
Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, Harrison SA, Brunt EM, Sanyal AJ (2018) The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67:328–357. https://doi.org/10.1002/hep.29367
Chen L, Zhernakova DV, Kurilshikov A, Andreu-Sánchez S, Wang D, Augustijn HE, Vich Vila A, Weersma RK, Medema MH, Netea MG, Kuipers F, Wijmenga C, Zhernakova A, Fu J (2022) Influence of the microbiome, diet and genetics on inter-individual variation in the human plasma metabolome. Nat Med 28:2333–2343. https://doi.org/10.1038/S41591-022-02014-8
Cuevas-Sierra A, Romo-Hualde A, Aranaz P, Goni L, Cuervo M, Martínez JA, Milagro FI, Riezu-Boj JI (2021) Diet- and sex-related changes of gut microbiota composition and functional profiles after 4 months of weight loss intervention. Eur J Nutr 60:3279–3301. https://doi.org/10.1007/s00394-021-02508-0
De La Iglesia R, Lopez-Legarrea P, Abete I, Bondia-Pons I, Navas-Carretero S et al (2014) A new dietary strategy for long-term treatment of the metabolic syndrome is compared with the American heart association (AHA) guidelines: the MEtabolic Syndrome REduction in NAvarra (RESMENA) project. Bri J Nutrition 111:643–652. https://doi.org/10.1017/S0007114513002778
Deprince A, Haas JT, Staels B (2020) Dysregulated lipid metabolism links NAFLD to cardiovascular disease. Mol Metab 42. https://doi.org/10.1016/J.MOLMET.2020.101092
Fang YL, Chen H, Wang CL, Liang L (2018) Pathogenesis of non-alcoholic fatty liver disease in children and adolescence: from “two hit theory” to “multiple hit model”. World J Gastroenterol 24:2974–2983. https://doi.org/10.3748/WJG.V24.I27.2974
Fattore E, Massa E (2018) Dietary fats and cardiovascular health: a summary of the scientific evidence and current debate. Int J Food Sci Nutr 69:916–927. https://doi.org/10.1080/09637486.2018.1455813
Fernández-Ballart JD, Piñol JL, Zazpe I, Corella D, Carrasco P, Toledo E, Perez-Bauer M, Martínez-González MÁ, Salas-Salvadó J, Martn-Moreno JM (2010) Relative validity of a semi-quantitative food-frequency questionnaire in an elderly Mediterranean population of Spain. Br J Nutr 103:1808–1816. https://doi.org/10.1017/S0007114509993837
Fernández-Macías JC, Ochoa-Martínez AC, Varela-Silva JA, Pérez-Maldonado IN (2019) Atherogenic index of plasma: novel predictive biomarker for cardiovascular illnesses. Arch Med Res 50:285–294. https://doi.org/10.1016/J.ARCMED.2019.08.009
Friedewald W, Levy R, Fredrickson D (1972) Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 18:499–502
Galarregui C, Cantero I, Marin-Alejandre BA, Monreal JI, Elorz M, Benito-Boillos A, Herrero JI, de la OV R-CM, HHM H, Bressan J, Tur JA, Martínez JA, Zulet MA, Abete I (2021) Dietary intake of specific amino acids and liver status in subjects with nonalcoholic fatty liver disease: Fatty Liver in Obesity (FLiO) study. Eur J Nutr 60:1769–1780. https://doi.org/10.1007/s00394-020-02370-6
Galmes-Panades AM, Konieczna J, Abete I, Colom A, Rosique-Esteban N, Zulet MA, Vázquez Z, Estruch R, Vidal J, Toledo E, Babio N, Fiol M, Casas R, Vera J, Buil-Cosiales P, De Paz JA, Goday A, Salas-Salvadó J, Alfredo Martínez J, Romaguera D (2019) Lifestyle factors and visceral adipose tissue: results from the PREDIMED-PLUS study. PLoS One 14:1–15. https://doi.org/10.1371/journal.pone.0210726
Gao P, You M, Li L, Zhang Q, Fang X, Wei X, Zhou Q, Zhang H, Wang M, Lu Z, Wang L, Sun F, Liu D, Zheng H, Yan Z, Yang G, Zhu Z (2022) Salt-induced hepatic inflammatory memory contributes to cardiovascular damage through epigenetic modulation of SIRT3. Circulation 145:375–391. https://doi.org/10.1161/CIRCULATIONAHA.121.055600
Garcia D, Hellberg K, Chaix A, Wallace M, Herzig S, Badur MG, Lin T, Shokhirev MN, Pinto AFM, Ross DS, Saghatelian A, Panda S, Dow LE, Metallo CM, Shaw RJ (2019) Genetic liver-specific AMPK activation protects against diet-induced obesity and NAFLD. Cell Rep 26:192–208.e6. https://doi.org/10.1016/J.CELREP.2018.12.036
Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK et al (2019) 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 139:E1082–E1143. https://doi.org/10.1161/CIR.0000000000000625
Harrell F (2015) Applications to linear models, logistic and ordinal regression, and survival analysis. In: Regression Modeling Strategies. Springer, New York, NY, USA
Hwang HJ, Jung TW, Kim BH, Hong HC, Seo JA, Kim SG, Kim NH, Choi KM, Choi DS, Baik SH, Yoo HJ (2015) A dipeptidyl peptidase-IV inhibitor improves hepatic steatosis and insulin resistance by AMPK-dependent and JNK-dependent inhibition of LECT2 expression. Biochem Pharmacol 98:157–166. https://doi.org/10.1016/J.BCP.2015.08.098
Ishibashi R, Furusawa Y, Honda H, Watanabe Y, Fujisaka S et al (2022) Isoliquiritigenin attenuates adipose tissue inflammation and metabolic syndrome by modifying gut bacteria composition in mice. Mol Nutr Food Res 66. https://doi.org/10.1002/MNFR.202101119
Izquierdo AG, Crujeiras AB, Casanueva FF, Carreira MC (2019) Leptin, obesity, and leptin resistance: where are we 25 years later? Nutrients 11:2704. https://doi.org/10.3390/nu11112704
Jacob M, Lopata AL, Dasouki M, Abdel Rahman AM (2019) Metabolomics toward personalized medicine. Mass Spectrom Rev 38:221–238. https://doi.org/10.1002/MAS.21548
Jin Q, Ma RCW (2021) Metabolomics in diabetes and diabetic complications: insights from epidemiological studies. Cells 10. https://doi.org/10.3390/CELLS10112832
Johnson CH, Ivanisevic J, Siuzdak G (2016) Metabolomics: beyond biomarkers and towards mechanisms. Nat Rev Mol Cell Biol 17:451–459. https://doi.org/10.1038/NRM.2016.25
Juo Y-Y, Livingston EH (2019) Testing for nonalcoholic fatty liver disease. JAMA 322:1836. https://doi.org/10.1001/jama.2019.10696
Karamfilova V, Gateva A, Alexiev A, Zheleva N, Velikova T, Ivanova-Boyanova R, Ivanova R, Cherkezov N, Kamenov Z, Mateva L (2022) The association between retinol-binding protein 4 and prediabetes in obese patients with nonalcoholic fatty liver disease. Arch Physiol Biochem 128:217–222. https://doi.org/10.1080/13813455.2019.1673429
Kim J, Ki Lee S, Kim D, Lee E, Yoon Park C, Choe H, Kang M-J, Jung Kim H, Kim J-H, Pio Hong J, Ji Lee Y, Soon Park H, Heo Y, Jin Jang Y, Yeon Jin Jang C (2022) Adipose tissue LECT2 expression is associated with obesity and insulin resistance in Korean women. Obesity (Silver Spring) 30:1430–1441. https://doi.org/10.1002/oby.23445
Kontush A (2020) HDL and reverse remnant-cholesterol transport (RRT): relevance to cardiovascular disease. Trends Mol Med 26:1086–1100. https://doi.org/10.1016/J.MOLMED.2020.07.005
Kumar S, Duan Q, Wu R, Harris EN, Su Q (2021) Pathophysiological communication between hepatocytes and non-parenchymal cells in liver injury from NAFLD to liver fibrosis. Adv Drug Deliv Rev 176. https://doi.org/10.1016/J.ADDR.2021.113869
Lazarus JV, Mark HE, Anstee QM, Arab JP, Batterham RL et al (2022) Advancing the global public health agenda for NAFLD: a consensus statement. Nat Rev Gastroenterol Hepatol 19:60–78. https://doi.org/10.1038/s41575-021-00523-4
Lee J, Vali Y, Boursier J, Duffin K, Verheij J, Julia Brosnan M, Zwinderman K, Anstee QM, Bossuyt PM, Zafarmand MH (2020) Accuracy of cytokeratin 18 (M30 and M65) in detecting non-alcoholic steatohepatitis and fibrosis: a systematic review and meta-analysis. PLoS One 15. https://doi.org/10.1371/JOURNAL.PONE.0238717
Lee Y, Kwon EY, Choi MS (2018) Dietary isoliquiritigenin at a low dose ameliorates insulin resistance and NAFLD in diet-induced obesity in C57BL/6J mice. Int J Mol Sci 19. https://doi.org/10.3390/IJMS19103281
Li X, Sun R, Liu R (2019) Natural products in licorice for the therapy of liver diseases: progress and future opportunities. Pharmacol Res 144:210–226. https://doi.org/10.1016/J.PHRS.2019.04.025
Liu H, Liu K, Pei L, Li S, Zhao J, Zhang K, Zong C, Zhao L, Fang H, Wu J, Sun S, Song B, Xu Y, Gao Y (2021) Atherogenic index of plasma predicts outcomes in acute ischemic stroke. Front Neurol 12:741754. https://doi.org/10.3389/FNEUR.2021.741754/FULL
Liu X, Zhu Q, Zhang M, Yin T, Xu R, Xiao W, Wu J, Deng B, Gao X, Gong W, Lu G, Ding Y (2018) Isoliquiritigenin ameliorates acute pancreatitis in mice via inhibition of oxidative stress and modulation of the Nrf2/HO-1 pathway. https://doi.org/10.1155/2018/7161592
Luo J, le Cessie S, van Heemst D, Noordam R (2021) Diet-derived circulating antioxidants and risk of coronary heart disease: a Mendelian randomization study. J Am Coll Cardiol 77:45–54. https://doi.org/10.1016/J.JACC.2020.10.048
Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M et al (2020) 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur Heart J 41:111–188. https://doi.org/10.1093/EURHEARTJ/EHZ455
Marin-Alejandre BA, Abete I, Cantero I, Riezu-Boj JI, Milagro FI, Monreal JI, Elorz M, Herrero JI, Benito-Boillos A, Quiroga J, Martinez-Echeverria A, Uriz-Otano JI, Huarte-Muniesa MP, Tur JA, Martínez JA, Zulet MA (2019) Association between sleep disturbances and liver status in obese subjects with nonalcoholic fatty liver disease: a comparison with healthy controls. Nutrients 11. https://doi.org/10.3390/NU11020322
Marin-Alejandre BA, Cantero I, Zulet MA (2021) Effects of two personalized dietary strategies during a 2-year intervention in subjects with nonalcoholic fatty liver disease: a randomized trial. Liver Int 41:1532–1544. https://doi.org/10.1111/liv.14818
Marques V, Afonso MB, Bierig N, Duarte-Ramos F, Santos-Laso Á et al (2021) Adiponectin, leptin, and IGF-1 are useful diagnostic and stratification biomarkers of NAFLD. Front Med (Lausanne) 8. https://doi.org/10.3389/FMED.2021.683250
Martínez-González MA, Buil-Cosiales P, Corella D, Bulló M, Fitó M et al (2019) Cohort profile: design and methods of the PREDIMED-plus randomized trial. Int J Epidemiol 48:387–388o. https://doi.org/10.1093/ije/dyy225
Martínez-González MÁ, Sánchez-Villegas A, Toledo E, Faulín-Fajardo J (2019) Bioestadística Amigable (4a edición), 4a. Elsevier, Pamplona
Masarone M, Troisi J, Aglitti A, Torre P, Colucci A, Dallio M, Federico A, Balsano C, Persico M (2021) Untargeted metabolomics as a diagnostic tool in NAFLD: discrimination of steatosis, steatohepatitis and cirrhosis. Metabolomics 17. https://doi.org/10.1007/S11306-020-01756-1
Mirabelli M, Chiefari E, Arcidiacono B, Corigliano DM, Brunetti FS, Maggisano V, Russo D, Foti DP, Brunetti A (2020) Mediterranean diet nutrients to turn the tide against insulin resistance and related diseases. Nutrients 12. https://doi.org/10.3390/NU12041066
Montemayor S, Mascaró CM, Ugarriza L, Casares M, Llompart I, Abete I, Zulet MÁ, Martínez JA, Tur JA, Bouzas C (2022) Adherence to Mediterranean diet and NAFLD in patients with metabolic syndrome: the FLIPAN study. Nutrients 14. https://doi.org/10.3390/NU14153186
Muntis FR, Smith-Ryan AE, Crandell J, Evenson KR, Maahs DM, Seid M, Shaikh SR, Mayer-Davis EJ (2023) A high protein diet is associated with improved glycemic control following exercise among adolescents with type 1 diabetes. Nutrients 15. https://doi.org/10.3390/NU15081981
Newton A, Majumder K (2023) Germination and simulated gastrointestinal digestion of chickpea ( Cicer arietinum L.) in exhibiting in vitro antioxidant activity in gastrointestinal epithelial cells. Antioxidants (Basel) 12. https://doi.org/10.3390/ANTIOX12051114
Nishida A, Ando Y, Kimura I, Miyamoto J (2022) Involvement of gut microbial metabolites derived from diet on host energy homeostasis. Int J Mol Sci 23. https://doi.org/10.3390/IJMS23105562
Norouzpour M, Marandi SM, Ghanbarzadeh M, Zaremaivan A (2022) The effect of combined exercises on the plasma levels of retinol-binding protein 4 and its relationship with insulin resistance and hepatic fat content in postmenopausal women with nonalcoholic fatty liver disease. J Sports Med Phys Fitness 62:684–690. https://doi.org/10.23736/S0022-4707.21.12233-9
Obradovic M, Sudar-Milovanovic E, Soskic S, Essack M, Arya S, Stewart AJ, Gojobori T, Isenovic ER (2021) Leptin and obesity: role and clinical implication. Front Endocrinol (Lausanne):12. https://doi.org/10.3389/FENDO.2021.585887
Paik JM, Mir S, Alqahtani SA, Younossi Y, Ong JP, Younossi ZM (2022) Dietary risks for liver mortality in NAFLD: global burden of disease data. Hepatol Commun 6:90–100. https://doi.org/10.1002/HEP4.1707
Pereira ENGDS, Paula DP, De ABP, Da FMDJM, Diniz MDFHS, Daliry A, Griep RH (2021) Advanced glycation end product: a potential biomarker for risk stratification of non-alcoholic fatty liver disease in ELSA-Brasil study. World J Gastroenterol 27:4913–4923. https://doi.org/10.3748/WJG.V27.I29.4913
Placzkowska S, Pawlik-Sobecka L, Kokot I, Piwowar A (2019) Indirect insulin resistance detection: current clinical trends and laboratory limitations. Biomed Papers 163:187–199. https://doi.org/10.5507/bp.2019.021
Ramai D, Tai W, Rivera M, Facciorusso A, Tartaglia N, Pacilli M, Ambrosi A, Cotsoglou C, Sacco R (2021) Natural progression of non-alcoholic steatohepatitis to hepatocellular carcinoma. Biomedicines 9:1–17. https://doi.org/10.3390/biomedicines9020184
Ramalingam M, Kim H, Lee Y, Il LY (2018) Phytochemical and pharmacological role of liquiritigenin and isoliquiritigenin from radix glycyrrhizae in human health and disease models. Front Aging Neurosci 10. https://doi.org/10.3389/FNAGI.2018.00348
Recaredo G, Marin-Alejandre BA, Cantero I, Monreal JI, Herrero JI, Benito-Boillos A, Elorz M, Tur JA, Martínez JA, Zulet MA, Abete I (2019) Association between different animal protein sources and liver status in obese subjects with non-alcoholic fatty liver disease: Fatty Liver in Obesity (FLiO) Study. Nutrients 11. https://doi.org/10.3390/nu11102359
Riazi K, Azhari H, Charette JH, Underwood FE, King JA, Afshar EE, Swain MG, Congly SE, Kaplan GG, Shaheen AA (2022) The prevalence and incidence of NAFLD worldwide: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 7:851–861. https://doi.org/10.1016/S2468-1253(22)00165-0
Rinschen MM, Ivanisevic J, Giera M, Siuzdak G (2019) Identification of bioactive metabolites using activity metabolomics. Nat Rev Mol Cell Biol 20:353–367. https://doi.org/10.1038/S41580-019-0108-4
Rives C, Fougerat A, Loiseau N, Guillou H, Gamet-Payrastre L, Wahli W (2020) Oxidative stress in NAFLD: role of nutrients and food contaminants. Biomolecules 10:1–69. https://doi.org/10.3390/BIOM10121702
Rysz J, Gluba-Brzózka A, Rysz-Górzyńska M, Franczyk B (2020) The role and function of HDL in patients with chronic kidney disease and the risk of cardiovascular disease. Int J Mol Sci 21. https://doi.org/10.3390/IJMS21020601
Schutte S, Esser D, Siebelink E, Michielsen CJR, Daanje M et al (2022) Diverging metabolic effects of 2 energy-restricted diets differing in nutrient quality: a 12-week randomized controlled trial in subjects with abdominal obesity. Am J Clin Nutr 116:132–150. https://doi.org/10.1093/AJCN/NQAC025
Sellem L, Eichelmann F, Jackson KG, Wittenbecher C, Schulze MB, Lovegrove JA (2023) Replacement of dietary saturated with unsaturated fatty acids is associated with beneficial effects on lipidome metabolites: a secondary analysis of a randomized trial. Am J Clin Nutr 117. https://doi.org/10.1016/J.AJCNUT.2023.03.024
Shatoor AS, al Humayed S, Almohiy HM (2022) Astaxanthin attenuates hepatic steatosis in high-fat diet-fed rats by suppressing microRNA-21 via transactivation of nuclear factor erythroid 2-related factor 2. J Physiol Biochem 78:151–168. https://doi.org/10.1007/S13105-021-00850-9
Song Z, Zhang Y, Zhang H, Rajendran RS, Wang R, Hsiao C der, Li J, Xia Q, Liu K (2020) Isoliquiritigenin triggers developmental toxicity and oxidative stress–mediated apoptosis in zebrafish embryos/larvae via Nrf2-HO1/JNK-ERK/mitochondrion pathway. Chemosphere 246. doi: https://doi.org/10.1016/J.CHEMOSPHERE.2019.125727
Tanase DM, Gosav EM, Costea CF, Ciocoiu M, Lacatusu CM et al (2020) The intricate relationship between type 2 diabetes mellitus (T2DM), insulin resistance (IR), and nonalcoholic fatty liver disease (NAFLD). J Diabetes Res 2020. https://doi.org/10.1155/2020/3920196
Tettamanzi F, Bagnardi V, Louca P, Nogal A, Monti GS, Mambrini SP, Lucchetti E, Maestrini S, Mazza S, Rodriguez-Mateos A, Scacchi M, Valdes AM, Invitti C, Menni C (2021) A high protein diet is more effective in improving insulin resistance and glycemic variability compared to a Mediterranean diet-a cross-over controlled inpatient dietary study. Nutrients 13. https://doi.org/10.3390/NU13124380
Wang L, Wang X, Kong L, Li Y, Huang K, Wu J, Wang C, Sun H, Sun P, Gu J, Luo H, Liu K, Meng Q (2022) Activation of PGC-1α via isoliquiritigenin-induced downregulation of miR-138-5p alleviates nonalcoholic fatty liver disease. Phytother Res 36:899–913. https://doi.org/10.1002/PTR.7334
Wang Y, Nakajima T, Gonzalez FJ, Tanaka N (2020) PPARs as metabolic regulators in the liver: lessons from liver-specific PPAR-null mice. Int J Mol Sci 21. https://doi.org/10.3390/IJMS21062061
Wishart DS (2019) Metabolomics for investigating physiological and pathophysiological processes. Physiol Rev 99:1819–1875. https://doi.org/10.1152/PHYSREV.00035.2018
Yahya MA, Alshammari GM, Osman MA, Al-Harbi LN, Yagoub AEGA, AlSedairy SA (2022) Liquorice root extract and isoliquiritigenin attenuate high-fat diet-induced hepatic steatosis and damage in rats by regulating AMPK. Arch Physiol Biochem. https://doi.org/10.1080/13813455.2022.2102654
Yang J, Fernández-Galilea M, Martínez-Fernández J, González-Muniesa P, Pérez-Chávez A, Martínez J, Moreno-Aliaga M (2019) Oxidative stress and non-alcoholic fatty liver disease: effects of omega-3 fatty acid supplementation. Nutrients 11. https://doi.org/10.3390/NU11040872
Yang L, Wang D, Zhang Z, Jiang Y, Liu Y (2022) Isoliquiritigenin alleviates diabetic symptoms via activating AMPK and inhibiting mTORC1 signaling in diet-induced diabetic mice. Phytomedicine 98. https://doi.org/10.1016/J.PHYMED.2022.153950
Younossi Z, Anstee QM, Marietti M, Hardy T, Henry L, Eslam M, George J, Bugianesi E (2018) Global burden of NAFLD and NASH: trends, predictions, risk factors and prevention. Nat Rev Gastroenterol Hepatol 15:11–20. https://doi.org/10.1038/nrgastro.2017.109
Younossi Z, Tacke F, Arrese M (2019) Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology 69:2672–2682. https://doi.org/10.1002/hep.30251
Yuan S, Chen J, Li X, Fan R, Arsenault B, Gill D, Giovannucci EL, Zheng J sheng, Larsson SC (2022) Lifestyle and metabolic factors for nonalcoholic fatty liver disease: Mendelian randomization study. Eur J Epidemiol 37:723–733. doi: https://doi.org/10.1007/S10654-022-00868-3
Zhang L, Yang SY, Qi-Li FR, Liu XX, Zhang WT, Peng C, Wu P, Li P, Li P, Xu X (2021) Administration of isoliquiritigenin prevents nonalcoholic fatty liver disease through a novel IQGAP2-CREB-SIRT1 axis. Phytother Res 35:3898–3915. https://doi.org/10.1002/PTR.7101
Zhang Z, Yung KKL, Ko JKS (2022) Therapeutic intervention in cancer by isoliquiritigenin from licorice: a natural antioxidant and redox regulator. Antioxidants (Basel) 11. https://doi.org/10.3390/ANTIOX11071349
(2022) PubChem Compound Summary for CID 638278, Isoliquiritigenin. In: National Center for Biotechnology Information. https://pubchem.ncbi.nlm.nih.gov/compound/Isoliquiritigenin. Accessed 7 Oct 2022
Acknowledgements
The authors would like to thank all the participants of this study as well as to Irene Cantero, Bertha Araceli Marin-Alejandre, Nuria Pérez-Díaz-Del-Campo, and Verónica Ciaurriz. Additionally, the authors thank the professional staff of the FLiO study (CUN, CIN, and CHN) for their contributions. The pre-doctoral research grant to Paola Mogna-Peláez from the Centre for Nutrition Research of the University of Navarra is gratefully acknowledged. The tractor role from LABORATORIOS CINFA, S.A. and VISCOFAN S.A. for financial support of the Center for Nutrition Research as well as the support from the Government of Navarra are also appreciated. Finally, the authors wish to express their gratitude to the Government of Navarra, CIBERobn, and Fundació La Marató de TV3 for the financial support.
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This research was funded by the Health Department of the Government of Navarra, with the FLiO (Ref. 61/2015) and EHGNA (PC082-083-084) projects, CIBERobn (Physiology of Obesity and Nutrition, CB12/03/30002), Fundació La Marató de TV3 (201630.10), and the Centre for Nutrition Research (CIN) of the University of Navarra.
Author information
Authors and Affiliations
Contributions
PMP, IA, and MAZ conceived, designed, and wrote the article. MAZ and IA were responsible for financial management, the global design, and coordination of this project. FM, IA, and MAZ coordinated the resources. JAT, JAM, IA, and MAZ handled funding acquisition. ABB, JIH, and JIM handled hepatic methodological matters. PMP, ARH, DMP, JIRB, FM, IA, and MAZ managed formal analyses and data curation matters. All the authors reviewed the manuscript of this publication. The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding author
Ethics declarations
Ethics approval
This research was performed under the principles of the Declaration of Helsinki, and it was approved by the Ethics Committee of the University of Navarra (ref. 54/2015).
Informed consent
Informed consent was obtained from all the participants involved in this study.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Key points
•NAFLD is recognized as a silent epidemic with severe complications.
•Metabolomics could be used as a tool to find non-invasive markers for NAFLD.
•Lower serum concentrations of ISO are associated with a higher risk of presenting NAFLD.
Supplementary Information
ESM 1
(52.9 KB)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mogna-Peláez, P., Romo-Hualde, A., Riezu-Boj, J.I. et al. Isoliquiritigenin in combination with visceral adipose tissue and related markers as a predictive tool for nonalcoholic fatty liver disease. J Physiol Biochem (2023). https://doi.org/10.1007/s13105-023-00998-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13105-023-00998-6