Abstract
Aims
The aim of this study is to enhance the accuracy of monitoring and treatment information for patients diagnosed with colorectal cancer (CRC).
Methods
Utilizing the Surveillance, Epidemiology, and End Results (SEER) database, a cohort of 335,948 eligible CRC patients was included in this investigation. Conditional survival probability and actuarial overall survival were employed as methodologies to investigate the association between clinicopathological characteristics and cancer prognosis.
Results
Among CRC patients, the 5-year survival rate was 59%, while the 10-year survival rate was 42%. Over time, conditional survival showed a consistent increase, with rates reaching 45% and 48% for individuals surviving 1 and 2 years, respectively. Notably, patients with unfavorable tumor stages exhibited substantial improvements in conditional survival, thereby narrowing the disparity with actuarial overall survival over time.
Conclusion
This study underscores the significance of time-dependent conditional survival probability, particularly for patients with a poorer prognosis. The findings suggest that long-term CRC survivors may experience improved cancer prognosis over time.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Colorectal cancer (CRC), alternatively referred to as colon or rectal cancer, stands as a prevalent malignant ailment on a global scale. Positioned as the third most prevalent cancer and the second primary contributor to cancer-associated fatalities worldwide, CRC imposes a substantial burden [1, 2]. Despite notable strides in diagnostic and therapeutic realms, the task of prognosticating individual patient outcomes at distinct junctures remains inherently challenging [3]. Prognostic models, epitomized by survival nomograms, assume pivotal roles in foreseeing patient survival by leveraging specific clinical and pathological variables [4, 5]. However, conventional nomograms conventionally presuppose constant hazard rates over time, a premise that might inadequately capture the dynamic evolution of cancer progression and treatment response [6].
To overcome this inherent limitation, we propose a pioneering approach: a novel conditional survival nomogram tailored specifically for monitoring the real-time prognosis of non-metastatic colorectal cancer [7,8,9]. This CS-nomogram harnesses sophisticated statistical modeling techniques, its efficacy contingent upon the underlying assumptions established during its development [10, 11]. Crucially, rigorous validation of the nomogram's predictive accuracy is imperative, alongside an assessment of its applicability across diverse patient cohorts and healthcare settings [12, 13]. This innovative methodology aims to furnish personalized prognostic insights grounded in patient-specific attributes and the dynamic nature of the disease trajectory. By integrating time-varying covariates, we afford a systematic exploration of patient data at various temporal junctures, facilitating meticulous monitoring of prognosis and treatment efficacy [14]. Given the pronounced clinical heterogeneity and treatment responsiveness exhibited by colorectal cancer, precise prognostic appraisal assumes paramount significance for optimal patient care. Traditional survival nomograms, predicated upon baseline patient characteristics, regrettably, falter in encapsulating the temporal dynamics of prognostic determinants [15]. Our proposed conditional survival nomogram bridges this critical lacuna by encompassing dynamic variables such as treatment response, disease progression, and late-effects, thereby enabling real-time prognosis monitoring. Moreover, the utilization of nomograms confers several notable advantages over conventional survival analysis methodologies. Nomograms furnish a visually intuitive depiction of prognostic factors and their corresponding weights, bolstering the interpretability and clinical utility of predictive models [16]. Furthermore, they afford personalized risk assessments tailored to an individual patient's unique profile and disease trajectory. This personalized prognostic evaluation approach holds promise in guiding treatment decisions, enriching patient counseling endeavors, and ultimately augmenting long-term survival outcomes [17].
In summary, our study endeavors to pioneer the development of a groundbreaking conditional survival nomogram tailored specifically for monitoring real-time prognosis in non-metastatic colorectal cancer patients. This innovative methodology will meticulously incorporate time-varying covariates, thereby furnishing personalized prognostic insights to clinicians. By empowering clinicians with patient-specific characteristics and insights into the dynamic evolution of the disease, we aim to equip them with the tools necessary to make informed decisions. Through the implementation of this cutting-edge prognostic tool, we anticipate a transformative impact on patient outcomes, alongside a deeper understanding of the evolving nature of colorectal cancer. We are optimistic that this novel approach will contribute significantly to the advancement of personalized medicine in the realm of colorectal cancer care.
2 Materials and methods
2.1 Data source and study population
The data utilized for this study were sourced from the Surveillance, Epidemiology, and End Results (SEER) database, accessible via https://seer.cancer.gov/. Renowned for its comprehensive repository of cancer patients spanning diverse geographic regions within the United States, the SEER database offers a wealth of meticulously documented clinical and epidemiological information [18]. Our study focused on patients diagnosed with colorectal cancer within a specified timeframe. Inclusion criteria encompassed histologically confirmed primary colorectal cancer cases, coupled with the availability of comprehensive demographic, clinical, and follow-up data. Furthermore, TNM staging was redefined in accordance with the eighth edition of TNM staging guidelines, accounting for tumor size, lymph node metastasis, and distant tumor metastasis. Patients with incomplete or missing data were excluded from the analysis, ensuring the integrity and robustness of our dataset.
2.2 Ethical considerations
This study rigorously adhered to the guidelines and regulations stipulated by the SEER database. Given that the SEER database houses de-identified patient information, ethical approval or informed consent was not deemed necessary for this research endeavor.
2.3 Variables of interest
The selection of clinical and pathological variables for analysis was guided by their established association with colorectal cancer prognosis. These variables comprised age at diagnosis, sex, race/ethnicity, tumor location, tumor stage, histological subtype, tumor grade, and treatment modalities (including surgery, chemotherapy, and radiation therapy). Additionally, pertinent data pertaining to vital status and survival duration were meticulously collected to facilitate the computation of conditional survival probabilities.
2.4 Development of the conditional survival nomogram
To construct the conditional survival nomogram, we employed a robust statistical modeling approach. Initially, least absolute shrinkage and selection operator (LASSO) regression analysis was conducted to identify significant prognostic factors associated with survival outcomes. Time-dependent covariates were integrated to capture the dynamic nature of prognostic factors over time. Subsequently, the identified prognostic factors were utilized to formulate the conditional survival nomogram. Conditional survival rate denotes the probability that a colorectal cancer patient will survive y years subsequent to surviving x years from the date of diagnosis, expressed mathematically as CS(y|x) = OS(x + y)/OS(x), where CS(y|x) represents the probability of the patient being alive for x + y years post-diagnosis, and x denotes successful survival for x years. Each variable’s contribution to the overarching prognostic model was quantified using hazard ratios (HR) alongside corresponding 95% confidence intervals (CI). Covariate coefficients were employed to allocate points on the nomogram's scale. The cumulative sum of these points for each patient facilitated the determination of their individualized probability of survival at specific time intervals.
2.5 CS-nomogram model accuracy
To evaluate the performance and accuracy of the conditional survival nomogram, we adopted rigorous internal validation techniques including bootstrapping and cross-validation. These methods were instrumental in assessing the nomogram's calibration and discrimination capabilities, ensuring its reliability in predicting survival probabilities over time. Furthermore, we conducted comparative analyses to juxtapose the performance of the conditional survival nomogram against that of traditional survival models, such as the TNM staging system. This enabled us to gauge the superiority of our proposed nomogram in prognostic accuracy and clinical utility, providing valuable insights into its potential as a robust prognostic tool for non-metastatic colorectal cancer patients.
2.6 Statistical analysis
The statistical analysis was conducted using R software version 4.3.5. Patient demographics and clinical characteristics were summarized using descriptive statistics. Survival analysis techniques, such as Kaplan–Meier estimation and log-rank tests, were employed to assess survival outcomes across different subgroups. LASSO regression models were utilized to identify prognostic factors associated with colorectal cancer outcomes. The development and validation of the conditional survival nomogram will be detailed, emphasizing its predictive accuracy and clinical applicability. The Materials and Methods section comprehensively outlined the study design, data source, patient selection criteria, variables of interest, development of the conditional survival nomogram, model validation procedures, ethical considerations, and statistical analysis methods. These methodologies were meticulously implemented to capture the dynamic nature of colorectal cancer prognosis using patient data from the SEER database.
3 Results
3.1 Patient demographics
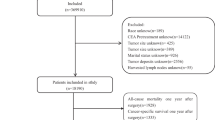
Our study analyzed data from 335,948 colorectal cancer (CRC) patients registered in the SEER database from years ranging 2004 to 2018. The median age at diagnosis was 66.6 years old. The ratio composition of thepatient population was 79.9% white, 11.3%black, and 8.8% from other racial backgrounds. Regarding the age population, 3.3% of patients under 40 years old, 53.3% fell within the 40–70 years old range, and 43.4% over 70 years old (Table 1, Fig. 1).
3.2 Overall survival and conditional survival analysis
The median survival time for CRC patients was 89 months (Fig. 2A). Utilizing Kaplan–Meier analysis, we observed that the 5-year survival rate for CRC patients stood at 59% (95% CI 59–59%), while the 10-year survival rate was 42% (95% CI 42–42%). Additionally, our conditional survival probability analysis unveiled a progressive increase in the 10-year overall survival rate with each additional year since diagnosis. For instance, among patients surviving 1 and 2 years post-diagnosis, the corresponding 10-year survival rates (representing the probability of living another 9 and 8 years) were determined to be 45% and 48%, respectively. Similarly, patients who survived 3–9 years from the date of diagnosis exhibited escalating 10-year survival rates of 51%, 55%, 59%, 64%, 70%, 78%, and 87%, respectively (Table 2, Fig. 3).
Furthermore, our analysis of the mortality rate and annual hazard rate revealed that initial diagnosis was associated with a mortality rate of 1.999%. However, upon surviving the first year post-diagnosis, patients experienced a notable decline in their average mortality rate to 0.754%. This downward trend persisted, with further reductions observed in the third year, fifth year, and eighth year, resulting in average mortality rates of 0.598%, 0.347%, and 0.289%, respectively (Fig. 2B). Moreover, the annual risk rate exhibited a non-linear relationship, with the highest risk occurring in the first year following diagnosis. However, as patients surpassed the initial year milestone, their probability of death gradually diminished, underscoring the dynamic nature of mortality risk over time.
3.3 Overall survival and conditional survival analysis based on TNM stage
We identified a significant correlation between TNM stage and prognosis among CRC patients. Specifically, the 3-year survival rates for Stage I, II, III, and IV were determined to be 85%, 78%, 70%, and 28%, respectively. Our conditional survival analysis revealed that the 3-year survival rates for patients with different TNM stages approached each other as the survival time increased. For patients who survived up to the fifth year after diagnosis, the probabilities of surviving to the eighth year were 84%, 80%, 80%, and 63% for Stage I, II, III, and IV, respectively. Moreover, we observed distinct fluctuations in survival rates based on specific factors. For instance, patients diagnosed with pathological T1 stage CRC exhibited an initial 3-year survival rate of 80%, which escalated to 86% if they survived up to the fifth year post-diagnosis. Analogous trends were discerned among patients stratified by other stage-specific criteria (Table 3).
3.4 Overall survival and conditional survival analysis based on type of surgery
Based on the type of surgery, we categorized patients into three subgroups: (1) non-surgical, (2) local ablation or excision, and (3) resection of partial or whole organ. The 3-year survival rates for these groups were 30%, 82%, and 72%, respectively, while the 10-year survival rates were 14%, 54%, and 43%. For patients who survived 5 years after diagnosis, the probabilities of still being alive at 8th year were 75%, 84%, and 81% for the three subgroups. The 3-year survival rate for patients who received radiation therapy was 73%, indicating an 81% chance of survival at 8th year if they lived up to the fifth year after diagnosis. We also observed varying changes in survival rates based on the provision of radiation and chemotherapy (Table 3).
3.5 LASSO regression analyses
We performed LASSO regression analysis to discern significant prognostic factors associated with survival outcomes in CRC patients. This analysis unveiled several variables that exerted a substantial impact on overall survival. These variables encompassed age, marital status, race, pathological stage (T, N, or M), histological grade, type of surgery, resection of lymph nodes, radiation therapy, chemotherapy, regional nodes positivity, and the number of tumors (Fig. 4).
3.6 Development of the conditional survival nomogram
Using the identified significant prognostic factors, we developed a novel conditional survival nomogram for CRC patients. This nomogram incorporated time-dependent covariates to capture dynamic changes in prognostic variables over time. By providing individualized survival probabilities at specific time intervals, the nomogram enables real-time prognosis monitoring. The nomogram is based on a scoring system that considered the impact of each included factor on overall survival prognosis. By combining the conditional survival rate formula with the nomogram, we created a conditional survival nomogram (CS-nomogram) that predicts the probability of each patient surviving y years after living x years, based on their clinicopathological parameters. For instance, a patient with a nomogram total score of 180 has a 10-year survival rate of 42%. If this patient is still alive at the third year after diagnosis, the probability of still being alive at the 10th year after diagnosis is 69% (Fig. 5).
4 Discussion
The development of a novel conditional survival nomogram for monitoring real-time prognosis in CRC patients marks a significant milestone in the field, as corroborated by previous studies [12, 19, 20]. This personalized tool integrates time-varying covariates and patient-specific characteristics to furnish individualized survival estimates at specific time intervals, thereby bolstering the foundation for tailored treatment decision-making [21, 22]. By offering real-time prognostic information, the nomogram serves as a valuable resource in patient counseling and shared decision-making processes, facilitating the dissemination of tailored survival estimates at distinct time points [23]. This enhanced communication fosters an environment conducive to alleviating patient anxiety, fostering realistic expectations, and empowering patients to actively engage in their care journey [24].
The analysis results underscored a 5-year survival rate of 59%, indicative of a moderate prognosis for CRC patients. However, the 10-year survival rate exhibited a decline to 42%, signaling a lower long-term survival outlook for these individuals. This underscores the imperative of timely diagnosis, efficacious treatment, and comprehensive long-term management strategies for CRC patients. Additionally, the conditional survival analysis provided valuable insights into the dynamic changes in survival rates over time. The probabilities of surviving for an additional 9 or 8 years increased to 45% and 48%, respectively, if patients lived another 1 or 2 years after their initial diagnosis. Notably, the overall 10-year survival rates significantly improved for patients who survived beyond the first year, with rates ranging from 51 to 87% depending on the number of years survived. This indicates that survival rates progressively improve as patients achieve longer-term remission.
The correlation between TNM stage and survival outcomes was strikingly evident in our analysis. Stage IV CRC patients exhibited the lowest 3-year survival rate of merely 28%, while those classified as stage I patients demonstrated the highest rate at 85%. However, as survival time extended, the survival rates for all stages progressively converged. This phenomenon suggests that regardless of the initial TNM stage, survival prospects may tend to become more similar over time. The type of surgery emerged as a pivotal determinant of survival rates. Non-surgical patients manifested the lowest 3-year survival rate of 30%, whereas individuals undergoing local ablation or excision and resection of partial or whole organs showcased substantially superior rates of 82% and 72%, respectively. Further analysis unveiled that patients who received radiation therapy exhibited a relatively higher 3-year survival rate of 73%, hinting at the potential benefits associated with this treatment modality. These observations underscore the pivotal role of surgical intervention and hint at the potential efficacy of radiation therapy in enhancing survival outcomes for CRC patients. Furthermore, the LASSO regression analysis unveiled several factors significantly influencing overall survival, including age, marital status, race, pathological stage, histological grade, type of surgery, lymph node resection, radiation therapy, chemotherapy, and tumor-related variables. These findings emphasize the multifactorial nature of CRC prognosis and underscore the imperative of considering multiple variables in clinical decision-making and prognosis estimation.
The CS-nomogram offers several noteworthy clinical implications. Firstly, it enables oncologists and clinicians to monitor patients' prognosis throughout the disease trajectory [13, 25, 26]. By considering dynamic variables such as treatment response, disease progression, and late-effects, the incorporation of dynamic variables in the nomogram allows for timely identification of patients at high risk of disease recurrence or progression [27]. This early risk stratification enables clinicians to intensify follow-up measures, implement adjuvant therapies, or consider alternative treatment approaches [28, 29]. Early intervention based on accurate prognostic information can potentially improve survival outcomes and enhance disease management. In the same time, there are certain limitations that need to be acknowledged. Firstly, this study utilized retrospective data from the SEER database, which may introduce inherent biases. The accuracy and reliability of the CS-nomogram's predictive performance depend on the quality of the data source and the completeness of the collected variables [30, 31]. Prospective studies with larger sample sizes and robust data collection methods are warranted to further validate the nomogram's clinical utility. Another limitation is the lack of inclusion of certain important prognostic factors, such as comorbidities and molecular biomarkers. The assessment of these variables could potentially enhance the accuracy and predictive power of the nomogram. Future research should explore incorporating these additional factors into the model to further improve prognostic accuracy [32].
FContinual refinement and enhancement of the conditional survival nomogram for CRC are imperative to keep pace with evolving clinical needs. One avenue for improvement involves incorporating emerging biomarkers, such as genetic mutations and microenvironment characteristics, into the model. By integrating these factors, a more comprehensive understanding of tumor biology can be attained, facilitating the development of individualized treatment strategies tailored to patients' specific molecular profiles. Moreover, prospective studies featuring long-term follow-up are indispensable for evaluating the sustained predictive value and clinical impact of the conditional survival nomogram. These investigations can furnish real-world evidence regarding the nomogram's efficacy in guiding treatment decisions, enhancing patient outcomes, and optimizing resource allocation in healthcare settings. The potential integration of machine learning algorithms and artificial intelligence techniques holds promise for further enhancing the accuracy and precision of the nomogram. Leveraging big data analytics and advanced computational methods enables the development of more sophisticated prediction models capable of capturing subtle changes in the disease course and treatment response, thereby facilitating personalized and proactive patient care. Continued research efforts in these directions are pivotal for advancing the field of CRC prognosis prediction and improving patient management strategies.
5 Conclusion
The development of a novel conditional survival nomogram for non-metastatic colorectal cancer represents a promising advancement in prognosis monitoring. This personalized tool, incorporating time-varying covariates and patient-specific characteristics, offers real-time prognostic information for individual patients. While certain limitations need to be addressed, the nomogram holds great potential to guide treatment decisions, improve patient counseling, and enhance long-term survival outcomes. Further research and validation are warranted to fully realize the clinical utility of this innovative approach.
Availability of data and materials
All data generated or analyzed during this study are included in this published article or are available from the corresponding author on reasonable request. The dataset generated and analyzed during the current study is available in the Surveillance Epidemiology and End Results (SEER) Database repository (https://seer.cancer.gov/).
References
Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2023. CA Cancer J Clin. 2023;73(3):233–54. https://doi.org/10.3322/caac.21772.
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics 2023. CA Cancer J Clin. 2023;73(1):17–48. https://doi.org/10.3322/caac.21763.
Kratzer TB, Jemal A, Miller KD, Nash S, Wiggins C, Redwood D, et al. Cancer statistics for American Indian and Alaska native individuals, 2022: including increasing disparities in early onset colorectal cancer. CA Cancer J Clin. 2023;73(2):120–46. https://doi.org/10.3322/caac.21757.
Iasonos A, Schrag D, Raj GV, Panageas KS. How to build and interpret a nomogram for cancer prognosis. J Clin Oncol. 2008;26(8):1364–70. https://doi.org/10.1200/jco.2007.12.9791.
Balachandran VP, Gonen M, Smith JJ, DeMatteo RP. Nomograms in oncology: more than meets the eye. Lancet Oncol. 2015;16(4):e173–80. https://doi.org/10.1016/s1470-2045(14)71116-7.
Bandini M, Fossati N, Briganti A. Nomograms in urologic oncology, advantages and disadvantages. Curr Opin Urol. 2019;29(1):42–51. https://doi.org/10.1097/mou.0000000000000541.
Dikken JL, Baser RE, Gonen M, Kattan MW, Shah MA, Verheij M, et al. Conditional probability of survival nomogram for 1-, 2-, and 3-year survivors after an r0 resection for gastric cancer. Ann Surg Oncol. 2013;20(5):1623–30. https://doi.org/10.1245/s10434-012-2723-6.
Chen M, Chen T. Individualized conditional survival nomograms for stage I–III early onset colorectal cancer patients. Jpn J Clin Oncol. 2023;53(2):115–21. https://doi.org/10.1093/jjco/hyac169.
Siddiqui MR, Li EV, Kumar S, Busza A, Lin JS, Mahenthiran AK, et al. Optimizing detection of clinically significant prostate cancer through nomograms incorporating MRI, clinical features, and advanced serum biomarkers in biopsy naïve men. Prostate Cancer Prostatic Dis. 2023. https://doi.org/10.1038/s41391-023-00660-8.
Meng X, Hao F, Ju Z, Chang X, Guo Y. Conditional survival nomogram predicting real-time prognosis of locally advanced breast cancer: analysis of population-based cohort with external validation. Front Public Health. 2022;10: 953992. https://doi.org/10.3389/fpubh.2022.953992.
Huang J, Yan K, Wu C, Tan QC, Bai H, Wang J, et al. Prognosis and conditional nomogram of cervical spine fracture in patients with severe spinal cord injury: a multicenter retrospective study. Int J Surg (London, England). 2023;109(5):1271–80. https://doi.org/10.1097/js9.0000000000000365.
Jung SH, Lee HY, Chow SC. Statistical methods for conditional survival analysis. J Biopharm Stat. 2018;28(5):927–38. https://doi.org/10.1080/10543406.2017.1405012.
Zabor EC, Gonen M, Chapman PB, Panageas KS. Dynamic prognostication using conditional survival estimates. Cancer. 2013;119(20):3589–92. https://doi.org/10.1002/cncr.28273.
Haydu LE, Scolyer RA, Thompson JF. Conditional survival estimates for cancer patients. Oncotarget. 2017;8(49):84639–40. https://doi.org/10.18632/oncotarget.21497.
Grobman WA, Stamilio DM. Methods of clinical prediction. Am J Obstet Gynecol. 2006;194(3):888–94. https://doi.org/10.1016/j.ajog.2005.09.002.
Park SY. Nomogram: an analogue tool to deliver digital knowledge. J Thorac Cardiovasc Surg. 2018;155(4):1793. https://doi.org/10.1016/j.jtcvs.2017.12.107.
Han L, Dai W, Mo S, Xiang W, Li Q, Xu Y, et al. Nomogram of conditional survival probability of long-term survival for metastatic colorectal cancer: a real-world data retrospective cohort study from seer database. Int J Surg (London, England). 2021;92: 106013. https://doi.org/10.1016/j.ijsu.2021.106013.
Doll KM, Rademaker A, Sosa JA. Practical guide to surgical data sets: surveillance, epidemiology, and end results (Seer) database. JAMA Surg. 2018;153(6):588–9. https://doi.org/10.1001/jamasurg.2018.0501.
de Jong MC, Khan S, Christakis I, Weaver A, Mihai R. Comparative performances of nomograms and conditional survival after resection of adrenocortical cancer. BJS Open. 2021; 5(1). https://doi.org/10.1093/bjsopen/zraa036.
Touijer K, Scardino PT. Nomograms for staging, prognosis, and predicting treatment outcomes. Cancer. 2009;115(13 Suppl):3107–11. https://doi.org/10.1002/cncr.24352.
Shariat SF, Capitanio U, Jeldres C, Karakiewicz PI. Can nomograms be superior to other prediction tools? BJU Int. 2009;103(4):492–5. https://doi.org/10.1111/j.1464-410X.2008.08073.x.
Nuersulitan R, Yang M, Mi L, Wu M, Liu X, Ping L, et al. Conditional survival and annual hazard estimates of classical hodgkin lymphoma. Cancer Manage Res. 2021;13:6731–41. https://doi.org/10.2147/cmar.S324543.
Ohori Tatsuo G, Riu Hamada M, Gondo T, Hamada R. Nomogram as predictive model in clinical practice. Cancer Chemothera. 2009;36(6):901–6.
Shariat SF, Karakiewicz PI, Suardi N, Kattan MW. Comparison of nomograms with other methods for predicting outcomes in prostate cancer: a critical analysis of the literature. Clin Cancer Res. 2008;14(14):4400–7. https://doi.org/10.1158/1078-0432.Ccr-07-4713.
Haydu LE, Scolyer RA, Lo S, Quinn MJ, Saw RPM, Shannon KF, et al. Conditional survival: an assessment of the prognosis of patients at time points after initial diagnosis and treatment of locoregional melanoma metastasis. J Clin Oncol. 2017;35(15):1721–9. https://doi.org/10.1200/jco.2016.71.9393.
Ruan DY, Lin ZX, Wang TT, Zhao H, Wu DH, Chen J, et al. Nomogram for preoperative estimation of long-term survival of patients who underwent curative resection with hepatocellular carcinoma beyond barcelona clinic liver cancer stage A1. Oncotarget. 2016;7(38):61378–89. https://doi.org/10.18632/oncotarget.11358.
Anderson C, Smitherman AB, Nichols HB. Conditional relative survival among long-term survivors of adolescent and young adult cancers. Cancer. 2018;124(14):3037–43. https://doi.org/10.1002/cncr.31529.
Mertens AC, Yong J, Dietz AC, Kreiter E, Yasui Y, Bleyer A, et al. Conditional survival in pediatric malignancies: analysis of data from the childhood cancer survivor study and the surveillance, epidemiology, and end results program. Cancer. 2015;121(7):1108–17. https://doi.org/10.1002/cncr.29170.
Carbognin L, Sperduti I, Ciccarese M, Fabi A, Petrucelli L, Vari S, et al. Prognostic model for advanced breast carcinoma with luminal subtype and impact of hormonal maintenance: implications for post-progression and conditional survival. Breast (Edinburgh, Scotland). 2016;29:24–30. https://doi.org/10.1016/j.breast.2016.06.021.
Lin Z, Lin H, Lin C. Dynamic prediction of cancer-specific survival for primary hypopharyngeal squamous cell carcinoma. Int J Clin Oncol. 2020;25(7):1260–9. https://doi.org/10.1007/s10147-020-01671-4.
Bischof DA, Kim Y, Dodson R, Jimenez MC, Behman R, Cocieru A, et al. Conditional disease-free survival after surgical resection of gastrointestinal stromal tumors: a multi-institutional analysis of 502 patients. JAMA Surg. 2015;150(4):299–306. https://doi.org/10.1001/jamasurg.2014.2881.
Kelly PD, Patel PD, Yengo-Kahn AM, Wolfson DI, Dawoud F, Ahluwalia R, et al. Incorporating conditional survival into prognostication for gunshot wounds to the head. J Neurosurg. 2021;135(5):1550–9. https://doi.org/10.3171/2020.9.Jns202723.
Acknowledgements
Not applicable.
Funding
Guizhou Province Qianxinan Prefecture Science and Technology Plan Project, Grant/Award Number: 2023-3-30.
Author information
Authors and Affiliations
Contributions
PL design the project; PL and YY L searched databases and performed literature screen; CH and JG extracted and analyzed the data, analysis; PL and YY L evaluated the quality of included literature; PL, YY L and YX contributed to writing the manuscript. Final draft was approved by all the authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No clinical patient study is conducted in this article, and no ethical statement is required.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, P., Li, Yy., Huang, C. et al. A novel conditional survival nomogram for monitoring real-time prognosis of non-metastatic colorectal cancer. Discov Onc 15, 179 (2024). https://doi.org/10.1007/s12672-024-01042-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-024-01042-9