Abstract
In patients with ST segment elevation and non-ST elevation myocardial infarction (MI), multivessel (MV) coronary artery disease is found in approximately 50%, leading to worse clinical outcomes. Recent data have suggested that complete revascularization with MV percutaneous coronary intervention is associated with a reduced risk of major adverse cardiovascular events as compared to culprit vessel-only revascularization. However, the optimal timing of MV intervention, appropriate non-culprit lesion assessment, and the best revascularization strategy in specific subsets such as cardiogenic shock remain to be established. This review article summarizes current evidence on revascularization strategies in patients with acute MI and MV disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite recent advances in pharmacological treatment and interventional technologies, acute myocardial infarction (MI) represents one of the leading causes of mortality and morbidity worldwide [1, 2]. Percutaneous coronary intervention (PCI) of the culprit vessel has become a standard-of-care procedure to improve clinical outcomes in patients with acute MI [3,4,5]. In a substantial proportion of patients with acute MI, however, coronary atherosclerosis is not limited to single vessel, and multivessel (MV) coronary artery disease (CAD) is found in approximately 50% in a setting of acute MI, including ST segment elevation myocardial infarction (STEMI) and non-ST segment elevation myocardial infarction (NSTEMI) [6, 7]. Patients with MV CAD rather than those with single-vessel CAD have an increased risk of ischemic events after acute MI, probably because of coronary plaque instability, impaired myocardial perfusion and contractility in non-infarct areas, and greater comorbidities [8, 9]. In this context, the concept of “complete revascularization”, the absence of residual epicardial CAD after treatment, has emerged and been established as a superior therapeutic strategy over culprit vessel-only PCI in patients with STEMI, although “complete revascularization” depends on various definitions including assessment with coronary angiography, non-invasive stress tests, and invasive physiological testing [10]. In addition to the evaluation of non-infarct related vessels, the optimal timing to perform PCI and revascularization strategies in specific subsets such as cardiogenic shock (CS) and NSTEMI have been subject to controversies [11]. This review article provides a practical overview on the current evidence of revascularization strategies in patients with acute MI complicated by MV CAD.
Prognostic impact of complete revascularization
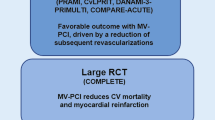
In patients presenting with STEMI within 12 h from symptom onset, primary PCI to achieve recanalization of the culprit lesion is recommended for the improvement of patient’s symptoms and prognosis [5]. Once the culprit lesion has been recanalized, complete revascularization should be considered in patients with acute MI and MV CAD. Previous observational studies have reported conflicting results for the comparison of culprit-only versus MV PCI [11], while several randomized controlled trials (RCTs) have shown the beneficial effect of PCI in the non-infarct-related vessels. Table 1 lists pivotal multi-center RCTs, in which culprit vessel-only PCI was compared with complete revascularization by PCI in patients with STEMI and MV CAD. The PRAMI trial was done in the UK and enrolled a total of 465 patients with STEMI complicated by MV CAD [12]. Patients were randomly allocated to either no further PCI (n = 231) or to undergo immediate MV PCI (n = 234) for the culprit and non-culprit vessels during the index procedure. The trial recruitment was prematurely terminated for efficacy. The primary composite endpoint of cardiac death, non-fatal MI, or refractory angina occurred in 21 (9.0%) and 53 (22.9%) patients in the MV primary PCI and culprit vessel-only PCI groups, respectively (p < 0.001) [12]. The incidence of composite of cardiac death and MI was also lower in the MV PCI group (4.7% vs. 11.7%, p = 0.004) (Table 1). The PRAMI trial compellingly demonstrated the benefit of preventive PCI in patients with STEMI and MV CAD, in which non-culprit lesions were left untreated in the culprit vessel-only PCI group even if very severely stenosed. The subsequent CvLPRIT, DANAMI-3-PRIMULTI, and COMPARE-ACUTE trials have similarly showed the effect of MV PCI in reducing major cardiovascular events [13,14,15], although the rates of all-cause or cardiovascular death and MI did not differ significantly between the two revascularization strategies in each trial (Table 1). The COMPLETE trial, which had a considerably larger sample size than the previous RCTs, confirmed the benefit of complete revascularization in patients with STEMI and MV CAD [16]. In this international RCT, a total of 4041 patients from 140 centers in 31 countries were included and were randomized to either complete revascularization with MV PCI of angiographically significant non-culprit lesions or no further revascularization. At a median follow-up of 3 years, the primary outcome of cardiovascular death or MI occurred in 7.8% and 10.5% in the complete revascularization and culprit vessel-only PCI groups (p = 0.004) [16]. A sub-analysis of the COMPLETE trial demonstrated that approximately 50% of patients with STEMI and MV CAD had at least one obstructive non-culprit lesion containing complex vulnerable plaque among patients undergoing intracoronary optical coherence tomography imaging [17]. This finding may explain the underlying mechanism of benefit of routine PCI of non-culprit lesions in patients with STEMI. After the publication of COMPLETE trial, several meta-analyses have consistently showed the superiority of complete revascularization with MV PCI over culprit vessel-only PCI in the reduction of hard clinical events including cardiovascular death and MI in patients with STEMI and MV CAD, without significantly increased risks of stroke, major bleeding, and kidney injury [18,19,20]. Another sub-analysis of the COMPLETE trial showed that complete revascularization resulted in a greater proportion of patients being angina-free as compared with culprit vessel-only PCI [21]. Taken together, the recent US guidelines for coronary artery revascularization strongly recommend PCI of a significant non-infarct artery stenosis after successful primary PCI of the culprit vessel, to reduce the risk of death or MI in this patient population (Class I, level of evidence A) [5]. Elective coronary artery bypass grafting (CABG) after primary PCI may be also reasonable to improve clinical outcomes in selected patients with STEMI and complex MV CAD [5]. Thus, the next step is to explore the evidence on the optimal evaluating system for non-culprit lesions and timing of MV revascularization, and different subsets of MI including NSTEMI and those complicated by CS. A proposed algorithm of revascularization strategies in patients with acute MI and MV CAD is displayed in Fig. 1.
Schematic algorism of revascularization strategies in patients with acute MI and MV CAD. CABG coronary artery bypass grafting; CAD coronary artery disease; CS cardiogenic shock; MI myocardial infarction; MV multivessel; NSTEMI non-ST segment elevation myocardial infarction; PCI percutaneous coronary intervention; STEMI ST segment elevation myocardial infarction
Non-culprit vessel assessment
The definition of complete revascularization and evaluating system for non-culprit lesions varies widely among studies, based on angiographic percentage of diameter stenosis (%DS) on visual estimation or quantitative coronary angiography, non-invasive stress tests, and invasive physiological testing such as fractional flow reserve (FFR) [10]. Furthermore, intracoronary imaging guidance may be an alternative to coronary physiological testing [22]. In the major RCTs listed in Table 1, non-culprit lesions were defined by %DS on angiography (cut-off values of 50% or 70%) with or without FFR values. Caution is warranted that only < 1% of patients underwent FFR for non-culprit lesion assessment in the COMPLETE trial, and thus, it can be recognized as a study of no FFR [16]. Whether additional FFR measurement for evaluating the severity of non-culprit lesions in acute MI would convey a clinical benefit remains unclear. Before the publication of COMPLETE trial, a meta-analysis indicated that angiographic visual estimation alone was superior to angiographic assessment with FFR as a guide of complete revascularization in reducing cardiac death and MI in patients with STEMI and MV CAD [23]. Even though early studies showed reliability and consistency of FFR during acute phase of MI and thereafter [24], hyperemic reaction is impaired in the culprit and non-culprit vessels in an acute MI setting due to multiple underlying mechanisms, such as myocardial necrosis, hemorrhagic microvascular injury, compensatory hyperkinesis, and neurohumoral vasoconstriction [25]. Indeed, FFR in non-culprit vessels was reported to significantly decrease from acute phase to 1-month follow-up after STEMI [26].
The FLOWER-MI trial tested the potential advantage of complete revascularization guided by FFR in STEMI with MV CAD, randomizing patients to either complete revascularization guided by angiography alone (n = 577) or angiography plus FFR (n = 586) [27]. The proportion of patients undergoing PCI of non-culprit vessels (66.2% vs. 97.1%) were lower, and the number of coronary stents implanted for non-culprit lesions (1.01 ± 0.99 vs. 1.50 ± 0.86) was fewer in the FFR-guided group than in the angiography-guided group. At 1 year, the primary outcome event of a composite of death, MI, or unplanned urgent revascularization occurred in 5.5% and 4.2% in the FFR- and angiography-guided groups (p = 0.31), failing to demonstrate the superiority of FFR guidance [27]. Meta-analyses following the publication of COMPLETE and FLOWER-MI trials demonstrated no superiority of FFR guidance over angiography alone when performing complete revascularization, and even angiographic guidance was non-significantly associated with a lower risk of unplanned revascularization in patients with STEMI and MV CAD [28, 29]. Given that FFR often underestimate the severity of non-culprit lesions in an acute setting of STEMI [26], underutilization of angiographically complete revascularization may deteriorate the prognosis. The recently reported FRAME-AMI trial included patients with both STEMI and NSTEMI complicated by MV CAD (n = 562), which had been terminated early with a small sample size than planned because of the COVID-19 pandemic [30]. In this study, the FFR-guided complete revascularization strategy was associated with a reduced risk of major adverse cardiac events, a composite of death, MI, or repeat revascularization, as compared to the angiography-guided MV PCI. Interestingly, although not statistically significant, the benefit of FFR-guided complete revascularization was more evident in patients with NSTEMI rather than STEMI [30], suggesting the potential disadvantage of FFR in STEMI and possible advantage in NSTEMI. A sub-analysis of the COMPLETE trial simply showed that in the more severe non-culprit lesions on angiography, the more beneficial effect of MV PCI was achieved, with the cut-off value of %DS of 60% on core laboratory assessment [31]. Therefore, among patients with STEMI and MV CAD, simple angiographic evaluation to decide whether performing revascularization of non-culprit lesions may be reasonable, while the potential advantage of FFR-guided MV PCI in NSTEMI population deserves further investigations.
Other assessment strategies on non-culprit lesions than coronary angiography and FFR include non-invasive stress tests and non-hyperemic pressure ratio (NHPR) in patients with acute MI and MV CAD. However, a few studies have examined these strategies. The 2017 ESC guidelines allowed non-invasive stress tests during hospital stay after primary PCI to evaluate myocardial ischemia and viability (Class IIb, level of evidence C) in patients with STEMI [32]. A consensus document by the Japanese Association of Cardiovascular Intervention and Therapeutics suggests the use of physiological evaluation following acute MI, such as FFR, NHPR, and quantitative flow ratio before staged PCI in non-culprit vessels [33]. Given that instantaneous wave-free ratio (iFR), one of NHPRs, was shown not to be altered in a setting of STEMI and in the follow-up evaluation [26, 34], acute NHPR assessment during the index procedure for MI might be considered. In this context, the randomized iMODERN trial will compare the two treatment strategies in patients with STEMI and MV CAD, (1) an active treatment arm with complete, iFR-guided revascularization of non-infarct coronary lesions with %DS > 50% during the primary PCI procedure when iFR ≤ 0.89; and (2) a deferred treatment arm, in which patients undergo stress perfusion cardiac magnetic resonance imaging within 6 weeks after STEMI, with revascularization of the non-culprit lesions when associated perfusion defects are found (Table 2) [35]. Despite the lack of angiography-guided control arm, the iMODERN trial will shed light on non-culprit lesion assessment guided by NHPR and non-invasive stress tests in patients with acute MI and MV CAD [35].
Immediate vs. staged multivessel revascularization
When performing complete revascularization in acute MI, the optimal timing of non-culprit vessel PCI has been a matter of debate. Non-culprit lesions can be revascularized either immediately during the primary procedure or by a staged procedure, unless the patient is indicated for CABG according to the heart team decision. Early intervention for non-culprit lesions has a potential to reduce major clinical events in an acute phase of MI during which patients are at an increased thrombotic risk [36, 37], while immediate complete revascularization is likely to lead to poor assessment of lesion severity of non-culprit vessels, prolonged procedure time, and an increased contrast volume, reportedly resulting in a higher complication rate in MV PCI during the primary procedure [36]. Although a few large-scale RCTs have been reported, the SMILE trial randomized patients with NSTEMI and MV CAD who were planned to undergo an early invasive strategy within 24 h either to immediate MV PCI during the index procedure or to culprit vessel-only PCI, followed by staged revascularization [38]. The primary outcome events, a composite of cardiac death, MI, rehospitalization for unstable angina, repeat revascularization, and stroke occurred in 13.6% and 23.2% in the immediate MV PCI and multistage PCI groups (p = 0.004). Although the SMILE investigators concluded that immediate MV PCI was the better approach than multistage PCI in patients with NSTEMI complicated by MV CAD [38], the results should be interpreted with caution, because the rate of repeat revascularization in the multistage PCI group was unprecedentedly high in the current era (15.4% at 1 year), and the event rates unexpectedly start to diverge after 6 months [11]. A meta-analysis including four RCTs, one of which was the SMILE trial, indicated a trend toward lower risks of mortality and major adverse cardiovascular events in patients with acute coronary syndrome (ACS) undergoing single-stage rather than multistage complete revascularization, despite the lack of statistical significance [39]. Another updated meta-analysis showed that both immediate and staged complete revascularization strategies in patients with STEMI were associated with a lower risk of cardiovascular death or MI in a similar magnitude as compared with culprit vessel-only PCI [40]. The latest guidelines recommend staged PCI of non-culprit lesions (Class I, level of evidence A), but immediate complete revascularization at the time of primary PCI may be also considered in selected STEMI patients when feasible and safe (Class IIb, level of evidence B) [5]. A sub-analysis of the COMPLETE trial, in which patients in the complete revascularization group underwent staged PCI procedures within 45 days either during or after the index hospitalization, demonstrated that the benefit of MV PCI over culprit vessel-only PCI was consistent regardless of the operator-determined timing of non-culprit vessel intervention in patients with STEMI [41]. Therefore, it is conceivable that complete revascularization should be achieved within 45 days with immediate or staged PCI procedures (during or after the index hospitalization) in acute MI patients with MV CAD.
STEMI versus NSTEMI
A body of evidence in terms of complete revascularization in acute MI has accumulated in patients with STEMI, while data are scarce in those with NSTEMI complicated by MV CAD. Although approximately 50% of patients with NSTEMI have MV CAD as seen in STEMI [6], the clinical benefit of complete revascularization has not been established in patients presenting with ACS when ST segment is not elevated. Even though guideline recommendations are mostly in the same direction between STEMI and NSTEMI with MV CAD [42], careful interpretation should be warranted when extrapolating the results of STEMI trials in patients with NSTEMI. An immediate or early invasive strategy may be considered among NSTEMI patients, despite the lack of established survival benefit [43]. In previous observational studies, complete revascularization with MV PCI, relative to culprit vessel-only PCI, was associated with better clinical outcomes in patients with NSTEMI [6, 44,45,46]. For instance, a large-scale UK registry indicated that complete revascularization appears to be superior to culprit vessel-only PCI in long-term morality upon multivariable analyses in patients with NSTEMI and MV CAD [6]. These observational data support the need for further RCTs to confirm the potential benefit of complete revascularization in NSTEMI.
In a setting of NSTEMI, CABG may be more likely to become a choice of means of complete revascularization than in STEMI. However, comparative effectiveness of PCI and CABG in patients with NSTEMI and MV CAD also remains uncertain, because no RCTs have exclusively investigated the patient population. A propensity-matched analysis of the ACUITY trial demonstrated lower rates of stroke, MI, major bleeding, and kidney injury during a peri-procedural period but more frequent repeat revascularization during follow-up in non-ST segment elevation ACS (NSTEACS) patients treated with PCI as compared to CABG-treated patients, with statistically similar mortality at 1 year [47]. A meta-analysis in which 1246 NSTEACS patients with left main or MV CAD were included from three RCTs comparing CABG with PCI as a coronary revascularization strategy showed that the risk of death, MI, and stroke at 5 years was lower in the CABG group than in the PCI group (13.4% vs. 18.0%, p = 0.04), mainly driven by a reduction in MI rates with CABG (3.8% vs. 7.5%, p = 0.006) [48]. Of note, however, most of patients included in this meta-analysis was presented with unstable angina (93.8%) rather than NSTEMI (6.2%) [48]. In another recent meta-analysis including mostly stable MV CAD populations, CABG was associated with lower long-term mortality as compared to PCI, especially in patients with diabetes [49]. Taken together, the evidence is limited to support one revascularization strategy over the other in patients with NSTEMI, and thus, the mode of revascularization, PCI and/or CABG, should be considered based on coronary lesion complexity and the patient’s risk profile [50].
Cardiogenic shock
In a setting of acute MI, 5–10% of patients present with CS, with higher incidence in STEMI compared to NSTEMI [51,52,53]. CS is a life-threatening condition characterized by systemic hypoperfusion due to primary cardiac dysfunction and an inadequate cardiac output [54]. Even in the current era, in-hospital mortality in patients with acute MI remains high at 40–60% when complicated by CS [51,52,53]. Emergency revascularization with PCI or CABG improves long-term survival in patients with acute MI and CS as shown in the SHOCK trial and is recommended in the guidelines [42, 55]. Although MV PCI has been increasingly used as the revascularization strategy in acute MI and CS [52, 56, 57], previous observational studies have indicated conflicting results. Some reports showed a possible benefit of MV PCI in reducing mortality [56, 58], while MV PCI was associated with a greater risk of in-hospital complication and no survival benefit in another registry [57]. In this context, the randomized CULPRIT-SHOCK trial demonstrated that among patients with CS complicating acute MI and MV CAD (> 50% underwent resuscitation before PCI), immediate MV PCI including intervention of chronic total occlusion (CTO) during the primary procedure was associated with higher mortality at 30 days (51.6% vs. 43.3%, p = 0.03) and at 1 year (56.9% vs. 50.0%) as compared to culprit vessel-only PCI [59, 60]. Several limitations of the CULPRIT-SHOCK trial should be noted that 12.5% of patients randomized to the culprit vessel-only PCI group underwent immediate MV revascularization (i.e., cross-over phenomenon) and an additional 17.7% received staged MV PCI procedures [56, 60]. In addition, > 20% of patients had at least one coronary CTO in non-culprit vessels in the CULPRIT-SHOCK trial, among whom immediate CTO recanalization was attempted in roughly 50% and was successful in only approximately one-third of attempts [61]. Although sub-group analyses on CTO and coronary complexity using the SYNTAX score did not show significant interactions between the tested revascularization strategies [60, 62], caution should be warranted. Nevertheless, the CULPRIT-SHOCK trial provided compelling data, and the guidelines was updated to indicate that routine revascularization of lesions in the non-infarct-related vessels is not recommended during primary PCI [42]. Thus, in a setting of acute MI complicated by CS, immediate complete revascularization should be avoided in most cases, while staged MV revascularization may be considered in individual patients.
Acute MI is the most common scenario of CS, accounting for up to 80% of etiologies [63]. Temporary mechanical circulatory support (MCS) devices may play important roles in patients with acute MI and CS, especially when performing coronary revascularization in those having MV CAD. MCS devices, such as extracorporeal membrane oxygenation (ECMO), intra-aortic balloon pumping (IABP), and intravascular microaxial left-ventricular assist device (Impella, Abiomed, Danvers, USA), are useful for hemodynamic support. Yet, whether these devices truly convey clinical benefits (e.g., reduced mortality) remains uncertain. ECMO-facilitated resuscitation might be superior to standard advanced cardiac life support treatment according to the single-center, proof-of-concept ARREST trial results (n = 30) [64]. However, the recent multi-center ECMO-CS trial (n = 117) showed that among patients with either rapidly deteriorating or severe CS (65.0% had acute MI as an etiology of CS), immediate implementation of ECMO was not associated with a reduced risk of mortality at 30 days as compared to the early conservative therapy group (50.0% vs. 47.5%) [65]. The routine use of IABP in patients with acute MI and CS failed to show better outcomes in the IABP Shock II trial [66, 67]. With the superior profile in hemodynamic support over IABP [68], the Impella has emerged in clinical practice. Despite the limited guideline recommendations, the use of Impella in patients with acute MI complicated by CS has been increasing in clinical practice [69,70,71,72]. While some observational studies showed favorable outcomes with the Impella use [73,74,75], plenty of registry data have demonstrated no clinical advantage of Impella over IABP with even higher complication rates, medical cost, and mortality [69,70,71, 76, 77]. In the IMPRESS trial, a small sample size RCT (n = 48), there was no differences in short- and long-term mortality between acute MI patients complicated by CS treated with the Impella and IABP [78, 79]. Additionally, as an adjunctive device with ECMO, the Impella rather than IABP was associated with an increased risk of major bleeding and renal injury in an international ECMO registry [80]. Thus, the results from adequately powered RCTs such as the DanGer Shock (n = 316) (NCT01633502), RECOVER IV (n = 560) (NCT05506449), and DTU-STEMI (n = 668) (NCT03947619) trials are eagerly awaited [81].
Ongoing trials
To fill the evidence gap, numerous RCTs are ongoing (Table 2). The benefit of complete revascularization as compared with culprit vessel-only PCI will be further tested in the FULL REVASC and FIRE trials in patients with STEMI and NSTEMI. The primary interest of the FRAME-AMI trial and a Chinese study by Chen et al. are clinical implications of coronary physiology guidance in patients with acute MI. The optimal timing for PCI of non-culprit lesions will be unveiled in the ASSIST-MI, BIOVASC, STAGED, MULTISTARS-AMI, TERMINAL, OPTION-NSTEMI, MILESTONE, and OPTION-STEMI trials in patients with STEMI and NSTEMI complicated by MV CAD. Interestingly, the MILESTONE trial addresses the potential non-inferiority of PCI to CABG in patients with NSTEACS and MV CAD (Table 2). These studies will improve the current limited knowledge in revascularization strategies in patients with acute MI and MV CAD.
Conclusions
Complete revascularization, the elimination of significant residual epicardial CAD, should be considered in patients with acute MI and MV CAD to improve clinical outcomes, when feasible and applicable. Although optimal timing of MV revascularization, appropriate non-culprit lesion assessment, and the evidence gap in specific subsets including NSTEMI and CS remain to be elucidated, future studies will shape our understanding in this rapidly progressing field of interventional cardiology.
Data availability
Not applicable.
References
Puymirat E, Simon T, Cayla G, et al. Acute myocardial infarction: changes in patient characteristics, management, and 6-month outcomes over a period of 20 years in the FAST-MI program (French Registry of Acute ST-Elevation or Non-ST-Elevation Myocardial Infarction) 1995 to 2015. Circulation. 2017;136:1908–19.
GBD 2013 Mortality and Causes of Death Collaborators. Global, regional, and national age–sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2013;385:117–71.
Ozaki Y, Hara H, Onuma Y, et al. CVIT expert consensus document on primary percutaneous coronary intervention (PCI) for acute myocardial infarction (AMI) update 2022. Cardiovasc Interv Ther. 2022;37:1–34.
Chacko L, Howard PJ, Rajkumar C, et al. Effects of percutaneous coronary intervention on death and myocardial infarction stratified by stable and unstable coronary artery disease: a meta-analysis of randomized controlled trials. Circ Cardiovasc Qual Outcomes. 2020;13:e006363.
Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022;145:e18-114.
Rathod KS, Koganti S, Jain AK, et al. Complete versus culprit-only lesion intervention in patients with acute coronary syndromes. J Am Coll Cardiol. 2018;72:1989–99.
Park DW, Clare RM, Schulte PJ, et al. Extent, location, and clinical significance of non-infarct-related coronary artery disease among patients with ST-elevation myocardial infarction. JAMA. 2014;312:2019–27.
Sorajja P, Gersh BJ, Cox DA, et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. 2007;28:1709–16.
Bates ER, Tamis-Holland JE, Bittl JA, et al. PCI strategies in patients with ST-segment elevation myocardial infarction and multivessel coronary artery disease. J Am Coll Cardiol. 2016;68:1066–81.
Gaba P, Gersh BJ, Ali ZA, et al. Complete versus incomplete coronary revascularization: definitions, assessment and outcomes. Nat Rev Cardiol. 2021;18:155–68.
Saito Y, Kobayashi Y. Percutaneous coronary intervention strategies in patients with acute myocardial infarction and multivessel disease: completeness, timing, lesion assessment, and patient status. J Cardiol. 2019;74:95–101.
Wald DS, Morris JK, Wald NJ, et al. Randomized trial of preventive angioplasty in myocardial infarction. N Engl J Med. 2013;369:1115–23.
Gershlick AH, Khan JN, Kelly DJ, et al. Randomized trial of complete versus lesion-only revascularization in patients undergoing primary percutaneous coronary intervention for STEMI and multivessel disease: the CvLPRIT trial. J Am Coll Cardiol. 2015;65:963–72.
Engstrøm T, Kelbæk H, Helqvist S, et al. Complete revascularisation versus treatment of the culprit lesion only in patients with ST-segment elevation myocardial infarction and multivessel disease (DANAMI-3—PRIMULTI): an open-label, randomised controlled trial. Lancet. 2015;386:665–71.
Smits PC, Abdel-Wahab M, Neumann FJ, et al. Fractional flow reserve-guided multivessel angioplasty in myocardial infarction. N Engl J Med. 2017;376:1234–44.
Mehta SR, Wood DA, Storey RF, et al. Complete revascularization with multivessel PCI for myocardial infarction. N Engl J Med. 2019;381:1411–21.
Pinilla-Echeverri N, Mehta SR, Wang J, et al. Nonculprit lesion plaque morphology in patients with ST-segment-elevation myocardial infarction: results from the COMPLETE trial optical coherence tomography substudys. Circ Cardiovasc Interv. 2020;13: e008768.
Levett JY, Windle SB, Filion KB, et al. Meta-analysis of complete versus culprit-only revascularization in patients with ST-segment elevation myocardial infarction and multivessel coronary disease. Am J Cardiol. 2020;135:40–9.
Ahmad Y, Howard JP, Arnold A, et al. Complete revascularization by percutaneous coronary intervention for patients with ST-segment-elevation myocardial infarction and multivessel coronary artery disease: an updated meta-analysis of randomized trials. J Am Heart Assoc. 2020;9: e015263.
Bainey KR, Engstrom T, Smits PC, et al. Complete vs culprit-lesion-only revascularization for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. JAMA Cardiol. 2020;5:881–8.
Mehta SR, Wang J, Wood DA, et al. Complete revascularization vs culprit lesion-only percutaneous coronary intervention for angina-related quality of life in patients with ST-segment elevation myocardial infarction: results from the COMPLETE randomized clinical trial. JAMA Cardiol. 2022;7:1091–9.
Koo BK, Hu X, Kang J, et al. Fractional flow reserve or intravascular ultrasonography to guide PCI. N Engl J Med. 2022;387:779–89.
Wald DS, Hadyanto S, Bestwick JP. Should fractional flow reserve follow angiographic visual inspection to guide preventive percutaneous coronary intervention in ST-elevation myocardial infarction? Eur Heart J Qual Care Clin Outcomes. 2020;6:186–92.
Ntalianis A, Sels JW, Davidavicius G, et al. Fractional flow reserve for the assessment of nonculprit coronary artery stenoses in patients with acute myocardial infarction. JACC Cardiovasc Interv. 2010;3:1274–81.
de Waard GA, Hollander MR, Teunissen PF, et al. Changes in coronary blood flow after acute myocardial infarction: insights from a patient study and an experimental porcine model. JACC Cardiovasc Interv. 2016;9:602–13.
van der Hoeven NW, Janssens GN, de Waard GA, et al. Temporal changes in coronary hyperemic and resting hemodynamic indices in nonculprit vessels of patients With ST-segment elevation myocardial infarction. JAMA Cardiol. 2019;4:736–44.
Puymirat E, Cayla G, Simon T, et al. Multivessel PCI guided by FFR or angiography for myocardial infarction. N Engl J Med. 2021;385:297–308.
Okuya Y, Gohil K, Moussa ID. Angiography versus FFR guided complete revascularization versus culprit-only revascularization for patients presenting with STEMI: network meta-analysis. Catheter Cardiovasc Interv. 2022;100:340–50.
Elbadawi A, Dang AT, Hamed M, et al. FFR-versus angiography-guided revascularization for nonculprit stenosis in STEMI and multivessel disease: a network meta-analysis. JACC Cardiovasc Interv. 2022;15:656–66.
Lee JM, Kim HK, Park KH, et al. Fractional flow reserve versus angiography-guided strategy in acute myocardial infarction with multivessel disease: a randomized trial. Eur Heart J. 2022. https://doi.org/10.1093/eurheartj/ehac763.
Sheth T, Pinilla-Echeverri N, Moreno R, et al. Nonculprit lesion severity and outcome of revascularization in patients with STEMI and multivessel coronary disease. J Am Coll Cardiol. 2020;76:1277–86.
Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–77.
Kawase Y, Matsuo H, Kuramitsu S, et al. Clinical use of physiological lesion assessment using pressure guidewires: an expert consensus document of the Japanese association of cardiovascular intervention and therapeutics-update 2022. Cardiovasc Interv Ther. 2022;37:425–39.
Thim T, Gotberg M, Frobert O, et al. Nonculprit stenosis evaluation using instantaneous wave-free ratio in patients with ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2017;10:2528–35.
Beijnink CWH, Thim T, van der Heijden DJ, et al. Instantaneous wave-free ratio guided multivessel revascularisation during percutaneous coronary intervention for acute myocardial infarction: study protocol of the randomised controlled iMODERN trial. BMJ Open. 2021;11: e044035.
Bagai A, Thavendiranathan P, Sharieff W, et al. Non-infarct-related artery revascularization during primary percutaneous coronary intervention for ST-segment elevation myocardial infarction: a systematic review and meta-analysis. Am Heart J. 2013;166:684–93.
Pasceri V, Patti G, Pelliccia F, et al. Complete revascularization during primary percutaneous coronary intervention reduces death and myocardial infarction in patients with multivessel disease: meta-analysis and meta-regression of randomized trials. JACC Cardiovasc Interv. 2018;11:833–43.
Sardella G, Lucisano L, Garbo R, et al. Single-staged compared with multi-staged PCI in multivessel NSTEMI Patients: the SMILE trial. J Am Coll Cardiol. 2016;67:264–72.
Gaffar R, Habib B, Filion KB, et al. Optimal timing of complete revascularization in acute coronary syndrome: a systematic review and meta-analysis. J Am Heart Assoc. 2017;6: e005381.
Cui K, Yin D, Zhu C, et al. Optimal revascularization strategy for patients with ST-segment elevation myocardial infarction and multivessel disease: a pairwise and network meta-analysis. Front Cardiovasc Med. 2021;8: 695822.
Wood DA, Cairns JA, Wang J, et al. Timing of staged nonculprit artery revascularization in patients with ST-segment elevation myocardial infarction: COMPLETE trial. J Am Coll Cardiol. 2019;74:2713–23.
Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165.
Kite TA, Kurmani SA, Bountziouka V, et al. Timing of invasive strategy in non-ST-elevation acute coronary syndrome: a meta-analysis of randomized controlled trials. Eur Heart J. 2022;43:3148–61.
Ibrahim H, Sharma PK, Cohen DJ, et al. Multivessel versus culprit vessel-only percutaneous coronary intervention among patients with acute myocardial infarction: insights from the TRANSLATE-ACS observational study. J Am Heart Assoc. 2017;6: e006343.
Kim MC, Hyun JY, Ahn Y, et al. Optimal revascularization strategy in non-ST-segment-elevation myocardial infarction with multivessel coronary artery disease: culprit-only versus one-stage versus multistage revascularization. J Am Heart Assoc. 2020;9: e016575.
Bainey KR, Alemayehu W, Armstrong PW, et al. Long-term outcomes of complete revascularization with percutaneous coronary intervention in acute coronary syndromes. JACC Cardiovasc Interv. 2020;13:1557–67.
Ben-Gal Y, Moses JW, Mehran R, et al. Surgical versus percutaneous revascularization for multivessel disease in patients with acute coronary syndromes: analysis from the ACUITY (Acute Catheterization and Urgent Intervention Triage Strategy) trial. JACC Cardiovasc Interv. 2010;3:1059–67.
Chang M, Lee CW, Ahn JM, et al. Comparison of outcome of coronary artery bypass grafting versus drug-eluting stent implantation for non-ST-elevation acute coronary syndrome. Am J Cardiol. 2017;120:380–6.
Head SJ, Milojevic M, Daemen J, et al. Mortality after coronary artery bypass grafting versus percutaneous coronary intervention with stenting for coronary artery disease: a pooled analysis of individual patient data. Lancet. 2018;391:939–48.
Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42:1289–367.
Awad HH, Anderson FA Jr, Gore JM, et al. Cardiogenic shock complicating acute coronary syndromes: insights from the Global Registry of Acute Coronary Events. Am Heart J. 2012;163:963–71.
Kolte D, Khera S, Aronow WS, et al. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. J Am Heart Assoc. 2014;3: e000590.
Sato T, Saito Y, Suzuki S, et al. Prognostic factors of in-hospital mortality in patients with acute myocardial infarction complicated by cardiogenic shock. Life (Basel). 2022;12:1672.
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021;42:3599–726.
Hochman JS, Sleeper LA, Webb JG, et al. Early revascularization and long-term survival in cardiogenic shock complicating acute myocardial infarction. JAMA. 2006;295:2511–5.
Omer MA, Brilakis ES, Kennedy KF, et al. Multivessel versus culprit-vessel percutaneous coronary intervention in patients with non-ST-segment elevation myocardial infarction and cardiogenic shock. JACC Cardiovasc Interv. 2021;14:1067–78.
Khera R, Secemsky EA, Wang Y, et al. Revascularization practices and outcomes in patients with multivessel coronary artery disease who presented with acute myocardial infarction and cardiogenic shock in the US, 2009–2018. JAMA Intern Med. 2020;180:1317–27.
Lee JM, Rhee TM, Hahn JY, et al. Multivessel percutaneous coronary intervention in patients with ST-segment elevation myocardial infarction with cardiogenic shock. J Am Coll Cardiol. 2018;71:844–56.
Thiele H, Akin I, Sandri M, et al. One-year outcomes after PCI strategies in cardiogenic shock. N Engl J Med. 2018;379:1699–710.
Thiele H, Akin I, Sandri M, et al. PCI strategies in patients with acute myocardial infarction and cardiogenic shock. N Engl J Med. 2017;377:2419–32.
Thiele H, Desch S. CULPRIT-SHOCK (culprit lesion only PCI versus multivessel percutaneous coronary intervention in cardiogenic shock): implications on guideline recommendations. Circulation. 2018;137:1314–6.
Guedeney P, Barthelemy O, Zeitouni M, et al. Prognostic value of SYNTAX score in patients with infarct-related cardiogenic shock: insights from the CULPRIT-SHOCK trial. JACC Cardiovasc Interv. 2020;13:1198–206.
Harjola VP, Lassus J, Sionis A, et al. Clinical picture and risk prediction of short-term mortality in cardiogenic shock. Eur J Heart Fail. 2015;17:501–9.
Yannopoulos D, Bartos J, Raveendran G, et al. Advanced reperfusion strategies for patients with out-of-hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial. Lancet. 2020;396:1807–16.
Ostadal P, Rokyta R, Karasek J, et al. Extracorporeal membrane oxygenation in the therapy of cardiogenic shock: results of the ECMO-CS randomized clinical trial. Circulation. 2022. https://doi.org/10.1161/CIRCULATIONAHA.122.062949.
Thiele H, Zeymer U, Thelemann N, et al. Intraaortic balloon pump in cardiogenic shock complicating acute myocardial infarction: long-term 6-year outcome of the randomized IABP-SHOCK II trial. Circulation. 2019;139:395–403.
Thiele H, Zeymer U, Neumann FJ, et al. Intraaortic balloon support for myocardial infarction with cardiogenic shock. N Engl J Med. 2012;367:1287–96.
Attinger-Toller A, Bossard M, Cioffi GM, et al. Ventricular unloading using the impella(TM) device in cardiogenic shock. Front Cardiovasc Med. 2022;9: 856870.
Bjarnason TA, Mentias A, Panaich S, et al. Diffusion of percutaneous ventricular assist devices in US markets. Circ Cardiovasc Interv. 2022;15: e011778.
Amin AP, Spertus JA, Curtis JP, et al. The evolving landscape of impella use in the United States among patients undergoing percutaneous coronary intervention with mechanical circulatory support. Circulation. 2020;141:273–84.
Chieffo A, Ancona MB, Burzotta F, et al. Observational multicentre registry of patients treated with IMPella mechanical circulatory support device in ITaly: the IMP-IT registry. EuroIntervention. 2020;15:e1343–50.
Dhruva SS, Ross JS, Mortazavi BJ, et al. Use of mechanical circulatory support devices among patients with acute myocardial infarction complicated by cardiogenic shock. JAMA Netw Open. 2021;4: e2037748.
O’Neill WW, Grines C, Schreiber T, et al. Analysis of outcomes for 15,259 US patients with acute myocardial infarction cardiogenic shock (AMICS) supported with the Impella device. Am Heart J. 2018;202:33–8.
Schrage B, Becher PM, Bernhardt A, et al. Left ventricular unloading is associated with lower mortality in patients with cardiogenic shock treated with venoarterial extracorporeal membrane oxygenation: results from an international, multicenter cohort study. Circulation. 2020;142:2095–106.
Sieweke JT, Berliner D, Tongers J, et al. Mortality in patients with cardiogenic shock treated with the Impella CP microaxial pump for isolated left ventricular failure. Eur Heart J Acute Cardiovasc Care. 2020;9:138–48.
Schrage B, Ibrahim K, Loehn T, et al. Impella support for acute myocardial infarction complicated by cardiogenic shock. Circulation. 2019;139:1249–58.
Dhruva SS, Ross JS, Mortazavi BJ, et al. Association of use of an intravascular microaxial left ventricular assist device vs intra-aortic balloon pump with in-hospital mortality and major bleeding among patients with acute myocardial infarction complicated by cardiogenic shock. JAMA. 2020;323:734–45.
Ouweneel DM, Eriksen E, Sjauw KD, et al. Percutaneous mechanical circulatory support versus intra-aortic balloon pump in cardiogenic shock after acute myocardial infarction. J Am Coll Cardiol. 2017;69:278–87.
Karami M, Eriksen E, Ouweneel DM, et al. Long-term 5-year outcome of the randomized IMPRESS in severe shock trial: percutaneous mechanical circulatory support vs. intra-aortic balloon pump in cardiogenic shock after acute myocardial infarction. Eur Heart J Acute Cardiovasc Care. 2021;10:1009–15.
Grandin EW, Nunez JI, Willar B, et al. Mechanical left ventricular unloading in patients undergoing venoarterial extracorporeal membrane oxygenation. J Am Coll Cardiol. 2022;79:1239–50.
Pahuja M, Johnson A, Kabir R, et al. Randomized trials of percutaneous microaxial flow pump devices. J Am Coll Cardiol. 2022;80:2028–49.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Yuichi Saito declares no conflicts of interest to disclose. Yoshio Kobayashi is a recipient of research grants from Abbott, Boston Scientific, Medtronic, Nipro, and Terumo.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Saito, Y., Kobayashi, Y. Complete revascularization in acute myocardial infarction: a clinical review. Cardiovasc Interv and Ther 38, 177–186 (2023). https://doi.org/10.1007/s12928-022-00907-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-022-00907-6