Abstract
Background
Patients with acute myocardial infarction (AMI) and large thrombus burden (LTB) still represent a challenge. Afflicted patients have a high morbidity and mortality. Aspiration thrombectomy is often ineffective in those cases. Mechanical thrombectomy devices (MTDs), which are effective for management of ischemic strokes, were recently CE-approved for treatment of thrombotic coronary lesions. Real-world data about their performance in AMI cases with LTB are scarce. This study sought to summarize our early experience with a novel MTD device in this context.
Methods
We analyzed consecutive patients from the prospective OPTIMISER registry (NCT04988672), who have been managed with the NeVa™ MTD (Vesalio, USA) for AMI with LTB at a tertiary cardiology facility. Outcomes of interest included, among others, periprocedural complications, target lesion failure (TLF), target lesion revascularization (TLR) and target vessel myocardial infarction (TV-MI).
Results
Overall, 15 patients underwent thrombectomy with the NeVa™ device. Thrombectomy was successfully performed in 14 (93%) patients. Final TIMI 3 flow was achieved in 13 (87%) patients, while 2 (13%) patients had TIMI 2 flow. We encountered no relevant periprocedural complications, especially no stroke, stent thrombosis or vessel closure. After a mean follow-up time of 26 ± 2.9 months, 1 (7%) patient presented with TLR due to stent thrombosis (10 months after treatment with the MTD and stenting).
Conclusions
In AMI patients with LTB, the deployment of the novel NeVa™ MTD seems efficient and safe. Further randomized trials are warranted to assess whether the use of the NeVa™ device in cases with LTB improves procedural and clinical outcomes.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The management of patients with acute myocardial infarction (AMI) and large thrombus burden (LTB) remains challenging. Despite the advent of potent antithrombotic regimens, percutaneous coronary intervention (PCI) in AMI cases with LTB often results in spontaneous and procedure-related distal thrombus embolization (DTE) with consecutive flow deterioration (“slow-flow or no-reflow phenomenon”) [1,2,3,4]. DTE is not only associated with microvascular obstruction (MVO), which in turn increases infarct size and adversely impacts ventricular remodelling and function, but it is furthermore linked to a higher risk for target vessel failure and stent thrombosis (ST) [1,2,3,4]. Of note, AMI patients with LTB have a two to fourfold greater risk for major adverse cardiovascular events compared to other AMI patients [5, 6].
Over the last decades, multiple approaches for management of thrombotic coronary lesions have been proposed [3]. Especially, thrombectomy devices, which are classified as manual or mechanical thrombectomy devices (MTD), have initially been promoted and investigated with a lot of enthusiasm, since they appeared to reduce the risk for DTE [7]. But the major trials have failed to show any clinical benefit with routine use of those devices [7, 8].
Stent-based MTDs, also referred to as stent retrievers, have lately changed the field of ischemic stroke treatment, since their use—compared to thrombolytic-therapy alone—was associated with improved clinical outcomes [9,10,11,12]. Stent retrievers represent self-expanding nitinol devices. By design, they enable capture and removal of the target thrombus upon device deployment, which permits flow restoration [13]. Stent-based MTDs, in combination with continuous aspiration techniques to omit distal or side branch thrombus embolization, have become the standard of care for ischemic stroke treatment [13]. In this context, the NeVa™ device (Vesalio, USA) has been successfully used for treatment of ischemic strokes [10]. Its successor—the EnVast™ device—has recently been cleared for use in coronary cases with large thrombus burden. Since data about the utility of stent-based MTDs for treatment of AMI cases with LTB is still very limited, we evaluated our early cohort of patients managed with the NeVa™ device.
Methods
Study design
We analyzed consecutive patients from the prospective OPTIMISER (A Prospective Cohort Study to Describe the OPTIMal Management and Outcomes of PatIents PreSEnting With Acute MyocaRdial Infarction) registry (ClinicalTrials.gov Identifier: NCT04988672), who have been treated with the NeVa™ MTD device for AMI with LTB. The study took place at the Heart Center of the Luzerner Kantonsspital (Lucerne, Switzerland), which represents the tertiary cardiology facility of the central part of Switzerland (annual PCI volume > 1700 procedures). The study complied with the Declaration of Helsinki and had been approved by the local ethics committee (BASEC ID 2020-02559). All patients gave their informed consent.
Study population
We analyzed patients presenting with AMI and LTB, defined as Thrombolyis In Myocardial Infarction (TIMI) thrombus grade (TTG) ≥ 3 upon coronary angiography according to the operator´s assessment, who were treated with the NeVa™ MTD as an upfront or bailout approach to re-establish coronary perfusion. We applied no clinical or anatomical exclusion criteria. Following the use of the NeVa™ MTD, patients underwent PCI and received pharmacologic treatment according to international guidelines [14, 15]. From every study participant, demographic and procedural data as well as outcome information were collected in a dedicated database.
Deployment of the NeVa™ mechanical thrombectomy device in coronary cases
The NeVa™ MTD (Vesalio, USA) is a self-expanding nitinol stent attached to a push wire [13]. The design of this MTD is highlighted in Fig. 1. It is equipped with large open pockets (drop zones) distributed along its length, which serve as entry ports for thrombus. The closed distal tip at the end of the device prevents thrombus material of escaping during device removal. There are various sizes and designs available on market. It has received the CE mark approved in 2019 for management of coronary lesions with LTB.
Deployment of the NeVa™ MTD goes as follows: (1) at the beginning of the procedure, a standard 0.014″ coronary guidewire is advanced distal to the thrombotically occluded site. This wire will remain in place during the thrombectomy phase, facilitating access to the infarcted vessel after MTD removal; (2) for the following steps, we have adopted the approach proposed by Spirito et al [13]. Using a parallel wire technique, a Rebar™ 18 130 cm microcatheter (Medtronic, USA) is inserted over a second 0.014″ coronary guidewire and through a 6F guiding catheter extension. By using a parallel wire approach, rapid deployment of a coronary stent might be possible following thrombus removal. After advancement of the microcatheter distal to the occlusion site, the guidewire is withdrawn and the NeVa™ MTD is pushed into the microcatheter until the distal markers are lined up with the microcatheter´s end. The NeVa™ stent retriever should be selected based on the estimated vessel diameter (typically oversized by at least 50%) and occlusion/thrombotic length. It is deployed by fixing the push wire in place and withdrawing the microcatheter in the proximal direction until complete expansion of the device. To avoid thrombus embolization, one needs to ensure that the guiding catheter/guide extension is well intubated. We also apply continuous aspiration, achieved with at least one VacLok 60 ml vacuum pressure syringes (Merit Medical, USA) attached to the side port of the guiding catheter hemostatic valve [13]. Afterwards, one should simultaneously remove the guiding catheter extension and the NeVa™ stent retriever, the initial 0.014″ coronary guidewire is kept in place. This maneuver can be repeated as long as there is thrombus visible in the vessel. In some cases, one might encounter coronary spasm following thrombus retrieval with the NeVa™ device. In those cases, we usually administer nitroglycerine or adenosine. Following usage of the MTD, PCI and stenting, if necessary, is performed according to the operator´s preferences.
Angiographic analyses and outcome assessment
For this study, all angiograms were reviewed by two independent physicians not involved in the PCI procedures (YZ and MM) using a dedicated software package (Intellispace cardiovascular, Phillips, Netherlands). They assessed the TIMI flow and myocardial blush grade (MBG) at baseline, after wire insertion, after treatment with the NeVa™ MTD and at the end of the intervention as well as the occurrence of procedural angiographic complications.
All patients underwent follow-up assessment performed by dedicated study personal (JB and LS). Clinical follow-up was obtained by phone call or outpatient clinic visit at 6 months, 1 and 2 years (if applicable). Efficacy outcomes were TIMI flow and MBG after NeVa™ MTD use. Clinical endpoints of interest included periprocedural complications (coronary dissection, perforation, occlusion, spasm, embolization) or clinical complications (cardiac tamponade, arrhythmias needing treatment), major adverse cardiac and cerebrovascular event (MACCE) defined as composite of cardiovascular death, target vessel myocardial infarction (TV-MI), target lesion revascularization (TLR), target vessel revascularization (TVR), stent thrombosis (ST) and stroke, as suggested by the Academic Research Consortium (ARC) criteria [16].
Statistical analysis
Statistical analyses were primarily descriptive. Categorical variables are displayed as numbers and percentages, and continuous variables are presented as means (± standard deviations, SD) or medians (interquartile ranges, IQR), as appropriate. A p-value < 0.05 was considered statistically significant. Statistical analyses were performed with STATA 17 (StataCorp LCC, Lakeway Drive, Texas, USA).
Results
Study population and baseline characteristics
Between September 2020 and February 2022, 15 patients underwent thrombectomy with the NeVa™ MTD for AMI with LTB. The baseline demographics are displayed in Table 1. In brief, most patients were males (73%), 6 (40%) patients had previous PCI and 2 (13%) had a previous coronary artery bypass graft (CABG) procedure. Overall, 12 (80%) patients presented with an acute ST-segment elevation myocardial infarction (STEMI).
Lesion and procedural characteristics
The lesion and procedural characteristics are summarized in Table 2. Thrombectomy was successfully performed in 14 (93%) patients. In 1 case presenting with very late stent thrombosis, within the left anterior descending (LAD), it was impossible to deliver and deploy the NeVa™ device. The suspected cause for device failure was most likely interaction (friction) with old underlying stent, which showed evidence of under-expansion and underlying calcifications. The culprit lesion was mainly (8, 53%) located in the LAD followed by the right coronary artery (5, 33%). Notably, 2 (13%) cases with AMI were related to thrombotic vein graft occlusion. In 12 (80%) patients, the lesions were additionally treated with last generation drug eluting stents (DES) following thrombectomy. Glycoprotein receptor (GP) IIb/IIIa antagonists were administered in 4 (27%) cases.
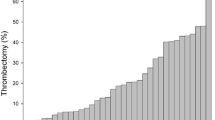
No relevant periprocedural complications (especially no stroke or acute stent thrombosis/vessel closure) were encountered. Final TIMI 3 flow was encountered in 13 (87%) patients (2, 13% patients ended up with TIMI 2 flow) and TIMI thrombus grade 0 was achieved in all patients, see Fig. 2. Figure 3 highlights a case, which was successfully managed using the NeVa™ stent retriever.
Clinical outcomes
The clinical outcomes are summarized in Table 3. After a mean follow-up time of 26 ± 2.9 months, one MACCE was observed. The patient presented with ST 10 months after the index procedure, in this case, we had previously treated the vein graft occlusion with the NeVa™ device. This case is illustrated in Fig. 4.
Case vignette: NSTEMI patient presenting with thrombotic saphenous vein graft occlusion: A Initial angiogram (TIMI 0 flow); B Final result following thrombus retrieval with NeVa™ device; C Target lesion failure (repeat TV-MI) after 10 months initial angiogram (TIMI 0 flow); D Final angiogram after repeat revascularization
Discussion
With regards to the poor outcomes of AMI patients with LTB and their high risk for DTE, there is an unmet need to enhance their interventional management. Stent retrievers might have the potential to bring this field forward.
This is one of the first reports summarizing procedural characteristics and outcomes of an all-comer AMI cohort, which has undergone up-front treatment with a novel stent-based MTD for highly thrombotic coronary lesions. The main findings of this study are as follows: (1) The use of the NeVa™ MTD in AMI with LTB seems safe and the risk for thrombus embolization is probably low; (2) after deployment of this stent-based MTD, immediate reperfusion with TIMI 3 flow and TIMI 0 thrombus grade can be observed in the majority of cases (at least 80%); (3) the use of stent retriever in LTB cases might be associated with favourable long-term outcomes (including low TLF rates); and (4) stent-based MTDs moreover could represent valuable tools to restore flow in thrombotic saphenous vein graft lesions.
Albeit early studies indicated potential benefits with thrombectomy devices in AMI treatment, e.g. reduced risk of DTE, repeat AMI and cardiac death [17,18,19,20,21,22]. Subsequent larger trials did not validate the initially positive signals, but moreover highlighted an increased stroke risk with routine use of MTDs in AMI [8, 23, 24]. The inability to sufficiently grasp and safely evacuate thrombotic material, as seen with most early thrombectomy strategies, may explain to some extent why there was no uniform benefit and even an increased stroke risk with those techniques.
The introduction of stent retriever techniques has revolutionized stroke interventions [9,10,11,12]. In this context, the combined use of balloon guide catheters or continuous aspiration over intermediate catheters and stent-based MTDs has not just proven to be efficient for evacuation of large amounts of thrombus and, therefore, useful for facilitating reperfusion, but this approach also mitigates the risk of thrombus embolization [13, 25].
Several case reports and a recent observational study indicated feasibility and safety of stent based MTDs for treatment of thrombotic coronary lesions [13, 26,27,28,29]. Spirito and colleagues showed very low rates of periprocedural complications and high rates of flow restoration (> 80%) with the use of NeVa™ device in patients presenting with acute coronary syndromes and LTB [13]. Of note, post-PCI MBG in AMI patients with LTB is associated with worse outcomes (e.g. mortality) [30]. In our case series, we found that post-PCI, not only TIMI 0 thrombus grade, but also moreover MBG grade 3, normal myocardial blush or contrast density, was achieved in the majority of cases (87%) managed with the NeVa™ device. In the TOTAL trial, a MBG grade 3 was achieved in 90% of all STEMI patients undergoing manual thrombus aspiration [30]. However, not all of those STEMI patients had evidence of LTB [30].
A modified stent retriever assisted vacuum-locked extraction (SAVE) technique involving the NeVa™ device or its successor the enVast™ device (Vesalio, USA), as recently reported, has the potential to overcome some of the limitations and risks associated with conventional manual or mechanical thrombectomy [13, 31]. Therefore, this approach may minimize the risk thrombus for dislocation from the coronary arteries to the systemic vasculature and thromboembolic strokes [32]. Moreover, the use of intermediate catheters for deployment of stent-based MTDs may reduce the chances for atheroembolic strokes originating from the aorta, which can occur with forced guide catheter manipulation to overcome lesions with some thrombectomy catheters [32].
With regards to the elevated risk for TVR following PCI in AMI, especially in cases with LTB, enhanced thrombus removal, as provided with the NeVa™ device, may facilitate optimal stent implantation (e.g. lower risk for stent under-expansion or geographic miss), which in turn improves long-term outcomes in those patients [33, 34]. Our data, which showed a low TVR rate, seem to point toward this direction.
We all aware of the limitation of the current study. This is an observational single-centre study with a small sample size and no control group, which limits generalizability and makes it impossible to draw any firm inferences. Furthermore, the MTD was used in two PCI scenarios with LTB, meaning upfront to re-establish flow as well as a bail-out strategy in AMI cases, where it was impossible to re-establish flow with established PCI devices. This may limit the interpretation of our results. Also, we did not systematically quantify the amount of thrombus extracted with the NeVa™ device or aspirated with the concomitant manual aspiration, which may have provided additional insights about the efficacy of this approach. Additionally, the small sample size of the studied cohort may not permit drawing any firm inferences with respect to long-term outcomes. Finally, the use of stent based MTDs (or modified SAVE technique) for coronary cases involves a learning curve. This could also have influenced the outcomes of our treated AMI cohort to some extent.
Of note, there are two ongoing randomized trials currently assessing the role of stent-based MTDs in primary PCI for STEMI treatment. The NATURE trial (NCT04969471), compares the effectiveness and safety of the enVast™ device to standard of care in STEMI patients with TIMI Thrombus Grade ≥ 3 in the infarct related artery. In addition, the RETRIEVE-AMI Study (NCT05307965) will determine the role of the Solitaire™ device (Medtronic, USA) in AMI treatment [35]. This study randomizes STEMI patients with TIMI 0 flow at presentation and angiographic thrombus score ≥ 4 in a 1:1:1 fashion to be either treated with stand-alone percutaneous coronary intervention (PCI) (Arm 1), thrombus aspiration plus PCI (Arm 2) or retriever thrombectomy in combination with PCI (Arm 3).[35].
Conclusions
In summary, we studied the performance of the stent based MTD NeVa™ in AMI cases with LTB. For this purpose, we applied a modified stent retriever assisted vacuum-locked extraction (SAVE) technique involving the stent retriever device. We found that this approach seems not just safe, but also efficient and results in a high rate of successful reperfusion in highly thrombotic lesions. Further investigation with dedicated randomized trials are required whether the use of the NeVa™ device in cases with LTB improves procedural outcomes and furthermore translates into improved long-term PCI outcomes. A series of ongoing trials will ultimately define the role of stent-based MTDs in PCI for AMI management.
Data availability
The data may become available upon reasonable request.
Abbreviations
- ACS:
-
Acute coronary syndrome
- AMI:
-
Acute myocardial infarction
- DTE:
-
Distal thrombus embolization
- LTB:
-
Large thrombus burden
- MBG:
-
Myocardial blush grade
- MTD:
-
Mechanical thrombectomy device
- NSTEMI:
-
Non-ST-segment elevation myocardial infarction
- PCI:
-
Percutaneous coronary intervention
- STEMI:
-
ST-segment elevation myocardial infarction
- TLF:
-
Target lesion failure
- TLR:
-
Target lesion revascularisation
- TV-MI:
-
Target vessel myocardial infarction
- TVR:
-
Target vessel revascularization
References
Niccoli G, Burzotta F, Galiuto L, Crea F. Myocardial no-reflow in humans. J Am Coll Cardiol. 2009;54(4):281–92. https://doi.org/10.1016/j.jacc.2009.03.054. (PubMed PMID: 19608025).
Niccoli G, Scalone G, Lerman A, Crea F. Coronary microvascular obstruction in acute myocardial infarction. Eur Heart J. 2016;37(13):1024–33. https://doi.org/10.1093/eurheartj/ehv484. (Epub 20150912 PubMed PMID: 26364289).
Rezkalla SH, Stankowski RV, Hanna J, Kloner RA. Management of no-reflow phenomenon in the catheterization laboratory. JACC Cardiovasc Interv. 2017;10(3):215–23. https://doi.org/10.1016/j.jcin.2016.11.059. (PubMed PMID: 28183461).
de Waha S, Patel MR, Granger CB, Ohman EM, Maehara A, Eitel I, et al. Relationship between microvascular obstruction and adverse events following primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: an individual patient data pooled analysis from seven randomized trials. Eur Heart J. 2017;38(47):3502–10. https://doi.org/10.1093/eurheartj/ehx414. (PubMed PMID: 29020248).
Singh M, Berger PB, Ting HH, Rihal CS, Wilson SH, Lennon RJ, et al. Influence of coronary thrombus on outcome of percutaneous coronary angioplasty in the current era (the Mayo clinic experience). Am J Cardiol. 2001;88(10):1091–6. https://doi.org/10.1016/s0002-9149(01)02040-9. (PubMed PMID: 11703950).
Napodano M, Dariol G, Al Mamary AH, Marra MP, Tarantini G, D’Amico G, et al. Thrombus burden and myocardial damage during primary percutaneous coronary intervention. Am J Cardiol. 2014;113(9):1449–56. https://doi.org/10.1016/j.amjcard.2014.01.423. (Epub 20140212 PubMed PMID: 24630783).
Jolly SS, Cairns JA, Yusuf S, Meeks B, Pogue J, Rokoss MJ, et al. Randomized trial of primary PCI with or without routine manual thrombectomy. N Engl J Med. 2015;372(15):1389–98. https://doi.org/10.1056/NEJMoa1415098. (PubMed PMID: 25853743).
Jolly SS, James S, Džavík V, Cairns JA, Mahmoud KD, Zijlstra F, et al. Thrombus aspiration in ST-segment-elevation myocardial infarction: an individual patient meta-analysis: thrombectomy trialists collaboration. Circulation. 2017;135(2):143–52. https://doi.org/10.1161/circulationaha.116.025371. (Epub 20161209 PubMed PMID: 27941066).
Touma L, Filion KB, Sterling LH, Atallah R, Windle SB, Eisenberg MJ. Stent retrievers for the treatment of acute ischemic stroke: a systematic review and meta-analysis of randomized clinical trials. JAMA Neurol. 2016;73(3):275–81. https://doi.org/10.1001/jamaneurol.2015.4441. (Epub 2016/01/27 PubMed PMID: 26810499).
Maus V, Styczen H, Liman J, Maier I, Brehm A, Tsogkas I, et al. Intracranial mechanical thrombectomy of large vessel occlusions in the posterior circulation using SAVE. BMC Neurol. 2019;19(1):197. https://doi.org/10.1186/s12883-019-1428-x. (Epub 20190816. PubMed PMID: 31419959; PubMed Central PMCID: PMC6696671).
Huo X, Ma G, Tong X, Zhang X, Pan Y, Nguyen TN, et al. Trial of endovascular therapy for acute ischemic stroke with large infarct. N Engl J Med. 2023;388(14):1272–83. https://doi.org/10.1056/NEJMoa2213379. (Epub 20230210 PubMed PMID: 36762852).
Sarraj A, Hassan AE, Abraham MG, Ortega-Gutierrez S, Kasner SE, Hussain MS, et al. Trial of endovascular thrombectomy for large ischemic strokes. N Engl J Med. 2023;388(14):1259–71. https://doi.org/10.1056/NEJMoa2214403. (Epub 20230210 PubMed PMID: 36762865).
Spirito A, Quagliana A, Coiro M, Melaku GD, Vandenberghe S, Leibundgut G, et al. A prospective, first-in-human use of the NeVa mechanical thrombectomy device for patients with acute coronary syndromes. EuroIntervention. 2022;18(3):242–52. https://doi.org/10.4244/eij-d-21-00741. (PubMed PMID:34992050; PubMed Central PMCID:PMC9912965).
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European society of cardiology (ESC). Eur Heart J. 2018;39(2):119–77. https://doi.org/10.1093/eurheartj/ehx393. (PubMed PMID: 28886621).
Neumann FJ, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40(2):87–165. https://doi.org/10.1093/eurheartj/ehy394. (PubMed PMID: 30165437).
Garcia-Garcia HM, McFadden EP, Farb A, Mehran R, Stone GW, Spertus J, et al. Standardized end point definitions for coronary intervention trials: the academic research consortium-2 consensus document. Circulation. 2018;137(24):2635–50. https://doi.org/10.1161/CIRCULATIONAHA.117.029289. (Epub 2018/06/13 PubMed PMID: 29891620).
Antoniucci D, Valenti R, Migliorini A, Parodi G, Memisha G, Santoro GM, et al. Comparison of rheolytic thrombectomy before direct infarct artery stenting versus direct stenting alone in patients undergoing percutaneous coronary intervention for acute myocardial infarction. Am J Cardiol. 2004;93(8):1033–5. https://doi.org/10.1016/j.amjcard.2004.01.011. (PubMed PMID: 15081450).
Svilaas T, Vlaar PJ, van der Horst IC, Diercks GF, de Smet BJ, van den Heuvel AF, et al. Thrombus aspiration during primary percutaneous coronary intervention. N Engl J Med. 2008;358(6):557–67. https://doi.org/10.1056/NEJMoa0706416. (Epub 2008/02/08 PubMed PMID: 18256391).
Vlaar PJ, Svilaas T, van der Horst IC, Diercks GF, Fokkema ML, de Smet BJ, et al. Cardiac death and reinfarction after 1 year in the thrombus aspiration during percutaneous coronary intervention in acute myocardial infarction study (TAPAS): a 1-year follow-up study. Lancet. 2008;371(9628):1915–20. https://doi.org/10.1016/s0140-6736(08)60833-8. (Epub 2008/06/10 PubMed PMID: 18539223).
Ikari Y, Sakurada M, Kozuma K, Kawano S, Katsuki T, Kimura K, et al. Upfront thrombus aspiration in primary coronary intervention for patients with ST-segment elevation acute myocardial infarction: report of the VAMPIRE (VAcuuM asPIration thrombus REmoval) trial. JACC Cardiovasc Interv. 2008;1(4):424–31. https://doi.org/10.1016/j.jcin.2008.06.004. (Epub 2009/05/26 PubMed PMID: 19463340).
Sardella G, Mancone M, Bucciarelli-Ducci C, Agati L, Scardala R, Carbone I, et al. Thrombus aspiration during primary percutaneous coronary intervention improves myocardial reperfusion and reduces infarct size: the EXPIRA (thrombectomy with export catheter in infarct-related artery during primary percutaneous coronary intervention) prospective, randomized trial. J Am Coll Cardiol. 2009;53(4):309–15. https://doi.org/10.1016/j.jacc.2008.10.017. (Epub 2009/01/24 PubMed PMID: 19161878).
Migliorini A, Stabile A, Rodriguez AE, Gandolfo C, Rodriguez Granillo AM, Valenti R, et al. Comparison of AngioJet rheolytic thrombectomy before direct infarct artery stenting with direct stenting alone in patients with acute myocardial infarction. The JETSTENT trial. J Am Coll Cardiol. 2010;56(16):1298–306. https://doi.org/10.1016/j.jacc.2010.06.011. (Epub 2010/08/10 PubMed PMID: 20691553).
Fröbert O, Lagerqvist B, Olivecrona GK, Omerovic E, Gudnason T, Maeng M, et al. Thrombus aspiration during ST-segment elevation myocardial infarction. N Engl J Med. 2013;369(17):1587–97. https://doi.org/10.1056/NEJMoa1308789. (PubMed PMID: 23991656).
Jolly SS, Cairns JA, Yusuf S, Rokoss MJ, Gao P, Meeks B, et al. Outcomes after thrombus aspiration for ST elevation myocardial infarction: 1-year follow-up of the prospective randomised TOTAL trial. Lancet. 2016;387(10014):127–35. https://doi.org/10.1016/s0140-6736(15)00448-1. (Epub 2015/10/18. PubMed PMID: 26474811; PubMed Central PMCID: PMC5007127).
Chueh JY, Puri AS, Wakhloo AK, Gounis MJ. Risk of distal embolization with stent retriever thrombectomy and ADAPT. J Neurointerv Surg. 2016;8(2):197–202. https://doi.org/10.1136/neurintsurg-2014-011491. (Epub 20141224. PubMed PMID: 25540180; PubMed Central PMCID: PMC4752657).
Patel N, Badiye A, Yavagal DR, Mendoza CE. Stent-based mechanical thrombectomy in left main coronary artery thrombus presenting as ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2017;10(3):302–3. https://doi.org/10.1016/j.jcin.2016.10.038. (Epub 2017/01/23. PubMed PMID: 28109870).
Bhoopalan K, Rajendran R, Alagarsamy S, Kesavamoorthy N. Successful extraction of refractory thrombus from an ectatic coronary artery using stent retriever during primary angioplasty for acute myocardial infarction: a case report. Eur Heart J Case Rep. 2019;3(1):yty161. https://doi.org/10.1093/ehjcr/yty161. (Epub 2019/04/26. PubMed PMID: 31020237; PubMed Central PMCID: PMC6439382).
Crimi G, Moramarco L, Mandurino-Mirizzi A, Quaretti P, Ferrario M. The combined use of stent retriever and neuro-aspiration as successful bail-out reperfusion strategy in a patient with embolic myocardial infarction. Catheter Cardiovasc Interv. 2019;94(2):E78–81. https://doi.org/10.1002/ccd.28167. (Epub 2019/03/10. PubMed PMID: 30851080).
Bongiovanni D, Loizzi F, Landi A, Utsch L, Araco M, Joner M, et al. EnVast mechanical thrombectomy after thrombus aspiration failure in a STEMI with a massive thrombotic burden. JACC Cardiovasc Interv. 2023;16(1):112–5. https://doi.org/10.1016/j.jcin.2022.09.050. (Epub 2023/01/05. PubMed PMID: 36599578).
Sharma V, Jolly SS, Hamid T, Sharma D, Chiha J, Chan W, et al. Myocardial blush and microvascular reperfusion following manual thrombectomy during percutaneous coronary intervention for ST elevation myocardial infarction: insights from the TOTAL trial. Eur Heart J. 2016;37(24):1891–8. https://doi.org/10.1093/eurheartj/ehw157. (Epub 20160428. PubMed PMID: 27125948; PubMed Central PMCID: PMC4917747).
Maus V, Behme D, Kabbasch C, Borggrefe J, Tsogkas I, Nikoubashman O, et al. Maximizing first-pass complete reperfusion with SAVE. Clin Neuroradiol. 2018;28(3):327–38. https://doi.org/10.1007/s00062-017-0566-z. (Epub 2017/02/15 PubMed PMID: 28194477).
Jolly SS, Cairns JA, Yusuf S, Meeks B, Gao P, Hart RG, et al. Stroke in the TOTAL trial: a randomized trial of routine thrombectomy vs. percutaneous coronary intervention alone in ST elevation myocardial infarction. Eur Heart J. 2015;36(35):2364–72. https://doi.org/10.1093/eurheartj/ehv296. (Epub 2015/07/02. PubMed PMID: 26129947; PubMed Central PMCID: PMC4568405).
Prati F, Romagnoli E, Gatto L, La Manna A, Burzotta F, Limbruno U, et al. Clinical impact of suboptimal stenting and residual intrastent plaque/thrombus protrusion in patients with acute coronary syndrome: the CLI-OPCI ACS substudy (Centro per la Lotta Contro L’Infarto-optimization of percutaneous coronary intervention in acute coronary syndrome). Circ Cardiovasc Interv. 2016. https://doi.org/10.1161/circinterventions.115.003726. (PubMed PMID: 27965297).
Kitahara H, Okada K, Kimura T, Yock PG, Lansky AJ, Popma JJ, et al. Impact of Stent size selection on acute and long-term outcomes after drug-eluting stent implantation in de novo coronary lesions. Circ Cardiovasc Interv. 2017. https://doi.org/10.1161/circinterventions.116.004795. (PubMed PMID: 28951394).
Kotronias RA, Marin F, Emfietzoglou M, Langrish JP, Lucking AJ, Channon KM, et al. Rationale and Design of a randomized controlled pilot trial to assess stent retriever thrombectomy for thrombus burden reduction in patients with acute myocardial infarction: the RETRIEVE-AMI study. Cardiovasc Revasc Med. 2023;52:75–85. https://doi.org/10.1016/j.carrev.2023.02.012. (Epub 2023/03/10. PubMed PMID: 36894360).
Acknowledgements
Not applicable.
Funding
Open access funding provided by University of Luzern. The authors received no funding for this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
AA has received consulting and speaker fees from SIS Medical. MB has received consulting and speaker fees from Abbott Vascular, Abiomed, Amarin, Amgen, Astra Zeneca, Bayer, Daichii, MedAlliance, Mundipharma, Novartis, OMpharma, SIS Medical and Vifor. FC has received consulting and speaker fees from Abbott Vascular, Abiomet and SIS Medical. All other authors report no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zhi, Y., Madanchi, M., Cioffi, G.M. et al. Initial experience with a novel stent-based mechanical thrombectomy device for management of acute myocardial infarction cases with large thrombus burden. Cardiovasc Interv and Ther 39, 262–272 (2024). https://doi.org/10.1007/s12928-024-00998-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-024-00998-3