Abstract
In the countries like Japan where anticoagulation is not recommended in hemodialysis patients, the feasibility of percutaneous left atrial appendage closure (LAAC) in hemodialysis patients with non-valvular atrial fibrillation (NVAF) accompanying high risks of thromboembolic stroke and bleeding remains unknown. Peri-procedural and 45-day clinical outcomes following LAAC using WATCHMAN system, which were performed in our institute between Jun 2020 and April 2022 according to the Japanese Circulation Society guidelines, were retrospectively compared between those with and without hemodialysis. 118 patients (median 79 years, 81 men) consisting of 25 hemodialysis patients and 93 non-hemodialysis patients were included. CHADS score was 3 (2, 4) in the hemodialysis patients and 3 (2, 4) in the non-hemodialysis patients (p = 0.98). HAS-BREAD score was 4 (3, 5) in the hemodialysis patients and 3 (2, 3) in the non-hemodialysis patients (p < 0.001). All procedures were successful, except for a non-hemodialysis patient with a larger left atrial appendage. There were no major complications during index hospitalization and 45-day observational period, except for a hemodialysis patient with suspected bleeding and a non-hemodialysis patient who died due to cardiac amyloidosis. LAAC seems to be feasible in hemodialysis patients with high risks of thromboembolic events and bleedings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Non-valvular atrial fibrillation (NVAF) is the most common cardiac arrhythmia. The prevalence of NVAF has increased with the aging of the world-wide population, affecting approximately 10% in Western countries [1] and approximately 4% in Japan [2]. One of the major and critical complications of NVAF is ischemic stroke. The existence of NVAF increases the risk of ischemic stroke approximately 4–5 times [3]. Current guidelines in Europe, United States, and Japan, recommend anticoagulation therapy using either warfarin or direct oral anticoagulants (DOACs) to prevent thromboembolic ischemic stroke in patients with NVAF and its high risk, according to several risk stratifying scoring systems [4,5,6].
The strategy for those with end-stage renal disease is controversial. The incidence of NVAF and its impact on increasing the risk of stroke are higher in patients with end-stage renal disease compared with general population [7]. Nevertheless, Japanese guidelines do not allow any anticoagulants for such a purpose among this cohort thus far [6], particularly given a high bleeding risk during anticoagulation therapy [8].
Percutaneous left atrial appendage closure (LAAC) is an established therapy for preventing thromboembolic stroke in patients with NVAF, who are not good candidates for long-term anticoagulation therapy (Fig. 1) [9]. However, the detailed clinical implication of LAAC therapy in hemodialytic patients remains uninvestigated [10]. Recently, the safety and efficacy of LAAC for Japanese patients were confirmed in a multi-center single-arm observational study [11], whereas clinical outcomes following LAAC in hemodialysis patients remain uncertain. In this proof-of-concept study, we investigated short-term clinical outcomes of LAAC therapy in NVAF patients with and without hemodialysis.
Left atrial appendage closure using WATCHMAN system. A catheter is inserted using a standard percutaneous technique from the femoral vein (A). The interatrial septum is crossed using a standard trans-septal access system (B). WATCHMAN is deployed and released in the left atrial appendage (C). Heart tissue grows over the WATCHMAN implant and the left atrial appendage is permanently sealed (D)
Methods
Patient selection
NVAF was defined as AF without moderate or severe mitral stenosis or mechanical prosthetic heart valve. Consecutive patients with NVAF who received LAAC using WATCHMAN system (Boston Scientific, St. Paul, Minnesota; Fig. 1) in our institute between June 2020 and April 2022 were prospectively included in our institutional registry and this study was retrospectively conducted using this registry data.
According to our institutional protocol, WATCHMAN 2.5 was used between June 2020 and June 2021. WATCHMAN FLX was used from July 2021. The study was approved by the local ethical board (R2020077) and informed consents were obtained from all participants before inclusion.
Procedure indication
The indication of LAAC was according to the Japanese Circulation Society guidelines. Patients should be those with NVAF who were at high risk of systemic embolisms and were highly recommended to receive anticoagulation therapy according to CHADS2 score and CHADS2-VASc score. On the contrary, they should also be at high risk of bleeding and satisfy either of them: HAS-BLED score equal to or above 3 points; multiple histories of trauma due to falling; cerebral amyloid angiopathy; requirement of multiple antiplatelets; histories of major bleeding with BARC type 3–5. All patients received transesophageal echocardiography for the anatomical assessments. The final indication was determined by the institutional heart-valve team conference.
The indication of LAAC for the hemodialysis patients was similar to the non-hemodialysis patients. All hemodialysis patients satisfied “A” in the HAS-BLEAD score (i.e., abnormal renal function).
Procedure
The WATCHMAN2.5 and FLX are self-expanding, nitinol-framed structures ranging in diameter from 21 to 33 mm (WATCHMAN2.5) and from 20 to 35 mm (WATCHMAN FLX), respectively, to accommodate varying LAA anatomy and size. These devices are fixed by anchor at the LAA ostium to avoid embolization and to prevent blood flow in the LAA. LAAC was performed under general anesthesia according to the standard procedure by the board-certified interventionists using angiography, transesophageal echocardiography, and double curve sheath via a trans-septal puncture approach.
Post-procedure follow-up
Following the procedures, anticoagulation therapy using warfarin or DOAC as well as antiplatelets were continued for 45 days to allow time for device endothelialization: (1) single antiplatelet and DOAC/warfarin with the therapeutic international normalized ratio between 2.0 and 2.6 for those with non-hemodialysis; single antiplatelet and warfarin with a therapeutic international normalized ratio between 1.5 and 2.0 for hemodialytic patients (Fig. 2).
In hemodialysis patients, warfarin and single antiplatelet were converted to dual antiplatelet, and warfarin alone was converted to single antiplatelet following a 45-day follow-up. In non-hemodialysis patients, DOAC and single antiplatelet were converted to dual antiplatelet, warfarin and single antiplatelet were converted to dual antiplatelet, and DOAC alone was converted to single antiplatelet following 45-day follow-up. All medications were converted to single antiplatelet following 6-month follow-up.
Study outcomes
Procedure-related events during the procedure, during the index hospitalization, and during the 45-day post-discharge observational period were counted and compared between those with and without hemodialysis. Of note, acute kidney injury was defined as an increase in serum creatinine level > 0.3 mg/dL per 48 h, 1.5-fold increase in serum creatinine level, or urine volume < 0.5 mL/kg/h for 6 h [12]. Device-related thrombus or residual peri-device flow > 5 mm in width were surveyed by transesophageal echocardiography (Fig. 3).
Statistical analysis
Continuous variables were expressed as mean and standard deviation and compared between the two groups (i.e., hemodialysis group versus non-hemodialysis group) using unpaired t-test. Categorical variables were expressed as numbers and percentages and compared between the two groups using Fischer’s exact test. A value of p <0.05 was considered statistically significant. Statistical analyses were performed using SPSS Statistics 24 (SPSS Inc, Armonk, IL, USA).
Results
Baseline characteristics
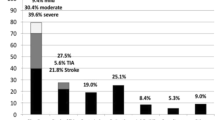
118 NVAF patients were included. Median age was 79 (73, 84) years old and 81 (69%) were men (Table 1). On median, CHADS2 score was 3 (2, 4) points, CHADS2-VASc score was 5 (4, 6) points, and HAS-BLEAD score was 3 (2, 3) points.
Of them, 25 patients were dependent on hemodialysis and other 93 patients were assigned to the non-hemodialysis group (Fig. 2). Hemodialysis patients were younger and had a lower incidence of major bleeding history and higher incidence of ischemic stroke history compared with the non-hemodialysis group (p < 0.05 for all). CHADS2 score and CHADS2-VASc score were not significantly different between the two groups, whereas the hemodialysis group had a higher HAS-BLEAD score (p < 0.001). Eighty patients received transesophageal echocardiography, which demonstrated no significant differences in the LAA parameters between the two groups (p > 0.05 for all; Table 2).
LAAC procedure
The procedure success rate was 99%: the procedure was unsuccessful in a patient in the non-hemodialysis group due to the inappropriately larger size of LAA (Table 3). The procedure time was longer and the contrast volume was higher in the hemodialysis group (p < 0.05 for both). The incidences of multiple device use and partial recapture were not significantly different between the two groups (p > 0.05 for both).
During the index hospitalization, there were no major complications including access site events, acute kidney injury, pericardial effusion, device embolization, infectious endocarditis, and stroke (Table 4). One hemodialysis patient had bleeding event due to suspected gastrointestinal bleeding, which improved by discontinuing warfarin without blood transfusion. The in-hospital duration was not significantly different between the two groups (p = 0.76). All patients could be discharged alive.
Trends in medications
At baseline, more hemodialysis patients received antiplatelets than the non-hemodialysis group (p < 0.05; Table 5). All hemodialysis patients received warfarin, whereas most of the non-hemodialysis patients (91%) received DOAC.
As for the antiplatelets, most of the patients (79%) received single antiplatelets at the index discharge according to the institutional protocol, irrespective of the dependence on hemodialysis (Fig. 2). No patients received dual antiplatelets.
94 patients were followed until day 45. The proportion of prescriptions remained almost unchanged from the index discharge. In the hemodialysis patients, 20 (95%) received warfarin. In the non-hemodialysis patients, 5 (7%) received warfarin and others (68 [93%]) received DOAC.
Short-term follow-up data
94 patients completed a 45-day follow-up (Table 6). Most of the device parameters, which were assessed using transesophageal echocardiography, were not statistically different between the two groups. Almost half of them had procedure-related residual atrial septum defect, irrespective of the dependence on hemodialysis (p = 0.63). No patients had right-to-left jet.
During the 45-day observational period, no patients had major complications including pericardial effusion and device-related thrombus. There were no deceased patients, except for a patient with cardiac amyloidosis in the non-hemodialysis group who died suddenly without any obvious reasons 5 days following the index discharge.
Discussion
In this prospective study, we reported for the first time the short-term feasibility of LAAC in hemodialysis patients with high risks of thromboembolic events and bleedings.
Safety and efficacy of LAAC in the non-hemodialysis patients
LAAC is an established alternative to anticoagulation therapy to prevent stroke events in patients with NVAF and high risk of bleedings [9]. LAAC has a non-inferiority in efficacy and safety to long-term warfarin therapy in this cohort. A recent 4-year observational study demonstrated comparable safety and efficacy of LAAC to DOAC therapy also in this cohort [13]. More feasibility has been achieved by the innovation of WATCHMAN FLX device over the conventional WATCHMAN 2.5 [14]. However, the strategy to prevent stroke in patients with hemodialysis and NVAF remains uncertain.
Prevention of stroke in the hemodialysis patients
In non-hemodialysis patients, the existence of NVAF is a major trigger of cardiac stroke. The hemodialysis patients have multiple high-risk origins of thromboembolic strokes due to systemic atherosclerosis, whereas cardiac stroke is reported to be a major etiology in Japan [15].
The applicability of CHADS2 score, which is an established score to consider the risk of stroke in the general cohort, to the hemodialysis cohort remains unknown, given that the original study did not include them [16]. However, the risk of stroke increases in NVAF patients with renal impairment compared with those without renal impairment [17].
Anticoagulation therapy is an established strategy to prevent stroke in the general cohort with NVAF and high risk of stroke. In hemodialysis patients, all types of DOAC are contraindicated. The Japanese society for dialysis therapy guidelines states that warfarin therapy is, in principle, contraindicated [18]. Preventive effect of warfarin on stroke remains unknown. Instead, warfarin may be associated with the incremental incidence of major bleeding [8]. Warfarin might facilitate atherosclerosis, which was assessed using pulse wave velocity analyses [19].
Given all together, strategies other than anticoagulation would be required for those with hemodialysis to prevent stroke.
LAAC for hemodialysis patients
One of the strategies to answer the above request is LAAC. Gotzmann and colleagues retrospectively analyzed 128 candidates of LAAC. Of them, mortality, bleeding incidence, and thromboembolic events incidence were not statistically different between 33 hemodialysis patients and others [20]. In another study, renal impairment was associated with higher in-hospital mortality, longer hospital stay, and a higher 30-day readmission rate [21].
This is the first study that demonstrated the short-term feasibility of LAAC in Japanese hemodialysis patients. According to the recommended standard regimen for post-LAAC 45 days consisting of the combination of DOAC and low-dose aspirin [22], we administered DOAC (for non-hemodialysis patients) or warfarin (for hemodialysis patients) and low-dose aspirin and/or thienopyridine P2Y12 receptor antagonist. We adjusted the dose of warfarin with a target range of international normalized ratio between 1.5 and 2.0, according to the recommendation of guidelines.
The incidences of peri-procedural complications were not significantly different between those with and without hemodialysis. There was no device-related thrombosis during the 45-day follow-up period among all cohort. Only a patient with hemodialysis required termination of warfarin during a 45-day follow-up period. The patient had a slight progression of anemia due to asymptomatic interstitial bleeding, which was ameliorated without blood transinfusion.
LAAC might be a feasible strategy also in hemodialysis patients. Short-term warfarin therapy following LAAC would be safe in this cohort. Further studies are warranted to validate the long-term feasibility and implication of LAAC in this cohort.
Limitations
This study was conducted in a single center using a small sample size. Statistical non-significance does not guarantee similarity. There are several differences in background and procedure-related parameters, including the incidence of major bleeding history and HAS-BLEAD score as well as procedure time between the two groups. More patients with hemodialysis received LAAC due to high HAS-BLEAD score rather than a history of major bleeding. Initial recommendations to receive LAAC were dominantly performed by cardiologists. Thus, there might be selection bias. We cannot ignore the impact of two different devices (2.5 and FLX) and the learning curve of the operators. Of note, hemodialysis patients trended to receive WATCHMAN 2.5 rather than FLX. Post-procedural medication regimens were different between the two groups. Such a difference might have affected clinical outcomes. We observed just 45 days following LAAC and a longer observational study is the next concern.
Conclusions
LAAC seems to be feasible in hemodialysis patients with high risks of thromboembolic events and bleedings.
Data availability
Data are available from the corresponding authors upon reasonable requests.
References
Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. Am J Cardiol. 2013;112(8):1142–7.
Inoue H, Fujiki A, Origasa H, Ogawa S, Okumura K, Kubota I, Aizawa Y, Yamashita T, Atarashi H, Horie M, Ohe T, Doi Y, Shimizu A, Chishaki A, Saikawa T, Yano K, Kitabatake A, Mitamura H, Kodama I, Kamakura S. Prevalence of atrial fibrillation in the general population of Japan: an analysis based on periodic health examination. Int J Cardiol. 2009;137(2):102–7.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS, American Heart Association Council on E, Prevention Statistics C, Stroke Statistics S. Heart Disease and Stroke Statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139(10):56–528.
Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom-Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL, Group ESCSD. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur Heart J. 2021;42(5):373–498.
January CT, Wann LS, Calkins H, Chen LY, Cigarroa JE, Cleveland JC Jr, Ellinor PT, Ezekowitz MD, Field ME, Furie KL, Heidenreich PA, Murray KT, Shea JB, Tracy CM, Yancy CW. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines and the heart rhythm society in collaboration with the society of thoracic surgeons. Circulation. 2019;140(2):e125–51.
Ono K, Iwasaki YK, Akao M, Ikeda T, Ishii K, Inden Y, Kusano K, Kobayashi Y, Koretsune Y, Sasano T, Sumitomo N, Takahashi N, Niwano S, Hagiwara N, Hisatome I, Furukawa T, Honjo H, Maruyama T, Murakawa Y, Yasaka M, Watanabe E, Aiba T, Amino M, Itoh H, Ogawa H, Okumura Y, Aoki-Kamiya C, Kishihara J, Kodani E, Komatsu T, Sakamoto Y, Satomi K, Shiga T, Shinohara T, Suzuki A, Suzuki S, Sekiguchi Y, Nagase S, Hayami N, Harada M, Fujino T, Makiyama T, Maruyama M, Miake J, Muraji S, Murata H, Morita N, Yokoshiki H, Yoshioka K, Yodogawa K, Inoue H, Okumura K, Kimura T, Tsutsui H, Shimizu W, Japanese Circulation S, Japanese Circulation S, Japanese Heart Rhythm Society Joint Working G. JCS/JHRS. Guideline on pharmacotherapy of cardiac arrhythmias. Circ J. 2020;86(11):1790–924.
Zimmerman D, Sood MM, Rigatto C, Holden RM, Hiremath S, Clase CM. Systematic review and meta-analysis of incidence, prevalence and outcomes of atrial fibrillation in patients on dialysis. Nephrol Dial Transplant. 2012;27(10):3816–22.
Pokorney SD, Black-Maier E, Hellkamp AS, Friedman DJ, Vemulapalli S, Granger CB, Thomas L, Peterson ED, Piccini JP Sr. Oral anticoagulation and cardiovascular outcomes in patients with atrial fibrillation and end-stage renal disease. J Am Coll Cardiol. 2020;75(11):1299–308.
Reddy VY, Doshi SK, Kar S, Gibson DN, Price MJ, Huber K, Horton RP, Buchbinder M, Neuzil P, Gordon NT, Holmes DR Jr. Prevail, investigators PA. 5-Year outcomes after left atrial appendage closure: from the PREVAIL and PROTECT AF trials. J Am Coll Cardiol. 2017;70(24):2964–75.
Genovesi S, Slaviero G, Porcu L, Casu G, Bertoli S, Sagone A, Pieruzzi F, Rovaris G, Buskermolen M, Danna P, Montoli A, Oreglia J, Contaldo G, Mazzone P. Implant success and safety of left atrial appendage occlusion in end stage renal disease patients: peri-procedural outcomes from an Italian dialysis population. Int J Cardiol. 2018;262:38–42.
Aonuma K, Yamasaki H, Nakamura M, Ootomo T, Takayama M, Ando K, Hirao K, Morino Y, Hayashida K, Kusano K, Main ML, Saito S. Percutaneous WATCHMAN left atrial appendage closure for japanese patients with nonvalvular atrial fibrillation at increased risk of thromboembolism- first results from the SALUTE trial. Circ J. 2018;82(12):2946–53.
Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–84.
Osmancik P, Herman D, Neuzil P, Hala P, Taborsky M, Kala P, Poloczek M, Stasek J, Haman L, Branny M, Chovancik J, Cervinka P, Holy J, Kovarnik T, Zemanek D, Havranek S, Vancura V, Peichl P, Tousek P, Lekesova V, Jarkovsky J, Novackova M, Benesova K, Widimsky P, Reddy VY, Investigators P-T. 4-year outcomes after left atrial appendage closure versus nonwarfarin oral anticoagulation for atrial fibrillation. J Am Coll Cardiol. 2022;79(1):1–14.
Kar S, Doshi SK, Sadhu A, Horton R, Osorio J, Ellis C, Stone J Jr, Shah M, Dukkipati SR, Adler S, Nair DG, Kim J, Wazni O, Price MJ, Asch FM, Holmes DR Jr, Shipley RD, Gordon NT, Allocco DJ, Reddy VY, Investigators PF. Primary outcome evaluation of a next-generation left atrial appendage closure device: results from the PINNACLE FLX trial. Circulation. 2021;143(18):1754–62.
Toida T, Sato Y, Nakagawa H, Komatsu H, Uezono S, Yamada K, Ishihara T, Hisanaga S, Kitamura K, Fujimoto S. Risk of cerebral infarction in japanese hemodialysis patients: miyazaki dialysis cohort study (MID study). Kidney Blood Press Res. 2016;41(4):471–8.
Gage BF, Waterman AD, Shannon W, Boechler M, Rich MW, Radford MJ. Validation of clinical classification schemes for predicting stroke: results from the National Registry of Atrial Fibrillation. JAMA. 2001;285(22):2864–70.
Olesen JB, Lip GY, Kamper AL, Hommel K, Kober L, Lane DA, Lindhardsen J, Gislason GH, Torp-Pedersen C. Stroke and bleeding in atrial fibrillation with chronic kidney disease. N Engl J Med. 2012;367(7):625–35.
Hirakata H, Nitta K, Inaba M, Shoji T, Fujii H, Kobayashi S, Tabei K, Joki N, Hase H, Nishimura M, Ozaki S, Ikari Y, Kumada Y, Tsuruya K, Fujimoto S, Inoue T, Yokoi H, Hirata S, Shimamoto K, Kugiyama K, Akiba T, Iseki K, Tsubakihara Y, Tomo T, Akizawa T, Japanese Society for Dialysis T. Japanese Society for Dialysis Therapy guidelines for management of cardiovascular diseases in patients on chronic hemodialysis. Ther Apher Dial. 2012;16(5):387–435.
Mac-Way F, Poulin A, Utescu MS, De Serres SA, Marquis K, Douville P, Desmeules S, Lariviere R, Lebel M, Agharazii M. The impact of warfarin on the rate of progression of aortic stiffness in hemodialysis patients: a longitudinal study. Nephrol Dial Transplant. 2014;29(11):2113–20.
Gotzmann M, Choudhury DS, Hogeweg M, Heringhaus F, Mugge A, Pflaumbaum A. Risk stratification in patients undergoing interventional left atrial appendage occlusion-Prognostic impact of EuroSCORE II. Clin Cardiol. 2020;43(5):508–15.
Ahuja KR, Ariss RW, Nazir S, Vyas R, Saad AM, Macciocca M, Moukarbel GV. The association of chronic kidney disease with outcomes following percutaneous left atrial appendage closure. JACC Cardiovasc Interv. 2021;14(16):1830–9.
Ledwoch J, Staubach S, Akin I, Ince H, Zeymer U, Pleger S, Sievert H, Hochadel M, Senges J, Lewalter T, Brachmann J, Mudra H. Anticoagulation versus antiplatelet therapy after percutaneous left atrial appendage closure-subanalysis from the multicenter LAARGE registry. J Interv Card Electrophysiol. 2021;64(2):489–96.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Ueno is a clinical proctor for Boston scientific.
Ethical approval
IRB approval: Ethical board of University of Toyama, R2020077
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ueno, H., Imamura, T., Tanaka, S. et al. Initial report of percutaneous left atrial appendage closure in hemodialysis patients with atrial fibrillation and high risk of bleeding in Japan. Cardiovasc Interv and Ther 38, 338–347 (2023). https://doi.org/10.1007/s12928-022-00904-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-022-00904-9