Abstract
Objectives
The study aimed to examine the effects of an online Mindfulness-Based Stress Reduction program on stress and quality of life levels of family caregivers of cancer patients.
Method
The study used a randomized controlled trial design with a pre-test (T1), follow-up (T2) and post-test (T3) which was conducted with 104 family caregivers of cancer patients. Data collection was conducted using the Caregiver and Patient Descriptive Information Form, Caregiver’s Stress Scale and The Caregiver Quality of Life Index Cancer Scale. T1 measurements were conducted for experimental (n = 50) and control groups (n = 54). After the 8-week online Mindfulness-Based Stress Reduction program of the experimental group, T2 measurements were taken for both groups. Four weeks later, the T3 measurement was collected for both experimental and control groups.
Results
A statistically significant difference over time was detected between the mean Caregiver’s Stress Scale scores of the experimental group in the T1, T2, and T3. There was no significant difference in the control group over time. A statistically significant difference was detected in the mean Caregiver Quality of Life Index Cancer Scale total score of the experimental group across T1, T2, and T3. When the scale pre-test mean scores were compared between the groups, no significant differences were detected for T1, but a statistically significant difference was found between the T2 and T3 scores.
Conclusion
In the study, it was determined that the online Mindfulness-Based Stress Reduction program had an effect on reducing stress and improving the quality of life.
Preregistration
The research was registered on http://clinicaltrials.gov (ID:NCT05831293).
Similar content being viewed by others
Cancer is a significant healthcare concern worldwide and in Turkey, with high mortality and morbidity rates. There were 19 million cancer patients globally in 2020, and this number is expected to reach 24 million by 2030 (Sung et al., 2021). In Turkey, there were 233,834 new cancer cases reported in 2020, with 126,335 cancer-related deaths. These numbers emphasize the critical need to address cancer and improve patient outcomes (Sung et al., 2021). Cancer not only affects individuals who have been diagnosed with it, but also has an impact on their caregivers, spouses, friends, and family members (Ugalde et al., 2021). As individuals with cancer undergo aggressive treatments to combat the disease, they often need their caregivers to help manage the various symptoms and side effects (Taleghani et al., 2021). The burden of caregivers increases in the last few years as they provide support and assistance during this challenging time (Washington et al., 2021). Studies have shown that this burden can lead to sleep disturbances, fatigue, depression, and reduced quality of life for caregivers (Ellis et al., 2021; Guerra-Martín et al., 2023). Caregivers must receive appropriate support to manage their responsibilities and maintain their well-being (Cai et al., 2021). To adequately address the needs of caregivers, healthcare staff should provide supportive interventions (Robbins et al., 2020). Among the various interventions available, the Mindfulness-Based Stress Reduction program (MBSR) has proven to be effective in reducing symptoms such as anxiety, stress, fatigue, chronic pain, and depression (Li et al., 2023). MBSR was developed by Kabat-Zinn in 1982 to relieve chronic pain in patients. This program focuses on providing individuals with self-regulation skills and ensuring mind-body integrity through awareness exercises (Kabat-Zinn, 1982). MBSR is used to treat a variety of psychological disorders, such as depression (Deyo et al., 2009), anxiety disorders (Vøllestad et al., 2011) and post-traumatic stress disorder (Schure et al., 2018). It has also been adapted and applied to other problems such as stress (Song & Lindquist, 2015), suicidal ideation (Serpa et al., 2014) and cancer (Carlson et al., 2007). MBSR has proven to be a useful tool to reduce stress levels and improve physical and emotional well-being of caregivers of cancer patients (Ahmad & Al-Daken, 2022; Noei et al., 2023; Vinci et al., 2019). MBSR is a technique that offers several benefits, including ease of use, low cost, and long-term effects (An et al., 2022).
Healthcare professionals need to consider incorporating such evidence-based programs into their practice to better support caregivers. By doing so, they can enhance the overall well-being of both the caregivers and the patients they care for (Kubo et al., 2019). However, integrating these interventions for caregivers, including complementary therapies, into healthcare models can be challenging (Sharp et al., 2018). With the rapid advancement of technology, online interventions have become the preferred form of communication for many people (Şen Pakyürek & Korkmaz Yayın, 2023). Online interventions have many advantages, including reaching a wider audience, reducing costs, and providing greater flexibility in time and location. (Sevim & Gezer, 2021). Online research on mindfulness interventions is limited. However, in their studies evaluating the effects of Glück and Maercker’s (2011) 2-week and Krusche et al.’s (2013) 4–6 week internet-based mindfulness intervention on perceived stress and awareness, they used audio files, animation studies and written text sources as training materials. They evaluated participants’ daily meditation experiences through a survey. The results showed a significant decrease in perceived stress level scores between pretest and posttest (Glück & Maercker, 2011; Krusche et al., 2013). The authors posited that online MBSR program may be effective in reducing stress and improving quality of life in cancer caregivers.
Thus, the current study used a randomized controlled design to test the following two hypotheses: The perceived stress level of cancer caregivers in the experimental group will decrease compared to those in the control group (Hypothesis 1); the quality of life of cancer caregivers in the experimental group will increase compared to those in the control group (Hypothesis 2).
Method
Participants
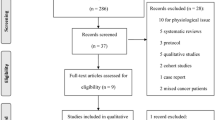
The study was conducted on 142 caregivers of cancer patients who received outpatient chemotherapy treatment at a university hospital between December 2022 and March 2023. The sample size for the study was determined using the “G. Power-3.1.9.2” program. According to Cohen (Jacob Cohen, 2013), a total of 124 people were needed for the study, with 62 participants in both the experimental and control groups. The effect size was medium, at 0.5%, with a level of error of 0.05% and a confidence interval of 0.95%. However, after applying the inclusion and exclusion criteria, a total of 20 participants had to be excluded from the study. As a result, the final sample consisted of 104 participants (Fig. 1; Participant Flow Chart).
Following the completion of pretests, the participants’ enrollment list was generated using the SPSS Program (version 20, SPSS Inc, Chicago, IL), and block randomization was conducted. The 104 participants were divided into two groups at a ratio of 1:1. To ensure unbiased results, the blinding method was employed for both the researcher who collected the data and the statistician who was not aware of the groups encoded the data on a computer.
Inclusion Criteria
The inclusion criteria for the caregivers: (a) to be primarily responsible for patient care, (b) have no psychiatric problems, (c) be at least 18 years of age, (d) be able to read and write, (e) have internet access at home, (f) not receive or plan to receive therapy support during the education process, and (g) have no previous experience with mindfulness (Ahmad & Al-Daken, 2022; Taleghani et al., 2021; Vinci et al., 2019).
Exclusion Criteria
The caregivers (a) who wanted to quit the study, (b) who did not agree to participate in the study, and (c) who were not at a level to answer cognitively to the questions asked (Guerra-Martín et al., 2023; Kubo et al., 2019; Unsar et al., 2021).
Exclusion Criteria during the Study
-
a)
Not participate in any of the eight sessions of the training program.
-
b)
Not participating in any of T1, T2, and T3.
Procedure
The online MBSR training program has been developed in accordance with the guidelines set by John Kabat-Zinn. The program incorporates the four fundamental components of MBSR, which are (1) body scanning exercises, (2) mental exercises that concentrate on the breath, (3) physical exercises that enhance awareness of bodily sensations, and (4) practicing being fully aware during everyday activities by using the breath as an anchor for the attention (Kabat-Zinn, 2003).
Pretest measurements (T1) were conducted on both the experimental and control groups before the start of the study. Additionally, an 8-week MBSR program was administered online to the caregivers of cancer patients (Table 1). Before starting the online MBSR practice in the experimental group, the researchers prepared verbal and visual materials about the sessions. The program was conducted 4 days a week with 1 session per day, and each session was held for 60–90 min in groups of 10–15 people. The literature suggests that the number of members should be at least 4 (Park et al., 2020) and at most 17 (Johannsen et al., 2016), with the ideal group size being 8–10 people (Norouzi et al., 2017; Zhao et al., 2020). The researcher had carefully planned the schedule of the sessions, taking into account the needs and preferences of the participants. The days, hours, and groups were determined in advance and communicated to the individuals in a timely manner for a smooth and efficient process, ensuring that everyone was well-prepared and able to participate fully.
During the program, participants received SMS messages prior to each session as a reminder to complete their homework and to encourage engagement. The sessions themselves were structured into three sections: a discussion of previous week’s experiences, training, and practice. Mindfulness and meditation exercises were typically conducted at the start of each session, followed by group discussions, review of homework assignments, and introduction of new exercises. The participants in the study were instructed to engage in 15–30 min of daily practice each week. To assist them in performing the assigned meditations, audio recordings were provided to the individuals on a weekly basis. They were encouraged to regularly practice the meditations using these recordings. Once the 8-week MBSR program for the experimental group was completed, data collection forms were administered again to both the experimental and control groups (first post-test measurement, T2). Four weeks after the T2 measurements, the individuals in both groups underwent a second post-test measurement (T3). Following the conclusion of the study, the control group participants who expressed interest in the MBSR program were given the same program and training materials as the experimental group.
Measures
Caregiver Descriptive Information Form
In order to gather information about the caregivers, the form that was prepared by the researcher in line with the literature. This form included descriptive questions aimed at determining the socio-demographic characteristics and caregiving status of the participants. The questions covered various aspects such as age, gender, educational background, marital status, degree of relation to the patient, presence of any chronic diseases, presence of another family member with a cancer diagnosis, and whether or not they received support in their caregiving role (Guerra-Martín et al., 2023; Taleghani et al., 2021; Unsar et al., 2021).
Patient Descriptive Information Form
The form determined the socio-demographic characteristics of the patients and included information on age, gender, and type of cancer.
Caregiver’s Stress Scale (CSS)
The scale was developed by Robinson (1983) to measure the subjective care burden of caregivers and to quickly identify families with care concerns (Robinson, 1983). The Turkish adaptation of the scale was performed by Uğur and Fadıloğlu (2013). The reliability coefficient of the scale was found to be 0.77. The scale consisted of 13 items. The scoring of the scale is between 0 and 1. The total score of the scale varies between 0 and 13. Scores above 7 indicate the subjective burden of care (Robinson, 1983; Ugur & Fadiloglu, 2013). In the present study, McDonald’s omega was 0.82, Cronbach’s alpha was 0.81.
The Caregiver Quality of Life Index Cancer Scale (CQOLC)
The CQOLC was developed by Weitzner et al. (1999) to measure the quality of life of caregivers of cancer patients, including physical functions, emotional functions, family functions, and social functions. In addition to the questions in the sub-dimensions of burden, discomfort, positive adaptation, and financial distress, there are 8 statements (sleep problems, satisfaction with sexual life, suppression of daily life, mental fatigue, being informed about the disease, patient information about the disease, protection, management of the pain, and family caregiving status), which are evaluated independently of the sub-dimensions, contributing to the total score of the scale. The total score of each sub-dimension and the scale varies between 0 and 140. Higher scores indicate a better quality of life (Weitzner et al., 1999). The reliability and validity of CQOLC in caregivers of cancer patients in our country (Cronbach’s alpha: 0.88) was performed by Karabuğa-Yakar and Pınar (Yakar & Pinar, 2013). In this study, McDonald’s omega of the COQLC was 0.86, Cronbach’s alpha was 0.87.
Data Analyses
The SPSS 20.0 package program was used to evaluate the study data. Categorical variables were evaluated by the Chi-Square to determine homogeneity. To assess baseline differences between the two groups at T1, independent t-tests were employed. For the main analysis, a repeated-measures analysis of variance (ANOVA) was conducted, with time (T1, T2, T3) as the within-factor and group (experimental, control) as the between-factor. Bonferroni post-hoc analyses were performed to explore interaction effects.
Results
There were no statistically significant differences between the experimental and control groups when it came to control variables such as age, gender, educational status, marital status, degree of relation to the patient, presence of any chronic disease, presence of another individual with a cancer diagnosis in the family, and receiving care support. The two groups were similar in terms of these factors (p > 0.05) (Table 2). The average age of the cancer patients who were being cared for by the participants in the study was 58.65 ± 9.65 years. Of these patients, 53.4% were female, and it was found that 32.1% of the patients had lung cancer.
A significant difference was detected in the CSS, T2 and T3 measurements between the groups (p < 0.001). An analysis of variance of two factors indicated a significant interaction between the factors “Group” and “Measurement time” (p < 0.001), as well as a main effect on the factor “Measurement time” (p < 0.001). Furthermore, a significant TIME x GROUP interaction was recorded for the CSS F(1, 102) = 15.59; p = 0.004). Post-hoc analysis using the Bonferroni test revealed a significant decrease in scores on T2 and T3 measurements relative to T1 measurements in the experimental group compared to the control group (p < 0.001). A statistically significant improvement was observed in the individuals of the experimental group after the end of the study, but not in the participants of the control group (Table 3).
A significant difference was detected in the CQOLC, T2 and T3 measurements between the groups (p < 0.001). An analysis of variance of two factors indicated a significant interaction between the factors “Group” and “Measurement time” (p < 0.001), and a main effect on the factor “Measurement time” (p < 0.001). Moreover, a significant TIME x GROUP interaction was recorded for the CQOLC F(1, 102) = 6.35; p = 0.001, with Bonferroni post-hoc analysis reveals a significant increase in scores on T2 and T3 measurements relative to T1 measurements in the experimental group compared to the control group (p < 0.001).
It was observed that the 8-week MBSR program applied to cancer caregivers in the experimental group significantly reduced stress levels and increased quality of life in T2 and T3 measurements, according to the pre-tests.
Discussion
The current study used a randomized controlled design to investigate the effect of an online MBSR program administered to cancer caregivers on their perceived stress and quality of life. While traditional face-to-face mindfulness-based interventions are time-consuming and costly, and qualified trainers are relatively scarce (Sanilevici et al., 2021), alternative online mindfulness interventions may be more accessible because they do not have time and space limitations (Bostock et al., 2019). However the use of technology as a means to deliver mindfulness interventions to cancer patients and their caregivers is a promising yet under-researched area (Mikolasek et al., 2018). Previous studies have shown that non-face-to-face mindfulness practices have become increasingly necessary in this population (Zernicke et al., 2016). However, the evaluation of the effectiveness of such interventions has been limited. Specifically, when reviewing the national and international literature on the MBSR program, it was found that its impact on perceived stress was only evaluated with face-to-face interventions (Yastıbaş & Dirik, 2018; Ding et al., 2023; Yüksel & Bahadır Yılmaz, 2020). In the present study, a significant decrease in CSS scores was observed between the groups at T2 and T3 measurements in comparison to T1. This finding aligns with the results reported by Querestret et al. (2018), who found significant reductions in perceived stress levels through online mindfulness-based cognitive therapy programs (Querstret et al., 2018). Similarly, in a study conducted on caregivers of individuals with intellectual disabilities and autism spectrum disorder, it was reported that the MBSR program led to a significant reduction in psychological stress levels (Singh et al., 2020). However, in contrast to the present study, El Morr et al. (2020) did not observe a significant effect on perceived stress levels during the Covid-19 period when comparing pre- and post-test outcomes of an 8-week MBSR application (El Morr et al., 2020). It is plausible to attribute this difference to the timing of their study, which took place amidst the Covid-19 pandemic and involved exposure to distinct stressors. Consequently, Hypothesis 1 of the present study was supported, suggesting that the MBSR program effectively reduces stress levels in the experimental group as compared to the control group.
The increasing cancer rates necessitate the development and implementation of mindfulness-based intervention programs aimed at enhancing the quality of life for cancer patients and their caregivers, while safeguarding their psychological and physical health (Ataç, 2021). The present study revealed a significant increase in T2 and T3 measurements when compared to T1 in the CQOLC scale. Similarly, a study conducted by Johns et al. (2020) demonstrated that mindfulness-based interventions improved the quality of life of caregivers of cancer patients (Johns et al., 2020). In a study conducted by Pagnini et al. (2016), it was found that caregivers who had high levels of mindfulness experienced lower care burden scores and higher quality of life scores. These findings may have significant implications for healthcare professionals who work with caregivers and emphasize the importance of incorporating mindfulness-based interventions in caregiving settings. It is important to further explore the role of mindfulness in caregiving and its potential to enhance the quality of life for all those involved (Pagnini et al., 2016). In a study examining the impact of the MBSR program on caregivers of individuals with intellectual disabilities and autism spectrum disorder, it was reported that there was a significant decrease in psychological stress levels and an increase in the quality of life among caregivers (Singh et al., 2020).
Mindfulness can aid in managing negative emotions, reduce the effects of care burden, and promote psychological adjustment. (Ellis et al., 2021; Noei et al., 2023). Practicing mindfulness may help prevent the negative effects of caregiving and a low level of mindfulness could even encourage negative effects (Delaney, 2018). The present study parallels this idea and supports these statements. This finding supports Hypothesis 2 that the MBSR program, which aims to improve mindfulness, can lead to a better quality of life in the experimental group compared to the control group.
Limitations and Future Research
This study demonstrated a statistically significant reduction in the Caregiver’s Stress Scale scores among participants in the experimental group at T2 and T3, following the completion of the 8-week online MBSR program. Moreover, a notable improvement in the Caregiver Quality of Life Index Cancer Scale total score was observed within the experimental group at T2 and T3. The absence of significant differences in the control group emphasizes the specificity of the program’s impact. Overall, our findings support the efficacy of the online MBSR program in alleviating stress and enhancing the quality of life for family caregivers of cancer patients.
This study has several strengths and limitations that should be taken into consideration in order to contribute to future research by examining its results. One of these suggests that increased mindfulness can have a positive impact on caregivers’ well-being by directly or indirectly influencing levels of stress, anxiety and depression (Ahmad & Al-Daken, 2022; Noei et al., 2023). Another is that mindfulness practices are important to include in interventions aimed at improving individuals’ overall quality of life (Johns et al., 2020; Pagnini et al., 2016). We also found that caregivers appreciated the intervention and that many participants learned mindfulness skills using this technology. However, our study has some limitations. First, although this study demonstrates a short-term benefit of using MBSR to improve caregivers’ mental health, long-term benefits have not yet been determined. More research is needed in this area. In addition, it may be recommended in future studies to question different characteristics of caregivers that may affect their stress and quality of life levels (for example, their level of independence in daily tasks or the amount of care they need).
References
Ahmad, M. M., & Al-Daken, L. I. (2022). Clinical trial on mindfulness with family caregivers for patients with cancer. Journal of Cancer Education: The Official Journal of the American Association for Cancer Education, 37(2), 304–310. https://doi.org/10.1007/S13187-020-01812-3
An, A., Hoang, H., Trang, L., Vo, Q., Tran, L., Le, T., Le, A., McCormick, A., Old, D., Williams, K., Mackellar, N. S., Nguyen, G., Luong, E., Nguyen, T., Nguyen, V., K., & Ha, H. (2022). Investigating the effect of mindfulness-based stress reduction on stress level and brain activity of college students. IBRO Neuroscience Reports, 12, 399–410. https://doi.org/10.1016/J.IBNEUR.2022.05.004
Ataç, M. (2021). The effect of mindfulness-based stress reduction program on the quality of life in patients with breast cancer: A systematic review. Journal of Psychiatric Nursing, 12(2), 165–172. https://doi.org/10.14744/phd.2021.68736
Bostock, S., Crosswell, A. D., Prather, A. A., & Steptoe, A. (2019). Mindfulness on-the-go: Effects of a mindfulness meditation app on work stress and well-being. Journal of Occupational Health Psychology, 24(1), 127–138. https://doi.org/10.1037/OCP0000118
Cai, Y., Simons, A., Toland, S., Zhang, J., & Zheng, K. (2021). Informal caregivers’ quality of life and management strategies following the transformation of their cancer caregiving role: A qualitative systematic review. International Journal of Nursing Sciences, 8(2), 227–236. https://doi.org/10.1016/j.ijnss.2021.03.006
Carlson, L. E., Speca, M., Faris, P., & Patel, K. D. (2007). One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behavior and Immunity, 21(8), 1038–1049. https://doi.org/10.1016/J.BBI.2007.04.002
Delaney, M. C. (2018). Caring for the caregivers: Evaluation of the effect of an eight-week pilot mindful self-compassion (MSC) training program on nurses’ compassion fatigue and resilience. PLoS ONE, 13(11), e0207261. https://doi.org/10.1371/journal.pone.0207261
Deyo, M., Wilson, K. A., Ong, J., & Koopman, C. (2009). Mindfulness and rumination: Does Mindfulness Training lead to reductions in the ruminative thinking Associated with Depression? EXPLORE, 5(5), 265–271. https://doi.org/10.1016/J.EXPLORE.2009.06.005
Ding, F., Wu, J., & Zhang, Y. (2023). Can mindfulness-based stress reduction relieve depressive symptoms? A systematic review and meta-analysis. Journal of Pacific Rim Psychology, 17, 1–16. https://doi.org/10.1177/18344909221145814
El Morr, C., Ritvo, P., Ahmad, F., & Moineddin, R. (2020). Effectiveness of an 8-week web-based mindfulness virtual community ıntervention for university students on symptoms of stress, anxiety, and depression: Randomized controlled trial. JMIR Mental Health, 7(7), e18595. https://doi.org/10.2196/18595
Ellis, K. R., Oh, S., Hecht, H. K., & Northouse, L. (2021). Symptom distress and quality of life among Black americans with cancer and their family caregivers. Psycho-Oncology, 30(8), 1356–1365. https://doi.org/10.1002/pon.5691
Glück, T. M., & Maercker, A. (2011). A randomized controlled pilot study of a brief web-based mindfulness training. BMC Psychiatry, 11, 175. https://doi.org/10.1186/1471-244X-11-175
Guerra-Martín, M. D., Casado-Espinosa, M. D. R., Gavira-López, Y., Holgado-Castro, C., López-Latorre, I., & Borrallo-Riego, Á. (2023). Quality of life in caregivers of Cancer patients: A Literature Review. International Journal of Environmental Research and Public Health, 20(2), 1570. https://doi.org/10.3390/ijerph20021570
Cohen, J. (2013). Statistical power analysis for the behavioral sciences (2nd ed.). Routledge.
Johannsen, M., O’Connor, M., O’Toole, M. S., Jensen, A. B., Højris, I., & Zachariae, R. (2016). Efficacy of mindfulness-based cognitive therapy on late post-treatment pain in women treated for primary breast cancer: A randomized controlled trial. Journal of Clinical Oncology, 34(28), 3390–3399. https://doi.org/10.1200/JCO.2015.65.0770
Johns, S. A., Beck-Coon, K., Stutz, P. V., Talib, T. L., Chinh, K., Cottingham, A. H., Schmidt, K., Shields, C., Stout, M. E., Stump, T. E., Monahan, P. O., Torke, A. M., & Helft, P. R. (2020). Mindfulness Training supports quality of life and advance care planning in adults with metastatic cancer and their caregivers: Results of a pilot study. American Journal of Hospice and Palliative Medicine, 37(2), 88–99. https://doi.org/10.1177/1049909119862254
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: Theoretical considerations and preliminary results. General Hospital Psychiatry, 4(1), 33–47. https://doi.org/10.1016/0163-8343(82)90026-3
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10(2), 144–156. https://doi.org/10.1093/CLIPSY.BPG016
Krusche, A., Cyhlarova, E., & Williams, J. M. G. (2013). Mindfulness online: An evaluation of the feasibility of a web-based mindfulness course for stress, anxiety and depression. British Medical Journal Open, 3(11), e003498. https://doi.org/10.1136/BMJOPEN-2013-003498
Kubo, A., Kurtovich, E., McGinnis, M., Aghaee, S., Altschuler, A., Quesenberry, C., Kolevska, T., & Avins, A. L. (2019). A Randomized controlled trial of mhealth mindfulness ıntervention for cancer patients and ınformal cancer caregivers: A feasibility study within an ıntegrated health care delivery system. Integrative Cancer Therapies, 18, 153473541985063. https://doi.org/10.1177/1534735419850634
Li, J., Li, C., Puts, M., Wu, Y., Lyu, M., Yuan, B., & Zhang, J. (2023). Effectiveness of mindfulness-based interventions on anxiety, depression, and fatigue in people with lung cancer: A systematic review and meta-analysis. International Journal of Nursing Studies, 140, 104447. https://doi.org/10.1016/j.ijnurstu.2023.104447
Mikolasek, M., Witt, C. M., & Barth, J. (2018). Adherence to a mindfulness and relaxation self-care app for cancer patients: mixed-methods feasibility study. JMIR Mhealth Uhealth, 6(12), e11271. https://Mhealth.Jmir.Org/2018/12/. https://doi.org/10.2196/11271
Noei, F., Atashi, V., & Ashouri, E. (2023). The effect of an online mindfulness self-compassion training program on psychological distress in caregivers of patients with cancer. Nursing and Midwifery Studies, 11(2), 90–95. https://doi.org/10.4103/nms.nms_101_21
Norouzi, H., Rahimian-Boogar, I., & Talepasand, S. (2017). Effectiveness of mindfulness-based cognitive therapy on posttraumatic growth, self-management and functional disability among patients with breast cancer. Nursing Practice Today, 4(4), 190–202. https://npt.tums.ac.ir/index.php/npt/article/view/271
Pagnini, F., Bercovitz, K., & Langer, E. (2016). Perceived control and mindfulness: Implications for clinical practice. Journal of Psychotherapy Integration, 26(2), 91–102. https://doi.org/10.1037/int0000035
Park, S., Sato, Y., Takita, Y., Tamura, N., Ninomiya, A., Kosugi, T., Sado, M., Nakagawa, A., Takahashi, M., Hayashida, T., & Fujisawa, D. (2020). Mindfulness-based cognitive therapy for psychological distress, fear of cancer recurrence, fatigue, spiritual well-being, and quality of life in patients with breast cancer—a randomized controlled trial. Journal of Pain and Symptom Management, 60(2), 381–389. https://doi.org/10.1016/j.jpainsymman.2020.02.017
Querstret, D., Cropley, M., & Fife-Schaw, C. (2018). The effects of an online mindfulness ıntervention on perceived stress, depression and anxiety in a non-clinical sample: A randomised waitlist control trial. Mindfulness, 9(6), 1825–1836. https://doi.org/10.1007/s12671-018-0925-0
Robbins, T., Hudson, S., Ray, P., Sankar, S., Patel, K., Randeva, H., & Arvanitis, T. N. (2020). COVID-19: A new digital dawn? Digital Health, 6.https://doi.org/10.1177/2055207620920083
Robinson, B. C. (1983). Validation of a caregiver strain index. Journal of Gerontology, 38(3), 344–348. https://doi.org/10.1093/GERONJ/38.3.344
Sanilevici, M., Reuveni, O., Lev-Ari, S., Golland, Y., & Levit-Binnun, N. (2021). Mindfulness-based stress reduction ıncreases mental wellbeing and emotion regulation during the first wave of the covıd-19 pandemic: A synchronous online ıntervention study. Frontiers in Psychology, 12(2), 720965. https://doi.org/10.3389/FPSYG.2021.720965
Schure, M. B., Simpson, T. L., Martinez, M., Sayre, G., & Kearney, D. J. (2018). Mindfulness-based processes of healing for veterans with post-traumatic stress disorder. Journal of Alternative and Complementary Medicine, 24(11), 1063–1068. https://doi.org/10.1089/ACM.2017.0404
Şen Pakyürek, G., & Korkmaz Yayın, B. (2023). Investigating online psychotherapy in the framework of ethical codes. Studies in Psychology, 43(1), 1–39. https://doi.org/10.26650/SP2022-810217
Serpa, J. G., Taylor, S. L., & Tillisch, K. (2014). Mindfulness-based stress reduction (MBSR) reduces anxiety, depression, and suicidal ideation in veterans. Medical Care, 52(12 Suppl 5), S19–S24. https://doi.org/10.1097/MLR.0000000000000202
Sevim, Y., & Gezer, Ş. B. (2021). A different touch of technology to our lives: Being online in family education. Journal of History School, 14, 2723–2752. https://johschool.com/?mod=tammetinandmakaleadi=andkey=50993
Sharp, D., Lorenc, A., Feder, G., Little, P., Hollinghurst, S., Mercer, S., & MacPherson, H. (2018). Trying to put a square peg into a round hole’: A qualitative study of healthcare professionals’ views of integrating complementary medicine into primary care for musculoskeletal and mental health comorbidity. BMC Complementary and Alternative Medicine, 18, 290. https://doi.org/10.1186/S12906-018-2349-8
Singh, N. N., Lancioni, G. E., Medvedev, O. N., Hwang, Y. S., Myers, R. E., & Townshend, K. (2020). Using mindfulness to improve quality of life in caregivers of individuals with intellectual disabilities and autism spectrum disorder. International Journal of Developmental Disabilities, 66(5), 370–380. https://doi.org/10.1080/20473869.2020.1827211
Song, Y., & Lindquist, R. (2015). Effects of mindfulness-based stress reduction on depression, anxiety, stress and mindfulness in Korean nursing students. Nurse Education Today, 35(1), 86–90. https://doi.org/10.1016/J.NEDT.2014.06.010
Sung, H., Ferlay, J., Siegel, R. L., Laversanne, M., Soerjomataram, I., Jemal, A., & Bray, F. (2021). Global Cancer statistics 2020: GLOBOCAN estimates of incidence and Mortality Worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians, 71(3), 209–249. https://doi.org/10.3322/caac.21660
Taleghani, F., Ehsani, M., Farzi, S., Farzi, S., Adibi, P., Moladoost, A., Shahriari, M., & Tabakhan, M. (2021). Challenges to family caregivers in caring for gastric cancer patients from perspectives of family caregivers, patients, and healthcare providers: A qualitative study. Indian Journal of Palliative Care, 27, 521. https://doi.org/10.25259/IJPC_98_21
Ugalde, A., Winter, N., Sansom-Daly, U. M., Rhee, J., Jongebloed, H., Bergin, R. J., & Livingstone, P. M. (2021). Effective integration of caregivers and families as part of the care team for people with cancer. Australian Journal of General Practice, 50(8), 527–531. https://doi.org/10.31128/AJGP-03-21-5897
Ugur, O., & Fadiloglu, C. (2013). Assesment of the reactions of caregivers of a cancer patients: Valdty and reliability of the scale of ‘your reactions helping your family member’ in Turksh society. Indian Journal of Cancer, 50(3), 219–226. https://doi.org/10.4103/0019-509X.118738
Unsar, S., Erol, O., & Ozdemir, O. (2021). Caregiving burden, depression, and anxiety in family caregivers of patients with cancer. European Journal of Oncology Nursing, 50, 101882. https://doi.org/10.1016/j.ejon.2020.101882
Vinci, C., Reblin, M., Bulls, H., Malkhasyan, L., Jim, H., Pidala, J., & Cutolo, E. (2019). Understanding coping strategies of cancer caregivers to inform mindfulness-based interventions: A qualitative study. European Journal of Integrative Medicine, 30, 100936. https://doi.org/10.1016/j.eujim.2019.100936
Vøllestad, J., Sivertsen, B., & Nielsen, G. H. (2011). Mindfulness-based stress reduction for patients with anxiety disorders: Evaluation in a randomized controlled trial. Behaviour Research and Therapy, 49(4), 281–288. https://doi.org/10.1016/J.BRAT.2011.01.007
Washington, K. T., Benson, J. J., Chakurian, D. E., Popejoy, L. L., Demiris, G., Rolbiecki, A. J., & Oliver, D. P. (2021). Comfort needs of Cancer Family caregivers in Outpatient Palliative Care. Journal of Hospice & Palliative Nursing, 23(3), 221–228. https://doi.org/10.1097/NJH.0000000000000744
Weitzner, M. A., Jacobsen, P. B., Wagner, H., Friedland, J., & Cox, C. (1999). The Caregiver Quality of Life Index-Cancer (CQOLC) scale: Development and validation of an instrument to measure quality of life of the family caregiver of patients with cancer. Quality of Life Research, 8(1–2), 55–63. https://doi.org/10.1023/A:1026407010614
Yakar, H. K., & Pinar, R. (2013). Reliability and validity of Turkish version of the caregiver quality of life index cancer scale. Asian Pacific Journal of Cancer Prevention, 14(7), 4415–4419. https://doi.org/10.7314/APJCP.2013.14.7.4415
Yastıbaş, C., & Dirik, G. (2018). Cancer and mindfulness based intervention programs: Systematic review. Current Approaches in Psychiatry, 10(3), 375–393. https://doi.org/10.18863/pgy.357261
Yüksel, A., & Bahadır Yılmaz, E. (2020). The effects of group mindfulness-based cognitive therapy in nursing students: A quasi-experimental study. Nurse Education Today, 85, 104268. https://doi.org/10.1016/j.nedt.2019.104268
Zernicke, K. A., Campbell, T. S., Speca, M., Ruff, K. M., Flowers, S., Tamagawa, R., & Carlson, L. E. (2016). The eCALM Trial: eTherapy for cancer applying mindfulness. Exploratory analyses of the associations between online mindfulness-based cancer recovery participation and changes in mood, stress symptoms, mindfulness, posttraumatic growth, and spirituality. Mindfulness, 7(5), 1071–1081. https://doi.org/10.1007/s12671-016-0545-5
Zhao, Y., Liu, J. E., Lewis, F. M., Nie, Z. H., Qiu, H., Han, J., Su, Y. L., & Yang, S. S. (2020). Effects of mindfulness-based cognitive therapy on breast cancer survivors with insomnia: A randomised controlled trial. European Journal of Cancer Care, 29(5), e13259. https://doi.org/10.1111/ecc.13259
Acknowledgements
We would like to thank all the caregivers who participated in this study.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK).
Author information
Authors and Affiliations
Contributions
Conception and design: NT, EK; data collection: NT, EK; analysis and result interpretation of data: NT; drafting of the manuscript: EK; critical revision of the manuscript for important intellectual content: NT, EK; statistical analysis: NT, EK. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical Approval
Ethical approval was obtained from the Ethics Committee of Atatürk University Faculty of Medicine (221-5/18).
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Use of Artifical Intelligence
Artificial intelligence was not used.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Türkoğlu, N., Kavuran, E. The Effect of Mindfulness-Based Stress Reduction Program on Stress and Quality of Life in Family Caregivers of Patients with Cancer: Randomized Controlled Trial. Mindfulness (2024). https://doi.org/10.1007/s12671-024-02336-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s12671-024-02336-3