Abstract
Standard modifiable cardiovascular risk factors (SMuRFs), such as hypertension, diabetes, dyslipidemia, and current smoking, are associated with the development of atherosclerotic cardiovascular diseases including acute myocardial infarction (MI). Thus, therapeutic approaches against SMuRFs are important as primary and secondary prevention of cardiovascular diseases. In patients with acute MI, however, the prognosis is counterintuitively poor when SMuRFs are lacking. The growing evidence has explored the prevalence, pathophysiology, and prognosis of SMuRF-less patients in acute MI and suggested the potential underlying mechanisms. This review article summarizes the clinical evidence and relevance of the lack of SMuRFs in acute MI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular diseases, represented by acute myocardial infarction (MI), are the most common non-communicable disorders globally and account for approximately one-third of all deaths worldwide [1,2,3]. Standard modifiable cardiovascular risk factors (SMuRFs), such as hypertension, diabetes, dyslipidemia, and current smoking, are associated with the development of cardiovascular diseases in a significant magnitude [4, 5]. A recent pivotal study with pooled individual-level data of more than a million participants across geographic regions demonstrated that nearly 60% of cases of incident cardiovascular disease are attributable to only five SMuRFs (the four factors above plus obesity) [5]. The identification and targeted treatment of SMuRFs can reduce the burden of cardiovascular events as primary and secondary prevention [6,7,8]. When focusing on patients who developed acute MI, however, it has been recently acknowledged that the prognosis is counterintuitively poor in those having none of the SMuRFs as compared to patients with at least one SMuRF (Table 1) [9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32]. The prevalence of SMuRF-less patients varies widely in the previous reports with possible geographic differences. In addition, the poor clinical outcomes in SMuRF-less patients may be time-dependent after acute MI with presumable underlying mechanisms. The current understanding, evidence, and guideline recommendations for ischemic heart disease may not be applicable to patients with no SMuRFs [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72]. This narrative review article provides a practical overview of the current evidence of the lack of SMuRFs in acute MI.
Prevalence of no SMuRFs in acute MI
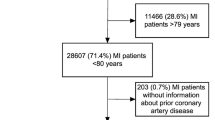
In the field of atherosclerotic cardiovascular disease, SMuRFs play significant roles. Treatment strategies against SMuRFs have been established as effective primary and secondary prevention for over 50 years [73], along with numerous investigations for the risk factors [74,75,76,77,78,79,80,81,82,83,84]. In daily clinical practice, however, we as a clinician often encounter patients who have none of the SMuRFs in a setting of acute MI. A meta-analysis including 1,285,722 patients with acute coronary syndrome (ACS) from 15 studies across regions reported that the prevalence of being SMuRF-less was overall 11.6% [85]. In key previous studies in this literature as shown in Table 1, the prevalence varied widely, ranging from 2 to 31%, which may, at least partially, depend on different definitions of SMuRFs [86]. For instance, some studies employed dyslipidemia as a part of SMuRFs [10, 24], while hypercholesteremia was defined as one of the SMuRFs in others [15, 32]. In addition, “current” smoking was defined as a history of smoking in the past year [24, 32], within 1 month [15], and others. In addition, regional or racial differences may exist in the prevalence of no SMuRFs. As shown in Table 1, the prevalence in studies from East Asia (Japan, China, and Singapore) ranged from 2 to 15%, while from 8 to 31% in Western countries (United States, Canada, Australia, United Kingdom, Sweden, and The Netherlands). Indeed, in the above-mentioned meta-analysis, the proportion of SMuRF-less ACS patients in each geographical region was reported to be lowest in Asia (7.5%), followed by Europe (10.1%), North America (11.7%), and Australia (21.3%) [85]. Nevertheless, it remains unclear whether the regional variation is derived from racial and ethnicity-based differences or is associated with a healthcare system (e.g., annual health checks) and the quality of data collection. Another important point for debate is a potentially increasing trend of the proportion of no SMuRFs in patients with acute MI during recent decades. Early Australian studies indicated an increasing proportion of ST-segment elevation MI (STEMI) patients with no SMuRFs until the mid-2010s [12, 14], while subsequent larger registries in Sweden and the United Kingdom showed no significant trend in the proportion in STEMI and non-ST-segment elevation MI (NSTEMI) [15, 19, 21]. A multi-ethnic registry in Singapore reported that the increasing trend of the proportion of SMuRF-less patients was found only in STEMI but not in NSTEMI [18]. The temporal trend of patients with acute MI and no SMuRFs may be ethnicity- and geography-specific but deserves further investigation (Fig. 1).
Pathophysiology of SMuRFs-less patients
The pathophysiology of patients with acute MI and no SMuRFs has also been investigated. Although underlying mechanisms of acute MI in patients who do not have any SMuRFs remain to be established, non-standard risks should be acknowledged, such as cancer, inflammatory conditions, nutrition, thrombotic factors, environmental and occupational exposures, mental, sleep and oral health, physical activity, social factors, and genetics [86,87,88,89,90,91,92,93,94,95,96,97,98,99,100,101,102,103,104,105]. It is conceivable that SMuRF-less acute MI patients are heterogeneous populations. Therefore, comprehensive screening for such non-standard risk factors is clinically relevant. Indeed, we previously reported that up to one-third of patients with acute MI and no SMuRFs had active cancer and chronic systemic inflammatory diseases (CSIDs) (e.g., rheumatoid arthritis and inflammatory bowel disease) [20, 106], both of which are associated with an increased risk of thrombotic/ischemic events [107, 108]. Importantly, in a setting of acute MI, SMuRF-less patients are likely to be presented with more severe manifestations, including STEMI rather than NSTEMI, left main coronary disease, cardiogenic shock, and cardiac arrest. The proportion of being SMuRF-less is reportedly higher in patient with STEMI than in those with NSTEMI in the previous studies [10, 11, 16, 18, 22, 24, 26, 27]. A Japanese large-scale registry showed that the proportion was even lower in patients with chronic coronary disease (2.5%) than in those with STEMI (4.4%) and NSTEMI (3.2%) [16]. From an angiographic perspective, MI is more likely to be attributable to the left main disease in SMuRF-less patients than in those with at least one SMuRF, particularly in NSTEMI [16, 24]. On the other hand, multivessel coronary artery disease was less frequently observed in acute MI patients with no SMuRFs [109]. In addition, a serial intravascular imaging study showed that SMuRF-less patients with established coronary disease had less atheroma and calcification volumes at baseline and similar rates of coronary plaque progression as compared to those with risk factors [110]. Another mechanistic study with pooled data from 10 randomized percutaneous coronary intervention (PCI) trials showed that SMuRF-less patients more frequently had poor pre-PCI coronary flow (i.e., Thrombolysis In Myocardial Infarction 0 and 1 flow) as compared to those with at least one SMuRF, while no independent associations were found between the presence or absence of SMuRFs and infarct size and left-ventricular ejection fraction after acute MI, assessed with cardiac magnetic resonance (CMR) [17]. An international study using CMR imaging confirmed the results of impaired pre-PCI coronary flow and similar left-ventricular damage in SMuRF-less patients [109]. Although a post hoc analysis of the DANAMI-3 trial showed that SMuRF-less patients had a larger infarct size and a smaller area of myocardial salvage on CMR following PCI, the association was mediated by a greater proportion of culprit vessel in the left anterior descending coronary artery and poor pre-PCI coronary blood flow [111]. Of note, patients with acute MI and no SMuRFs are predisposed to be presented with cardiogenic shock and cardiac arrest, leading to a poor prognosis in this patient subset. Although unestablished yet, we believe that the higher risks of cardiogenic shock and cardiac arrest may be attributed to no preconditioning in SMuRF-less patients and the potential underreporting of risk factors (Fig. 1). Acute MI can be driven by a sudden and aggressive thrombotic alteration with the lack of ischemic preconditioning in patients without SMuRFs [112]. In a previous study, the presence of pre-existing ischemic events and diseases was associated with better short-term prognosis after acute MI [113]. Another possible mechanism of severe clinical presentation in SMuRF-less patients with acute MI includes the underreporting of risk factors. It is conceivable that patients with severe clinical presentation of acute MI are likely to have incomplete medical records, particularly when they die shortly after admission [21, 114], potentially resulting in lower recorded rates of SMuRFs in patients with cardiogenic shock and cardiac arrest. Although the pathophysiology under acute MI without standard risks remains to be elucidated, comprehensive evaluation and scrutiny should be done when managing SMuRF-less patients and interpreting the results of studies focusing on no SMuRFs in acute MI [115].
Prognosis of no SMuRFs after acute MI
The prognosis after acute MI in patients with no SMuRFs is counterintuitively worse than those with SMuRFs. Although some studies showed neutral results or even lower mortality rates in SMuRF-less patients [16, 19, 32], in-hospital or 30-day mortality after MI is higher when SMuRFs are absent (Table 1). Intriguingly, the prevalence of being SMuRF-less in acute MI may be lower, while the short-term mortality in patients with no SMuRFs might be higher in studies from Asian countries, especially in East Asia (Table 1). Overall, a meta-analysis demonstrated a 1.5-fold higher in-hospital mortality in SMuRF-less patients [85]. The sex difference in the prevalence of being SMuRF-less in patients with acute MI is unclear [85], and the impact of sex on short-term prognosis is complicated. The traditional understanding is that among general ACS and acute MI populations, women have a worse prognosis than men [116, 117]. Similarly, women without any SMuRFs reportedly have higher mortality after acute MI than men with no SMuRFs [15, 23, 28]. However, the “negative” prognostic impact of the lack of SMuRFs as compared to having such risk factors might be greater in men than in women [29]. Contrary to short-term mortality, the prognostic impact of being SMuRF-less on long-term outcomes after acute MI has not been established [22, 27]. The mechanisms of the higher in-hospital mortality are still unclear, but it may be associated with different patient profiles, severe clinical presentation, and less aggressive medical treatment in patients without SMuRFs. Acute MI in patients with no SMuRFs may be attributable to background cancer and CSIDs in up to one-third of cases [20], which are potentially associated with the high mortality rate. However, even after excluding patients with active cancer and CSIDs, the absence of SMuRFs was associated with increased in-hospital mortality in our previous report [106]. Another important point to note is that patients with no SMuRFs are less likely to receive intensive therapeutic strategies, including primary PCI and medications (e.g., angiotensin-converting-enzyme inhibitor, β-blocker, and statin) [19, 23, 85, 118]. Nonetheless, even when focusing only on patients undergoing PCI, the short-term prognosis after MI is worse in SMuRF-less patients [20, 24, 29, 31]. The lack of hypertension, diabetes, dyslipidemia, and current smoking as a therapeutic target presumably makes it challenging to improve clinical outcomes in SMuRF-less patients. Given that long-term outcomes do not differ considerably between patients with and without SMuRFs, it is currently uncertain whether the less frequent prescription of guideline-directed medical therapy in SMuRF-less patients has a prognostic impact, but to improve outcomes, guideline-recommended management should be considered in this vulnerable patient subset.
Conclusions
Despite recent advances in the evidence-based management of acute MI, patients who develop coronary atherosclerosis and thrombotic events in the absence of traditional risk factors are underrecognized, and diagnostic and therapeutic pathways are unestablished in patients with MI and no SMuRFs. Although the prevalence, pathophysiology, and prognosis of SMuRF-less patients with acute MI have been increasingly reported, dedicated clinical studies are warranted to better define characteristics and outcomes and to clarify novel risk factors and specific secondary preventive strategies in this unique and vulnerable patient population.
References
Saito I, Yamagishi K, Kokubo Y, Yatsuya H, Iso H, Sawada N, et al. Impact of cardiovascular disease on the death certificate diagnosis of heart failure, ischemic heart disease, and cerebrovascular disease—The Japan Public Health Center-based prospective study. Circ J. 2023;87:1196–202.
Joseph P, Leong D, McKee M, Anand SS, Schwalm JD, Teo K, et al. Reducing the global burden of cardiovascular disease, part 1: the epidemiology and risk factors. Circ Res. 2017;121:677–94.
GBD 2021 Causes of Death Collaborators. Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. 2024;403:2100–32.
Walli-Attaei M, Rosengren A, Rangarajan S, Breet Y, Abdul-Razak S, Sharief WA, et al. Metabolic, behavioural, and psychosocial risk factors and cardiovascular disease in women compared with men in 21 high-income, middle-income, and low-income countries: an analysis of the PURE study. Lancet. 2022;400:811–21.
Magnussen C, Ojeda FM, Leong DP, Alegre-Diaz J, Amouyel P, Aviles-Santa L, et al. Global effect of modifiable risk factors on cardiovascular disease and mortality. N Engl J Med. 2023;389:1273–85.
Nakano S, Kohsaka S, Chikamori T, Fukushima K, Kobayashi Y, Kozuma K, et al. JCS 2022 guideline focused update on diagnosis and treatment in patients with stable coronary artery disease. Circ J. 2022;86:882–915.
Byrne RA, Rossello X, Coughlan JJ, Barbato E, Berry C, Chieffo A, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023;44:3720–826.
Nohara A. The worst combination for coronary artery disease under strong-statin therapy is chronic kidney disease and diabetes—non-lipid residual risk assessment from the REAL-CAD study. Circ J. 2024;88:1004–6.
Roe MT, Halabi AR, Mehta RH, Chen AY, Newby LK, Harrington RA, et al. Documented traditional cardiovascular risk factors and mortality in non-ST-segment elevation myocardial infarction. Am Heart J. 2007;153:507–14.
Nauta ST, Deckers JW, van der Boon RM, Akkerhuis KM, van Domburg RT. Risk factors for coronary heart disease and survival after myocardial infarction. Eur J Prev Cardiol. 2014;21:576–83.
Wang JY, Goodman SG, Saltzman I, Wong GC, Huynh T, Dery JP, et al. Cardiovascular risk factors and in-hospital mortality in acute coronary syndromes: insights from the canadian global registry of acute coronary events. Can J Cardiol. 2015;31:1455–61.
Vernon ST, Coffey S, Bhindi R, Soo Hoo SY, Nelson GI, Ward MR, et al. Increasing proportion of ST elevation myocardial infarction patients with coronary atherosclerosis poorly explained by standard modifiable risk factors. Eur J Prev Cardiol. 2017;24:1824–30.
Singh A, Collins BL, Gupta A, Fatima A, Qamar A, Biery D, et al. Cardiovascular risk and statin eligibility of young adults after an MI: partners YOUNG-MI Registry. J Am Coll Cardiol. 2018;71:292–302.
Vernon ST, Coffey S, D’Souza M, Chow CK, Kilian J, Hyun K, et al. ST-segment-elevation myocardial infarction (STEMI) patients without standard modifiable cardiovascular risk factors—how common are they, and what are their outcomes? J Am Heart Assoc. 2019;8: e013296.
Figtree GA, Vernon ST, Hadziosmanovic N, Sundstrom J, Alfredsson J, Arnott C, et al. Mortality in STEMI patients without standard modifiable risk factors: a sex-disaggregated analysis of SWEDEHEART registry data. Lancet. 2021;397:1085–94.
Yamamoto K, Natsuaki M, Morimoto T, Shiomi H, Takeji Y, Yamaji K, et al. Coronary artery disease without standard cardiovascular risk factors. Am J Cardiol. 2022;164:34–43.
Figtree GA, Redfors B, Kozor R, Vernon ST, Grieve SM, Mazhar J, et al. Clinical outcomes in patients with ST-segment elevation MI and no standard modifiable cardiovascular risk factors. JACC Cardiovasc Interv. 2022;15:1167–75.
Sia CH, Ko J, Zheng H, Ho AF, Foo D, Foo LL, et al. Comparison of mortality outcomes in acute myocardial infarction patients with or without standard modifiable cardiovascular risk factors. Front Cardiovasc Med. 2022;9: 876465.
Moledina SM, Rashid M, Nolan J, Nakao K, Sun LY, Velagapudi P, et al. Addressing disparities of care in non-ST-segment elevation myocardial infarction patients without standard modifiable risk factors: insights from a nationwide cohort study. Eur J Prev Cardiol. 2022;29:1084–92.
Suzuki S, Saito Y, Yamashita D, Matsumoto T, Sato T, Wakabayashi S, et al. Clinical characteristics and prognosis of patients with no standard modifiable risk factors in acute myocardial infarction. Heart Lung Circ. 2022;31:1228–33.
Figtree GA, Vernon ST, Hadziosmanovic N, Sundstrom J, Alfredsson J, Nicholls SJ, et al. Mortality and cardiovascular outcomes in patients presenting with non-ST elevation myocardial infarction despite no standard modifiable risk factors: results from the SWEDEHEART registry. J Am Heart Assoc. 2022;11: e024818.
Kong G, Chew NWS, Ng CH, Chin YH, Zeng R, Foo R, et al. Long-term outcomes in acute coronary syndrome patients without standard modifiable risk factors: a multi-ethnic retrospective cohort study of 5400 asian patients. J Thromb Thrombolysis. 2022;54:569–78.
Li S, Gao X, Yang J, Xu H, Wang Y, Zhao Y, et al. Number of standard modifiable risk factors and mortality in patients with first-presentation ST-segment elevation myocardial infarction: insights from China Acute Myocardial Infarction registry. BMC Med. 2022;20:217.
Saito Y, Inohara T, Kohsaka S, Wada H, Takamisawa I, Yamaji K, et al. Characteristics and outcomes of patients with no standard modifiable risk factors undergoing primary revascularization for acute myocardial infarction: insights from the nationwide Japanese percutaneous coronary intervention registry. Am Heart J. 2023;258:69–76.
Kelly C, Lan NSR, Phan J, Hng C, Matthews A, Rankin JM, et al. Characteristics and outcomes of young patients with ST-elevation myocardial infarction without standard modifiable risk factors. Am J Cardiol. 2023;202:81–9.
Sheikh S, Peerwani G, Hanif B, Virani S. Clinical characteristics, management, and 5-year survival compared between no standard modifiable risk factor (SMuRFless) and ≥ 1 SMuRF ACS cases: an analysis of 15,051 cases from Pakistan. BMC Cardiovasc Disord. 2023;23:320.
Gonzalez-Del-Hoyo M, Rossello X, Peral V, Pocock S, Van de Werf F, Chin CT, et al. Impact of standard modifiable cardiovascular risk factors on 2-year all-cause mortality: insights from an international cohort of 23,489 patients with acute coronary syndrome. Am Heart J. 2023;264:20–30.
Sheikhy A, Fallahzadeh A, Jameie M, Aein A, Masoudkabir F, Maghsoudi M, et al. In-hospital and 1-year outcomes of patients without modifiable risk factors presenting with acute coronary syndrome undergoing PCI: a sex-stratified analysis. Front Cardiovasc Med. 2023;10:1235667.
Jang SJ, Kim LK, Sobti NK, Yeo I, Cheung JW, Feldman DN, et al. Mortality of patients with ST-segment-elevation myocardial infarction without standard modifiable risk factors among patients without known coronary artery disease: age-stratified and sex-related analysis from nationwide readmissions database 2010–2014. Am J Prev Cardiol. 2023;14: 100474.
Justin Paul G, Sankaran S, Saminathan K, Iliyas M, Sethupathy S, Saravanan S, et al. Outcomes of ST segment elevation myocardial infarction without standard modifiable cardiovascular risk factors—newer insights from a prospective registry in India. Glob Heart. 2023;18:13.
Iwata J, Inohara T, Shiraishi Y, Nakamaru R, Niimi N, Ueda I, et al. Standard modifiable cardiovascular risk factors in patients with acute coronary syndrome: a report from multicenter percutaneous coronary intervention registry. J Cardiol. 2023;81:571–6.
Zhao G, Zhou M, Zhao X, Ma C, Han Y, Liu J, et al. Characteristics, treatment, and in-hospital outcomes of older patients with stemi without standard modifiable risk factors. JACC Asia. 2024;4:73–83.
Akase H, Okamura T, Nagoshi R, Fujimura T, Miyazaki Y, Takenaka H, et al. Risk assessment of side branch compromise after coronary bifurcation stenting—a substudy of the 3D-OCT bifurcation registry. Circ J. 2024;88:959–69.
Akashi N, Matoba T, Kohro T, Oba Y, Kabutoya T, Imai Y, et al. Sex differences in long-term outcomes in patients with chronic coronary syndrome after percutaneous coronary intervention—insights from a Japanese real-world database using a storage system. Circ J. 2023;87:775–82.
Arai R, Okumura Y, Murata N, Fukamachi D, Honda S, Nishihira K, et al. Prevalence and impact of polyvascular disease in patients with acute myocardial infarction in the contemporary era of percutaneous coronary intervention—insights from the Japan acute myocardial infarction registry (JAMIR). Circ J. 2024;88:911–20.
Asada K, Saito Y, Sato T, Matsumoto T, Yamashita D, Suzuki S, et al. Prognostic value of natriuretic peptide levels and in-hospital heart failure events in patients with acute myocardial infarction. Circ J. 2023;87:640–7.
Feng X, Xu Y, Zeng M, Qin Y, Weng Z, Sun Y, et al. Optical coherence tomography assessment of coronary lesions associated with microvascular dysfunction in ST-segment elevation myocardial infarction. Circ J. 2023;87:1625–32.
Fujihara M, Tsukizawa T, Yazu Y, Tsujikawa S, Yokoi Y, Uesima D. Cost change of elective percutaneous coronary artery intervention for chronic coronary syndrome in Japan from 2010 to 2019. Circ J. 2023;87:767–74.
Fukui K, Takahashi J, Hao K, Honda S, Nishihira K, Kojima S, et al. Disparity of performance measure by door-to-balloon time between a rural and urban area for management of patients with ST-segment elevation myocardial infarction - insights from the nationwide Japan acute myocardial infarction registry. Circ J. 2023;87:648–56.
Godo S, Yasuda S. New landscape of acute myocardial infarction complicated by cardiogenic shock with the advent of a small but mighty heart pump. Circ J. 2023;87:598–9.
Hanada K, Kinjo T, Yokoyama H, Tsushima M, Senoo M, Ichikawa H, et al. Incidence, predictors, and outcome associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0023.
Hokimoto S, Kaikita K, Yasuda S, Tsujita K, Ishihara M, Matoba T, et al. JCS/CVIT/JCC 2023 guideline focused update on diagnosis and treatment of vasospastic angina (coronary spastic angina) and coronary microvascular dysfunction. Circ J. 2023;87:879–936.
Horikoshi T, Nakamura T, Yoshizaki T, Nakamura J, Uematsu M, Kobayashi T, et al. Predictive value of CHADS(2), CHA(2)DS(2)-VASc and R(2)-CHADS(2) scores for short- and long-term major adverse cardiac events in non-ST-segment elevation myocardial infarction. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0733.
Ikeda Y, Ako J, Toda K, Hirayama A, Kinugawa K, Kobayashi Y, et al. Short-term outcomes of Impella support in japanese patients with cardiogenic shock due to acute myocardial infarction—Japanese Registry for Percutaneous Ventricular Assist Device (J-PVAD). Circ J. 2023;87:588–97.
Ishii H. Importance of the assessment of infarction size in patients undergoing percutaneous coronary intervention for acute myocardial infarction. Circ J. 2022;86(12):1980–1.
Ishii M, Nakamura T, Tsujita K. Intravascular imaging and coronary microvascular dysfunction after percutaneous coronary intervention in ST-segment elevation myocardial infarction. Circ J. 2023;87(11):1633–4.
Itoh T. Just because the acute myocardial infarction patient is simply elderly, or is there something else?—We need to acknowledge sex differences. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0755.
Kikuchi M, Tahara Y, Yamaguchi J, Nakashima T, Nomura O, Tanaka A, et al. Executive summary—acute coronary syndrome in the Japan Resuscitation Council guidelines for resuscitation 2020. Circ J. 2023;87:866–78.
Kimura S, Isshiki A, Shimizu M, Fujii H, Suzuki M. Clinical significance of coronary healed plaques in stable angina pectoris patients undergoing percutaneous coronary intervention. Circ J. 2023;87:1643–53.
Kitahara H. How can we prevent both bleeding and ischemic events after percutaneous coronary intervention in high-bleeding risk patients? Circ J. 2022;86:1362–4.
Kondo Y, Noda T, Takanashi Y, Sasaki S, Sato Y, Nitta T, et al. Two-year outcomes of primary prophylactic use of defibrillators for ischemic and non-ischemic cardiomyopathy—propensity score-matched analysis from the Nippon Storm Study. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0613.
Moriwaki K, Kurita T, Hirota Y, Ito H, Ishise T, Fujimoto N, et al. Prognostic impact of prehospital simple risk index in patients with ST-elevation myocardial infarction. Circ J. 2023;87:629–39.
Muramatsu T, Masuda S, Kotoku N, Kozuma K, Kawashima H, Ishibashi Y, et al. Prasugrel monotherapy after percutaneous coronary intervention with biodegradable-polymer platinum-chromium everolimus eluting stent for Japanese patients with chronic coronary syndrome (ASET-JAPAN). Circ J. 2023;87:857–65.
Nakatani S, Sotomi Y, Suzuki S, Kobayashi T, Hamanaka Y, Omatsu T, et al. Angioscopic comparison of early- and mid-term vascular responses following treatment of ST-elevation acute myocardial infarction with biodegradable vs. durable polymer everolimus-eluting stents—a prespecified subanalysis of the MECHANISM AMI RCT. Circ J. 2023;87:619–28.
Natsuaki M, Morimoto T, Iimuro S, Fujita R, Iwata H, Miyauchi K, et al. Thrombotic risk stratification and intensive statin therapy for secondary prevention of coronary artery disease—insights from the REAL-CAD study. Circ J. 2022;86:1416–27.
Ohashi J, Sakakura K, Jinnouchi H, Taniguchi Y, Tsukui T, Watanabe Y, et al. Comparison of long-term clinical outcomes in patients stratified by a novel acute myocardial infarction risk stratification (nARS) system. Circ J. 2022;86:1519–26.
Okamoto H, Nishi T, Ishii M, Tsujita K, Koto S, Nakai M, et al. Clinical characteristics and outcomes of patients presenting with acute myocardial infarction without cardiogenic shock. Circ J. 2022;86:1527–38.
Omori H, Kawase Y, Mizukami T, Tanigaki T, Hirata T, Okubo M, et al. Diagnostic accuracy of artificial intelligence-based angiography-derived fractional flow reserve using pressure wire-based fractional flow reserve as a reference. Circ J. 2023;87:783–90.
Roh JW, Bae S, Johnson TW, Heo SJ, Kim Y, Cho DK, et al. Impact of intravascular ultrasound-guided percutaneous coronary intervention in patients with acute myocardial infarction and chronic kidney disease. Circ J. 2023;87:1339–46.
Sasaki K, Koeda Y, Yoshizawa R, Ishikawa Y, Ishida M, Itoh T, et al. Comparing in-hospital outcomes for acute myocardial infarction patients in high-volume hospitals performing primary percutaneous coronary intervention vs. regional general hospitals. Circ J. 2023;87:1347–55.
Sawayama Y, Tomita Y, Kohyama S, Higo Y, Kodama K, Asada K, et al. Clopidogrel use in CYP2C19 loss-of-function carriers with high bleeding risk after percutaneous coronary intervention. Circ J. 2023;87:755–63.
Shikuma A, Nishi M, Matoba S. Sex differences in process-of-care and in-hospital prognosis among elderly patients hospitalized with acute myocardial infarction. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0543.
Suzuki N, Yokoi T, Kimura T, Ikeda Y, Takahashi S, Aoyagi T, et al. Prediction of slow-flow phenomenon after stent implantation using near-infrared spectroscopy in patients with acute and chronic coronary syndrome. Circ J. 2024;88:972–9.
Takagi R, Kubo T. Clinical value of optical coherence tomography in guiding bifurcation percutaneous coronary intervention. Circ J. 2024;88:970–1.
Takeji Y, Morimoto T, Shiomi H, Kato ET, Imada K, Yoshikawa Y, et al. Sex differences in clinical outcomes after percutaneous coronary intervention. Circ J. 2023;87:277–86.
Ueda Y. Slow-flow phenomenon caused by distal embolization should be predicted and prevented to maximize the efficacy of coronary intervention. Circ J. 2024;88:980–1.
Ueno H, Hoshino M, Usui E, Sugiyama T, Kanaji Y, Hada M, et al. Prognostic implications of fractional flow reserve and coronary flow reserve after drug-eluting stent implantation. Circ J. 2024;88:853–9.
Watanabe H, Morimoto T, Yamamoto K, Obayashi Y, Natsuaki M, Yamaji K, et al. Prevalence and effects of high-intensity statins for japanese patients presenting with acute coronary syndrome—a post hoc secondary analysis of STOPDAPT-2 ACS. Circ J. 2023;87:657–68.
Yamamoto K, Shiomi H, Morimoto T, Miyazawa A, Watanabe H, Nakamura S, et al. Dual antiplatelet therapy duration after multivessel optimal intravascular ultrasound-guided percutaneous coronary intervention. Circ J. 2023;87:1661–71.
Yamamoto K, Shiomi H, Morimoto T, Watanabe H, Miyazawa A, Yamaji K, et al. Comparison of the OPTIVUS-complex PCI multivessel cohort with the historical CREDO-Kyoto registry cohort-3. Circ J. 2023. https://doi.org/10.1253/circj.CJ-22-0837.
Yufu K, Shimomura T, Kawano K, Sato H, Yonezu K, Saito S, et al. Usefulness of prehospital 12-lead electrocardiography system in ST-segment elevation myocardial infarction patients in Oita—comparison between urban and rural areas, weekday daytime and weekday nighttime/holidays. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0365.
Yamamoto K, Morimoto T, Natsuaki M, Shiomi H, Ozasa N, Sakamoto H, et al. Polypharmacy and bleeding outcomes after percutaneous coronary intervention. Circ J. 2024;88:888–99.
Avis SR, Vernon ST, Hagström E, Figtree GA. Coronary artery disease in the absence of traditional risk factors: a call for action. Eur Heart J. 2021;42:3822–4.
Geng L, Shi X, Yuan Y, Du P, Gao L, Wang Y, et al. Anatomical and functional discrepancy in diabetic patients with intermediate coronary lesions—an intravascular ultrasound and quantitative flow ratio study. Circ J. 2023;87:320–8.
Higuma T, Akashi YJ, Fukumoto Y, Obara H, Kakuma T, Asaumi Y, et al. Residual coronary risk factors associated with long-term clinical outcomes in patients with coronary artery disease treated with high- vs. low-dose statin therapy—REAL-CAD substudy. Circ J. 2024;88:995–1003.
Hisamatsu T, Kinuta M. Long-term effect of smoking ban legislation on hospitalization for acute coronary syndrome. Circ J. 2023;87:1686–8.
Kiyosue A, Yasuda S, Tomura A, Usami M, Arai H. Safety and effectiveness of alirocumab, a proprotein convertase subtilisin/kexin type 9 (PCSK9) inhibitor, in patients with familial or non-familial hypercholesterolemia—a post-marketing survey (J-POSSIBLE). Circ J. 2023;87:834–46.
Nakai M, Iwanaga Y, Sumita Y, Amano T, Fukuda I, Hirano T, et al. Long-term follow-up study of hospitalizations for acute coronary syndrome in kobe-city and other districts under the Hyogo smoking ban legislation—a nationwide database study. Circ J. 2023;87:1680–5.
Ogura M. Is high-density lipoprotein functionality useful as a residual risk marker for familial hypercholesterolemia? Circ J. 2023;87:813–4.
Otake H. Obesity paradox in patients with acute myocardial infarction. Circ J. 2022;86:640–1.
Tada H, Okada H, Nohara A, Toh R, Harada A, Murakami K, et al. Impact of high-density lipoprotein function, rather than high-density lipoprotein cholesterol level, on cardiovascular disease among patients with familial hypercholesterolemia. Circ J. 2023;87:806–12.
Takeuchi F, Takano K, Yamamoto M, Isono M, Miyake W, Mori K, et al. Clinical implication of smoking-related aryl-hydrocarbon receptor repressor (AHRR) hypomethylation in japanese adults. Circ J. 2022;86:986–92.
Toyota T, Morimoto T, Iimuro S, Fujita R, Iwata H, Miyauchi K, et al. Low-density lipoprotein cholesterol levels on statins and cardiovascular event risk in stable coronary artery disease—an observation from the REAL-CAD study. Circ J. 2023;87:360–7.
Zhan R, Zhang J, Chen X, Liu T, He Y, Zhang S, et al. Targeting the efficacy of intensive blood pressure treatment in hypertensive patients—an exploratory analysis of SPRINT. Circ J. 2023;87:1212–8.
Kong G, Chin YH, Chong B, Goh RSJ, Lim OZH, Ng CH, et al. Higher mortality in acute coronary syndrome patients without standard modifiable risk factors: results from a global meta-analysis of 1,285,722 patients. Int J Cardiol. 2023;371:432–40.
Figtree GA, Vernon ST, Harmer JA, Gray MP, Arnott C, Bachour E, et al. Clinical pathway for coronary atherosclerosis in patients without conventional modifiable risk factors: JACC state-of-the-art review. J Am Coll Cardiol. 2023;82:1343–59.
Abe S, Haruyama Y, Kobashi G, Toyoda S, Inoue T, Tomiyama H, et al. Effect of novel stratified lipid risk by “LDL-Window” and flow-mediated dilation on the prognosis of coronary artery disease using the FMD-J study a data. Circ J. 2022;86:1444–54.
Ashikawa H, Adachi T, Iwatsu K, Kamisaka K, Kamiya K, Uchiyama Y, et al. Physical frailty may predict 2-year prognosis in elderly patients with acute myocardial infarction—a report from the FLAGSHIP study. Circ J. 2023;87:490–7.
Fujiu K. Brain-heart dialogue—decoding its role in homeostasis and cardiovascular disease. Circ J. 2023. https://doi.org/10.1253/circj.CJ-23-0579.
Iijima R. Polypharmacy as new risk factor of major bleeding in patients undergoing coronary stent implantation—which come first, the chicken or the egg? Circ J. 2024;88:900–1.
Ikenaga H, Nakano Y. Importance of the assessment of physical frailty in elderly Japanese patients with acute myocardial infarction. Circ J. 2023;87:498–9.
Ishii H. Acute coronary syndrome and cancer—cardio-oncology in the super aged society in Japan. Circ J. 2024;88:215–6.
Kadowaki H, Akazawa H, Shindo A, Ueda T, Ishida J, Komuro I. Shared and reciprocal mechanisms between heart failure and cancer—an emerging concept of heart-cancer axis. Circ J. 2024;88:182–8.
Kobayashi T, Kitahara H, Kato K, Saito Y, Kobayashi Y. Impact of parathyroid hormone level on intracoronary calcification and short- and long-term outcomes in dialysis patients undergoing percutaneous coronary intervention. Circ J. 2023;87:247–55.
Mizuno A, Kaneko H, Suzuki Y, Okada A, Takeda N, Morita H, et al. Enduring relevance of the stages of change model for transforming lifestyle behaviors. Circ J. 2023;87:1138–42.
Numasawa Y. Impact of platelet reactivity on ischemic and bleeding events after percutaneous coronary intervention—a long-term perspective. Circ J. 2022;86:1350–1.
Otsuki H, Yamaguchi J. Intact parathyroid hormone in hemodialysis patients undergoing percutaneous coronary intervention—is it just a marker or a diamond in the rough? Circ J. 2023;87:256–7.
Suzuki T, Mizuno A, Yasui H, Noma S, Ohmori T, Rewley J, et al. Scoping review of screening and assessment tools for social determinants of health in the field of cardiovascular disease. Circ J. 2024;88:390–407.
Takei Y, Tomiyama H, Higashi Y, Yamashina A, Chikamori T. Association between endothelial dysfunction and left ventricular diastolic stiffness—subanalysis of the flow-mediated dilation Japan (FMD-J) study. Circ J. 2023;87:1203–11.
Takeuchi T, Kosugi S, Ueda Y, Ikeoka K, Yamane H, Takayasu K, et al. Impact of a cancer history on cardiovascular events among patients with myocardial infarction who received revascularization. Circ J. 2024;88:207–14.
Tamura Y, Tamura Y, Taniguchi H, Imanaka-Yoshida K. Acute myocarditis after discontinuation of immune checkpoint inhibitor therapy. Circ J. 2023;87:376.
Tokeshi T, Date A, Miura H, Kumasaka L, Arakawa T, Nakao K, et al. Predictors of improvement in exercise capacity after cardiac rehabilitation differ between octogenarian and young-old patients with acute myocardial infarction. Circ J. 2023;87:815–23.
Yoshifuji H, Nakaoka Y, Uchida HA, Sugihara T, Watanabe Y, Funakoshi S, et al. Organ damage and quality of life in Takayasu arteritis—evidence from a national registry analysis. Circ J. 2024;88:285–94.
Zhang Y, Hao W, Fan J, Guo R, Ai H, Que B, et al. Association between obstructive sleep apnea and cardiovascular events in acute coronary syndrome patients with or without revascularization—a prospective cohort study. Circ J. 2023;87:1369–79.
Makita S, Yasu T, Akashi YJ, Adachi H, Izawa H, Ishihara S, et al. JCS/JACR 2021 guideline on rehabilitation in patients with cardiovascular disease. Circ J. 2022;87:155–235.
Yaginuma H, Saito Y, Goto H, Asada K, Shiko Y, Sato T, et al. Impact of cancer, inflammation, and no standard risk factors in patients with myocardial infarction. JACC Asia. 2024. https://doi.org/10.1016/j.jacasi.2024.03.008.
Matsumoto T, Saito Y, Yamashita D, Sato T, Wakabayashi S, Kitahara H, et al. Impact of active and historical cancer on short- and long-term outcomes in patients with acute myocardial infarction. Am J Cardiol. 2021;159:59–64.
Yaginuma H, Saito Y, Sato T, Yamashita D, Matsumoto T, Suzuki S, et al. Clinical characteristics and outcomes of patients with chronic systemic inflammatory disease in acute myocardial infarction. PLoS ONE. 2023;18: e0289794.
Reindl M, Stiermaier T, Lechner I, Tiller C, Holzknecht M, Fink P, et al. Infarct severity and outcomes in ST-elevation myocardial infarction patients without standard modifiable risk factors—a multicenter cardiac magnetic resonance study. Eur J Intern Med. 2024;119:78–83.
Mazhar J, Figtree G, Vernon ST, Galougahi KK, Carlo J, Nissen SE, et al. Progression of coronary atherosclerosis in patients without standard modifiable risk factors. Am J Prev Cardiol. 2020;4: 100116.
Mazhar J, Ekstrom K, Kozor R, Grieve SM, Nepper-Christensen L, Ahtarovski KA, et al. Cardiovascular magnetic resonance characteristics and clinical outcomes of patients with ST-elevation myocardial infarction and no standard modifiable risk factors-A DANAMI-3 substudy. Front Cardiovasc Med. 2022;9: 945815.
Pineda JRE, Lee KS. Defining outcomes in East Asian elderly STEMI patients without standard modifiable risk factors. JACC Asia. 2024;4:84–6.
Herrett E, Bhaskaran K, Timmis A, Denaxas S, Hemingway H, Smeeth L. Association between clinical presentations before myocardial infarction and coronary mortality: a prospective population-based study using linked electronic records. Eur Heart J. 2014;35:2363–71.
Kanaoka K, Iwanaga Y, Okada K, Terasaki S, Nishioka Y, Nakai M, et al. Validity of diagnostic algorithms for cardiovascular diseases in Japanese health insurance claims. Circ J. 2023;87:536–42.
Moysidis DV, Daios S, Anastasiou V, Liatsos AC, Papazoglou AS, Karagiannidis E, et al. Association of clinical, laboratory and imaging biomarkers with the occurrence of acute myocardial infarction in patients without standard modifiable risk factors—rationale and design of the “Beyond-SMuRFs Study.” BMC Cardiovasc Disord. 2023;23:149.
Smilowitz NR, Mahajan AM, Roe MT, Hellkamp AS, Chiswell K, Gulati M, et al. Mortality of myocardial infarction by sex, age, and obstructive coronary artery disease status in the ACTION Registry-GWTG (acute coronary treatment and intervention outcomes network registry-get with the guidelines). Circ Cardiovasc Qual Outcomes. 2017;10: e003443.
Berger JS, Elliott L, Gallup D, Roe M, Granger CB, Armstrong PW, et al. Sex differences in mortality following acute coronary syndromes. JAMA. 2009;302:874–82.
Oba Y, Kabutoya T, Kohro T, Imai Y, Kario K, Sato H, et al. Relationships among heart rate, beta-blocker dosage, and prognosis in patients with coronary artery disease in a real-world database using a multimodal data acquisition system. Circ J. 2023;87:336–44.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yuichi Saito received lecture fees from Daiichi Sankyo. Kenichi Tsujita received lecture fees from Abbott Medical, Amgen, Bayer Yakuhin, Daiichi Sankyo, Kowa Pharmaceutical, Nippon Boehringer Ingelheim, Novartis Pharma, Otsuka Pharmaceutical, Pfizer Japan, Takeda Pharmaceutical, and TERUMO; research grants from Bayer Yakuhin, Bristol-Myers, Daiichi Sankyo, MOCHIDA PHARMACEUTICAL, EA Pharma, Novo Nordisk Pharma, and PRA Health Sciences; and scholarship funds from Abbott Medical, Boehringer Ingelheim, Otsuka Pharmaceutical, and Boston Scientific Japan; and belongs to the endowed departments donated by Abbott Japan, Boston Scientific Japan, Fides-one, GM Medical, ITI, Kaneka Medix, NIPRO, TERUMO, Philips Japan, Getinge Group Japan, Orbusneich Medical, Abbott Medical, BIOTRONIK JAPAN, Boston Scientific Japan, Fukuda Denshi, Japan Lifeline, Medtronic Japan, and Nippon Boehringer Ingelheim. Yoshio Kobayashi received lecture fees from Abbott Medical Japan and Daiichi Sankyo and research grants from Abbott Medical Japan, Win International, Otsuka Pharmaceutical, Boehringer Ingelheim, Nipro, and Japan Lifeline.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saito, Y., Tsujita, K. & Kobayashi, Y. No standard modifiable cardiovascular risk factors in acute myocardial infarction: prevalence, pathophysiology, and prognosis. Cardiovasc Interv and Ther (2024). https://doi.org/10.1007/s12928-024-01022-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12928-024-01022-4