Abstract
Assessment of adrenal incidentaloma relies on imaging analysis and evaluation of adrenal function. Radiomics as a tool for quantitative image analysis is useful for evaluation of adrenal incidentaloma. In this review, we examined radiomic literature on adrenal incidentaloma including both adrenal functional assessment and structural differentiation of benign versus malignant adrenal tumors. In this review, we summarized the status of radiomic application on adrenal incidentaloma and suggested potential direction for future research.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Adrenal incidentaloma (AI) is defined as an adrenal mass greater than 1 cm in diameter incidentally detected on imaging performed for indications other than evaluation for adrenal disease [1]. AI has been identified more frequently in recent years with a prevalence of 1.05–8.7%, which may be due to the increasing use of diagnostic imaging [2]. AI may have clinical consequences in two aspects, i.e., the biological behavior as benign versus malignant tumors, and the adrenal endocrine function. It is prudent to assess its secretory function and malignant nature, which affects treatment and prognosis of patients with AI [3].
Computed tomography (CT) is the most common imaging modality for diagnosis of AI and it is also the most useful non-invasive tool for assessing its malignant potential and endocrine function. Traditional imaging features favoring benign AI included the following: (1) size < 4 cm in diameter; (2) ≤ 10 Hounsfield units on CT; and (3) homogeneous density. However, these general features may only help with the initial evaluation of AI but not sufficient for endocrine function and malignant potential. For patients with AI, imaging evaluation and a subsequent endocrine testing have been recommended by most clinical guidelines [1, 4,5,6,7]. Developing a non-invasive strategy based on the initial CT could potentially assist decision-making and clinical management.
Radiomics was first introduced by Lambin et al. in 2012 [8] and refers to the high-throughput computational extraction of quantitative features from medical images. Radiomics generally consists of four steps: tumor segmentation, extraction and selection of features, model building, and model performance. It transforms the medical digital images into deep-level data for quantitative analysis [9,10,11]. Radiomics has been used for tumor classification, assessment of prognosis and recurrence, and evaluation of treatment effect in various cancers including cancers in lung, breast, thyroid and adrenal gland [12,13,14]. However, there is relative lack of literature on radiomics in AI. In this review, we assessed the current status of radiomic application for AI, and suggested future directions of radiomic research for AI.
2 Adrenal incidentaloma (AI)
Most AIs are nonfunctioning benign tumors and their prevalence increases with age, reaching the highest in the 55–70 year age group [15]. Histologically, AIs are adrenal adenoma (41–52%), followed by metastatic diseases (19%), adrenocortical carcinoma (5–10%), myelolipoma (9%), and pheochromocytoma (8%) [16, 17]. There have been multiple guidelines for diagnosis and management of AI with complicated workflow including imaging methods to distinguish malignant from benign AI tumors and blood tests to assess adrenal endocrine function [1, 4,5,6,7]. The typical AI work-up has been time-consuming and costly (Figure S1).
3 Literature search strategy
A literature search was conducted in PubMed including publications from year 2012 to year 2022. The search strategy included the following terms: ("logistic regression"[Title/Abstract] OR ("artificial intelligence"[Title/Abstract] OR "radiomics"[Title/Abstract] OR "deep learning"[Title/Abstract] OR "machine learning"[Title/Abstract])) AND (("incidentaloma"[Title/Abstract] OR "incidentalomas"[Title/Abstract]) AND "adrenal"[Title/Abstract]). The inclusion criteria were the following: (a) human studies on adrenal incidentaloma; (b) studies with imaging data; (c) studies with radiomic data and predictive modeling; and (d) studies published in any language. Exclusion criteria were the following: (a) secondary analyses only, without the primary imaging data; and (b) abstracts only, review articles, letters, case reports or editorials. No restrictions were placed on study design or population.
A total of 27 articles were initially identified through this strategy (Fig. 1). However, only 5 studies were deemed relevant after detailed review of the retrieved articles [18,19,20,21] and one of them was the latest research from our team [22]. After the initial literature search in PubMed, we identified 4 additional articles through manual search of the relevant literature [23,24,25,26]. Our manual search included searching other databases, retrieving the references cited in the included articles, and checking the radiomic literature, etc. The rationale for including these 4 additional articles not identified on the initial PubMed search was the following: these articles fulfilled the inclusion criteria as original imaging research on AI with detailed radiomics and modeling data from machine learning or deep learning methods.
4 Radiomic method
Radiomics is a computational tool for medical imaging analysis and it may capture intra-tumoral heterogeneity and biological phenotypes [27]. Compare to clinical evaluation that relies on the physician’s personal expertise, the findings from radiomics through advanced statistical methods are more objective and repeatable.
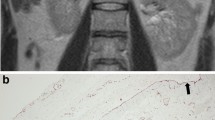
Radiomic analysis generally consists of the following: (a) Imaging acquisition and volume of interest segmentation; (b) Extraction and selection of radiomic features; (c) Analysis and modeling; and (d) Evaluation of model performance, as presented in Fig. 2.
Accurate tumor segmentation through volume of interest (VOI) approach is critical for subsequent analysis. Manual, automatic, and semi-automatic segmentations are the three commonly used method for tumor segmentation [28, 29]. Manual segmentation by expert readers is often regarded as the “golden standard”. However, it is laborious and time-consuming, and there is also concern for variability between imagers [30]. Quantitative features can be extracted from the segmented tumors [9]. Second-order statistical features or textural features can quantify the intra-tumoral heterogeneity [31]. Textural features are computed from various matrices, but not calculated directly from the original image. The gray-level co-occurrence matrix (GLCM), the neighborhood gray-tone difference matrix (NGTDM), the gray level run-length matrix (GLRLM) and the Gray Level Size Zone Matrix (GLSZM) are typical parameters from textural feature analysis [32].
Following selection of radiomic features, a mathematical model can be built and used for predicting tumor type, treatment response, and prognosis. Support vector machines, decision trees, neural networks, linear and logistic regression are commonly used algorithms in radiomics [28, 33,34,35]. The classification efficiency of the model is generally evaluated with the receiver operating characteristic (ROC) curve, and the area under the curve (AUC). The consistency between the predicted classification results of the model and the actual classification is evaluated by calibration curve, and the clinical usefulness is evaluated by a decision curve analysis.
5 Radiomic application on AI
A major challenge in clinical management of AI is to ascertain benign versus malignant nature of the tumor because the biological nature of AI affects its treatment and prognosis. The current research has mainly focused on the following two aspects of AI: endocrine functional assessment and differentiation of benign versus malignant tumors. An overview of the included studies is presented in Table 1.
5.1 Endocrine function
Our own study by Yi et al. performed machine learning-based quantitative radiomic texture analysis on unenhanced CT to differentiate subclinical pheochromocytoma (sPHEO) from lipid-poor adenoma (LPAs) [19]. We selected 30 textural features on 80 LPAs from79 patients and 30 sPHEOs from 29 patients. Logistic multiple regression analysis was performed and our model had an accuracy rate of 94.4% with sensitivity 86.2% and specificity 97.5%. More importantly, this model was based on unenhanced CT which had the advantage over contrasted CT such as saving time, cost, avoiding additional radiation and potential complication from contrast enhancement.
In another study by our group, we distinguished sPHEO from LPAs based on both pre-enhanced and enhanced CT images [18]. Our study consisted of 265 consecutive patients [training cohort, 212 (LPA, 145; sPHEO, 67); validation cohort, 53 (LPA, 36; sPHEO, 17)]. Radiomic features were used to construct a radiomic signature (Rad-score) and a radiomic nomogram. The final model based on enhanced CT achieved an AUC of 0.957 in the training cohort and 0.967 in the validation cohort. The final model based on pre-enhanced CT resulted in an AUC of 0.955 in the training cohort and 0.958 in the validation cohort.
In a more recent publication from our group [22], we used CT-based machine learning models to differentiate sPHEO from LPAs, and our study included 188 tumors in the 183 patients with LPA and 92 tumors in 86 patients with sPHEO. Six imaging features were used to build models, and we assessed all combinations of these features and the three machine-learning models, i.e., logistic regression, support vector machine and random forest. Overall performance, conciseness and high sensitivity were the three parameters used to evaluate the model performance. Ultimately, the model consisting of features from pre-enhanced CT, tumor shape and necrosis/cystic degeneration with logistic regression approach performed the best, achieving an AUC of 0.919 and an accuracy of 0.859.
5.2 Differentiation of benign versus malignant tumor
CT imaging features such as size, Hounsfield units and homogeneous density are the three common parameters for assessing the biological nature of AI tumors [15]. However, these general features would not work on special AI tumors. Taking LPA for example, most LPAs have CT attenuation values over 10 HU, similar to other adrenal tumors. A study by Ho et al. focused on distinguishing the LPAs from malignant adrenal nodules and they found that chemical-shift MRI could be useful for this purpose [23]. Specifically, they assessed 23 adrenal nodules in 20 patients, and obtained 21 second-order texture features. Except the unenhanced CT attenuation of the AI tumors, other imaging features revealed notable differences between benign and malignant adrenal nodules. Their model showed that contrast-enhanced CT and chemical-shift MRI were predictive of malignant AI (p = 0.003 and p = 0.02, respectively). This was the first study using chemical-shift MRI for distinguishing the LPAs from malignant adrenal masses. However, the study was limited by a small sample size.
A study by Elmohr [24] used quantitative CT texture analysis to differentiate between large adrenal adenomas and carcinomas in a cohort of 54 patients. Interestingly, they compared the accuracy of the prediction model to that of the radiologists. Their study revealed that combination of CT texture analysis and CT attenuation values, was likely to improve imaging evaluation by radiologists. A study by Shi [25] included 225 patients with 265 adrenal tumors (101 metastases, 98 pheochromocytomas, and 66 lipid-poor adenomas) for differentiating metastases from benign adrenal masses. Their study showed significant differences between metastases and benign adrenal masses in the texture parameters including the standard deviation (SD), entropy, mean of positive pixels and kurtosis on unenhanced images, and mean, SD of pixel distribution histogram, mean of positive pixels, and entropy on enhanced images. Their best performing model yielded a mean AUC of 0.85 with four texture parameters mentioned above on enhanced images. A study by Yu [26] performed texture analysis for differentiation between benign from malignant adrenal lesions on enhanced CT for a cohort of 125 patients. Their study showed that entropy and standard deviation were the two imagine features with significant differences between benign and malignant tumors. Entropy demonstrated a mean AUC of 0.96 and standard deviation demonstrated a mean AUC of 0.925 for discriminating tumors. These studies have a common limitation in that malignant adrenal lesions consisted of mostly metastases and were hence heterogeneous from various primary cancers.
A study by Torresan et al. used CT radiomics to differentiate between adrenocortical adenoma and carcinoma on 19 patients (9 adenomas, 10 carcinomas) [20]. First-order features and second-order features were extracted by principal component analysis [36]. In addition, they applied a K-means clustering technique, an unsupervised machine learning approach in their data analysis and accurately predicted malignancy in 7 of 8 adrenocortical carcinomas. In another study by Moawad [21], they used enhanced CT and machine learning algorithm to determine the pathology of the adrenal tumors in 40 patients. Their binary classification model using a random forest algorithm showed an AUC = 0.85 (sensitivity 84.2%, and specificity 71.4%).
The findings from our review were generally in agreement with the more recent literature and a review on the topic by Crimì et al. who performed a systematic review on CT radiomic texture analysis in AI [37]. Their review included 9 papers with a pooled median AUC of 0.85, indicating a diagnostic accuracy of 93% in differentiating adrenal adenoma from adrenocortical carcinomas. Our current review also included 9 papers but mostly different papers yet our results were similar to theirs with our AUC ranging from 0.8 to 0.96 for differentiating benign from malignant adrenal tumors such as adrenal metastases. In addition, our review was complimentary to their study as we also provided an assessment of the endocrine functioning adrenal tumors in addition to structural differentiation between benign and malignant AI tumors. For instance, we assessed studies including research from our own group on radiomic CT texture analysis for differentiating pheochromocytoma from atypical adrenal adenoma with low lipid [19]. Our own machine learning-based radiomic studies showed high performance of our prediction models for classifying pheochromocytoma from lipid-poor adenoma with AUC reaching 0.95. Overall, our studies and other’s data all suggest that CT radiomics may be used as a non-invasive tool for assessing both endocrine function and imaging characterization of AI.
The guideline set by European Society of Endocrinology for management of adrenocortical carcinoma specifically indicates the importance of imaging for diagnosis and treatment of adrenocortical carcinoma [38]. A CT scan of chest abdomen and pelvis is recommended for all patients with high suspicion for adrenocortical carcinoma. In addition, preoperative imaging and postoperative follow-up imaging are also recommended for patients undergoing treatment for adrenocortical carcinoma. Radiomics is a computational analysis of the existing imaging data and it generates multiple higher-order features for detailed characterization of adrenocortical carcinoma. Radiomics does not acquire additional imaging beyond what has already obtained per recommendations by the guidelines. Since the existing imaging complies with the guideline for management of adrenocortical carcinoma, the subsequent radiomic analysis of this imaging data should also meet the criteria of the guidelines for management of adrenocortical carcinoma.
In summary, all studies included in this review applied radiomics on CT including both unenhanced and enhanced CT images [18,19,20,21,22,23,24,25,26]. This could be due to CT being the most commonly used modality for initial imaging of abdominal pathology. In this review, one study included only unenhanced CT in their radiomic analysis [19], and two studies included only enhanced CT [21, 26], while the remaining studies reported radiomics on both unenhanced and enhanced CT images from texture analysis. All studies except one [20], utilized ROC and AUC to assess the accuracy of their radiomic results. The highest AUC was 0.96 by Yu et al. [26], while the lowest AUC was 0.8 by Ho et al. [23], and the mean AUC was 0.88 among all included studies in this review. Taken together, the radiomic analysis based on CT imaging of AI was robust and could be potentially useful in clinical management of AI. Nevertheless, more work needs to be done to improve its efficacy for broader clinical application.
6 Limitation
There were two main limitations of this review. First, the studies reviewed here had one common issue. i.e., lack of interpretability. For instance, results from radiomic analysis may not be directly correlated with underlying tumor pathology and treatment response. Second, the studies in this review may have subjected to selection bias because of its retrospective nature. In addition, small sample size was a common problem among the included studies and therefore the generalizability of the radiomic findings was limited.
7 Future direction
Functional assessment and differentiation of benign versus malignant tumors are the two main points for diagnosis and management of AI. The main challenge of managing functional AI tumors pertains to appropriate diagnosis and treatment of autonomous cortisol secretion [2]. Predicting the risk of distant metastasis and recurrence, genotyping of AI tumors such as pheochromocytoma and monitoring treatment response are important aspects for personalized patient care. Fortunately, most of the radiomic approaches have been studied extensively in various cancers [12, 14], which should be adoptable for AI tumors. For example, Huynh et al. analyzed CT images of 113 patients with stage I–II non-small cell lung cancer treated with stereotactic body radiation therapy. Their study showed that radiomic features had the potential to be prognostic for outcomes that conventional imaging metrics could not do in patients with radiation treatment [39]. Hence, similar radiomic approach may be applied to identify prognostic factors in AI tumors. Another potential future direction is in the management of AI tumors. Arshad et al. conducted a multi-center study and found that PET-CT based radiomics could provide potential information for risk classification of non-small cell lung cancer patients with radiotherapy and chemo-radiotherapy [40]. Future radiomic studies on management of autonomous cortisol secretion, risk factors and prognostic prediction of AI tumors are needed to advance the field and to improve clinical decision making.
8 Conclusion
This review supports radiomics being a potentially useful non-invasive imaging tool for differentiating benign from malignant adrenal tumors. More studies need to be done to overcome the common issues with all radiomic applications such as the lack of explainability related to the tumor heterogeneity and to improve personalized care for patients with AI.
Data availability
All data including codes will be available to qualified researchers.
References
Fassnacht M, Arlt W, Bancos I, et al. Management of adrenal incidentalomas: European society of endocrinology clinical practice guideline in collaboration with the European network for the study of adrenal tumors. Eur J Endocrinol. 2016;175(2):G1-g34.
Sherlock M, Scarsbrook A, Abbas A, et al. Adrenal incidentaloma. Endocr Rev. 2020;41(6):775–820.
Gaujoux S, Mihai R. European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal Tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br J Surg. 2017;104(4):358–76.
Kapoor A, Morris T, Rebello R. Guidelines for the management of the incidentally discovered adrenal mass. Can Urol Assoc J. 2011;5(4):241–7.
Lee JM, Kim MK, Ko SH, et al. Clinical guidelines for the management of adrenal incidentaloma. Endocrinol Metab. 2017;32(2):200–18.
Mayo-Smith WW, Song JH, Boland GL, et al. Management of incidental adrenal masses: a white paper of the ACR Incidental Findings Committee. J Am Coll Radiol. 2017;14(8):1038–44.
Zeiger MA, Thompson GB, Duh QY, et al. The American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr Pract. 2009;15(Suppl 1):1–20.
Lambin P, Rios-Velazquez E, Leijenaar R, et al. Radiomics: extracting more information from medical images using advanced feature analysis. Eur J Cancer. 2012;48(4):441–6.
Gillies RJ, Kinahan PE, Hricak H. Radiomics: images are more than pictures, they are data. Radiology. 2016;278(2):563–77.
Kumar V, Gu Y, Basu S, et al. Radiomics: the process and the challenges. Magn Reson Imaging. 2012;30(9):1234–48.
Lambin P, Leijenaar RTH, Deist TM, et al. Radiomics: the bridge between medical imaging and personalized medicine. Nat Rev Clin Oncol. 2017;14(12):749–62.
Avanzo M, Stancanello J, Pirrone G, et al. Radiomics and deep learning in lung cancer. Strahlenther Onkol. 2020;196(10):879–87.
Conti A, Duggento A, Indovina I, et al. Radiomics in breast cancer classification and prediction. Semin Cancer Biol. 2021;72:238–50.
Cao Y, Zhong X, Diao W, et al. Radiomics in differentiated thyroid cancer and nodules: explorations, application, and limitations. Cancers. 2021. https://doi.org/10.3390/cancers13102436.
Kebebew E. Adrenal incidentaloma. N Engl J Med. 2021;384(16):1542–51.
Mansmann G, Lau J, Balk E, et al. The clinically inapparent adrenal mass: update in diagnosis and management. Endocr Rev. 2004;25(2):309–40.
Mantero F, Terzolo M, Arnaldi G, et al. A survey on adrenal incidentaloma in Italy. Study group on adrenal tumors of the Italian Society of Endocrinology. J Clin Endocrinol Metab. 2000;85(2):637–44.
Yi X, Guan X, Zhang Y, et al. Radiomics improves efficiency for differentiating subclinical pheochromocytoma from lipid-poor adenoma: a predictive, preventive and personalized medical approach in adrenal incidentalomas. Epma j. 2018;9(4):421–9.
Yi X, Guan X, Chen C, et al. Adrenal incidentaloma: machine learning-based quantitative texture analysis of unenhanced CT can effectively differentiate sPHEO from lipid-poor adrenal adenoma. J Cancer. 2018;9(19):3577–82.
Torresan F, Crimì F, Ceccato F, et al. Radiomics: a new tool to differentiate adrenocortical adenoma from carcinoma. BJS Open. 2021. https://doi.org/10.1093/bjsopen/zraa061.
Moawad AW, Ahmed A, Fuentes DT, et al. Machine learning-based texture analysis for differentiation of radiologically indeterminate small adrenal tumors on adrenal protocol CT scans. Abdom Radiol. 2021;46(10):4853–63.
Liu H, Guan X, Xu B, et al. Computed tomography-based machine learning differentiates adrenal pheochromocytoma from lipid-poor adenoma. Front Endocrinol. 2022. https://doi.org/10.3389/fendo.2022.833413.
Ho LM, Samei E, Mazurowski MA, et al. Can texture analysis be used to distinguish benign from malignant adrenal nodules on unenhanced CT, contrast-enhanced CT, or in-phase and opposed-phase MRI? AJR Am J Roentgenol. 2019;212(3):554–61.
Elmohr MM, Fuentes D, Habra MA, et al. Machine learning-based texture analysis for differentiation of large adrenal cortical tumours on CT. Clin Radiol. 2019;74(10):818.e1-818.e7.
Shi B, Zhang GM, Xu M, et al. Distinguishing metastases from benign adrenal masses: what can CT texture analysis do? Acta Radiol. 2019;60(11):1553–61.
Yu H, Parakh A, Blake M, et al. Texture analysis as a radiomic marker for differentiating benign from malignant adrenal tumors. J Comput Assist Tomogr. 2020;44(5):766–71.
Chicklore S, Goh V, Siddique M, et al. Quantifying tumour heterogeneity in 18F-FDG PET/CT imaging by texture analysis. Eur J Nucl Med Mol Imaging. 2013;40(1):133–40.
Rizzo S, Botta F, Raimondi S, et al. Radiomics: the facts and the challenges of image analysis. Eur Radiol Exp. 2018;2(1):36.
Ge L, Chen Y, Yan C, et al. Study progress of radiomics with machine learning for precision medicine in bladder cancer management. Front Oncol. 2019;9:1296.
Chang X, Deng W, Wang X, et al. Interobserver variability in target volume delineation in definitive radiotherapy for thoracic esophageal cancer: a multi-center study from China. Radiat Oncol. 2021;16(1):102.
Haralick RM, Shanmugam KS, Dinstein IH. Textural features for image classification. IEEE Trans Syst Man Cybern. 1973;3:610–21.
Schick U, Lucia F, Dissaux G, et al. MRI-derived radiomics: methodology and clinical applications in the field of pelvic oncology. Br J Radiol. 2019;92(1104):20190105.
Breiman L. Random forests. Mach Learn. 2001;45(1):5–32.
Langs G, Menze BH, Lashkari D, et al. Detecting stable distributed patterns of brain activation using Gini contrast. Neuroimage. 2011;56(2):497–507.
Shin HC, Roth HR, Gao M, et al. Deep convolutional neural networks for computer-aided detection: CNN architectures, dataset characteristics and transfer learning. IEEE Trans Med Imaging. 2016;35(5):1285–98.
Ringnér M. What is principal component analysis? Nat Biotechnol. 2008;26(3):303–4.
Crimì F, Quaia E, Cabrelle G, et al. Diagnostic accuracy of CT texture analysis in adrenal masses: a systematic review. Int J Mol Sci. 2022. https://doi.org/10.3390/ijms23020637.
Fassnacht M, Dekkers OM, Else T, et al. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2018;179(4):G1-g46.
Huynh E, Coroller TP, Narayan V, et al. CT-based radiomic analysis of stereotactic body radiation therapy patients with lung cancer. Radiother Oncol. 2016;120(2):258–66.
Arshad MA, Thornton A, Lu H, et al. Discovery of pre-therapy 2-deoxy-2-(18)F-fluoro-d-glucose positron emission tomography-based radiomics classifiers of survival outcome in non-small-cell lung cancer patients. Eur J Nucl Med Mol Imaging. 2019;46(2):455–66.
Funding
This research was funded by Xiangya-Peking University, Wei Ming Clinical and Rehabilitation Research Fund (No. xywm2015I35), Natural Science Foundation of Hunan Province (2022JJ1179, 2022JJ40781), and China Post-Doctoral Science Foundation (2018M632997, 2022M710369), and Natural Science Foundation of China (81902727).
Author information
Authors and Affiliations
Contributions
CL and XY designed the study. CL, YF and XG searched, collected and reviewed the literature. CL and XY wrote the first draft of the manuscript. XY, XG, LL and BC supervised the study and reviewed the manuscript. All authors contributed to the study. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Institutional Review Board and the Research Ethics Committee at Xiangya Hospital approved this study (IRB: 2022020227). Written informed consent was waived due to the literature review nature of this study.
Competing interests
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
12672_2022_577_MOESM1_ESM.jpg
Additional file1 (JPG 255 KB) Figure S1. Flowchart summary of existing guidelines in diagnosing and management of patients with adrenal incidentalomas. The main differences among the guidelines are in imaging and hormone testing.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Li, C., Fu, Y., Yi, X. et al. Application of radiomics in adrenal incidentaloma: a literature review. Discov Onc 13, 112 (2022). https://doi.org/10.1007/s12672-022-00577-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12672-022-00577-z