Abstract
Objectives
Mindfulness-Based Stress Reduction (MBSR) has been shown to decrease general feelings of distress. It is not known to what extent such beneficial effects are associated with attenuation of physiological responses to challenging psychological situations. The aim of the present study was to examine potential associations between general decreases in subjective distress and changes in acute cardiac and cortical responses during recall of a recent stressful episode between pre- and post-MBSR.
Method
Fifty-eight MBSR participants (77.6% female, mean age 43.8 years, SD = 13.1) took part in a laboratory examination before and after MBSR. Measurements of the electrocardiogram (ECG) and electroencephalogram (EEG) were performed during the whole protocol including the stress recall task.
Results
The MBSR group showed overall decreases in general negative affect and an increase in heart rate variability from pre- to post-intervention. Out of six physiological outcomes (heart rate, heart rate variability, theta, alpha, beta, and gamma power at Fz), only a decreased response of gamma power during the stress task was significant. The subjective and physiological changes were unrelated.
Conclusions
The present results suggest that the favourable effects of MBSR on general stress reduction may not be clearly reflected in cortical electrical wave activity or vagal cardiac response during recall of a recent stressful episode. The few changes found in cardiac and cortical activity may be due to either effects independent of general subjective feelings or independent of the intervention altogether.
Preregistration
The study is not preregistered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mindfulness is a construct that has been widely and increasingly studied in the past two decades. Mindfulness may be defined as “a process of regulating attention in order to bring a quality of nonelaborative awareness to current experience and a quality of relating to one’s experience within an orientation of curiosity, experiential openness, and acceptance “ (Bishop et al., 2004, p. 234). It is claimed to be a favourable state of mind, as it is positively associated with psychological well-being and negatively with symptoms of psychopathology (Baer et al., 2006; Brown & Ryan, 2003). Psychological interventions have been developed, such as Mindfulness-Based Stress Reduction (MBSR) intervention (Kabat-Zinn, 1990) and Mindfulness-Based Cognitive Therapy (Segal et al., 2002), together termed mindfulness-based interventions (MBIs). Beneficial effects have been reported on various psychological outcomes, such as symptoms of anxiety, depression, and quality of life in a variety of patient and healthy populations (Goldberg et al., 2018, 2022). Meta-analyses have corroborated these effects typically showing about medium-sized effects, in both pre–post and randomized controlled designs (Goldberg et al., 2018, 2022; Khoury et al., 2013, 2015).
As MBSR was originally designed to reduce feelings of stress, it was hypothesized that MBIs would also favourably affect stress physiological systems, such as the sympatho-adreno-medullary system and the hypothalamus–pituitary–adrenal axis (Creswell & Lindsay, 2014). According to such stress-reducing theories, mindfulness is expected to decrease responses of such systems and facilitate recovery by dampening the sympathetic branch of the nervous system and enhancing the activity of the parasympathetic nervous system.
In psychophysiological research, responsivity of such systems is traditionally examined using a stress-inducing protocol, in which peripheral physiological responses, such as cardiac, vascular, and cortisol responses, to a stress task are examined (Kirschbaum et al., 1993). However, such stress-inducing protocols have hardly been applied in mindfulness-focused research. The few studies performed have yielded inconsistent findings (Creswell et al., 2019; Morton et al., 2020). Some studies reported the hypothesized dampening effects of MBIs on physiological responses, such as blood pressure and cortisol responses (Lindsay et al., 2018), but others did not find such outcomes on cardiac autonomic, vascular, and cortisol responses (Creswell et al., 2014; Nyklíček et al., 2013). In addition, some researchers found effects on some physiological systems, but not other systems. For instance, in one study, a larger recovery of diastolic blood pressure after a stress recall task was seen in participants of a MBI, but no such dampening effects on cardiac or systolic blood pressure responses (Crosswell et al., 2017), while another study found reduced inflammatory cytokine, but not cortisol, responses after a social stress task in MBI participants (Rosenkranz et al., 2013). These inconsistencies in findings might have to do with the different systems involved, contextual factors, including which specific MBI or mindfulness training has been used, the setting in which measurements are performed, and to what extent the stressor is ecologically valid and personally relevant.
Effects on brain activity associated with stress reduction in the context of MBIs are even less studied. The few exceptions include a pilot randomized trial of combat veterans with post-traumatic stress disorder, of which those who received an MBI showed stronger anterior cingulate cortex and smaller insula responses to trauma-related stimuli (Bremner et al., 2017). Another small, randomized trial showed reduced amygdala response to fearful pictures in middle-school children after meditation training (Bauer et al., 2019). Finally, using electroencephalography (EEG), lower late positive potential was reported in a small group of experienced meditators compared to non-meditators in response to unpleasant visual stimuli (Sobolewski et al., 2011). It has been proposed that such findings might be the result of fear extinction through exposure to present-moment experience during mindfulness practice (Kummar et al., 2019). Outside stress-related protocols, mindfulness meditation has been correlated with EEG spectral power in lower frequency bands, such as alpha and theta, reflecting a more relaxed state (Chiesa & Serretti, 2010).
It may be expected that any acute physiological stress reactivity reducing effects of MBIs would predominantly work by decreasing emotional states associated with stress responsivity (Creswell & Lindsay, 2014), mainly anxiety (Miller & Kirschbaum, 2019) and anger (Pauls & Stemmler, 2003). However, there is a paucity of studies examining interrelations between subjective stress reduction effects of MBIs and physiological responses, especially regarding peripheral physiological systems. An exception is a study reporting an absence of a significant correlation between subjective and cortisol responses to a social stress task (Creswell et al., 2014). In the field of affective neuroscience, a few small studies have reported correlations between mindfulness-related subjective stress effects and brain activity, yielding mixed findings (Bauer et al., 2019; Eddy et al., 2015).
The findings discussed above together with the paucity of studies on psychophysiological working mechanisms of stress responsivity call for a study using a full standardized MBI program examining combined changes of several physiological systems, such as cardiac and cortical activity during a stressful task, together with changes in subjective stress indices. More insight into such combined changes and their interrelations are important to better understand the existence of a potential positive impact of MBIs on physiological systems.
Therefore, in the present study, we aimed at examining the associations of the standard 8-week group MBSR program (Kabat-Zinn, 1990) with subjective affective, cardiac, and cortical activity in an experimental setting, in which exposure to a personally relevant stressor was part of the protocol. We hypothesized that after the intervention, the MBSR group would show lower stress response and/or stronger recovery after stress as reflected in lower negative affect, smaller heart rate variability decrease (as an index of parasympathetic cardiac drive), and smaller cortical EEG alpha and theta decrease (as index of more relaxed state) and beta and gamma increase (as index of higher cognitive activity) during a stressful laboratory protocol compared to pre-intervention. In addition, we examined if any changes found in the cardiac and cortical activity indices would be correlated with any changes in overall decrease in subjective negative affect (i.e. anxiety and anger) and increase in mindfulness skills over the course of the intervention. Specifically, we hypothesized that any decrease in physiological responsivity would be correlated with overall decreases in anxiety and anger and increases in mindfulness skills.
Method
Participants
Consecutive participants of a standard 8-week MBSR (Kabat-Zinn, 1990) intervention (n = 140) at a local meditation centre were asked to participate in a laboratory experiment before and after the intervention. Exclusion criteria were current psychopathology, i.e. severe depression, acute burnout, or psychoticism tendency. The participants received a € 32 discount on the training fee. Fifty-nine (42.1%) agreed to participate. One participant did not adhere to the protocol and dropped out of the study before the first measurement, resulting in 58 participants. This number was deemed sufficient according to the sample size computation using GPower 3.1.9.2 for a within-group effect of a repeated-measures ANOVA with at least a small-to-medium effect size (partial eta squared of 0.04), alpha of 0.05, and power of 0.80, resulting in a required estimated sample size of 36 participants. However, for correlations between outcomes, the present sample would be somewhat underpowered, with a power of 0.66.
Procedure
The intervention involved the standard 8-week MBSR program (Kabat-Zinn, 1990), which was delivered in groups of 8–15 participants at a local centre. Participants from 13 such groups were recruited for the current study. The MBSR program consists of 8 weekly group sessions and a silent retreat of a day in the sixth week. The eight sessions consist of a combination of psychoeducation on themes relating to stress and mindfulness, mindfulness meditation and yoga practices, and sharing of experiences during the practices. The trainer was experienced (having supervised > 30 MBSR groups before start of the study) and was the same for all groups.
Because of the pre–post design, all participants were asked to individually visit the laboratory at Tilburg University twice, with an 8–10-week interval between the two sessions, as the intervention lasted 8 weeks. First, they were asked to complete online questionnaires on demographics, psychological health, general affect, and mindfulness skills before their visit to the lab.
The laboratory protocol was part of a larger study on psychophysiological responses to various tasks in the context of MBSR, of which the stress recall task was part of. Participants were asked to refrain from consuming caffeinated beverages, alcohol, or nicotine at least 3 hr prior to the experiment sessions.
The protocol was identical at the two occasions and included the following tasks, in total lasting for about 90 min. After the physiological equipment was attached, the order of the tasks was as follows: (i) baseline assessment (5 min), during which participants were asked just to relax; (ii) first momentary affect self-report (GMS, see below); (iii) several tasks during which participants were asked to monitor aspects of their momentary experience (e.g. breathing, bodily sensations, and thoughts), of about 30 min duration in total (Burg & Michalak, 2011; Nyklíček, 2020), which is a part of another investigation and will be reported on elsewhere. Then (iv) an adapted 5-min version of a stress recall task was administered (Sinha et al., 2000), see below for details, after which (v) there was a recovery period of 10 min. Finally, (vi) the second affect self-report (GMS) was completed, after which the participants were debriefed.
During the stress recall task, participants were asked to vividly recall and think about “the most stressful situation that took place in the past two months; situations like for example a quarrel, during which you clearly felt an emotion such as anger, anxiety, or sadness”. The participants were first given time to search their memory for a suitable event and to indicate when an event was found. No instructions were provided regarding whether the recalled event should be the same or different at both occasions. The test leader asked if the situation was specific and stressful, in which case the participant was asked to close their eyes and imagine they were in that situation again. The test leader prompted the participant to imagine being in the situation as vividly as possible by asking four specific questions about the context, sensory input, others’ behavior, and one’s own behavior and emotions (first 2 min). After these questions, the participant was asked to further imagine being again in that situation by their own, for 3 more minutes (total stress recall time being 5 min).
Measures
Self-report Measures
Questions were asked to assess demographic and health-related variables, including sex, age, educational level, history of psychotherapy (yes/no), and current use of psychotropics for emotional problems, including depressed mood, anxiety, sleeping problems, and stress (yes/no).
Mindfulness skills were assessed by the Dutch version (Bohlmeijer et al., 2011) of the Five Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006). This questionnaire is the most widely used to assess mindfulness skills and consists of 39 items, divided across five subscales measuring different mindfulness facets: Observing (sensory and internal phenomena), Acting with Awareness, Non-judging (one’s thoughts and feelings), Non-reacting (to one’s unpleasant thoughts), and Describing (one’s thoughts and feelings). The items are answered on 5-point Likert scales ranging from 1 (never or very rarely true) to 5 (always or almost always true). As the original, the Dutch version has shown in previous studies to be a reliable (Cronbach’s alpha ranging from 0.73 to 0.91) and valid instrument, including sensitivity to change with participation in a mindfulness intervention (Bohlmeijer et al., 2011). In the current study, Cronbach’s alphas ranged between 0.76 for Observing at pre-intervention and 0.93 for Describing at post-intervention.
To assess global pre–post intervention changes in affect associated with MBSR, the Dutch shortened version (Wald & Mellenbergh, 1990) of the Profile of Mood States (POMS) (McNair et al., 1971) was used. The 32 items assess the following five affective states: depression, anxiety, anger, fatigue, and vigour. We include here only the outcomes on depression, anxiety, and anger, as these are the affective states most often examined in MBIs and are most relevant to acute stress (Miller & Kirschbaum, 2019; Pauls & Stemmler, 2003). Participants are asked to indicate “to what extent they felt that way lately”. The items are scored on 5-point Likert scale ranging from 0 (not at all) to 4 (extremely). In previous studies, internal consistency of these subscales was adequate, with Cronbach’s alpha ranging from 0.82 to 0.91, while correlations with related and unrelated constructs showed convergent and discriminant validity, respectively (Wald & Mellenbergh, 1990). In addition, these subscales have been found to be sensitive to change over the course of a MBI (Haenen et al., 2016). In the current study, Cronbach’s alphas were all at least 0.83.
Changes in negative affect in the laboratory setting were assessed using the Global Mood Scale (GMS) (Denollet, 1993). This questionnaire comprises 20 adjectives, of which 10 reflect negative affect (e.g. “helpless” and “insecure”). By using a 5-point Likert scale, ranging from 0 (not at all) to 4 (extremely), respondents are asked to indicate to what extent they experience each feeling just now. The GMS has been found to be an internally consistent scale (Cronbach’s alpha’s > 0.90) and correlations with existing measures of emotional functioning and self-deception indicated its convergent and discriminant validity (Denollet, 1993). Sensitivity to change across a mindfulness-based intervention has also been established (Nyklíček et al., 2014). In the current study, Cronbach’s alphas ranged between 0.86 for negative affect at pre-intervention recovery and 0.92 for negative affect at post-intervention baseline.
Perceived stressfulness of the event recalled during the stress recall task was assessed by the question “How stressful was the situation for you?”, answered on a scale of 0 (not at all) to 10 (extremely stressful). In addition, the participant was asked to rate “How vivid was the imagery?” also on a scale of 0 (not at all) to 10 (extremely vivid).
Physiological Measures
Biosemi Active2 equipment was used to assess both the electrocardiogram (ECG) and electroencephalogram EEG during the whole experimental session. Ag–AgCl electrodes were placed on the sternum and the left lateral margin of the chest (roughly V1 versus V6 lead) to measure the ECG signal with minimal distortion. This lead has been shown to be most adequate for R-peak scoring (Mulder, 1988). The signal was sampled at a 512-Hz rate. R-peaks were determined on the 0.05–60-Hz band-pass filtered ECG signal with a recommended method (Afonso et al., 1999), which has a very high accuracy (> 99.5%). The correct identification of the R-peaks was checked by a combination of visual inspection and an automated method applied to the cardiotachogram, which signalled R-peak occurrences outside a mean plus or minus a number of standard deviations, where this number was determined separately for each individual participant and measurement. Occurrences signalled by this method were removed from the series and re-inserted back using a spline interpolation method, as recommended by the Kubios HRV analysis software (Tarvainen et al., 2014). Two indices of cardiac activity, which are influenced by stress, were assessed. Inter-beat interval (IBI) is the mean interval between heart beats (R-peaks), and as such exactly the reverse of heart rate, which is driven by a combination of sympathetic and parasympathetic input. Root mean square of successive differences (RMSSD) was also calculated because it reflects a parasympathetically mediated heart rate variability (HRV), which withdraws during fight-flight stress, increases during relaxation, and is recommended for short-term measurements (Task Force of the European Society of Cardiology & the North American Society of Pacing & Electrophysiology, 1996). The RMSSD was calculated by determining the differences between successive IBIs, squaring the differences, calculating the mean of the squared differences, and then taking the square root of the result, again based on the method in the Kubios software (Tarvainen et al., 2014).
EEG was measured at the following sites according to the standard international 10–20 system: F3, Fz, F4, C3, Cz, C4, P3, Pz, P4, Oz, and at both mastoids, which served as a reference. The Welch (Welch, 1967) method was used to estimate the EEG power spectrum, using segments of 4 s with an overlap of 75%. The EEG in each segment and at each EEG electrode was corrected for eye movements using linear regression of horizontal and vertical EOGs, recorded by horizontally and vertically placed electrodes around the eyes. A segment was accepted into the Welch average after tapering with a Hanning window, if the difference between the maximum and minimum amplitudes within that segment was within the 95% confidence interval of a normal distribution based on all segments. Power in the EEG bands of theta (4–8 Hz), alpha (8–12 Hz), gamma (30–50 Hz), and beta (13–30 Hz) was calculated, as effects of stress have been found on most EEG power spectra, but mainly alpha and beta (Katmah et al., 2021). Power was calculated based on the Welch spectrum of each participant site to control for muscle tension artefacts. Besides overall (all sites) effects, we will mainly focus on the frontal midline electrode (Fz) because (i) mindfulness meditation is shown to work mainly via attentional areas in the prefrontal and anterior cingulate cortices (Lomas et al., 2015; Lutz et al., 2008), whose activity is picked up by frontal midline EEG (Kummar et al., 2019); (ii) theta waves in this region are supposed to reflect attention processes including interoceptive processes associated with meditation (Aftanas & Golocheikine, 2001); and (iii) meditation has been associated with enhanced alpha and theta power rhythms predominantly in the frontal areas (Takahashi et al., 2005; Travis & Shear, 2010), while default mode network activity is reflected by frontal midline gamma activity and is decreased in mindfulness meditators (Berkovich-Ohana et al., 2012). Power values were log-transformed prior to statistical analysis.
Data Analyses
First, paired samples t-tests were used to determine pre–post intervention changes in general affect and mindfulness skills. Changes in affect during the laboratory sessions were analysed using a linear mixed model (LMM) analysis with the experimental Task (baseline, recovery) in addition to Session (pre-post intervention) as fixed effects.
An LMM analysis was used to test differences in changes in cardiac parameters across Tasks between Sessions (pre–post intervention), only with more conditions as besides baseline and recovery two periods of the stress recall tasks were defined (min 1–2 and min 3–5) to potentially discriminate between the two phases of the stress recall task: guided imagery and self-imagery. Fixed effects were estimated for the two-way interaction of Task × Session.
Because of their typical non-normal distributions, EEG power of the various bands was first log transformed and winsorized before entering them as dependent measures in a linear mixed model (LMM) analysis. Fixed effects were estimated for the three-way interaction Electrode position × Task × Session. A random intercept was included in each LMM model, as well as random slopes for all within-subjects variables (i.e. Electrode, Task, Session). However, models including a random slope for the three-way interaction did not converge, so we restricted our random effects structure to the two-way interactions and first-order effects of these within-subjects variables (Singmann & Kellen, 2019). The linear mixed model analyses were conducted using the software R-studio and the R-package afex (Singmann et al., 2015). All remaining statistical analyses were conducted using IBM SPSS (version nr. 24). p-values smaller than 0.05 were considered statistically significant.
Results
The sample consisted of 58 participants, with a mean age of 43.8 years (SD = 13.1), of whom 77.6% were female, 70.7% were highly educated (high professional level, college or university), 65.5% were in a stable romantic partner relationship, 79.3% had previous psychotherapy, and 27.6% reported current use of psychotropics.
The MBSR group showed the expected overall changes in self-reported mindfulness skills and negative affect between pre- and post-intervention. Participants improved significantly on all mindfulness skills with medium to large effect sizes and also showed significant decreases in negative affect dimensions, also with medium to large effect sizes (Table 1).
Regarding laboratory data, nine participants did not attend the post-intervention session, as a result of which multilevel analyses were performed, to keep their completed data in the analysis, thereby reducing possible bias (Kadengye et al., 2012) (those with a missing post-session did not differ from the other participants in laboratory mood, p > 0.10).
In the analysis on laboratory negative affect, the Task × Session interaction was significant (F(1, 49) = 6.80, p = 0.012) reflecting a small increase in negative affect from baseline to recovery at pre-intervention, while post-intervention a decrease was evident. Also the main effect of Session was significant F(1, 52) = 11.93, p = 0.001, reflecting an overall decrease from pre- to post-intervention (Table 2).
During the stress recall task, situations participants were thinking about were very diverse, frequent themes involving a quarrel (28%), unpleasant job situation (15%), and fear (6%). Emotions experienced in the situation recalled were most often anger (58%), sadness (42%), and tension/anxiety (38%). Mean perceived stressfulness of the situation decreased from pre- to post-intervention from 8.21 (SD = 1.19) on a scale of 1–10 to 7.59 (SD = 1.44) (F(1, 50) = 7.20, p = 0.010). Vividness (mean = 7.0, SD = 1.63) did not change across sessions (F(1, 48) = 0.32, p = 0.58).
Regarding ECG, inter-beat interval (IBI) showed normal distribution, which was also the case for RMSSD after removing extreme values (> 3 × inter-quartile range; > 100 ms; 4.6% of the cases), usually due to artefacts. Linear multilevel analysis revealed that there was no significant Task × Session interaction effect for IBI (F(3, 39) = 1.07, p = 0.37). The only significant effect was the main effect of Task (F(3, 40) = 8.67, p < 0.001), which reflected an increasing IBI across time during the experiment (Table 3).
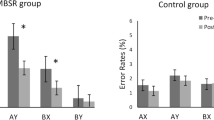
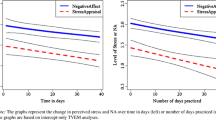
Also for RMSSD, no significant Task × Session interaction effect emerged (F(3, 42) = 0.63, p = 0.60). Both main effects were significant: the effect of Session (F(1, 39) = 5.52, p = 0.024) reflected overall higher RMSSD at post-intervention compared to pre-intervention and the main effect of Task (F(3, 47) = 3.75, p = 0.017) reflected an increasing RMSSD during the experimental sessions (Fig. 1).
Regarding EEG, the first LMM analysis revealed no significant three-way Electrode position × Task × Session interaction effects for any power band (all p > 0.10). This finding corroborated our decision to further focus on one of the electrodes, the frontal midline (Fz). Subsequent analyses on Fz showed a significant differential effect on response to the stress recall task for gamma power only (Task × Session interaction: F(3, 51) = 3.65, p = 0.018). This reflected a smaller increase in gamma at post-intervention compared to pre-intervention (Fig. 2). A similar trend was obtained for the beta band (F(3, 52) = 2.36, p = 0.082) as well as theta band (F(3, 52) = 2.77, p = 0.051). For all bands, a main effect of Task was revealed: theta (F(3, 53) = 5.64, p = 0.002), alpha (F(3, 54) = 6.45, p < 0.001), beta (F(3, 51) = 7.90, p < 0.001), and gamma (F(3, 52) = 26.62, p < 0.001), reflecting the lowest powers across the bands during baseline with often subsequent increasing values (Table 4).
To examine potential associations between subjective and physiological changes between pre- and post-intervention, several Pearson product-moment correlations were computed between the respective change scores (pre–post). In order to reduce the number of correlations, only those outcomes that have shown significant pre–post effects were included. As a result, correlations were computed for pre- to post-intervention changes in resting (mean of baseline and recovery) RMSSD, in EEG gamma power response to the task, in resting (mean of baseline and recovery) EEG power of the gamma band, and improvement in feelings of negative affect in the lab (mean of baseline and recovery), and pre–post overall changes in depression, anxiety, and anger, as well as the five mindfulness facets.
Regarding response to the stress task, change in gamma power response was not associated with improvements in affect pre- to post-intervention (all |r|< 0.14, p > 0.30) or improvements in most self-reported mindfulness facets, except Acting with Awareness (r = 0.35, p = 0.02) (Table 5). However, this correlation was in the direction opposite to our expectations: increase in this mindfulness skill was associated with increased gamma power response. Regarding changes in resting values of the gamma band or RMSSD between pre- and post-interventions, none of the changes was correlated with either changes in affect or changes in mindfulness skills (all |r|< 0.23, p > 0.14) (Table 5).
Discussion
Based on accounts suggesting stress reactivity buffering effects of mindfulness (Creswell & Lindsay, 2014; Ditto et al., 2006), the main aim of the current study was to examine potential combined changes in subjective, cardiac autonomic, and cortical activity during a laboratory protocol including a personally relevant stress recall task in the context of participation in a standardized 8-week MBSR program. The focus was on examining the extent to which favourable overall improvements in subjective affect, normally found in the context of MBIs (Goldberg et al., 2022; Khoury et al., 2013), would be related to acute cardiac and cortical responses to a personally relevant stress task.
Regarding stress task–related activity, only cortical responses in the power spectrum of the gamma band showed significant changes between pre- and post-intervention: at post-intervention, a decrease in the response to the task was found. Similar trends were obtained for not only beta, but also theta spectra. The effects on beta and gamma were in line with our hypothesis. As beta and gamma bands reflect higher cognitive processing, this effect may suggest a lower impact of recalling a stressful event after mindfulness training. Although in a different context and using different measures, this finding is also in line with lower event-related potentials found in a small group of meditators in response to unpleasant visual stimuli (Sobolewski et al., 2011). However, in light of a lack of a randomized control group, we cannot ascribe this effect to the intervention. Other effects, such as regression to the mean, might have been responsible for this finding.
Regarding acute effects on the heart, no changes between pre- and post-intervention responses in heart rate or HRV to the stress recall task were evident, despite the fact that subjective perceived stressfulness of the recalled event decreased at post-intervention. This lack of effect was not anticipated, as mindfulness-based interventions have been suggested to buffer stress responsivity (Creswell & Lindsay, 2014; Morton et al., 2020). However, it is also important to note that the task itself did not result in the expected decrease in HRV, as usually is seen during stressful tasks (Schommer et al., 2003). This does not seem to be the result of a lack of stressfulness of the task, as the average rating across participants indicated substantial subjective stressfulness. It may be speculated that the physiological response might have been different between participants, in some dominated by a classic fight/flight response, but in others by either a freeze response or even prosocial tend-and-befriend response (Keller et al., 2006; Lee et al., 2014; Taylor et al., 2000). As a result, in some participants, this may have yielded a predominant increase in vagal (parasympathetic) tone to the heart instead of a decrease (Adjei et al., 2018; Riem et al., 2020; Scott & Weems, 2014; Sousa et al., 2021). Because most of our participants were female, this might have even been the case for most of our participants, as in previous studies an increase in vagal tone to mental stress has been found in female compared to male participants (Adjei et al., 2018). A similar effect was also reported in participants high in anxiety (Scott & Weems, 2014), a characteristic also present in our sample. In addition, variability in the contents of the recalled event and specific emotion may also play a role, the latter ranging from anger to sadness. Thus, the kind and strength of responses may depend on a combination of (i) characteristics of the participants (here predominantly female with relatively high stress), (ii) the contents of the stressor recalled, and (iii) experienced emotion and subsequent coping strategy. The current findings are in line with findings of a similar study, also reporting a general increase in vagal HRV to a stress recall task in the context of a mindfulness intervention study (Crosswell et al., 2017). The authors speculated that emotion regulation may have been employed during the recall task, which may have increased vagal tone, as found earlier in a female sample (Butler et al., 2006). In addition, our findings are also in line with the overall picture of effects of mindfulness-based interventions on stress-related cardiac autonomic responses, which have been largely equivocal (Morton et al., 2020), possibly as a result of the many factors influencing this effect.
An overall change in heart rate variability was found: RMSSD increased from pre-to-post intervention. This reflects a more vagally driven autonomic influence on the heart, which is in line with the effect obtained regarding subjective negative affect. However, despite this effect being in the expected direction, again in light of a lack of a randomized control group, we cannot ascribe this effect to the intervention. Other effects, such as regression to the mean, might have been responsible for this finding. In previous studies, sometimes similar increases in HRV have been observed of mindfulness-related interventions (Arch et al., 2014), but more often not (Creswell et al., 2014; Crosswell et al., 2017; Nyklíček et al., 2013). To date, it remains difficult to identify the contextual factors responsible for this discrepancy, but it does suggest that the well-documented favourable effects on decrease in subjective negative affect (Goldberg et al., 2018, 2022; Khoury et al., 2013, 2015), also found in the present study, are often not (immediately) translatable to autonomic nervous system functioning.
This is also in line with the finding that none of the correlations between changes in subjective negative affect and in mindfulness skills pre- and post-intervention with changes in cardiac and cortical parameters was significant (except one correlation in the opposite direction, perhaps due to chance in light of multiple testing). While such correlations are seldomly performed, in the few studies that examined an association between subjective and peripheral physiological stress responses, no associations were found (Creswell et al., 2014). Regarding associations between subjective stress reduction and cortical responses, correlations have sometimes been reported in small studies, yielding inconsistent findings: stress reduction correlated with a decrease in amygdala activation in response to unpleasant pictures (Bauer et al., 2019), higher mindfulness as a state correlated with lower ERP response to emotional pictures, and higher mindfulness as a trait correlated with a higher ERP response to emotional pictures (Eddy et al., 2015).
Overall, we can conclude that the favourable general improvements in subjective affect, found both in the context of MBIs (Goldberg et al., 2022; Khoury et al., 2013) and the present study, do not seem to be clearly related to acute cardiac or cortical responses to a personally relevant stress task. It may be speculated that any peripheral physiological effects, if present, may take a longer time to get established with mindfulness meditation practice. This should be examined in future investigations including a longer-term follow-up (at least 6 months or longer) (Loucks et al., 2019; Morton et al., 2020).
Limitations and Future Research
Several limitations should be acknowledged. First and foremost, the uncontrolled design prevents any possible conclusions along causal lines. However, the changes found regarding scores on subjective negative affect and mindfulness skills, which are comparable to previous studies, strengthen the confidence in the likelihood that the subjective changes are associated with the intervention and, as a consequence, the examination of their correlations with physiological indices may be meaningful. A second limitation is the limited size of the group, which reduced the power to obtain effects especially regarding correlations between outcomes (power of 0.66), although power was sufficient to establish medium-sized pre–post intervention effects.
Next, we did not include a measure of sympathetic influence on the heart, such as pre-ejection period. Future research should include such measure to obtain a more complete picture of the autonomic cardiac activity. The number of EEG electrodes employed was limited. However, as we found no differential effects between the electrodes used, the effect of this limitation on the results is expected not to be substantial.
A strength of the current study is the multisystem approach, including subjective affective and cardiac, as well as cortical measures. Furthermore, the current stress recall task was personalized. This has both advantages and disadvantages. A personalized stressor is by its definition more ecologically valid, more relevant, and as a consequence possibly also more stressful. However, it is less standardized and as a result, more interindividual variability in both the content and coping is likely to occur. As discussed above, the latter might have obscured effects on physiological response by different emotions experienced and different coping styles employed. Future research should take into account the different coping strategies participants employ in response to a stressful situation.
Data Availability
Data and analysis scripts used for these studies can be accessed at the Open Science Framework: https://osf.io/5kb2m/. Materials used in the present study can be accessed by the respective references provided in the “Methods” section.
References
Adjei, T., Xue, J., & Mandic, D. P. (2018). The female heart: Sex differences in the dynamics of ECG in response to stress. Frontiers in Physiology, 9, 1616. https://doi.org/10.3389/fphys.2018.01616
Afonso, V. X., Tompkins, W. J., Nguyen, T. Q., & Luo, S. (1999). ECG beat detection using filter banks. IEEE Transactions on Biomedical Engineering, 46(2), 192–202. https://doi.org/10.1109/10.740882
Aftanas, L. I., & Golocheikine, S. A. (2001). Human anterior and frontal midline theta and lower alpha reflect emotionally positive state and internalized attention: High-resolution EEG investigation of meditation. Neuroscience Letters, 310(1), 57–60. https://doi.org/10.1016/s0304-3940(01)02094-8
Arch, J. J., Brown, K. W., Dean, D. J., Landy, L. N., Brown, K. D., & Laudenslager, M. L. (2014). Self-compassion training modulates alpha-amylase, heart rate variability, and subjective responses to social evaluative threat in women. Psychoneuroendocrinology, 42, 49–58. https://doi.org/10.1016/j.psyneuen.2013.12.018
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
Bauer, C. C. C., Caballero, C., Scherer, E., West, M. R., Mrazek, M. D., Phillips, D. T., Whitfield-Gabrieli, S., & Gabrieli, J. D. E. (2019). Mindfulness training reduces stress and amygdala reactivity to fearful faces in middle-school children. Behavioral Neuroscience, 133(6), 569–585. https://doi.org/10.1037/bne0000337
Berkovich-Ohana, A., Glicksohn, J., & Goldstein, A. (2012). Mindfulness-induced changes in gamma band activity - implications for the default mode network, self-reference and attention. Clinical Neurophysiology, 123(4), 700–710. https://doi.org/10.1016/j.clinph.2011.07.048
Bishop, S. R., Lau, M. A., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., Segal, Z. V., Abbey, S., Speca, M., Velting, D., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11(3), 230–241. https://doi.org/10.1093/clipsy/bph077
Bohlmeijer, E., ten Klooster, P. M., Fledderus, M., Veehof, M., & Baer, R. (2011). Psychometric properties of the Five Facet Mindfulness Questionnaire in depressed adults and development of a short form. Assessment, 18(3), 308–320. https://doi.org/10.1177/1073191111408231
Bremner, J. D., Mishra, S., Campanella, C., Shah, M., Kasher, N., Evans, S., Fani, N., Shah, A. J., Reiff, C., Davis, L. L., Vaccarino, V., & Carmody, J. (2017). A pilot study of the effects of Mindfulness-Based Stress Reduction on post-traumatic stress disorder symptoms and brain response to traumatic reminders of combat in operation enduring freedom/operation Iraqi freedom combat veterans with post-traumatic stress disorder. Frontiers in Psychiatry, 8, 157. https://doi.org/10.3389/fpsyt.2017.00157
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: Mindfulness and its role in psychological well-being. Journal of Personality and Social Psychology, 84(4), 822–848. https://doi.org/10.1037/0022-3514.84.4.822
Burg, J. M., & Michalak, J. (2011). The healthy quality of mindful breathing: Associations with rumination and depression. Cognitive Therapy and Research, 35, 179–185. https://doi.org/10.1007/s10608-010-9343-x
Butler, A. C., Chapman, J. E., Forman, E. M., & Beck, A. T. (2006). The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26(1), 17–31. https://doi.org/10.1016/j.cpr.2005.07.003
Chiesa, A., & Serretti, A. (2010). A systematic review of neurobiological and clinical features of mindfulness meditations. Psychological Medicine, 40(8), 1239–1252. https://doi.org/10.1017/S0033291709991747
Creswell, J. D., & Lindsay, E. K. (2014). How does mindfulness training affect health? A mindfulness stress buffering account. Current Directions in Psychological Science, 23(6), 401–407. https://doi.org/10.1177/0963721414547415
Creswell, J. D., Pacilio, L. E., Lindsay, E. K., & Brown, K. W. (2014). Brief mindfulness meditation training alters psychological and neuroendocrine responses to social evaluative stress. Psychoneuroendocrinology, 44, 1–12. https://doi.org/10.1016/j.psyneuen.2014.02.007
Creswell, J. D., Lindsay, E. K., Villalba, D. K., & Chin, B. (2019). Mindfulness training and physical health: Mechanisms and outcomes. Psychosomatic Medicine, 81(3), 224–232. https://doi.org/10.1097/PSY.0000000000000675
Crosswell, A. D., Moreno, P. I., Raposa, E. B., Motivala, S. J., Stanton, A. L., Ganz, P. A., & Bower, J. E. (2017). Effects of mindfulness training on emotional and physiologic recovery from induced negative affect. Psychoneuroendocrinology, 86, 78–86. https://doi.org/10.1016/j.psyneuen.2017.08.003
Denollet, J. (1993). Emotional distress and fatigue in coronary heart disease: The Global Mood Scale (GMS). Psychological Medicine, 23(1), 111–121. https://doi.org/10.1017/s0033291700038903
Ditto, B., Eclache, M., & Goldman, N. (2006). Short-term autonomic and cardiovascular effects of mindfulness body scan meditation. Annals of Behavioral Medicine, 32(3), 227–234. https://doi.org/10.1207/s15324796abm3203_9
Eddy, M. D., Brunye, T. T., Tower-Richardi, S., Mahoney, C. R., & Taylor, H. A. (2015). The effect of a brief mindfulness induction on processing of emotional images: An ERP study. Frontiers in Psychology, 6, 1391. https://doi.org/10.3389/fpsyg.2015.01391
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Wampold, B. E., Kearney, D. J., & Simpson, T. L. (2018). Mindfulness-based interventions for psychiatric disorders: A systematic review and meta-analysis. Clinical Psychology Review, 59, 52–60. https://doi.org/10.1016/j.cpr.2017.10.011
Goldberg, S. B., Riordan, K. M., Sun, S., & Davidson, R. J. (2022). The empirical status of mindfulness-based interventions: A systematic review of 44 meta-analyses of randomized controlled trials. Perspectives on Psychological Science, 17(1), 108–130. https://doi.org/10.1177/1745691620968771
Haenen, S., Nyklíček, I., Van Son, J., Pop, V., & Pouwer, F. (2016). Mindfulness facets as differential mediators of short and longterm effects of Mindfulness-Based Cognitive Therapy in diabetes outpatients: Findings from the DiaMind randomized trial. Journal of Psychosomatic Research, 85, 44–50. https://doi.org/10.1016/j.jpsychores.2016.04.006
Kabat-Zinn, J. (1990). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Delacourt.
Kadengye, D. T., Cools, W., Ceulemans, E., & Van den Noortgate, W. (2012). Simple imputation methods versus direct likelihood analysis for missing item scores in multilevel educational data. Behavior Research Methods, 44(2), 516–531. https://doi.org/10.3758/s13428-011-0157-x
Katmah, R., Al-Shargie, F., Tariq, U., Babiloni, F., Al-Mughairbi, F., & Al-Nashash, H. (2021). A review on mental stress assessment methods using EEG signals. Sensors, 21(15). https://doi.org/10.3390/s21155043
Keller, N. R., Diedrich, A., Appalsamy, M., Miller, L. C., Caron, M. G., McDonald, M. P., Shelton, R. C., Blakely, R. D., & Robertson, D. (2006). Norepinephrine transporter-deficient mice respond to anxiety producing and fearful environments with bradycardia and hypotension. Neuroscience, 139(3), 931–946. https://doi.org/10.1016/j.neuroscience.2006.01.008
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M. A., Paquin, K., & Hofmann, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771. https://doi.org/10.1016/j.cpr.2013.05.005
Khoury, B., Sharma, M., Rush, S. E., & Fournier, C. (2015). Mindfulness-based stress reduction: A meta-analysis. Journal of Psychosomatic Research, 78(6), 519–528. https://doi.org/10.1016/j.jpsychores.2015.03.009
Kirschbaum, C., Pirke, K. M., & Hellhammer, D. H. (1993). The ‘Trier Social Stress Test’: A tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology, 28(1–2), 76–81. https://doi.org/10.1159/000119004
Kummar, A. S., Correia, H., & Fujiyama, H. (2019). A brief review of the EEG literature on mindfulness and fear extinction and its potential implications for Posttraumatic Stress Symptoms (PTSS). Brain Science, 9(10), 258. https://doi.org/10.3390/brainsci9100258
Lee, S. W., Gerdes, L., Tegeler, C. L., Shaltout, H. A., & Tegeler, C. H. (2014). A bihemispheric autonomic model for traumatic stress effects on health and behavior. Frontiers in Psychology, 5, 843. https://doi.org/10.3389/fpsyg.2014.00843
Lindsay, E. K., Young, S., Smyth, J. M., Brown, K. W., & Creswell, J. D. (2018). Acceptance lowers stress reactivity: Dismantling mindfulness training in a randomized controlled trial. Psychoneuroendocrinology, 87, 63–73. https://doi.org/10.1016/j.psyneuen.2017.09.015
Lomas, T., Ivtzan, I., & Fu, C. H. (2015). A systematic review of the neurophysiology of mindfulness on EEG oscillations. Neuroscience and Biobehavioral Reviews, 57, 401–410. https://doi.org/10.1016/j.neubiorev.2015.09.018
Loucks, E. B., Nardi, W. R., Gutman, R., Kronish, I. M., Saadeh, F. B., Li, Y., Wentz, A. E., Webb, J., Vago, D. R., Harrison, A., & Britton, W. B. (2019). Mindfulness-based blood pressure reduction (MB-BP): Stage 1 single-arm clinical trial. PLoS ONE, 14(11), e0223095. https://doi.org/10.1371/journal.pone.0223095
Lutz, A., Slagter, H. A., Dunne, J. D., & Davidson, R. J. (2008). Attention regulation and monitoring in meditation. Trends in Cognitive Science, 12(4), 163–169. https://doi.org/10.1016/j.tics.2008.01.005
McNair, D. M., Lorr, M., & Droppelman, L. F. (1971). Profile of mood states (POMS) manual. Educational and Industrial Testing Service.
Miller, R., & Kirschbaum, C. (2019). Cultures under stress: A cross-national meta-analysis of cortisol responses to the Trier Social Stress Test and their association with anxiety-related value orientations and internalizing mental disorders. Psychoneuroendocrinology, 105, 147–154. https://doi.org/10.1016/j.psyneuen.2018.12.236
Morton, M. L., Helminen, E. C., & Felver, J. C. (2020). A systematic review of mindfulness interventions on psychophysiological responses to acute stress. Mindfulness, 11(9), 2039–2054. https://doi.org/10.1007/s12671-020-01386-7
Mulder, L. J. M. (1988). Assessment of cardiovascular reactivity by means of spectral analysis (unpublished doctoral dissertation). University of Groningen, Groningen, Netherlands.
Nyklíček, I. (2020). Aspects of self-awareness in meditators and meditation-naïve participants: Self-report versus task performance. Mindfulness, 11(4), 1028–1037. https://doi.org/10.1007/s12671-020-01318-5
Nyklíček, I., Mommersteeg, P. M. C., Van Beugen, S., Ramakers, C., & Van Boxtel, G. (2013). Mindfulness-based stress reduction and physiological activity during acute stress: A randomized controlled trial. Health Psychology, 32, 1110–1113. https://doi.org/10.1037/a0032200
Nyklíček, I., Dijksman, S. C., Lenders, P. J., Fonteijn, W. A., & Koolen, J. J. (2014). A brief mindfulness based intervention for increase in emotional well-being and quality of life in percutaneous coronary intervention (PCI) patients: The MindfulHeart randomized controlled trial. Journal of Behavioral Medicine, 37, 135–144. https://doi.org/10.1007/s10865-012-9475-4
Pauls, C. A., & Stemmler, G. (2003). Repressive and defensive coping during fear and anger. Emotion, 3(3), 284–302. https://doi.org/10.1037/1528-3542.3.3.284
Riem, M. M. E., Kunst, L. E., Bekker, M. H. J., Fallon, M., & Kupper, N. (2020). Intranasal oxytocin enhances stress-protective effects of social support in women with negative childhood experiences during a virtual Trier Social Stress Test. Psychoneuroendocrinology, 111, 104482. https://doi.org/10.1016/j.psyneuen.2019.104482
Rosenkranz, M. A., Davidson, R. J., Maccoon, D. G., Sheridan, J. F., Kalin, N. H., & Lutz, A. (2013). A comparison of mindfulness-based stress reduction and an active control in modulation of neurogenic inflammation. Brain Behavior and Immunity, 27(1), 174–184. https://doi.org/10.1016/j.bbi.2012.10.013
Schommer, N. C., Hellhammer, D. H., & Kirschbaum, C. (2003). Dissociation between reactivity of the hypothalamus-pituitary-adrenal axis and the sympathetic-adrenal-medullary system to repeated psychosocial stress. Psychosomatic Medicine, 65(3), 450–460. https://doi.org/10.1097/01.psy.0000035721.12441.17
Scott, B. G., & Weems, C. F. (2014). Resting vagal tone and vagal response to stress: Associations with anxiety, aggression, and perceived anxiety control among youths. Psychophysiology, 51(8), 718–727. https://doi.org/10.1111/psyp.12218
Segal, Z., Williams, J. M., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression. Guilford.
Singmann, H., Bolker, B., Westfall, J., Aust, F., & Ben-Schachar, M. S. (2015). Afex: Analysis of factorial experiments. R package version 0.13–145. Retrieved from https://cran.r-project.org/web/packages/afex/index.html
Singmann, H., & Kellen, D. (2019). An introduction to mixed models for experimental psychology. In D. H. Spieler & E. Schumacher (Eds.), New methods in cognitive psychology (pp. 4–31). Psychology Press.
Sinha, R., Fuse, T., Aubin, L. R., & O’Malley, S. S. (2000). Psychological stress, drug-related cues and cocaine craving. Psychopharmacology, 152(2), 140–148. https://doi.org/10.1007/s002130000499
Sobolewski, A., Holt, E., Kublik, E., & Wrobel, A. (2011). Impact of meditation on emotional processing–a visual ERP study. Neuroscience Research, 71(1), 44–48. https://doi.org/10.1016/j.neures.2011.06.002
Sousa, R., Petrocchi, N., Gilbert, P., & Rijo, D. (2021). HRV patterns associated with different affect regulation systems: Sex differences in adolescents. International Journal of Psychophysiology, 170, 156–167. https://doi.org/10.1016/j.ijpsycho.2021.10.009
Takahashi, T., Murata, T., Hamada, T., Omori, M., Kosaka, H., Kikuchi, M., Yoshida, H., & Wada, Y. (2005). Changes in EEG and autonomic nervous activity during meditation and their association with personality traits. International Journal of Psychophysiology, 55(2), 199–207. https://doi.org/10.1016/j.ijpsycho.2004.07.004
Tarvainen, M. P., Niskanen, J. P., Lipponen, J. A., Ranta-aho, P. O., & Karjalainen, P. A. (2014). Kubios HRV - heart rate variability analysis software. Computer Methods and Programs in Biomedicine, 113, 210–220. https://doi.org/10.1016/j.cmpb.2013.07.024
Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. (1996). Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Circulation, 93(5), 1043–1065. https://doi.org/10.1161/01.CIR.93.5.1043
Taylor, S. E., Klein, L. C., Lewis, B. P., Gruenewald, T. L., Gurung, R. A., & Updegraff, J. A. (2000). Biobehavioral responses to stress in females: Tend-and-befriend, not fight-or-flight. Psychological Review, 107(3), 411–429. https://doi.org/10.1037/0033-295x.107.3.411
Travis, F., & Shear, J. (2010). Focused attention, open monitoring, and automatic self-transcending: Categories to organize meditations from Vedic, Buddhist, and Chinese traditions. Consciousness and Cognition, 19(4), 1110–1118. https://doi.org/10.1016/j.concog.2010.01.007
Wald, F. D. M., & Mellenbergh, G. J. (1990). De verkorte versie van de Nederlandse vertaling van de Profile of Mood States (POMS) [The shortened version of the Dutch translation of the Profile of Mood States (POMS)]. Nederlands Tijdschrift Voor De Psychologie, 45, 86–90.
Welch, P. D. (1967). The use of Fast Fourier Transform for the estimation of power spectra: A method based on time averaging over short, modified periodograms. IEEE Transactions on Audio and Electroacoustics, 15(2), 70–73.
Author information
Authors and Affiliations
Contributions
IN has initiated the manuscript, conducted Studies 1 and 3, performed analyses of Studies 1 and 3, and had largely written the manuscript. BO has conducted Study 2, including the analyses, written parts of the manuscript, and edited other parts of the manuscript. MB has co-conducted Study 1 and has edited the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The study has been approved by the Ethical Review Board of Tilburg University (EC-2012.20) and has therefore been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Informed Consent
All participants provided written informed consent before start of the study.
Conflict of Interest
The authors declare no competing interests.
Use of Artificial Intelligence
The authors declare not to have used artificial intelligence for any purpose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Nyklíček, I., van Boxtel, G.J.M., van der Donk, L.J. et al. Are Subjective Benefits of Mindfulness-Based Stress Reduction Related to Changes in Cardiac and Cortical Responses to a Stress Task?. Mindfulness (2024). https://doi.org/10.1007/s12671-024-02358-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s12671-024-02358-x