Abstract
Objective
This study aimed to evaluate the clinical effectiveness of chemotherapy following immune checkpoint inhibitors (ICI). The association between inflammatory and nutritional factors and prognosis has also been investigated.
Methods
We retrospectively reviewed the medical records of recurrent or metastatic head and neck squamous cell carcinoma (RMHNSCC) patients who received chemotherapy following ICI therapy. The response rate and survival after chemotherapy, and nutritional and inflammatory factors, were examined.
Results
The ICI before chemotherapy was nivolumab in 36 patients (70.6%) and pembrolizumab in 15 patients (29.4%). The chemotherapy regimens consisted of PTX in 32 patients (62.7%), PTX + Cmab in 9 (17.6%), and S1 in 10 (19.6%). The median overall survival (OS) was 20 months (95% CI 12–25), the estimated 12-month OS rate was 63.3%, the median progression-free survival (PFS) was 5 months (CI 4–6), and the 12-month PFS estimate was 8.9%. Univariate analysis significantly correlated Neutrophil-to-Lymphocyte Ratio (NLR), platelet-to-lymphocyte ratio (PLR), controlling nutritional status score (CONUT), and prognostic nutrition index (PNI) with OS and PFS. Additionally, these factors were significantly correlated with OS and PFS in the log-rank tests.
Conclusions
Chemotherapy following ICI is highly effective. There were no significant differences in the chemotherapy regimens. Inflammatory and nutritional factors may associate with patient prognosis after chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Various chemotherapy regimens have been used to treat recurrent and recurrent or metastatic head and neck squamous cell carcinoma (RMHNSCC), but their prognosis remains poor [1,2,3,4,5,6]. However, treatment with a recently approved immune checkpoint inhibitor (ICI) has significantly prolonged the prognosis of RMHNSCC patients compared to conventional chemotherapy [7, 8]. In addition, adverse events were less severe than chemotherapy [9, 10], and treatment was possible while maintaining the patient's quality of life. Therefore, ICI has become widely used as the first-choice treatment for RMHNSCC. However, the response rates in the Checkmate 141 [7] and Keynote 048 [8] trials were 13.3% and 16.9% (pembrolizumab alone), respectively, and chemotherapy was the subsequent treatment of choice for nonresponders. Chemotherapy for patients with disease progression after ICI treatment is effective, and regimens combining platinum, cetuximab (Cmab), paclitaxel (PTX), and tegafur–gimeracil–oteracil potassium (S1) have been reported to date [11,12,13,14,15,16]. However, it is currently unclear which regimen is most effective in patients with RMHNSCC. Furthermore, several inflammatory and nutritional factors have been reported to be associated with prognosis [17,18,19,20,21,22,23,24]. However, few studies have examined the association with the efficacy or prognosis of chemotherapy in RMHNSCC [25]. The neutrophil-to-lymphocyte ratio (NLR) is a well-known prognostic factor for head and neck cancer [26]. Furthermore, various factors that can be easily assessed through blood tests, including the platelet to lymphocyte ratio (PLR) [27, 28], lymphocyte to monocyte ratio (LMR) [29], systemic immune-inflammation index (SII) [30, 31], C-reactive protein (CRP) to albumin ratio (CAR) [32, 33], controlling nutritional status (CONUT) score [18, 34], prognostic nutrition index (PNI) [23, 35], prognostic index (PI) [36], and the Glasgow Prognostic Score (GPS) [17], have been identified as valuable indicators for predicting the prognosis of individuals undergoing treatment for head and neck cancer [27, 28, 32, 33, 37]. However, it is unclear whether they are helpful in subsequent chemotherapy following ICI for RMHNSCC.
This study aimed to evaluate the clinical effectiveness of chemotherapy following ICI therapy. In addition, the effectiveness and response rates of each regimen were examined. Moreover, we investigated whether inflammatory and nutritional factors were associated with the effectiveness of chemotherapy following ICI in RMHNSCC, and also examined their correlation with the prognosis.
2 Materials and methods
2.1 Patient and data collection
We retrospectively reviewed the medical records of RMHNSCC patients who received ICI at Tokai University Hospital in Kanagawa, Japan, from April 2017 to June 2022 and those who received chemotherapy after receiving ICI. Patients were included if they had an Eastern Cooperative Oncology Group (ECOG) performance status of (0–2), had received at least one cycle of immunotherapy, had adequate hematologic, hepatic, pulmonary and renal functions, and could be imaged or clinically evaluated after chemotherapy.
Nivolumab was administered to patients every 2 weeks at 3 mg/kg or 240 mg/body doses. Pembrolizumab was administered at a dose of 200 mg every 3 weeks. After disease progression, chemotherapy with PTX, paclitaxel + cetuximab (PTX + Cmab), or S1 was administered.
PTX was administered at 100 mg/m2 once a week for 3 weeks, followed by a 1-week rest period. PTX + Cmab was initially administered with Cmab at 400 mg/m2 and 250 mg/m2 weekly. PTX was administered once weekly at a dose of 80 mg/m2, and S1 was administered at 80–120 mg/body/day, depending on the body surface area. S1 was administered for 2 weeks, followed by a 1-week rest period. Chemotherapy was selected and was decided at our multidisciplinary head and neck cancer conference based on each patient's condition. As a standard procedure, PTX or S1 was selected for patients with a history of Cmab use or pulmonary complications. S1 was also prescribed for patients over 80 years old and those who preferred outpatient treatment with oral therapy. For other cases, the combination of PTX and Cmab was utilized. Chemotherapy was continued until disease progression or unacceptable toxicity was observed, and the patients were followed up until death or the cutoff date (June 30, 2022).
The Institutional Review Board of Tokai University Hospital (20R248 and 22R223) approved this study, which was conducted according to the principles of the Declaration of Helsinki. Furthermore, the requirement for informed consent was waived because this study was a retrospective analysis of existing administrative and clinical data.
The clinical response to treatment was assessed every 4–12 weeks using computed tomography (CT). Tumor response was evaluated according to (Response Evaluation Criteria in Solid Tumors) version 1.1. The objective response rate (ORR) was defined as the percentage of patients who achieved a complete response (CR) or partial response (PR) as the best response. The disease control rate (DCR) was defined as the percentage of patients with CR, PR, or stable disease (SD) with the best response.
Overall survival (OS) was defined as the time from the start of treatment to the date of death or cutoff, regardless of the cause. Progression-free survival (PFS) was defined as the time from the beginning of treatment to the cutoff date when disease progression, death from any reason, or progression was no longer observed. The duration of response was defined as the time from the initial response (SD, PR, PD) to disease progression. Adverse events (AEs) were recorded using the National Cancer Institute Common Terminology Criteria for Adverse Events version (4.0).
2.2 Definitions of inflammatory and nutritional factors
Albumin (Alb), C-reactive protein (CRP), and total cholesterol levels in serum and leukocytes, including neutrophils, lymphocytes, and monocytes, and platelet counts in peripheral blood were determined by blood analysis before starting chemotherapy. Based on the results, the values of following parameters were calculated: LMR, the ratio of lymphocyte count to monocyte count; NLR, the ratio of neutrophil count to lymphocyte count; PLR, the ratio of platelet count to lymphocyte count; CAR, the ratio of serum CRP level to serum Alb level; CONUT score, calculated using the serum Alb level, total lymphocyte count, and total cholesterol level; GPS, measured using the serum CRP level and serum Alb level: A CRP level > 1.0 mg/dL and Alb level < 3.5 g/dL were given a score of 2, a CRP level > 1.0 mg/dL or Alb level < 3.5 g/dL was given a score of 1, and a CRP level ≤ 1.0 mg/dL and Alb level ≥ 3.5 g/dL were given a score of 0.; PNI, which is 10 × serum Alb level + 0.005 × total lymphocyte count; and PI, measured using the serum CRP level and white bllod cell (WBC) count: PI 0 for CRP 1 mg/dL or less and WBC 11,000/μL or less, PI 1 if one of the two markers was elevated, and PI 2 if both markers were elevated.
2.3 Statistical analysis
OS and PFS were estimated using the Kaplan–Meier method and evaluated using the log-rank test. The association between ORR, DCR, and subsequent chemotherapy groups was tested using the Kruskal–Wallis test for comparison of the three groups. Cutoff values for nutritional and inflammatory factors were determined by referring to ROC curves and were classified into two groups (high and low). The association between ORR, DCR, and each factor was assessed using the univariate logistic regression model. A Cox regression model analyzed the relationship between nutritional and inflammatory factors and OS or PFS. Logistic regression model and Cox regression model analyses were performed using EZR (Saitama Medical Center, Jichi Medical University, Japan), and other statistical analyses were performed using GraphPad Prism 8 software (GraphPad Software Inc., San Diego, CA, USA). Statistical significance was set at p < 0.05.
3 Results
3.1 Patient characteristics
From June 2017 to June 2022, 51 of the 110 RMHNSCC patients treated with ICI were eligible for treatment evaluation after chemotherapy following ICI. Their characteristics are summarized in Table 1. There were 48 males and three females with a median age of 66 years (range: 47–83 years). In 24 cases, the primary site was the hypopharynx, the oropharynx in 11 cases, and the larynx in 7 cases. The ECOG was 0–1 in almost all cases. The disease sites evaluated were locoregional recurrence in 32 cases and distant metastases in 19 cases. Regarding the line of chemotherapy, 43 cases received chemotherapy as second-line treatment after ICI, 7 cases for 3rd, and 1 for 4th. The type of ICI before chemotherapy was nivolumab in 36 patients and pembrolizumab in 15 patients. Regarding prior cetuximab treatment before ICI, seven patients received it, and 44 patients had never received it. The chemotherapy regimens consisted of PTX in 32 cases (62.7%), PTX + Cmab in 9 cases (17.6%), and S1 in 10 cases (19.6%).
3.2 Effectiveness of subsequent chemotherapy
The ORR for patients after chemotherapy following ICI was 71.2% (37/51), and the DCR was 84.6% (44/51) (Table 2). The ORR by chemotherapy was 78.1% (25/32 patients), 88.9% (8/9 patients), and 40.0% (4/10 patients) for PTX, PTX + Cmab, and S1, respectively. DCR was 87.5% (28/32), 100% (9/9), and 70.0% (7/10). There was no significant difference in the ORR, but there was a significant difference in the ORR among the three groups.
Figure 1 shows the estimated OS (Fig. 1a) and PFS (Fig. 1b) after the first dose of chemotherapy with ICI. The median OS was 10 months (95% CI 6–18), and the estimated 12-month OS rate was 44.5% (Fig. 1a). The median PFS was 5 months (95% CI 4–6), and the 12-month PFS estimate was 8.9%. The OS after chemotherapy (Fig. 2a) and PFS (Fig. 2b) are shown. No significant differences in OS and PFS were observed between the chemotherapy groups.
Kaplan–Meier curves of overall survival (a) and progression-free survival (b) for patients after chemotherapy following immune checkpoint inhibitor therapy. The median OS was 10 months (95% CI 6–18), and the estimated 12-month OS rate was 44.5% (a). The median PFS was 5 months (95% CI 4–6), and the 12-month PFS estimate was 8.9%
3.3 Adverse event
The adverse events observed during chemotherapy are listed in Table 3. The most common AE was peripheral neuropathy in 6 patients (11.5%). The most common was thyroid dysfunction, pneumonia, liver dysfunction, and skin toxicity. Grade 3 or higher adverse events were observed in 10 patients (19.6%), and one died of interstitial pneumonia.
3.4 Prognostic analysis of patients who received chemotherapy following immune checkpoint inhibitors therapy
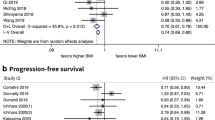
ORR, DCR and nutritional and inflammatory factors were analyzed for chemotherapy after ICI therapy (Table 4). Regarding the CUTOFF values (area under the curve) of each factor, BMI Cutoff: 20 (0.665), albumin cutoff: 3.5 (0.654), CRP Cutoff: 1.2 (0.672), LMR Cutoff: 2.5 (0.710), NLR Cutoff: 4.5 (0.659), PLR Cutoff: 268 (0.683), CAR Cutoff: 0.58 (0.678), CONUT Cutoff: 4 (0.703), and PNI Cutoff: 40 (0.715). No significant correlation was found between ORR or DCR and each factor. However, there was a trend for ORR to be associated with Age (odds ratio (OR) = 0.30, 95% confidence interval (CI) 0.08–1.09, P = 0.07) and for DCR to be associated with the NLR (OR = 6.57, 95% CI 0.73–59.2, P = 0.09) and PLR (OR = 4.37, 95% CI 0.76–25.2, P = 0.09). Table 5 shows the results of the Cox regression analysis between nutritional and inflammatory factors and OS and PFS in patients after chemotherapy. Examination of OS and nutritional and inflammatory factors showed significant correlations with Alb (hazard ratio (HR) = 3.00, 95% CI 1.49–6.04, P = 0.002), NLR (HR = 0.40, 95% CI 0.20–0.83, P = 0.013), PLR (HR = 0.26, 95% CI 0.12–0.55, P < 0.001), CAR (HR = 0.41, 95% CI 0.21–0.83, P = 0.012), CONUT score (HR = 0.25, 95% CI 0.12–0.52, P < 0.001), and PNI (HR = 4.32, 95% CI 2.03–9.16, P < 0.001). In addition, there was a significant correlation between PFS and NLR (HR = 0.53, 95% CI 0.28–0.98, P = 0.044), PLR (HR = 0.46, 95% CI 0.25–0.87, P = 0.016), CONUT score (HR = 0.50, 95% CI 0.26–0.95, P = 0.035), and PNI (HR = 2.36, 95% CI 1.27–4.38, P = 0.006).
Figure 3 shows the results of Kaplan–Meier survival curves and log-rank tests by cutoff values for NLR, PLR, CONUT score, and PNI, which were highly correlated with OS and PFS using the Cox regression model. Significant differences in OS and PFS were observed between the two groups for NLR (p = 0.0088, p = 0.264), PLR (p = 0.0001, p = 0.0075), CONUT score (p < 0.0001, p = 0.0203), and PNI (p < 0.0001, p = 0.0025).
4 Discussion
Immunotherapy, a breakthrough treatment for head and neck cancer, has become more widely used, and treatment outcomes and prognoses are gradually becoming clearer [10, 15, 38]. In addition, many studies have reported relatively better results with chemotherapy after ICI compared to conventional chemotherapy for RMHNSCC [12, 13, 15, 39] Our department employs three regimens: PTX, PTX + Cmab, and S1, but the single agent, PTX regimen, is primarily used. However, this was because many patients had a history of cetuximab when nivolumab was started in our department, and we wanted to avoid duplication of cetuximab. After its initiation, the PTX regimen was clinically effective and had few adverse events; therefore, the PTX monotherapy regimen has been used as a general rule. In this study, the ORR and DCR for patients treated with chemotherapy following ICI were 71.2% and 84.6%, respectively, and the ORR after chemotherapy was 78.1%, 88.9%, and 40.0% for PTX, PTX + Cmab, and S1, respectively. The highest ORR for PTX + Cmab and lowest ORR for S1 were observed. PTX + Cmab had the best response rate but was not significantly different from that of PTX. In addition, a study on the estimated OS and PFS from the first dose of chemotherapy after ICI showed favorable results, with a median OS of 10 months (95% CI 6–18), an estimated 12-month OS rate of 44.5%, a median PFS of 5 months (95% CI 4–6), and an estimated 12-month PFS rate of 8.9%. Compared to reports of patients receiving PTX + Cmab [14], we found no significant difference in OS, although PFS was slightly lower. In addition, there were no significant differences among the three groups by regimen, similar to the results reported by Yasumatsu et al. [15]. Although the effects between regimens vary from report to report [12,13,14,15, 40,41,42,43], all reports indicate that chemotherapy after ICI is effective. Our results also showed that chemotherapy was effective regardless of regimen, and the results were comparable to previous reports [14, 15, 41]. Due to the small number of cases and some biases in our study, it was difficult to describe the differences in efficacy between regimens. However, as more patients accumulate, it is expected to become clearer which regimen is more effective.
Regarding safety, although there was a concern about an increase in adverse events with chemotherapy after using ICIs, this study showed no particular increase in adverse events. However, there was one case of serious interstitial pneumonia. Matsuo et al. stated that patients treated with nivolumab followed by Cmab-containing chemotherapy have a higher risk of drug-induced interstitial lung disease compared to other regimens [44]. In patients with documented pulmonary dysfunction, Cmab-containing chemotherapy should be administered with careful monitoring.
Although several factors may be associated with the prognosis or efficacy of chemotherapy after ICI in RMHNSCC, few studies have examined those factors [25]. Recently, nutritional and inflammatory factors have been reported to be associated with prognosis [17, 19, 21,22,23,24,25], and we investigated whether these factors were associated with prognosis after chemotherapy in RMHNSCC.
The results of this study showed no significant differences between the ORR or DCR and each factor. However, there was a trend suggesting that ORR might be associated with age, whereas DCR might be associated with NLR and PLR. Matsuki et al. reported that hematological inflammatory markers, specifically elevated NLR and modified GPS, were significantly associated with DCR, but not with ORR, in patients with RMHNSCC treated with nivolumab [45]. Our previous study found no significant correlation between inflammatory and nutritional factors and the ORR in patients receiving ICI therapy [46]. However, DCR showed a significant correlation with the systemic immune-inflammation index and a trend associated with other factors such as PLR. Clinical studies examining the association between ORR or DCR and survival after chemotherapy have reported that ORR is not associated with prognosis and that DCR is associated with prognosis [47]. These results suggest that inflammatory and nutritional factors may be associated with DCR rather than ORR, which may be correlated with long-term prognosis.
Furthermore, we examined the associations between these inflammatory and nutritional factors and prognosis. Univariate Cox regression analysis for OS and PFS by factor showed that Alb, NLR, PLR, CAR, CONUT, GPS, and PNI were significantly correlated with OS, and NLR, PLR, CONUT, and PNI were significantly correlated with PFS. Additionally, these four factors (NLR, PLR, CONUT score, and PNI) were significantly correlated with OS and PFS in the log-rank test.
And reflect prognosis, with better nutritional status and lower inflammatory status associated with better prognosis. Wakasaki et al. reported that CRP and NLR were prognostic factors for chemotherapy after nivolumab in RMHNSCC [25]. The NLR is a well-known biomarker that has been reported to be an independent prognostic factor in head and neck cancer [26]. The results of the present study, as well as previous reports, showed that NLR is associated with the prognosis of chemotherapy after ICI. However, to date, no other studies have examined the prognostic value of inflammatory and nutritional factors for chemotherapy after ICI, and the role of these factors remains unclear. Our results also demonstrated that PLR, CONUT score, and PNI were significantly associated with prognosis. PLR is defined as the platelet-to-lymphocyte ratio. Increased platelet counts have been implicated in increased cancer invasiveness and indirect interactions between cancer cells and platelets through secreted molecules, making them more aggressive [48]. In contrast, lymphocytes constitute a significant component of the host immune system and can eliminate cancer cells and prevent tumor progression [49]. In other words, relatively high platelet and low lymphocyte counts may predict a poor prognosis. Takenaka et al. [50] reported that PLR was associated with poor survival in patients with HNSCC. Additionally, PLR is reportedly associated with poor prognosis in various carcinomas [24, 51, 52]. These results showed that PLR was also a prognostic factor for the patients in ICI after chemotherapy.
The CONUT score is a nutritional scoring tool used to screen and identify hospitalized patients with malnutrition [34]. This score, calculated from serum albumin, total lymphocyte count, and total cholesterol, has recently emerged as a tool to assess the nutritional and immunological status of patients with malignancies [18, 21, 53]. The PNI, which is calculated based on the serum albumin concentration and peripheral blood lymphocyte count, is a nutritional scoring tool that is used to assess the nutritional and immune status of patients with cancer [19]. The PNI has been shown to be a useful prognostic tool in predicting survival and guiding treatment decisions in patients with various types of cancer [20, 23]. The CONUT score and PNI are indicators of nutritional status. However, Lin et al. demonstrated that the CONUT score has a superior prognostic value compared to the NLR, PLR, and LMR [18]. This finding further emphasizes the correlation between nutritional status, immune status, and prognosis. Notably, they also revealed that the prognostic value of the CONUT score was superior to that of the PNI score, suggesting an important role of cholesterol in determining the prognosis of tumors. Our results revealed no significant differences between the two factors. However, both factors were associated with prognosis, suggesting they could be useful tools for chemotherapy following ICI treatment.
In summary, our results showed that several inflammatory and nutritional factors are correlated with the prognosis of patients treated with chemotherapy after ICI. Although the usefulness of these factors differs among reports, they all indicate that inflammatory and nutritional factors are associated with cancer patient prognosis. In the future, these factors are expected to contribute to the prognosis of cancer patients by providing nutritional support at an early stage concurrently with cancer treatment.
This study had several limitations. First, this was a single-center retrospective study that evaluated a small number of patients. Second, the PTX + Cmab and S1 groups were small, making it difficult to assess the usefulness of the regimen and possibly causing bias in drug selection. Third, nutritional and inflammatory factors must be interpreted cautiously because of the many factors involved. Finally, randomized prospective trials are needed to optimize chemotherapy after ICI treatment for RMHNSCC.
5 Conclusions
We evaluated the effectiveness of chemotherapy after ICI treatment in our department. The median OS was 20 months (95% CI 12–25), the estimated 12-month OS rate was 63.3%, the median PFS was 5 months (95% CI 4–6), and the 12-month PFS estimate was 8.9%, with favorable results. There were no significant differences in each chemotherapy regimen's effectiveness and response rates. Inflammatory and nutritional factors were examined in terms of OS and PFS. These factors may associate with patient prognosis of chemotherapy after ICI treatment.
Data availability
All relevant data has been presented in this manuscript.
Abbreviations
- ICI:
-
Immune checkpoint inhibitors
- PFS:
-
Progression-free survival
- PLR:
-
Platelet-to-lymphocyte ratio
- RMHNSCC:
-
Recurrent and recurrent or metastatic head and neck squamous cell carcinoma
- CT:
-
Computed tomography
- ORR:
-
Objective response rate
- DCR:
-
Disease control rate
- CI:
-
Confidence interval
- CR:
-
Complete response
- PR:
-
Partial response
- SD:
-
Stable disease
- OS:
-
Overall survival
- PFS:
-
Progression-free survival
- AE:
-
Adverse event
- BMI:
-
Body mass index
- Alb:
-
Albumin
- CRP:
-
C-reactive protein
- LMR:
-
Lymphocyte-to-monocyte ratio
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet to lymphocyte ratio
- CAR:
-
CRP to albumin ratio
- CONUT:
-
Controlling nutritional status
- GPS:
-
Glasgow Prognostic Score
- PI:
-
Prognostic index
- PNI:
-
Prognostic nutrition index
- PTX:
-
Paclitaxel
- Cmab:
-
Cetuximab
- S1:
-
Tegafur–gimeracil–oteracil potassium
- ECOG:
-
Eastern Cooperative Oncology Group
References
Jacobs C, Lyman G, Velez-García E, Sridhar KS, Knight W, Hochster H, Goodnough LT, Mortimer JE, Einhorn LH, Schacter L, et al. A phase III randomized study comparing cisplatin and fluorouracil as single agents and in combination for advanced squamous cell carcinoma of the head and neck. J Clin Oncol. 1992;10:257–63.
Forastiere AA, Metch B, Schuller DE, Ensley JF, Hutchins LF, Triozzi P, Kish JA, McClure S, VonFeldt E, Williamson SK, et al. Randomized comparison of cisplatin plus fluorouracil and carboplatin plus fluorouracil versus methotrexate in advanced squamous-cell carcinoma of the head and neck: a Southwest Oncology Group study. J Clin Oncol. 1992;10:1245–51.
Brockstein B, Haraf DJ, Rademaker AW, Kies MS, Stenson KM, Rosen F, Mittal BB, Pelzer H, Fung BB, Witt ME, et al. Patterns of failure, prognostic factors and survival in locoregionally advanced head and neck cancer treated with concomitant chemoradiotherapy: a 9-year, 337-patient, multi-institutional experience. Ann Oncol. 2004;15:1179–86.
Cohen MH, Chen H, Shord S, Fuchs C, He K, Zhao H, Sickafuse S, Keegan P, Pazdur R. Approval summary: cetuximab in combination with cisplatin or carboplatin and 5-fluorouracil for the first-line treatment of patients with recurrent locoregional or metastatic squamous cell head and neck cancer. Oncologist. 2013;18:460–6.
Hitt R, Irigoyen A, Cortes-Funes H, Grau JJ, Garcia-Saenz JA, Cruz-Hernandez JJ, Spanish H. Neck Cancer Cooperative G: Phase II study of the combination of cetuximab and weekly paclitaxel in the first-line treatment of patients with recurrent and/or metastatic squamous cell carcinoma of head and neck. Ann Oncol. 2012;23:1016–22.
Leon X, Hitt R, Constenla M, Rocca A, Stupp R, Kovacs AF, Amellal N, Bessa EH, Bourhis J. A retrospective analysis of the outcome of patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck refractory to a platinum-based chemotherapy. Clin Oncol (R Coll Radiol). 2005;17:418–24.
Ferris RL, Blumenschein G Jr, Fayette J, Guigay J, Colevas AD, Licitra L, Harrington K, Kasper S, Vokes EE, Even C, et al. Nivolumab for recurrent squamous-cell carcinoma of the head and neck. N Engl J Med. 2016;375:1856–67.
Burtness B, Harrington KJ, Greil R, Soulieres D, Tahara M, de Castro G, Jr., Psyrri A, Baste N, Neupane P, Bratland A, et al. Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet. 2019;394:1915–28.
Matsuo M, Yasumatsu R, Masuda M, Toh S, Wakasaki T, Hashimoto K, Taura M, Uchi R, Nakagawa T. Relationship between immune-related adverse events and the long-term outcomes in recurrent/metastatic head and neck squamous cell carcinoma treated with nivolumab. Oral Oncol. 2020;101: 104525.
Matsuki T, Okamoto I, Fushimi C, Takahashi H, Okada T, Kondo T, Sato H, Ito T, Tokashiki K, Tsukahara K, et al. Real-world, long-term outcomes of nivolumab therapy for recurrent or metastatic squamous cell carcinoma of the head and neck and impact of the magnitude of best overall response: a retrospective multicenter study of 88 patients. Cancers (Basel). 2020;12:3247.
Cabezas-Camarero S, Cabrera-Martin MN, Merino-Menendez S, Paz-Cabezas M, Garcia-Barberan V, Saiz-Pardo Sanz M, Iglesias-Moreno M, Alonso-Ovies A, Perez-Segura P. Safety and efficacy of cetuximab-based salvage chemotherapy after checkpoint inhibitors in head and neck cancer. Oncologist. 2021;26:e1018–35.
Fushimi C, Baba D, Masubuchi T, Yamazaki M, Kitani Y, Kitajima T, Tanaka J, Hanyu K, Tanaka N, Miura K, Tada Y. Weekly cetuximab and paclitaxel for recurrent or metastatic head and neck squamous cell carcinoma. In Vivo. 2020;34:2653–7.
Kurosaki T, Mitani S, Tanaka K, Suzuki S, Kanemura H, Haratani K, Fumita S, Iwasa T, Hayashi H, Yoshida T, et al. Safety and efficacy of cetuximab-containing chemotherapy after immune checkpoint inhibitors for patients with squamous cell carcinoma of the head and neck: a single-center retrospective study. Anticancer Drugs. 2021;32:95–101.
Wakasaki T, Manako T, Yasumatsu R, Hara H, Toh S, Masuda M, Yamauchi M, Kuratomi Y, Nishimura E, Takeuchi T, et al. Effectiveness and safety of weekly paclitaxel and cetuximab as a salvage chemotherapy following immune checkpoint inhibitors for recurrent or metastatic head and neck squamous cell carcinoma: a multicenter clinical study. PLoS ONE. 2022;17: e0271907.
Yasumatsu R, Shimizu Y, Hanai N, Kariya S, Yokota T, Fujii T, Tsukahara K, Ando M, Hanyu K, Ueda T, et al. Outcomes of long-term nivolumab and subsequent chemotherapy in Japanese patients with head and neck cancer: 2-year follow-up from a multicenter real-world study. Int J Clin Oncol. 2022;27:95–104.
Wakasaki T, Yasumatsu R, Uchi R, Taura M, Matsuo M, Komune N, Nakagawa T. Outcome of chemotherapy following nivolumab treatment for recurrent and/or metastatic head and neck squamous cell carcinoma. Auris Nasus Larynx. 2020;47:116–22.
Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2003;89:1028–30.
Lin Q, Li C, Lin X, Lin S, Chen W, Chen X, Huang X, Wang D. Prognostic value of controlling nutritional status score in advanced hypopharyngeal cancer. Laryngoscope. 2023. https://doi.org/10.1002/lary.30568.
Onodera T, Goseki N, Kosaki G. Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi. 1984;85:1001–5.
Luo Z, Zhou L, Balde AI, Li Z, He L, ZhenWei C, Zou Z, Huang S, Han S, Wei Zhou M, et al. Prognostic impact of preoperative prognostic nutritional index in resected advanced gastric cancer: a multicenter propensity score analysis. Eur J Surg Oncol. 2019;45:425–31.
Tokunaga R, Sakamoto Y, Nakagawa S, Ohuchi M, Izumi D, Kosumi K, Taki K, Higashi T, Miyamoto Y, Yoshida N, et al. CONUT: a novel independent predictive score for colorectal cancer patients undergoing potentially curative resection. Int J Colorectal Dis. 2017;32:99–106.
Magnes T, Melchardt T, Weiss L, Mittermair C, Neureiter D, Klieser E, Gampenrieder S, Moser G, Gaggl A, Greil R, Egle A. Prognostic score in patients with recurrent or metastatic carcinoma of the head and neck treated with cetuximab and chemotherapy. PLoS ONE. 2017;12: e0180995.
Migita K, Matsumoto S, Wakatsuki K, Ito M, Kunishige T, Nakade H, Kitano M, Nakatani M, Sho M. The prognostic significance of inflammation-based markers in patients with recurrent gastric cancer. Surg Today. 2018;48:282–91.
Ying HQ, Deng QW, He BS, Pan YQ, Wang F, Sun HL, Chen J, Liu X, Wang SK. The prognostic value of preoperative NLR, d-NLR, PLR and LMR for predicting clinical outcome in surgical colorectal cancer patients. Med Oncol. 2014;31:305.
Wakasaki T, Yasumatsu R, Masuda M, Takeuchi T, Manako T, Matsuo M, Jiromaru R, Uchi R, Komune N, Noda T, Nakagawa T. Prognostic biomarkers of salvage chemotherapy following nivolumab treatment for recurrent and/or metastatic head and neck squamous cell carcinoma. Cancers (Basel). 2020;12:2299.
Mariani P, Russo D, Maisto M, Troiano G, Caponio VCA, Annunziata M, Laino L. Pre-treatment neutrophil-to-lymphocyte ratio is an independent prognostic factor in head and neck squamous cell carcinoma: meta-analysis and trial sequential analysis. J Oral Pathol Med. 2022;51:39–51.
Diem S, Schmid S, Krapf M, Flatz L, Born D, Jochum W, Templeton AJ, Fruh M. Neutrophil-to-Lymphocyte ratio (NLR) and Platelet-to-Lymphocyte ratio (PLR) as prognostic markers in patients with non-small cell lung cancer (NSCLC) treated with nivolumab. Lung Cancer. 2017;111:176–81.
Xu H, He A, Liu A, Tong W, Cao D. Evaluation of the prognostic role of platelet-lymphocyte ratio in cancer patients treated with immune checkpoint inhibitors: a systematic review and meta-analysis. Int Immunopharmacol. 2019;77: 105957.
Kano S, Homma A, Hatakeyama H, Mizumachi T, Sakashita T, Kakizaki T, Fukuda S. Pretreatment lymphocyte-to-monocyte ratio as an independent prognostic factor for head and neck cancer. Head Neck. 2017;39:247–53.
Hu B, Yang XR, Xu Y, Sun YF, Sun C, Guo W, Zhang X, Wang WM, Qiu SJ, Zhou J, Fan J. Systemic immune-inflammation index predicts prognosis of patients after curative resection for hepatocellular carcinoma. Clin Cancer Res. 2014;20:6212–22.
Wang YT, Kuo LT, Weng HH, Hsu CM, Tsai MS, Chang GH, Lee YC, Huang EI, Tsai YT. Systemic immune-inflammation index as a predictor for head and neck cancer prognosis: a meta-analysis. Front Oncol. 2022;12: 899518.
Tanoue K, Tamura S, Kusaba H, Shinohara Y, Ito M, Tsuchihashi K, Shirakawa T, Otsuka T, Ohmura H, Isobe T, et al. Predictive impact of C-reactive protein to albumin ratio for recurrent or metastatic head and neck squamous cell carcinoma receiving nivolumab. Sci Rep. 2021;11:2741.
Ikoma T, Shimokawa M, Matsumoto T, Boku S, Yasuda T, Shibata N, Kurioka Y, Takatani M, Nobuhisa T, Namikawa T, et al. Inflammatory prognostic factors in advanced or recurrent esophageal squamous cell carcinoma treated with nivolumab. Cancer Immunol Immunother. 2022;72:427.
Ignacio de Ulíbarri J, González-Madroño A, de Villar NG, González P, González B, Mancha A, Rodríguez F, Fernández G. CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp. 2005;20:38–45.
Jiang C, Xiu Y, Zhang S, Yu X, Qiao K, Huang Y. A novel inflammatory and nutritional prognostic scoring system for nonpathological complete response breast cancer patients undergoing neoadjuvant chemotherapy. Dis Markers. 2022;2022:8044550.
Kasymjanova G, MacDonald N, Agulnik JS, Cohen V, Pepe C, Kreisman H, Sharma R, Small D. The predictive value of pre-treatment inflammatory markers in advanced non-small-cell lung cancer. Curr Oncol. 2010;17:52–8.
Matsuo M, Yasumatsu R, Masuda M, Toh S, Wakasaki T, Hashimoto K, Jiromaru R, Manako T, Nakagawa T. Inflammation-based prognostic score as a prognostic biomarker in patients with recurrent and/or metastatic head and neck squamous cell carcinoma treated with nivolumab therapy. In Vivo. 2022;36:907–17.
Otsuki S, Hori R, Shinohara S, Kojima T, Tamaki H, Asato R, Kitamura M, Ichimaru K, Kitani Y, Kumabe Y, et al. Real-world 2-year long-term outcomes and prognostic factors in patients receiving nivolumab therapy for recurrent or metastatic squamous cell carcinoma of the head and neck. Auris Nasus Larynx. 2022;49:834–44.
Saleh K, Daste A, Martin N, Pons-Tostivint E, Auperin A, Herrera-Gomez RG, Baste-Rotllan N, Bidault F, Guigay J, Le Tourneau C, et al. Response to salvage chemotherapy after progression on immune checkpoint inhibitors in patients with recurrent and/or metastatic squamous cell carcinoma of the head and neck. Eur J Cancer. 2019;121:123–9.
Suzuki S, Toyoma S, Kawasaki Y, Koizumi K, Iikawa N, Shiina K, Endo T, Abe T, Kouga T, Yamada T. Clinical outcomes of cetuximab and paclitaxel after progression on immune checkpoint inhibitors in recurrent or metastatic head and neck squamous cell carcinoma. Medicina (Kaunas). 2021;57:1151.
Guiard E, Clatot F, Even C, Perreard M, Abdeddaim C, Johnson A, Vauleon E, Rambeau A. Impact of previous nivolumab treatment on the response to taxanes in patients with recurrent/metastatic head and neck squamous cell carcinoma. Eur J Cancer. 2021;159:125–32.
Fukuoka O, Saito Y, Mukai T, Hayashi T, Yamamura K, Sakai T, Kobayashi K, Akashi K, Yoshida M, Ando M, Yamasoba T. Efficacy of chemotherapy after immune checkpoint inhibitor discontinuation in head and neck cancer. Laryngoscope. 2023. https://doi.org/10.1002/lary.30851.
Ueki Y, Takahashi T, Ota H, Shodo R, Yamazaki K, Horii A. Role of programmed death-ligand 1 in predicting the treatment outcome of salvage chemotherapy after nivolumab in recurrent/metastatic head and neck squamous cell carcinoma. Head Neck. 2020;42:3275–81.
Matsuo M, Yasumatsu R, Masuda M, Toh S, Wakasaki T, Hashimoto K, Uchi R, Jiromaru R, Sato K, Manako T, Nakagawa T. Drug-induced interstitial lung disease in recurrent and/or metastatic head and neck cancer patients treated with cetuximab and/or nivolumab. Oral Oncol. 2021;113: 105129.
Matsuki T, Okamoto I, Fushimi C, Sawabe M, Kawakita D, Sato H, Tsukahara K, Kondo T, Okada T, Tada Y, et al. Hematological predictive markers for recurrent or metastatic squamous cell carcinomas of the head and neck treated with nivolumab: a multicenter study of 88 patients. Cancer Med. 2020;9:5015–24.
Sakai A, Iijima H, Ebisumoto K, Yamauchi M, Teramura T, Yamazaki A, Watanabe T, Inagi T, Maki D, Okami K. Prognostic value of inflammatory and nutritional biomarkers of immune checkpoint inhibitor treatment for recurrent or metastatic squamous cell carcinoma of the head and neck. Cancers (Basel). 2023;15:2021.
Matsumoto H, Horita N, Ito K, Ebina-Shibuya R, Hara Y, Kobayashi N, Kaneko T. Disease control and objective responsive rates in randomized phase II trials evaluating non-first-line chemotherapy for non-small cell lung cancer: a systematic review of 74 trials. Transl Lung Cancer Res. 2021;10:2278–89.
Kassassir H, Karolczak K, Siewiera KM, Wojkowska DW, Braun M, Watala CW. Time-dependent interactions of blood platelets and cancer cells, accompanied by extramedullary hematopoiesis, lead to increased platelet activation and reactivity in a mouse orthotopic model of breast cancer - implications for pulmonary and liver metastasis. Aging (Albany NY). 2020;12:5091–120.
Rosenberg SA. Progress in human tumour immunology and immunotherapy. Nature. 2001;411:380–4.
Takenaka Y, Oya R, Kitamiura T, Ashida N, Shimizu K, Takemura K, Yamamoto Y, Uno A. Platelet count and platelet-lymphocyte ratio as prognostic markers for head and neck squamous cell carcinoma: meta-analysis. Head Neck. 2018;40:2714–23.
Chen N, Li W, Huang K, Yang W, Huang L, Cong T, Li Q, Qiu M. Increased platelet-lymphocyte ratio closely relates to inferior clinical features and worse long-term survival in both resected and metastatic colorectal cancer: an updated systematic review and meta-analysis of 24 studies. Oncotarget. 2017;8:32356–69.
Lu C, Gao P, Yang Y, Chen X, Wang L, Yu D, Song Y, Xu Q, Wang Z. Prognostic evaluation of platelet to lymphocyte ratio in patients with colorectal cancer. Oncotarget. 2017;8:86287–95.
Ding T, Li W, Liu Y, Liu L, Dong Y. Prognostic value of preoperative controlling nutritional status in hypopharyngeal cancer patients undergoing surgery-oriented comprehensive treatment. Ear Nose Throat J. 2023. https://doi.org/10.1177/01455613221148314.
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by AS, KE, HI, MY, TT, AY, TW, TI, DM and KO. The first draft of the manuscript was written by AS and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was performed in line with the principles of the Declaration of Helsinki. The institutional review board approved the study protocol (20R248 and 22R223). The institutional review board waived the informed consent requirement owing to the study's retrospective nature.
Consent for publication
None.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sakai, A., Ebisumoto, K., Iijima, H. et al. Chemotherapy following immune checkpoint inhibitors in recurrent or metastatic head and neck squamous cell carcinoma: clinical effectiveness and influence of inflammatory and nutritional factors. Discov Onc 14, 158 (2023). https://doi.org/10.1007/s12672-023-00774-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-023-00774-4