Abstract
Background/Aim
Lenvatinib, a multikinase inhibitor, has become a second-line treatment option for unresectable liver cancer, while its monotherapy response rate is limited. Hence, we aim to investigate whether one of the epigenetic inhibitors will be synthetic lethal with Lenvatinib in liver cancer cells.
Materials and Methods
We performed high-throughput drug screening in combination with Lenvatinib. And we employed CCK-8-based Bliss Synergy Score analysis, colony formation and western blotting to confirm our screening results in both HepG2 and HCCC9810 cells.
Results
We identified that LSD1 inhibitor Pulrodemstat in combination with Lenvatinib dramatically suppressed the PI3K-AKT signaling and induced a more significant activation of Caspase3 compared to Lenvatinib monotherapy.
Conclusion
Pulrodemstat synergized with Lenvatinib based on suppression of PI3K-AKT signaling and activation of apoptotic signaling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Liver cancer is a major cause of cancer-associated death in the world [1]. Primary liver cancer (PLC) has three main histological subtypes-hepatocellular carcinoma (accounting for approximate 90% of liver cancers), intrahepatic cholangiocarcinoma (ICC) and combined hepatocellular and intrahepatic cholangiocarcinoma (CHC) [2, 3]. Multikinase inhibitor, including Sorafenib and Lenvatinib, has been successfully used for clinical treatment for liver cancer patients [4]. Although Lenvatinib is not yet a first-line treatment option for unresectable liver cancer like Atezolizumab plus Bevacizumab, it is non-inferior to Sorafenib and has become a second-line treatment option for unresectable liver cancer [5,6,7,8]. Yet, the efficacy of Lenvatinib alone remains limited, which calls for the investigation of potential drug combination treatments to improve the therapeutic effect of Lenvatinib.
Epigenetic dysregulation is one of the Hallmarks of Cancer [9]. Accumulated evidence revealed that targeting epigenetic modifiers is not only a highly promising treatment for cancers but also an important way to overcome the multiple drug resistance [10]. Therefore, large number of inhibitors are in robust development that aim to blocking epigenetic modulators, including writers, erasers and readers[11]. To date, epigenetic drugs have already achieved an inspiring clinical benefits in combination with chemotherapy [12], hormone therapy [13], antiangiogenic therapy [14], targeted therapy [15] and radiotherapy [16] which enlarge the scope of utilization of epigenetic drugs. While, little is known whether epigenetic drugs could be a sensitizer for Lenvatinib in liver cancer. Hence, we performed an epigenetic drug synergy screening to identify new strategies for expanding the use of Lenvatinib.
Aberrant activation of PI3K-AKT signaling is the one of the major causes of the limited response of Lenvatinib [17, 18]. On the contrary, restriction of PI3K-AKT signaling activation contributes to the response of Lenvatinib [19]. Lysine Specific Demethylase 1 (LSD1, also known as KDM1A), a key histone demethylase, regulates gene transcription via demethylating H3K9me2 or H3K4me1/2 [20]. LSD1 has been indicated to promote the multiple cancer progression [21,22,23,24]. LSD1 inhibitors currently undergo clinical assessment in hematologic malignancies and solid tumors [25]. Notably, LSD1 depletion has been reported to suppress activation of PI3K-AKT signaling [26, 27]. Taken together, these evidences suggest that LSD1 inhibitor is a plausible candidate that possesses the giant potential for Lenvatinib sensitization in liver cancer.
Here, Lenvatinib combined with a variety of epigenetic drugs was applied to liver cancer cells. Pulrodemstat, a LSD1 inhibitor, exhibited the most effective inhibitor in increasing the efficacy of Lenvatinib. Mechanistically, Pulrodemstat synergized with Lenvatinib based on suppression of PI3K-AKT signaling and activation of apoptotic signaling.
2 Results
2.1 Epigenetic drug screening identifies pulrodemstat as a potential sensitizer for lenvatinib in liver cancer cells
To investigate whether targeting epigenetic modulator has an impact on the Lenvatinib sensitivity in hepatocellular carcinoma, we performed an epigenetic drug screening in hepatocellular carcinoma cell line, HepG2. As shown in Fig. 1A, thirty-nine preclinical and clinical “eraser” inhibitors were subjected to screening in combination with Lenvatinib. The visualization of drug screening was achieved in a heatmap (Fig. 1B). As the results shown, several epigenetic drugs were shown a much stronger cell-killing function in comparison with Lenvatinib even though the concentration we chose was only half of the Lenvatinib which indicated that epigenetic modulators were the critical therapeutic target for hepatocellular carcinoma and cholangiocarcinoma cells and these candidates will be chosen for our further studies. Notably, Lenvatinib exhibited a much more suppressive effect when combined with Pulrodemstat. Collectively, our screening results not only indicated that epigenetic modulators were the highly promising therapeutic targets but also unveiled that Pulrodemstat as a potential sensitizer for Lenvatinib in liver cancer.
Pulrodemstat is a potential sensitizer for Lenvatinib in liver cancer cells. A The flow work of epigenetic drugs screening. B The heatmap summarizing the synergistic effects of 39 epigenetic inhibitors and Lenvatinib in HepG2 cells. The color intensity depicts the inhibitory rate with indicated treatment. HepG2 cells treated with Lenvatinib (10 μM), epigenetic drugs (5 μM) or the mixed two drugs for 96 h
2.2 Pulrodemstat synergizes with lenvatinib in hepatocellular carcinoma and cholangiocarcinoma cells
Inspired by the high-throughput drug screening results, we therefore evaluated the synergy score between these two drugs in two liver cancer cell lines. In consistence with our hypothesis, drug combination between Pulrodemstat and Lenvatinib was synergistic in two liver cancer cell lines, as shown by the Bliss Synergy Score (Fig. 2A, B). Intriguingly, although some concentrations of Pulrodemstat or Lenvatinib monotherapy didn’t lead to cell growth inhibition, the combination strongly blunted the cell viability which indicated LSD1-mediated epigenetic reprogramming was critical for Lenvatinib to achieve its function on RTK inhibition (Fig. 2A, B and Additional file 1: Table S2). Moreover, we employed colony formation assay to support the result of synergy score and found Pulrodemstat or Lenvatinib mono-treatment merely inhibited the tumorigenic function of liver cancer cells, while the combination of these two drugs drastically blunted cell growth (Fig. 2C, D). Taken together, these results raised a potent drug combination which may expanding the population for which the Lenvatinib was indicated.
Pulrodemstat synergizes with Lenvatinib in hepatocellular carcinoma and cholangiocarcinoma cells. A, B Loewe plots highlight the drug synergism between indicated drugs. For the HepG2, the Lenvatinib was gradient from 0 to 10 μM in combination with Pulrodemstat from 0 to 5 μM. As for the HCCC9810 the Lenvatinib was gradient from 0 to 20 μM in combination with Pulrodemstat from 0 to 5 μM. C, D The anti-tumor potential of indicated treatment was determined by colony formation assay. HepG2 and HCCC9810 cells were treated with Lenvatinib (5 μM), Pulrodemstat (2.5 μM) or the mixed two drugs for at least two weeks
2.3 LSD1 expression predicts the prognosis of liver cancer
Our screening and validation results driven us to explore the clinical prediction role of LSD1 in liver cancer. Based on TCGA analysis, we found LSD1 was frequently overexpressed across human cancers which indicated LSD1 might be a pan-cancer therapeutic target (Fig. 3A). Next, we focus on LSD1 expression in liver cancer. Notably, LSD1 was drastically overexpressed in liver cancer tumor tissues in comparison with normal tissues (Fig. 3B). Additionally, we found LSD1 was positively correlated with the degree of malignancy of hepatocellular carcinoma, as evidenced by higher expression levels of LSD1 in late-stage liver cancer compared with other stages (here, samples of stage IV had been excluded due to the small sample size), indicating LSD1 might contribute to the de novo resistance of Lenvatinib in patients with late-stage liver cancer (Additional file 1: Figure S1). Moreover, LSD1 expression levels were also significantly higher in the metastatic liver cancer samples in comparison with both normal and tumor tissues (Fig. 3B). More importantly, we noticed that aberrantly high expression of LSD1 predicted the shorter overall survival (OS, Logrank p = 2.5 × 10–6) and progress free survival (PFS, Logrank p = 3.2 × 10–3) (Fig. 3C, D). These data highlighted LSD1 might be a potential therapeutic target and biomarker for liver cancer. Thought-provokingly, these results and our in vitro functional analysis might give an explanation why the therapeutic effect of Lenvatinib is limited and further supported our hypothesis that LSD1 inhibitor might expand the population for which the Lenvatinib was indicated.
LSD1 expression predicts the prognosis of liver cancer. A TCGA RNA-sequencing data indicated that LSD1 transcripts were aberrantly high across cancers. B TCGA RNA-sequencing data indicated that LSD1 was highly expressed in liver cancer or Metastatic liver cancer tissues in comparison with normal tissues. C Kaplan–Meier plots analysis of overall survival rates (OS) in liver cancer patient with high or low LSD1 mRNA levels. Patient number at risk at different times of analysis was shown at the bottom of the plots. D Kaplan–Meier plots analysis of progress free survival rates (PFS) in liver cancer patients with high or low LSD1 mRNA levels. Patient number at risk at different times of analysis was shown at the bottom of the plots
2.4 Pulrodemstat-mediated epigenetic reprogramming promotes the inhibitory function of Lenvatinib on PI3K-AKT signaling
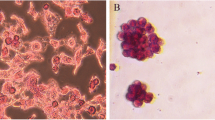
Inactivation of PI3K-AKT signaling is critical for the anti-tumor function of Lenvatinib [17]. And, reactivation of PI3K-AKT is the key mechanism for RTK drug resistance including Lenvatinib [19]. Meanwhile, accumulated evidence revealed that LSD1 is a positive regulator of PI3K-AKT signaling pathway [26, 27]. Based on this, we hypothesize that Pulrodemstat might enhance the Lenvatinib by promoting its inhibitory function on PI3K-AKT signaling. To confirm our hypothesis, we employed immunoblotting analysis and found the combined treatment of Lenvatinib and Pulrodemstat drastically blunted activation of PI3K-AKT signaling cascade in comparison with control or Lenvatinib monotherapy in both liver cancer cell lines as shown by decreased the phosphorylation levels of PI3K and AKT (Fig. 4A, B). Inactivation of PI3K-AKT signaling pathway is known to induce the cleaved caspase 3 levels which is a marker of apoptosis [28]. Consistent with this, morphological observation suggested that the combined treatment led to cell death, as evidenced by the shrunken cell morphology (Fig. 4C). Meanwhile, we observed that Lenvatinib and Pulrodemstat co-treatment led to the significantly elevated of cleaved caspase 3 without affecting the total caspase 3 expression in both liver cancer cell lines (Fig. 4D, E). Take all together, our data roughly indicated Pulrodemstat synergized with Lenvatinib based on suppression of PI3K-AKT signaling and the follow-up activation of apoptotic signaling.
Pulrodemstat promotes the inhibitory function of Lenvatinib on PI3K-AKT signaling and induces the activation of apoptosis. A, B IB analysis of PI3K-AKT signaling upon indicated treatment as the colony formation assay. C Cells were treated with indicated drugs for 96 h and then photographed. D, E IB analysis of the activation of apoptotic signaling upon indicated treatment as the colony formation assay
3 Discussion
TKIs, including Sorafenib and Lenvatinib, has been utilized as the second-line treatment for the unresectable liver cancer [6]. During the clinical observation, liver cancer patients are easily to develop Sorafenib resistance [29]. Although Lenvatinib had significantly longer progression-free survival than Sorafenib, relapse remains inevitable [6]. Additionally, Lenvatinib also has been suggested to be a therapeutic option for Advanced and Unresectable Intrahepatic Cholangiocarcinoma [30]. Unfortunately, the response rate of Lenvatinib is limited [6]. It can’t be ignored that several adverse effects were accompanied with Lenvatinib monotherapy including hypertension, diarrhea, fatigue or asthenia, decreased appetite, and weight loss [31]. The drug combination based on precise feature of cancers shows the light to improving efficacy while minimizing adverse events. Turn back to Lenvatinib, reactivation of the key nodes of RTK signaling is the main cause that limit the drug response rate and resistance [19, 32]. Meanwhile, epigenetic drugs have been suggested to synergize with multiple clinical used drugs [12,13,14,15,16, 33, 34]. However, whether epigenetic drugs can improve the therapeutic efficacy of Lenvatinib in liver cancer need to be better investigated.
By performing a drug synergy screening, we identify Pulrodemstat as a potent Lenvatinib sensitizer. Our results demonstrated pharmaceutical inhibition of LSD1 by Pulrodemstat drastically increased the Lenvatinib sensitivity in liver cancer cell lines. Accumulated evidence reveals that LSD1 as an oncogene, participates in promoting tumor progression [22], metastasis [24] and drug resistance [21] which highlights that LSD1 is a highly promising therapeutic target across the cancers. Precisely for this reason, several LSD1 inhibitors have undergone clinical trial ranged from phase I to phase II [25]. Notably, some LSD1 inhibitors also exhibited therapeutic potentials in clinical investigation in MDS, myelofibrosis and Alzheimer’s disease [35,36,37]. Therefore, our research might not only provide a new aspect of LSD1 inhibitor application in liver cancer therapy but also present a certain clinical benefit once LSD1 inhibitor is indeed used in clinical.
Lenvatinib is one of TKIs and PI3K-AKT serves as the key note for the RTK signaling transduction [5]. Therefore, many investigations suggest reactivation or constituted activation of PI3K-AKT signaling contributes to the TKIs resistance or limits TKIs therapeutic efficacy [19]. Meanwhile, LSD1 is reported to contribute to the activation of PI3K-AKT signaling by transcriptional activating the upstream of PI3K [26, 27]. In this story, our data unveil pharmaceutical disruption of the regulatory of PI3K by LSD1 is sufficient to elevate the response of Lenvatinib in liver cancer cell lines. Moreover, our bioinformatic analysis reveals LSD1 transcripts are overexpressed in liver cancer in comparison with normal liver tissues which may provide a potent explanation why the clinical use of Lenvatinib is limited and further support the clinical value of our study. We did not perform in vivo experiments due to the limitations of experimental conditions. However, given the remarkable results of cellular experiments, we believe that our study is expected to provide a new therapeutic strategy for the clinical treatment of liver cancer.
In conclusion, our high-throughput drug combination screening unveiled that targeting the critical therapeutic target-LSD1, is sufficient to enhance the therapeutic efficacy of Lenvatinib in liver cancer cell lines via disrupting the PI3K-AKT signaling transduction and therefore triggering the apoptotic events.
4 Materials and methods
4.1 Cell culture
HepG2, a hepatocellular carcinoma cell line, was purchased from ATCC and HCCC9810, an intrahepatic cholangiocarcinoma cell line, was obtained from Procell (Catalog, CL-0095). HepG2 and HCCC9810 cells were individually cultured in DMEM (Gibco) or RPM1640 (Gibco) containing 10% FBS. Cells were maintained at 37 °C in a saturated humidity atmosphere containing 95% air and 5% CO2.
4.2 IC50 determination
HepG2 and HCCC9810 cells were seeded as 3000 cells per well in 96-well plate. After being cultured for 24 h, the media containing gradient diluted Lenvatinib (from 40 μM) was used to replace the old media and then continued to be cultured for 96 h. The cell viability was determined by CCK-8 assay. In this assay, the IC50 of Lenvatinib in these two cell lines were approximate 12.25 and 23.86 μM and these concentrations were selected for the further bliss score related experiments.
4.3 Drug screening
Epigenetic drugs were purchased from MedChemExpress (Shanghai, China), pre-dissolved in DMSO or distilled water, and stocked at − 80 °C according to the product data sheets. Details of indicated drugs were listed in Additional file 1: Table S1.
HepG2 cells were seeded as 3000 cells per well in 96-well plate, incubated for 24 h, and then treated with Lenvatinib (10 μM), epigenetic drugs (5 μM) or the mixed two drugs for 96 h. After treatment for indicated time window, the cell viability was determined by CCK-8 assay.
4.4 CCK8
The CCK-8 kit (MedChemExpress) was utilized to detect cell viability and proliferation. After incubated as indicated time window, the OD value was measured at 450 nm following a 2 h incubation with fresh media containing 10 μl of CCK-8 solution per well.
4.5 Western blotting
Cell lysis, SDS-PAGE, and western blot were performed using standard methods as described [16]. For Western blot analysis, the following antibodies were used: anti-phospho-PI3K p85 (Cell signaling technology, Danvers, MA, USA), anti-phospho-PI3K p85 (Tyr-458) (Cell signaling technology, Danvers, MA, USA), anti-AKT (Cell signaling technology, Danvers, MA, USA), anti-phospho-AKT (Ser-473) (Cell signaling technology, Danvers, MA, USA), anti-Caspase 3 (Cell signaling technology, Danvers, MA, USA), anti-Cleaved-Caspase 3 (Asp175) (Cell signaling technology, Danvers, MA, USA)and anti-β-actin (Sigma, St. Louis, MO, USA).
4.6 Colony formation
Based on a previous study [38], HepG2 and HCCC9810 cells were seeded as 3000 cells per well in 6-well plate. After cultured for 24 h, cells were treated with Lenvatinib (5 μM), Pulrodemstat (2.5 μM) or the mixed two drugs for 1 week and add 1 ml fresh media containing indicated drugs every 2 day. After 1 week, the cells were fixed by methanol and then stained by Cristal Violet.
5 Bioinformatic analysis
The LSD1 transcripts levels in pan-Cancer and liver cancer were analyzed by using TNM plot [5] (https://tnmplot.com/analysis/). And the survival plot was drawn in GEPIA 2.0 (http://gepia2.cancer-pku.cn).
6 Statistical analysis
Results were reported as mean ± SEM of 3 or more independent experiments. Statistical significance was examined using a two-tailed Student t test. Statistical calculations were executed using GraphPad Prism software, version 8.0 (GraphPad Software, Inc., San Diego, California).
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Ju PC, et al. Kaempferol inhibits the cell migration of human hepatocellular carcinoma cells by suppressing MMP-9 and Akt signaling. Environ Toxicol. 2021;36(10):1981–9.
Marquardt JU, Andersen JB, Thorgeirsson SS. Functional and genetic deconstruction of the cellular origin in liver cancer. Nat Rev Cancer. 2015;15(11):653–67.
Donne R, Lujambio A. The liver cancer immune microenvironment: Therapeutic implications for hepatocellular carcinoma. Hepatology. 2023;77(5):1773–96.
Llovet JM, et al. Sorafenib in advanced hepatocellular carcinoma. N Engl J Med. 2008;359(4):378–90.
Zhao Y, et al. Lenvatinib for hepatocellular carcinoma: from preclinical mechanisms to anti-cancer therapy. Biochim Biophys Acta Rev Cancer. 2020;1874(1): 188391.
Kudo M, et al. Lenvatinib versus sorafenib in first-line treatment of patients with unresectable hepatocellular carcinoma: a randomised phase 3 non-inferiority trial. Lancet. 2018;391(10126):1163–73.
Casak SJ, et al. FDA approval summary: atezolizumab plus bevacizumab for the treatment of patients with advanced unresectable or metastatic hepatocellular carcinoma. Clin Cancer Res. 2021;27(7):1836–41.
Finn RS, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–905.
Hanahan D. Hallmarks of cancer: new dimensions. Cancer Discov. 2022;12(1):31–46.
Hogg SJ, et al. Targeting the epigenetic regulation of antitumour immunity. Nat Rev Drug Discov. 2020;19(11):776–00.
Conery AR, Rocnik JL, Trojer P. Small molecule targeting of chromatin writers in cancer. Nat Chem Biol. 2022;18(2):124–33.
Glasspool RM, et al. A randomised, phase II trial of the DNA-hypomethylating agent 5-aza-2’-deoxycytidine (decitabine) in combination with carboplatin vs carboplatin alone in patients with recurrent, partially platinum-sensitive ovarian cancer. Br J Cancer. 2014;110(8):1923–9.
Munster PN, et al. A phase II study of the histone deacetylase inhibitor vorinostat combined with tamoxifen for the treatment of patients with hormone therapy-resistant breast cancer. Br J Cancer. 2011;104(12):1828–35.
Jiang Z, et al. Tucidinostat plus exemestane for postmenopausal patients with advanced, hormone receptor-positive breast cancer (ACE): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Oncol. 2019;20(6):806–15.
Bitzer M, et al. Resminostat plus sorafenib as second-line therapy of advanced hepatocellular carcinoma - The SHELTER study. J Hepatol. 2016;65(2):280–8.
Ni M, et al. BRD4 inhibition sensitizes cervical cancer to radiotherapy by attenuating DNA repair. Oncogene. 2021;40(15):2711–24.
Ye J, et al. Lenvatinib induces anticancer activity in gallbladder cancer by targeting AKT. J Cancer. 2021;12(12):3548–57.
Buttell A, Qiu W. The action and resistance mechanisms of Lenvatinib in liver cancer. Mol Carcinog. 2023;62(12):1918–34.
Lu Y, et al. Genome-scale CRISPR-Cas9 knockout screening in hepatocellular carcinoma with lenvatinib resistance. Cell Death Discov. 2021;7(1):359.
Metzger E, et al. LSD1 demethylates repressive histone marks to promote androgen-receptor-dependent transcription. Nature. 2005;437(7057):436–9.
Sheng W, et al. Simultaneous inhibition of LSD1 and TGFbeta enables eradication of poorly immunogenic tumors with anti-PD-1 treatment. Cancer Discov. 2021;11(8):1970–81.
Li H, et al. YAP/TAZ drives cell proliferation and tumour growth via a polyamine-eIF5A hypusination-LSD1 axis. Nat Cell Biol. 2022;24(3):373–83.
Faletti S, et al. LSD1-directed therapy affects glioblastoma tumorigenicity by deregulating the protective ATF4-dependent integrated stress response. Sci Transl Med. 2021;13(623):7036.
Gong Z, et al. OTUD7B deubiquitinates LSD1 to govern its binding partner specificity, homeostasis, and breast cancer metastasis. Adv Sci. 2021;8(15): e2004504.
Fang Y, Liao G, Yu B. LSD1/KDM1A inhibitors in clinical trials: advances and prospects. J Hematol Oncol. 2019;12(1):129.
Chen C, et al. LSD1 sustains estrogen-driven endometrial carcinoma cell proliferation through the PI3K/AKT pathway via di-demethylating H3K9 of cyclin D1. Int J Oncol. 2017;50(3):942–52.
Miller SA, et al. Lysine-specific demethylase 1 mediates AKT activity and promotes epithelial-to-mesenchymal transition in PIK3CA-mutant colorectal cancer. Mol Cancer Res. 2020;18(2):264–77.
Lim FQ, et al. Targeting dual oncogenic machineries driven by TAL1 and PI3K-AKT pathways in Tcell acute lymphoblastic leukemia. Haematologica. 2022. https://doi.org/10.3324/haematol.2022.280761.
Huang M, et al. New insights into antiangiogenic therapy resistance in cancer: mechanisms and therapeutic aspects. Drug Resist Updat. 2022;64: 100849.
Shi GM, et al. Toripalimab combined with lenvatinib and GEMOX is a promising regimen as first-line treatment for advanced intrahepatic cholangiocarcinoma: a single-center, single-arm, phase 2 study. Signal Transduct Target Ther. 2023;8(1):106.
Cabanillas ME, Takahashi S. Managing the adverse events associated with lenvatinib therapy in radioiodine-refractory differentiated thyroid cancer. Semin Oncol. 2019;46(1):57–64.
Jin H, et al. EGFR activation limits the response of liver cancer to lenvatinib. Nature. 2021;595(7869):730–4.
Kwon NH, et al. DNA methylation and the expression of IL-4 and IFN-gamma promoter genes in patients with bronchial asthma. J Clin Immunol. 2008;28(2):139–46.
Yardley DA, et al. Randomized phase II, double-blind, placebo-controlled study of exemestane with or without entinostat in postmenopausal women with locally recurrent or metastatic estrogen receptor-positive breast cancer progressing on treatment with a nonsteroidal aromatase inhibitor. J Clin Oncol. 2013;31(17):2128–35.
Christopher MA, et al. LSD1 protects against hippocampal and cortical neurodegeneration. Nat Commun. 2017;8(1):805.
Gill H. Lysine-specific demethylase 1 (LSD1/KDM1A) inhibition as a target for disease modification in myelofibrosis. Cells. 2022. https://doi.org/10.3390/cells11132107.
Wu B, et al. Epigenetic drug library screening identified an LSD1 inhibitor to target UTX-deficient cells for differentiation therapy. Signal Transduct Target Ther. 2019;4:11.
Sang N, et al. Pharmacological inhibition of LSD1 suppresses growth of hepatocellular carcinoma by inducing GADD45B. MedComm. 2023;4(3):269.
Acknowledgements
This study was supported by the fourth affiliated hospital, Zhejiang University school of medicine.
Author information
Authors and Affiliations
Contributions
Yi Zong performed the most experiments and Minyuan Wang performed the bioinformatic analysis. Yi Zong, Zhigang Tao and Weihua Yu prepared the initial version of the paper. Yi Zong, Siyi Jiang and Weihua Yu designed the study, performed the literature review, and prepared the final versions of the paper.
Corresponding author
Ethics declarations
Competing interests
The Authors declare no competing interests regrading this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file1: Table S1.
Details of drug library and related IC50. Table S2. Cell viability details for each combination in Figure 2A-B Figure S1. analysis of LSD1 expressions in different liver hepatocellular carcinomas (LIHC) based UALCAN, a TCGA based webtool.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Zong, Y., Tao, Z., Jiang, S. et al. Repression of LSD1/KDM1A activity improves the response of liver cancer cells to the lenvatinib. Discov Onc 15, 89 (2024). https://doi.org/10.1007/s12672-024-00947-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-024-00947-9